Abstract
Background and aim
The aim of this prospective observational cohort study was to verify the relationship between number of drugs used and functional outcome in hip fracture patients undergoing rehabilitation.
Methods
This study was conducted on 139 patients with hip fracture who underwent a rehabilitation program. Efficiency rate in the Functional Independence Measure (FIM) and Berg Balance Scale (BBS), and length of stay (LOS) were the outcome measures.
Results
At the end of rehabilitation, 66.1% of patients showed an increase in number of drugs used, while 33.9% used the same or lower number of drugs than at admission. At the end of rehabilitation patients with increased pharmacotherapy took a higher total number of drug classes (p = 0.001), had longer LOS (p = 0.009) and lower Berg efficiency (p = 0.048) than patients with the same or lower pharmacotherapy. The number of drugs used at discharge was an independent determinant of LOS (beta = 0.19, p = 0.022) and FIM efficiency (beta = − 0.20, p = 0.025). Age was a determinant of LOS (beta = 0.17, p = 0.044) and BBS efficiency (beta = − 0.23, p = 0.009), while CIRS severity was a determinant of BBS efficiency only (beta = − 0.22, p = 0.016).
Discussion
Findings of study indicate that in hip fracture patients, the number of drugs prescribed at discharge is an important indicator of LOS and rehabilitation efficiency.
Conclusions
These findings can help the physician to better plan the rehabilitation of hip fracture patients who require polypharmacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are one of the most common orthopedic injuries affecting the elderly and a common cause of disability and mortality. Of all diseases of the lower limbs, hip fracture is considered to be the one involving the highest costs, whether from a medical, surgical or insurance point of view [1]. Surgery is the definitive treatment for almost all hip fractures, but evidence indicates that a return to optimal functional levels after surgery is not determined so much by the type of operation as by preoperative comorbidities and perioperative (postoperative) complications [2, 3]. Among them, infection, delirium, pressure sores, deep vein thrombosis and hardware failure are considered to be negative prognostic factors [2].
On account of comorbidities and postoperative complications, people with hip fracture are often treated with multiple drugs [4]. However, despite the numerous studies on drugs in patients undergoing surgery for hip fracture [4,5,6,7,8,9], the effect of drugs on the rehabilitation of these patients has not yet been clearly defined. Research interest has mainly focused on the effects that specific single drugs or drug categories have on rehabilitation. Studies have analyzed painkillers, minor tranquillizers and antipsychotics and found that scheduled analgesic intake can improve the functional outcomes of patients with hip fractures after surgery [6], while use of antipsychotics and anticholinergics have a negative effect on functional outcomes of these patients [9, 10]. However, few studies have analyzed the total number of drug classes prescribed [4, 11] and those that did so, did not clearly define correlations between rehabilitation outcome and the number of drugs prescribed at admission to rehabilitation, during rehabilitation, and at discharge. Knowledge of this could be useful for physicians managing the drug therapy and planning rehabilitation of hip fracture patients.
The aim of this prospective observational cohort study was to verify relationships between number of drugs and functional outcome in hip fracture patients undergoing rehabilitation.
Materials and methods
Patients
This prospective cohort study was carried out at Rehabilitation Department of Fondazione Salvatore Maugeri (now Istituti Clinici Scientifici Maugeri IRCCS). All consecutive patients with primary diagnosis of hip fracture admitted to our Rehabilitation Unit between January 2015 and December 2016 were considered for inclusion. Patients referred from other departments outside our district for concomitant acute events, patients having complications related to the surgery during rehabilitation and patients who died or were transferred back to acute care during the course of rehabilitation were excluded.
Patients who did not give informed consent or were not able to walk prior to fracture or perform basic activities without assistance, were not living at home at the time of the fracture, were aged < 66 years, or who had pathological fractures were also excluded.
The Technical Scientific Committee of our Institute approved the study protocol and all patients gave their written informed consent to participate. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Mode of assessment
Clinical evaluation of all patients was performed at admission and at the end of rehabilitation by a qualified team of physiatrists plus geriatrician by means of scales of demonstrated reliability, validity and sensitivity that have been used in previous studies concerning hip fracture recovery. Patient demographic characteristics and comprehensive clinical data including orthopedic treatment (arthroplasty, osteosynthesis, other), time from fracture to admission for rehabilitation (days), and length of stay in hospital (days) (LOS) were also recorded. The instruments used for assessment were:
-
The Anatomical Therapeutic Chemical (ATC) classification was used to measure drug use in hip fractures patients [12]. In the ATC system, drugs are divided into several groups according to the target organ, the mechanism of action and chemical and therapeutic characteristics. The ATC system has 14 main groups. In this study, we recorded only the number of chemical substance (drug classes) and principal therapeutic groups.
-
The Berg Balance Scale (BBS) was used to measure balance among hip fracture patients by assessing the performance of functional tasks [13]. It is a 14-item ordinal scale with four levels ranging from 0 (lowest level of function) to 4 (highest level of function). The maximum total score is 56.
-
The Cumulative Illness Rating Scale (CIRS) was used at admission to evaluate comorbidities [14]. In this study, we considered the average severity of all comorbidities (severity index).
-
The Functional Independence Measure (FIM) was used to assess the patients’ degree of independence and need of assistance in performing basic activities of daily living (ADLs) [15]. It is an 18-item ordinal scale with seven levels ranging from 1 (total dependence) to 7 (total independence). The FIM can be subdivided into a 13-item motor subscale (motor-FIM) and a five-item cognitive subscale (cognitive-FIM). Motor-FIM scores range from 13 to 91 and cognitive-FIM from 5 to 35 with a maximum total score of 126.
-
The Katz ADL scale was used to assess patients’ functional status at admission [16]. It is a six-item scale assessing bathing, dressing, toileting, transferring, continence, and feeding. Katz scores range from 6 (severe functional impairment) to 0 (full function).
-
Hip pain intensity was measured using an 11-point Visual Numeric Scale (VNS) from 0 (no pain) to 10 (intolerable pain) [17].
-
The Muscle Strength Grading Scale (Oxford Scale) [18] was used to assess hip muscle strength. The score ranged from 0 to 5 (where 0 = no movement and 5 = muscle contracts against full resistance). In the current study, the sum of strength of flexor and abductor muscles of hip and strength of quadriceps was considered.
-
A manual goniometer was used to measure the range of motion (ROM) of the hip joint. The sum of ROM in flexion (0–120°), abduction (0–45°) was considered.
Outcome measures
Efficiency in total FIM and BBS and LOS were the outcome measures. Efficiency is the improvement in the rating score of each scale divided by the duration of rehabilitation. It represents the average increase per day obtained by the rehabilitation program [19].
Rehabilitation program
Rehabilitation commenced the day after admission. It consisted of an average of 330 min/week of motor rehabilitation (6 days/week) and, in the last 2 weeks of hospital stay, 150 min/week of occupational therapy (5 days/week). Each patient’s needs, specific goals of rehabilitation and progress/outcomes were discussed at admission and bi-monthly by the rehabilitation team (composed of physicians, physiotherapists, and an occupational therapist). The motor rehabilitation program was based on hip ROM, strengthening and conditioning exercises, and bed to chair mobility, wheelchair skills, pre-gait (sit to stand, standing balance) and gait (parallel bars, walker, crutches) activities, bathroom skills, and ADL training. Patients were discharged when, in the opinion of the rehabilitation team, no further in-hospital improvement with rehabilitation was expected.
Statistical analysis
All statistical analyses were performed with the software application Statistica Version 6 (StatSoft, Tulsa, OK, 2001). Statistical analysis was performed using Shapiro–Wilk test, descriptive statistic tests (mean ± SD, percentage), χ2 tests (Fisher exact or Pearson as appropriate) and Student’s t test to examine differences within and between groups. Sample size was calculated on BBS improvement by a two-sided hypothesis test (type I error rate = 0.01 and a type II error rate = 0.10, 90% power) according to our previous experience in a similar cohort of patients. Postulating a difference in BBS improvement at T1 of 100%, a sample of 27 patients was required.
Spearman’s rank correlation coefficient was used to assess correlations between variables and pre-select the set of independent variables to be used in forward stepwise multiple regression analyses to identify determinants of outcome measures.
Only significant variables at the univariate analysis underwent multivariate analysis. Age, gender, orthopedic treatment, time from fracture to admission for rehabilitation, CIRS severity index, pain VNS, hip ROM, hip muscle strength, Katz ADL score, and pharmacotherapy (drug classes prescribed at admission, discharge, and during rehabilitation) were independent variables investigated in univariate analysis.
Multiple regression analysis was performed and residual distribution and homoscedasticity were checked on efficiency in total FIM and BBS and in LOS as dependent variables. Among dependent variables, LOS only had a normal (Gaussian) distribution. On the contrary, efficiency in total FIM and BBS had not, but could be analyzed with the multiple regression analysis thanks to their unimodal and symmetrical distributions and to the large number of cases (139 patients).
Results
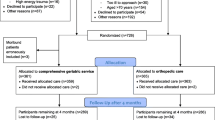
During the study period, 167 patients with primary diagnosis of hip fracture were admitted to our Rehabilitation Unit. During in-hospital rehabilitation, two patients died, 14 were transferred back to acute care hospitals, and 12 patients were aged < 66 years. Thus, 139 patients were eligible for the outcome analysis.
Table 1 shows the demographic and clinical characteristics of the study population.
The average number of drug classes used by hip fracture patients was 7.26 ± 3.8 (range 1–23) at admission and 8.87 ± 3.9 (range 2–20) at discharge and was significantly higher at discharge with respect to admission (p < 0.001). The mean change in drug classes was 1.60 ± 2.3.
At the end of rehabilitation, 66.1% of patients showed an increase in the number of drug classes used, 22.30% had the same number, and 11.6% a lower number. Table 2 reports the characteristics of patients who at discharge had an increased pharmacotherapy (n = 92) vs. those who did not (n = 47). The table shows that patients with increased pharmacotherapy had at admission a higher CIRS comorbidity burden (p = 0.006), while at the end of rehabilitation they received a higher number of total drug classes (p = 0.001) and had a longer LOS (p = 0.005) and lower BBS efficiency (p = 0.048) compared to patients without increased pharmacotherapy.
At admission, patients with increased pharmacotherapy also had a lower use of mineral supplements compared to patients without increased pharmacotherapy (0.08 ± 0.31 vs. 0.23 ± 0.52, p = 0.036). At discharge, they had a higher use of vitamin supplements (1.01 ± 0.48 vs. 0.63 ± 0.48, p < 0.001), antianemic preparations (0.51 ± 0.70 vs. 0.23 ± 0.52, p = 0.019), analgesics (0.50 ± 0.60 vs. 0.28 ± 0.50, p = 0.036), and psychoanaleptic drugs (0.57 ± 0.60 vs. 0.35 ± 0.52, p = 0.041).
After adjusting for psychoanaleptic drugs, there were no differences between groups in LOS (p = 0.069), FIM (p = 0.495) and BBS (p = 0.199) efficiency. During the hospital stay for rehabilitation, 22% of patients with increased pharmacotherapy vs. 13% of those without increased pharmacotherapy (p = 0.127) took drugs short-term for chest and urinary tract infections.
Tables 3 and 4 report relationships between drugs, outcome measures and clinical and demographic characteristics of study patients, assessed by Spearman’s correlation.
Table 3 shows that drugs used at admission had relationships only with drugs taken at discharge (rho 0.80, p < 0.01), while drugs taken at discharge had relationships both with drugs used at admission (rho 0.80, p < 0.01) and with those prescribed during rehabilitation (rho 0.40, p < 0.01).
In addition, the table shows that the number of drugs used at admission (rho 0.38, p < 0.01), drugs prescribed during rehabilitation (rho 0.31, p < 0.01), and drugs taken at discharge (rho 0.54, p < 0.01) were related to CIRS severity.
Table 5 shows the results of multivariate linear regression analyses on outcome measures.
The number of drug classes prescribed at discharge was an independent determinant of final total FIM efficiency score (beta − 0.20 p = 0.025). The number of drug classes at discharge (beta 0.19, p = 0.022) and age (beta = 0.17, p = 0.044) were independent determinants of LOS, while CIRS severity (beta = − 0.22, p = 0.016) and age (beta = − 0.23, p = 0.009) were independent determinants of final BBS efficiency score. The R2 of models was 0.10, 0.06 and 0.20, respectively.
Discussion
The aim of this study was to verify relationships between number of drug classes used during rehabilitation and outcome measures in hip fracture patients. The main finding was that, among the number of drug classes used at admission, during rehabilitation and at discharge, drugs at discharge had the strongest relationship with the outcome measures and were independent determinants of LOS and FIM efficiency.
Relationships between drugs at discharge and LOS were positive, while relationships between drugs at discharge and FIM were negative. Hence, the LOS was longer and the FIM efficiency was lower when the number of drugs prescribed at discharge was higher.
The drugs at discharge were the sum of those at admission plus those added during rehabilitation and, therefore, reflected the comorbidities and clinical picture of discharge in hip fracture patients. This may explain why drugs at discharge had more important associations with outcome measures than either those at admission or those added during rehabilitation (considered separately).
Relationships between drugs and functional recovery have been verified in a few studies [11, 20]. Heltne et al. [20] found a significant negative association between the number of drug changes during the hospital stay and mobility and function 4 months later in hip fracture patients. Laboni found that the use of two or more potentially inappropriate medications at baseline was associated with a longer time to achieve full functional recovery in older adults with hip fracture [11]. Our findings are in line with these two studies, although the aim and methodology of our study was different.
Conversely, drug classes used at admission and during rehabilitation were not determinants of outcomes. They had positive relationships with drug classes at discharge, indicating that, in hip fracture patients, the number of drugs classes at discharge is higher in patients who take a higher number of drug classes at admission and have a higher number of drug changes during rehabilitation.
In the study, associations between drugs used at discharge and outcome measures were present also when we compared patients with vs. without increased pharmacotherapy. At the end of the rehabilitation period patients with increased pharmacotherapy received a higher number of total drugs and demonstrated a longer LOS and lower BBS efficiency. This indicates that a higher use of drugs at discharge is associated with a longer rehabilitation stay and lower average increase in BBS per day obtained by the rehabilitation program.
At admission patients with increased pharmacotherapy differed in CIRS severity score from those with unchanged pharmacotherapy. This finding might have influenced the results observed in patients with increased pharmacotherapy. However, drugs and comorbidities are closely associated factors [10, 19] (the consumption of drugs is higher in patients with higher comorbidity and comorbidity is more severe in patients taking a higher number of drug classes) and either can slow down the rehabilitation program [3, 4, 21,22,23,24,25,26,27] even if in different ways: severe comorbidities can be more frequently complicated by adverse clinical events (as chest infection and heart failure), [3, 21] while single drug can cause adverse effects on muscles, balance, cognitive functions and vigilance [4, 22,23,24,25,26,27].
Therefore, the results observed in patients with increased pharmacotherapy can be influenced by both drugs and comorbidities.
At the end of rehabilitation, patients with increased pharmacotherapy had a higher use of vitamins, antianemic preparations, analgesics, and psychoanaleptic drugs compared to patients without increased pharmacotherapy. These drug classes were added to the drugs prescribed at admission to treat the clinical worsening of pre-existing chronic diseases or new clinical manifestations occurring during the rehabilitation.
Patients with increased pharmacotherapy showed a longer LOS and lower BBS efficiency, but when we adjusted patients with increased pharmacotherapy for psychoanaleptic drugs there were no differences between groups in LOS, FIM and BBS efficiency, showing the presence of negative associations between psychoanaleptic drugs and outcome measures. This is in line with findings of previous studies. Hye–Young Jung et al. found that, in patients with no evidence of delirium symptomatology on admission, those who received antipsychotics during hospital stay had an increased likelihood of death prior to discharge, were more likely to stay longer in the nursing home, and had less functional improvement [9]. Hershkovitz at al. [10] showed that a high admission Anticholinergic drug burden is significantly associated with less favorable discharge functional status in post-acute hip-fractured patients. Moreover, psychoanaleptic drugs are considered “fall-risk increasing drugs” (FRIDs), which can cause adverse effects on muscles, balance, cognitive functions and vigilance of hip fracture patients [4, 22,23,24,25,26,27] and so interfere with the rehabilitation program and slow down functional recovery.
In patients with increased pharmacotherapy the BBS efficiency was lower than that of patients without increased pharmacotherapy. Efficiency represents the average increase per day obtained by the rehabilitation program and is measured dividing the final FIM and BBS score by LOS. At the end of rehabilitation, patients with increased pharmacotherapy differed from those without in LOS but not in final BBS score, indicating that the lower BBS efficiency of patients with increased pharmacotherapy was mainly due to longer LOS.
Our study found that also CIRS severity was a determinant outcome. It was related to LOS and Berg efficiency, but was an independent determinant of Berg efficiency only. This is in line with previous studies demonstrating negative associations between comorbidities and rehabilitation results [3, 28,29,30].
Summarizing, the study shows that in hip fracture patients the number of drugs used at discharge is an important indicator of the duration of rehabilitation and rehabilitation efficiency. These findings can help the physician to better plan the rehabilitation of hip fracture patients who require polypharmacy.
The knowledge that in hip fracture patients the use of a high number of drugs is associated to longer LOS and lower efficiency in total FIM, can help the physician to better plan the rehabilitation of hip fracture patients who require polypharmacy. In these patients, the physician has to plan more intensive rehabilitation programs if he wants to achieve the pre-established objectives within the scheduled times.
Despite these positive considerations, our study has some limitations.
The main limitation of the study is that patients with increased pharmacotherapy also had a higher CIRS severity scores at admission and this may have influenced some results of the study. The size and characteristics of the sample of this study and the close relationships between drugs and comorbidities do not allow to discriminate the role of drugs from that of comorbidity.
Moreover, it was not a population-based study (patients were referred from general hospitals) and, therefore, it does not represent all hip fracture patients. Our patients were admitted to a specific rehabilitation program and, therefore, the results may not apply to other programs with different entry criteria. The study analyzed only therapeutic groups classified by the ATC classification but not specific drug classes or dosage. Finally, we did not include in the regression analysis all possible predictors (i.e., complications related to the surgery were considered exclusion criteria in this study, or reasons for the modification of the pharmacotherapy), but only those independent variables that in previous studies showed to be important predictors of outcome in hip fracture patients [29, 31].
Conclusions
The study showed that in hip fracture patients the number of drugs used at discharge is an important indicator of duration and efficiency of rehabilitation. These findings can help the physician to better plan the rehabilitation program of hip fracture patients who require polypharmacy.
References
Sylliaas H, Thingstad P, Wyller TB et al (2012) Prognostic factors for self-rated function and perceived health in patient living at home three months after a hip fracture. Disabil Rehabil 34:1225–1231
Bruyere O, Brandi ML, Burlet N et al (2008) Post-fracture management of patients with hip fracture: a perspective. Curr Med Res Opin 24:2841–2851
Gialanella B, Prometti P, Monguzzi V et al (2018) Determinants of functional outcome in hip fracture: the role of comorbidity. Aging Clin Exp Res 30:643–650
Kragh A, Elmståhl S, Atroshi I (2011) Older adults’ medication use 6 months before and after hip fracture: a population-based cohort study. J Am Geriatr Soc 59:863–868
Koshoedo S, Soiza RL, Purkayastha R et al (2012) Anticholinergic drugs and functional outcomes in older patients undergoing orthopaedic rehabilitation. Am J Geriatr Pharmacother 10:251–257
Makridis KG, Karachalios T, Kontogeorgakos VA et al (2015) The effect of osteoporotic treatment on the functional outcome, re-fracture rate, quality of life and mortality in patients with hip fractures: a prospective functional and clinical outcome study on 520 patients. Injury 46:378–383
Chin RP, Ho CH, Cheung LP (2013) Scheduled analgesic regimen improves rehabilitation after hip fracture surgery. Clin Orthop Relat Res 47:2349–2360
Shiri-Sharvit O, Arad M, Mizrahi EH et al (2005) The association between psychotropic medication use and functional outcome of elderly hip-fracture patients undergoing rehabilitation. Arch Phys Med Rehabil 86:1389–1393
Jung HY, Meucci M, Unruh MA et al (2013) Antipsychotic use in nursing home residents admitted with hip fracture. J Am Geriatr Soc 61:101–106
Hershkovitz A, Angel C, Brill S et al (2018) The association between anticholinergic drug use and rehabilitation outcome in post-acute hip fractured patients: a retrospective cohort study. Drugs Aging 35:333–341. https://doi.org/10.1007/s40266-018-0533-7
Iaboni A, Rawson K, Burkett C et al (2017) Potentially inappropriate medications and the time to full functional recovery after hip fracture. Drugs Aging 34:723–728
WHO Collaborating Centre for Drug Statistics Methodology (2016) Guidelines for ATC classification and DDD assignment, WHO, Oslo
Berg KO, Wood-Dauphinee SL, Williams JI, Maki B (1992) Measuring balance in the elderly: validation of an instrument. Can J Public Health 83:S7–S11
Parmelee PA, Thuras PD, Katz IR et al (1995) Validation of the cumulative illness rating scale in a geriatric residential population. J Am Geriatr Soc 43:130–137
Tesio L, Granger CV, Perucca L et al (2002) The FIM instrument in the United States and Italy: a comparative study. Am J Phys Med Rehabil 81:168–176
Katz S, Ford AB, Moskowitz RW et al (1963) Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 21:914–919
Ritter PL, González VM, Laurent DD et al (2006) Measurement of pain using the visual numeric scale. J Rheumatol 33:574–580
Miller DW, Hahn JF (1996) General methods of clinical examination. In: Youmans JR (ed) Neurological surgery, ed 4, W.B. Saunders, Philapdelphia, pp 31–32
Tan AK, Taiju R, Menon EB et al (2014) Postoperated hip fracture rehabilitation effectiveness and efficiency in a community hospital. Ann Acad Med Singapore 43:209–215
Heltne M, Saltvedt I, Lydersen S et al (2017) Patterns of drug prescriptions in an orthogeriatric ward as compared to orthopaedic ward: results from the trondheim hip fracture trial-a randomised clinical trial. Eur J Clin Pharmacol 73:937–947
Mathew RO, Hsu WH, Young Y (2013) Effect of comorbidity on functional recovery after hip fracture in the elderly. Am J Phys Med Rehabil 92:686–696
Allain H, Bentué-Ferrer D, Polard E et al (2005) Postural instability and consequent falls and hip fractures associated with use of hypnotics in the elderly: a comparative review. Drugs Aging 22:749–765
Thorell K, Ranstad K, Midlöv P et al (2014) Is use of fall risk-increasing drugs in an elderly population associated with an increased risk of hip fracture, after adjustment for multimorbidity level: a cohort study. BMC Geriatr 4:131
Aizenberg D, Weizman A, Weiss A et al (2015) The association in elderly hospitalized patients, between psychotropic drugs and hip fractures resulting from falls. Exp Aging Res 41:546–555
Correa-Pérez A, Delgado-Silveira E, Martín-Aragón S et al (2018) Fall-risk increasing drugs and prevalence of polypharmacy in older patients discharged from an orthogeriatric unit after a hip fracture. Aging Clin Exp Res. https://doi.org/10.1007/s40520-018-1046-2
Huang AR, Mallet L, Rochefort CM et al (2012) Medication-related falls in the elderly: causative factors and preventive strategies. Drugs Aging 29:359–376
Komagamine J, Hagane K (2017) Intervention to improve the appropriate use of polypharmacy for older patients with hip fractures: an observational study. BMC Geriatr 16: 288
Kristensen MT (2011) Factors affecting functional prognosis of patients with hip fracture. Eur J Phys Rehabil Med 47:257–264
Di Giorgio L, Sodano L, Touloupakis G et al (2012) Proximal femur fractures in elderly patients: the influence of comorbidity on prognosis in the short, medium and long term. Clin Ter 163:95–99
Press Y, Grinshpun Y, Berzak A et al (2007) The effect of co-morbidity on the rehabilitation process in elderly patients after hip fracture. Arch Gerontol Geriatr 45:281–294
Bellelli G, Noale M, Guerini F et al (2012) A prognostic model predicting recovery of walking independence of elderly patients after hip-fracture surgery. An experiment in a rehabilitation unit in Northern Italy. Osteoporos Int 23:2189–2200
Acknowledgements
The Authors thank Rosemary Allpress for English revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. The research was not supported by Pharmaceutical Companies. The research was supported by Institutional funding.
Statement of human and animal rights
The study was conducted in accordance with the principles of the Declaration of Helsinki. The study protocol was approved by the Technical Scientific Committee of our Institute.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gialanella, B., Santoro, R., Prometti, P. et al. Functional recovery in hip fracture patients: the role of pharmacotherapy. Aging Clin Exp Res 32, 49–57 (2020). https://doi.org/10.1007/s40520-019-01175-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01175-w