Key summary points
To determine the prevalence and risk factors for osteoporosis in persons over 65 who live in nursing homes.
AbstractSection FindingsThe prevalence of osteoporosis among residents in nursing homes, based on QUS bone measurements and defined as QUI-T score ≤ − 2.2, was 51.9% in women and 8.5% in men. Physical activity was a more important factor for preserving bone health than calcium intake.
AbstractSection MessageRegular screening for osteoporosis, together with nutrition assessment and physical activity promotion, should be implemented in nursing home settings.
Abstract
Purpose
Low bone mineral density has been reported in institutionalized old people, but limited data are available on the association between bone density and physical activity (PA) and calcium intake in that population. We explored the predictors of bone density in old people living in nursing homes, focusing on PA and calcium intake.
Methods
In a cross-sectional study, we measured bone density with quantitative ultrasound (QUS) in 292 nursing homes residents (233 women and 59 men), mean age 82.4 ± 6.5 years. Information on lifestyle habits and calcium intake was obtained with questionnaires.
Results
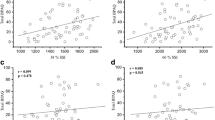
All QUS bone parameters were significantly higher in men than in women (p < 0.001). A T score for quantitative ultrasound index (QUI) of − 2.2 or lower was found in 8.5% of men and 51.9% of women. Participants of both genders with low PA had a significantly lower QUI, QUI-T score compared to those with good/very good PA. When controlling for age, gender, body mass index and calcium intake, participants with good PA had better QUI than those with low PA (β = 7.12 with 95% CI [2.51, 11.74]) The odds of QUI-T score < − 2.2 were lower (OR 0.49 with 95% CI [0.27, 0.90]) in participants with good PA compared to those with low PA.
Conclusions
The prevalence of osteoporosis measured by QUS was high in women but not in men. In our study sample, PA played a more important role than calcium intake in preserving bone density in old people.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis becomes more prevalent with age as bones progressively deteriorate throughout adult’s life. Osteoporotic fractures significantly affect the ability of people to carry out activities of daily living and that is one of the main reasons why older people lose their independence. Many of them require long-term nursing care, and almost one in five people die in the first year after suffering a hip fracture [1]. It has been estimated that 85% of nursing home residents worldwide have osteoporosis and about 40% of all hip fractures occur in this population. [2]. Therefore, it is of great importance to identify institutionalized older people at risk [3]. In order to diagnose osteoporosis in old institutionalized people, it is not always possible to perform a dual-energy x-ray densitometry since it requires transporting them to a radiological facility. A number of studies have reported QUS parameters to be significantly associated with bone structure independently of BMD [4, 5]. QUS has been demonstrated to be sensitive to age-related changes in bone, and it can be useful as an indication of osteoporosis [6, 7].
Living in nursing homes usually includes some sort of change in life habits such as nutrition and physical activity, which are also the most important predictors of bone health. Nutrition is often a significant problem in nursing homes as evidenced by high percentage of old people suffering from malnutrition and consequently low calcium intake [8]. Many studies have shown the necessity for calcium and vitamin D supplementation in old institutionalized people due to their low intake [9,10,11]. However, studies on physical activity prevalence in institutionalized old people are rare, especially those which analyzed the association between the PA and bone mineral density. These studies estimated physical activity through the activities of daily living [12], weekly participation in physical activity [13] or through the present functional status [14] of institutionalized people. All found that systematic physical activity or independence in basic daily activities was significantly associated with better bone mass and lower fracture risk. Moreover, all of the studies agreed that old people in nursing homes have a predominantly sedentary life and that physical activity can improve not only physical functioning but also the overall quality of life.
The objectives of this research are to: (1) assess the bone mineral density in persons over 65 who live in nursing homes; (2) determine the correlation of physical activity (PA) and calcium intake with QUS bone parameters and osteoporotic fractures.
Methods
Participants
The study comprised a population from six public nursing homes for older people in Zagreb. Prior to the measurements, informative lectures were held in the nursing homes about the purpose and method of the investigation. All participants were recruited on a voluntary basis. Participants who had been institutionalized for more than 1 year were included in the study. Informed consent was obtained from all individuals included in the study. The study was designed in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards and was approved by the Ethics Committee of the Institute of Medical Research and Occupational Health.
Measurements
Data were collected using an interviewer-administered questionnaire. History data included information of present or past diseases (including bone fractures), drug consumption, information on PA and smoking. An osteoporotic fracture was defined as either a fracture resulting from a low-impact fall in participants with diagnosis of osteoporosis or a fall resulting in a low-trauma fracture [15]. PA was assessed by time (hours/day) spent in recreational activities including outside walking and exercises. All nursing homes had organized exercises every morning in the duration of half an hour. Physical activity lessons in all nursing homes were quite uniform and included: (a) exercises in the sitting position: chest stretch, arm raises, neck rotation, neck stretch, upper body twist, hip marching and ankle stretch; (b) exercises in standing position: sideways bend and calf stretch, mini squats, sit to stand, sideways leg lift, leg extension and wall press up. Only one exercise for the biceps included light weights. According to duration, PA was categorized as: bad (less than 150 min per week), good (between 150 and 420 min per week) and very good (more than 420 min per week or 1 h per day). A special category were people using invalid chairs but not paralyzed. Although the recommended PA in older adults varied across the studies, the minimum recommended PA level in the guidelines in most studies was 150 min of moderate or vigorous PA per week [16].
A validated, quantitative food frequency questionnaire was used to determine the average daily calcium intake [17]. The amount of calcium intake was calculated using national food composition tables [18].
Anthropometry
Height and weight were measured on a portable stadiometer and scale (Model TTM; Zagreb, Croatia) and were rounded to the nearest 0.1 cm and 0.1 kg, respectively, for each subject. The body mass index (BMI) was calculated as weight (kg) divided by the square of height (m2).
Quantitative ultrasonography
Quantitative ultrasound (QUS) measurements of the heel (non-dominant side) were performed on a Sahara sonometer (Hologic, Bedford, MA). QUS parameters are useful as indicators of low bone density and osteoporosis. The primary parameters measured with ultrasound are broadband ultrasound attenuation (BUA; dB/MHz) and speed of sound (SOS; m/s). These two parameters are combined to give the quantitative ultrasound index (QUI), estimated heel bone mineral density (BMD) and BMD-T score. T scores for QUI were calculated using Croatian QUS normative data [19] according to the formula: (P-YA)/SDya (P patient result, YA young adult mean value, SDya standard deviation of young adult population). Since World Health Organization (WHO) criteria [20] cannot be directly applied to the QUS, we used a QUI-T score ≤ − 2.2 as a criterion for diagnosing osteoporosis, with the Croatian population as referential. A threshold of − 2.2 was suggested for Sahara ultrasound devices to define participants as having osteoporosis at the hip or being at high risk of fracture [21]. We also used BMD-T scores for comparing our results to studies that used WHO criteria in QUS. Instrumental quality control was performed daily by scanning a manufacturer-provided, temperature-sensitive phantom.
Statistics
The results are shown as mean ± standard deviation for continuous variables and as percentages for categorical variable (physical activity). The distribution of variables was tested using the Kolmogorov–Smirnov test. Since most variables were distributed normally, parametric functions were used in data analyses. Differences between groups (means) were tested using the t test. For the categorical variable (physical activity), differences were tested using Chi-squared test or Fisher’s test (if any of the expected frequencies was 5 or less).
Association of QUI with age, gender, body mass index, PA and calcium intake was estimated using a linear regression model. Associations of low QUI (defined as QUI-T score lower than − 2.2) with the same predictors were estimated using a logistic regression model. The logistic regression model predicting osteoporotic fractures additionally included a low QUI as a predictor. Since there were only four male participants in the low QUI model, coefficients and standard errors for this model were estimated using Firth’s correction [22]. For all regression analyses, the unit of calcium intake was set to 100 mg. Since there were no underweight participants, body mass index was included as a continuous variable, while physically disabled participants were excluded from the analyses. All analyses were performed in R, version 3.4.3. (R Foundation for Statistical Computing, Vienna, Austria [23].
Results
The mean age of participants was 82.6 ± 6.4 years for men and 82.4 ± 6.6 years for women (Table 1). The mean time spent in nursing homes was around 10 years. Women had a significantly higher BMI than men (p = 0.001). According to the BMI, the majority of men (51.7%) and women (61.6%) were overweight. Only 41.4% of men and 19.8% of women had normal weight. Men had significantly higher food calcium intake (p = 0.003) than women. Around 15% of men and 2.6% of women were current smokers (p < 0.001). The majority of past smokers (63.2%) had stopped smoking more than 10 years earlier. All bone density parameters were significantly higher in men than in women (p < 0.001). Five men (8.5%) had a QUI-T score of − 2.2 or lower, and five men (8.5%) had a QUI-T score and BMD-T score of − 2.5 or lower. Among the women, 120 (51.9%) had a QUI-T score of − 2.2 or lower, while 92 women (39.8%) had a QUI-T score of − 2.5 or lower and 123 women (52.8%) had a BMD-T score of − 2.5 or lower.
At the time of measurement, 14% of women were taking osteoporosis therapy during 1 year or longer; 10% were taking calcium supplements and 15% vitamin D3. No man was taking osteoporosis therapy, calcium supplements or vitamin D. Nine women (3.9%) and one man were taking anticoagulant therapy, and also 11 women (4.7%) and one man were taking thyroxine therapy. There were no significant differences in QUS parameters between participants who were taking any of these therapies and those who were not taking the therapy (results not presented in tables).
Significantly more women than men had experienced osteoporotic fracture (p = 0.006). Those women had significantly lower QUS parameters as well as BMI (p = 0.011) compared to women without an osteoporotic fracture (Table 2). There were no significant differences in QUS bone parameters or BMI between men with or without osteoporotic fracture.
The majority of women (54.3%) and 42.4% of men had a calcium intake below 600 mg/day, which is half of the DRI (Table 3). These women had a significantly lower QUI (p = 0.039), QUI-T score (p = 0.022), BMD (p = 0.033) and BMD-T score (p = 0.043) and were less physically active (p = 0.001), but were also significantly older (p = 0.009) compared to women with higher calcium intake. There were no significant differences in QUS parameters between men with calcium intake lower or higher than 600 mg/day.
Most men had a good PA (59.3%) or very good PA (13.6%). That prevalence was much lower in women (46.3% and 11.2% respectively). Participants of both genders with low PA had a significantly lower QUI, QUI-T score, BUA and BMD compared to those with a good/very good PA (Table 4). Men with low PA also had a significantly lower SOS (p = 0.0029) compared to men with good/very good PA. Women with low PA were also a significantly older compared to those with good PA (p = 0.002) and had lower BMD-T score (p = 0.007) and lower calcium intake (p < 0.001).
Linear regression showed that, when controlling for age, gender, body mass index and calcium intake, participants with good PA had better QUI than those with low PA (β = 7.12 with 95% confidence interval [2.51, 11.74]) (Table 5). Although participants with very good PA had higher QUI compared to participants with low PA as well (β = 6.63 [− 0.68, 13.95], this effect was not statistically significant.
When controlling for age, gender, body mass index and calcium intake, odds of QUI-T score ≤ − 2.2 were lower (odds ratio 0.49 with 95% confidence interval [0.27, 0.90]) in participants with good PA compared to those with low PA (Table 5), meaning that participants with better PA had better QUI. Although participants with very good PA had even lower odds of a T score < − 2.5 (odds ratio 0.46 [0.17, 1.20]), this effect was not statistically significant. Participants with osteoporosis had twice as high odds of osteoporotic fracture (odds ratio 2.16 [1.11, 4.19]) as those with higher QUI-T scores.
Discussion
The results of our study showed that the prevalence of osteoporosis, based on QUS bone measurements and defined as QUI-T score ≤ − 2.2, was high among old women in nursing homes, but not in men. Our participants had lower QUS parameters compared to their non-institutionalized Croatian counterparts, where the prevalence of osteoporosis using a QUI-T score threshold of –2.5 was 39.0% in women [19]. When the criteria for definition of osteoporosis were equalized within that population, the prevalence in our institutionalized female participants was slightly higher. In another sample of old healthy Croatian people, with a mean age around 78 years, the prevalence of osteoporosis using the same threshold of T < − 2.5 was 4.0% in men and 18.6% in women [24], which was significantly lower than in our participants from nursing homes. When comparing our results with older community-dwelling people from non-Croatian populations, the osteoporosis prevalence, based on QUS measurement, was higher in our female participants [25,26,27]. That difference was not as pronounced in our male participants.
Studies on osteoporosis in institutionalized old people are rare. To the best of our knowledge, there are three studies that were based on ultrasound bone densitometry and to which we have been able to compare our results directly. In one study on institutionalized older Thai people (mean age 77.3 years), the cutoff value for defining osteoporosis was set much lower (BMD-T score < 1.6), so the prevalence of osteoporosis was 71.4% in men and 81.6% in women [12]. If the same criteria were applied to our study population, the prevalence of osteoporosis would be 94.9% in men and 100% in women, which is much higher than in the Thais. A study from Ekman [28] showed that 95% women and 51% of men, nursing home residents from Sweden, aged 84 years, had osteoporosis, which is a higher prevalence than in our study. The third study on 49 women from the USA, aged 89 years, showed a prevalence of osteoporosis of 59% [29]. Studies on institutionalized people based on DXA measurements are also relatively uncommon. They showed a prevalence of T score < 2.5 between 67% and 92% in nursing home residents, older than 80 years [14, 30, 31]. Two studies [32, 33] comprised a relatively low number of institutionalized adults, but with intellectual or developmental disability and much lower age (mid-40s). In most of those participants (between 50 and 89%), a low BMD, defined as T score < − 1.0, was found.
In our study group, the strongest lifestyle predictor of bone density and osteoporotic fractures was PA. It is expected that older age groups are less likely to be regularly active. Nursing homes in our study provided their residents the opportunity for low-intensity exercises, focused on strength and balance, in the duration of half an hour, 5 days a week and under the supervision of a physiotherapist. Approximately one-third of our participants (36.6%) attended these exercises on a daily basis. That is similar to a study by Almeida [34], where nearly 41% participants from nursing homes always attended exercises. Moreover, four of six nursing homes from our study were surrounded with quite large landscaped green areas, which allowed their users to walk around the nursing homes. So, our participants had relatively good settings for appropriate PA, but a relatively small number of residents used them routinely. In general, PA in old people, especially in those from nursing homes, does not attract great interest so limited data are available. Most studies proved that regular exercises in institutionalized old people were well tolerated and that they also improved their strength and mobility in different ranges [16, 35, 36]. Considering bone density, it is known that PA and mechanical forces created by muscle contraction exert the load to bones which impacts bone density, strength and architecture. However, the bone–muscle interaction changes with aging. In old people, osteoporosis often coexists with sarcopenia, and there is more evidence about common pathogenic pathways between those two conditions, which include reduced anabolic hormone secretion, increased inflammatory cytokine activity and reduced physical activity. It is therefore suggested that regular physical activity is considered as the main treatment to improve both muscle health and bone density [37]. Although no specific study included nursing home residents, interventional studies generally showed positive effects of physical activity on bone density and fracture incidence in old people of both genders [38,39,40] or only in men [41].
Our results indicate that bone mineral density in old people was more influenced by PA than by calcium intake. The dietary calcium intake in our participants was very low, approximately half of the recommended dairy intake. All nursing homes from our study had similar menus and nursing home residents usually consumed very similar foods. Only a small proportion of our participants supplemented their diet with dairy products. These findings are consistent with previous research on diet quality in nursing home residents in Zagreb, which showed that their entire diet needed improvement [42]. In that study, only 3.2% of participants had an adequate calcium intake (6.5% men and 2.5% women) and approximately 53% of residents had calcium intake below 50% of adequate intake value, which is similar to our results.
We confirmed in regression analysis that better QUS parameters were more associated with better PA than with greater calcium intake. Since our participants, but probably most older people, consume insufficient amounts of calcium, physical activities in older age may be dominant as a positive factor in preserving an adequate bone mass. Although there is a lack of data on old institutionalized people, results from other studies commonly suggest a positive and interactive association of bone density with dietary calcium intake and PA. Some studies have shown a greater influence of calcium intake than PA [43] while others have shown the opposite [13, 44]. Only one study [45] included institutionalized older people and showed that calcium and vitamin D supplementation resulted in a moderate reduction in femoral neck bone loss. However, it should be considered that the association between calcium and PA with bone is influenced by complex genetic and environmental interaction and that the measurements of dietary calcium intake and PA at a single time point may not reflect long-term exposure. It is expected that people from nursing homes change their usual domestic habits when they enter an institution. Our participants were mostly over 80 years old and had spent a relatively long time in nursing homes. Therefore, they had been “exposed” to living conditions in nursing homes long enough for us to presume that their lifestyle, including PA and nutrition, could have had an impact on their bone health.
There are several limitations to this study. Firstly, the cross-sectional design and retrospective data collection did not permit reliable conclusions about the causality. However, the data on QUS bone parameters in older people from previous studies in Croatia enabled us to compare our results with non-institutionalized peers, which made it possible to make conclusions about the differences in QUS parameters. The second limitation is the lack of DXA measurements. Though many studies found a good correlation between QUS and DXA measurements, it is mainly used as a pre-screening tool for osteoporosis due to lower precision of the QUS method and also due to different skeletal regions. Our study took place in nursing homes, since we assume that old people would not respond to DXA measurements which should be performed in medical institutions. We also had to compare our results of ultrasound densitometry to DXA bone density results from other studies, since published studies on ultrasound bone stiffness in old people from nursing homes are rare. Another limitation to this study is the relatively small number of participants. However, our study sample was uniform according to age and therefore comparable to other studies that comprised participants of a similar age. It should also be noted that most studies on old people over 80 also comprised a small number of respondents. The lack of a structured questionnaire for assessing physical activity, which could probably have included the period before entering nursing homes, and also a relatively low recruitment rate (around 33%) are also among the limitations of the study.
Conclusions
The prevalence of osteoporosis, estimated by QUS, was high in old female nursing home residents who participated in this study. Although men did not have a high prevalence of osteoporosis, in both genders the prevalence was higher than in other national studies on old people who did not live in nursing homes. Therefore, we presume that living in an institutionalized place was an independent risk factor for losing bone density in our study sample. Our nursing home residents had low mean calcium intake and inadequate PA. However, the PA showed to be a more important factor for preserving bone health than calcium intake. Together with regular screening for osteoporosis, which could be performed by QUS, it is necessary to implement other screenings and preventive measures for osteoporosis in nursing home settings, like nutrition assessment and PA promotion.
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Duque G, Lord SR, Mak J, Ganda K, Close JJT, Ebeling P, Papaioannou A, Inderjeeth CA (2016) Treatment of osteoporosis in Australian residential aged care facilities: update on consensus recommendations for fracture prevention. J Am Med Dir Assoc 17:852–859
US Preventive Services Task Force (2018) Screening for osteoporosis to prevent fractures US preventive services task force recommendation statement. JAMA 319:2521–2531
Wuster C, de Terlizzi F, Becker S, Cadossi M, Cadossi R, Muller R (2005) Usefulness of quantitative ultrasound in evaluating structural and mechanical properties of bone: comparison of ultrasound, dual-energy X-ray absorptiometry, micro-computed tomography, and mechanical testing of human phalanges in vitro. Technol Health Care 13:497–510
Knapp KM (2009) Quantitative ultrasound and bone health. Salud Publica Mex 51(suppl 1):S18–S24
Gudmundsdottir SL, Indridason OS, Franzson L, Sigurdsson G (2005) Age-related decline in bone mass measured by dual-energy x-ray absorptiometry and quantitative ultrasound in a population-based sample of both sexes. J Clin Densitom 8:80–86
Ding Z, Chen Y, Xu Y, Zhou X, Xu Y, Ma Z, Sun Y (2018) Impact of age, gender, and body composition on bone quality in an adult population from the middle areas of China. J Clin Densitom 21:83–90
Crogan NL, Alvine C, Pasvogel A (2006) Improving nutrition care for nursing home residents using the INRx process. J Nutr Elder 25:89–103
Suominen MH, Hosia-Randell HM, Muurinen S, Peiponen A, Routasalo P, Soini H, Suur-Uski I, Pitkala KH (2007) Vitamin D and calcium supplementation among aged residents in nursing homes. J Nutr Health Aging 11:433–437
Curtain CM, Williams M, Cousins JM, Peterson GM, Winzenberg T (2016) Vitamin D and calcium supplementation among aged residents in nursing homes. Drugs Aging 33:747–754
Smith RL (2003) Calcium and vitamin D supplementation in nursing home residents. JAMDA 4(suppl):S1–S88
Assantachai P, Angkamat W, Pongpim P, Weattayasuthum C, Komoltri C (2006) Risk factors of osteoporosis in institutionalized older Thai people. Osteoporos Int 17:1096–1102
Dionyssiotis Y, Paspati I, Trovas G, Galanos A, Lyritis GP (2010) Association of physical exercise and calcium intake with bone mass measured by quantitative ultrasound. BMC Women’s Health 10:12
Chandler JM, Zimmerman SI, Girman CJ, Martin AR, Hawkes W, Hebel JR, Sloane PD (2000) Low bone mineral density and risk of fracture in white female nursing home residents. JAMA 284:972–977
Morrison A, Fan T, Sen SS, Weisenfluh L (2013) Epidemiology of falls and osteoporotic fractures: a systematic review. Clinicoecon Outcomes Res 5:9–18
Sun F, Norman IJ, While AE (2013) Physical activity in older people: a systematic review. BMC Public Health 13:449
Satalic Z, Colic Baric I, Cecic I, Keser I (2007) Short food frequency questionnaire can discriminate inadequate and adequate calcium intake in Croatian postmenopausal women. Nutr Res 27:542–547
Kaić-Rak A, Antonic K (1990) Food composition tables. Croatian Institute of Public Health, Zagreb
Kraljevic I, Kastelan D, Kolcic I, Kardum I, Mazalin-Protulipac J, Korsic M (2007) Calcaneal ultrasound parameters in men and women from central Croatia. Med Sci Monit 13:29–33
World Health Organization (1994 ) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. Geneva (WHO Technical Report Series, No. 843)
Hans D, Hartl F, Krieg MA (2003) Device-specific weighted T-score for two quantitative ultrasounds: operational propositions for the management of osteoporosis for 65 years and older women in Switzerland. Osteoporos Int 14:251–258
Firth D (1993) Bias reduction of maximum likelihood estimates. Biometrika 80:27–38
R Core Team (2017 R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Cvijetic S, Pavlovic M, Pasalic D, Dodig S (2011) Ultrasound bone measurement in an older population with metabolic syndrome. Aging Clin Exp Res 23:29–34
Maggi S, Noale M, Giannini S, Adami S, Defeo D, Isaia G, Sinigaglia L, Filipponi P, Crepaldi G, ESOPO Study Group (2005) Quantitative heel ultrasound in a population-based study in Italy and its relationship with fracture history: the ESOPO study. Osteoporos Int 17:237–244
Ou LC, Sun ZJ, Chang YF, Chang CS, Chao TH, Kuo PH, Lin RM, Wu CH (2013) Epidemiological survey of quantitative ultrasound in risk assessment of falls in middle-aged and elderly people. PLoS ONE 8:e71053
de Oliveira PP, Figueiredo Marinheiro IP, Osório Wender MC, Bossoni Mendes J, Oisenberg F (2011) Quantitative ultrasound and risk of fractures in elderly women. Rev Assoc Med Bras 57:637–642
Ekman A, Michaelsson K, Ljunghall S, Mallmin H (2001) Almost all institutionalized women are osteoporotic, when measured by heel and finger ultrasound. J Int Med 249:173–180
Elliott ME, Binkley NC, Carnes M, Zimmerman DR, Petersen K, Knapp K, Behlke JM, Ahmann N, Kieser MA (2003) Fracture risks for women in long-term care: high prevalence of calcaneal osteoporosis and hypovitaminosis D. Pharmacotherapy 23:702–710
Greenspan SL, Myers ER, Kiel DP, Parker RA, Hayes WC, Resnick NM (1998) Fall direction, bone mineral density, and function: risk factors for hip fracture in frail nursing home elderly. Am J Med 104:539–545
Sallin U, Mellström D (2005) Eggertsen R. Osteoporosis in a nursing home, determined by the DEXA technique. Med Sci Monit 11:CR31-70
Hess M, Campagna EJ, Jensen KM (2018) Low bone mineral density risk factors and testing patterns in institutionalized adults with intellectual and developmental disabilities. J Appl Res Intellect Disabil 31(Suppl. 1):157–164
Vive MA, Nahar VK, Ford MA, Bass MA, Johnson AK, Davis AB, Biviji-Sharma R (2015) Risk factors for low bone mineral density in institutionalized individuals with developmental disabilities. Health Promot Perspect 5:147–152
Almeida P, Neves R (2014) Physical activity—the attitude of the institutionalized elderly. JPES 14:12–15
Rydwik E, Kerstin F, Akner G (2005) Physical training in institutionalized elderly people with multiple diagnoses—a controlled pilot study. Arch Gerontol GeriatR 40:29–44
Liubicich ME, Magistro D, Candela F, Rabaglietti E, Ciairano S (2012) PA and mobility function in elderly people living in residential care facilities. “Act on aging”: a pilot study. Adv Phys Educ 2:54–60
Reginster JY, Beaudart C, Buckinxa F, Bruyère O (2016) Osteoporosis and sarcopenia: Two diseases or one? Curr Opin Clin Nutr Metab Care 19:31–36
Santos L, Elliott-Sale KJ, Sale C (2017) Exercise and bone health across the lifespan. Biogerontology 18:931–946
Marques EA, Mota J, Carvalho J (2012) Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. Age(Dordr) 34:1493–1515
McMillan L, Zengin A, Ebeling P, Scott D (2017) Prescribing PA for the prevention and treatment of osteoporosis in older adults. Healthcare 5:E85
Maddalozzo G, Snow C (2000) High intensity resistance training: effects on bone in older men and women. Calcif Tissue Int 66:399–404
Rumbak I, Satalić Z, Keser I, Krbavcić IP, Giljević Z, Zadro Z, Barić IC (2010) Diet quality in elderly nursing home residents evaluated by Diet Quality Index Revised (DQI-R). Coll Antropol 34:577–585
Nguyen TV, Center JR, Eisman JA (2000) Osteoporosis in elderly men and women: effects of dietary calcium, PA, and body mass index. J Bone Min Res 15:322–331
Vannucci L, Masi L, Gronchi G, Fossi C, Carossino AM, Brandi ML (2017) Calcium intake, bone mineral density, and fragility fractures: evidence from an Italian outpatient population. Arch Osteoporos 12:40
Chapuy MC, Pamphile R, Paris E, Kempf C, Schlichting M, Arnaud S, Garnero P, Meunier PJ (2002) Combined calcium and vitamin D3 supplementation in elderly women: confirmation of reversal of secondary hyperparathyroidism and hip fracture risk: the Decalyos II study. Osteoporos Int 13:257–264
Acknowledgements
The authors thank the residents and personnel of the nursing homes: Centar, Ksaver, Maksimir, Park, Sveti Josip and Tresnjevka for their participation, help and support.
Funding
The study was supported by the Institute for Medical Research and Occupational Health (Project “Bone mineral density and fracture risk in older institutionalized people”).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The study was designed in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards and was approved by the Ethics Committee of the Institute of Medical Research and Occupational Health.
Informed consent
Informed consent was obtained from all individuals included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cvijetic, S., Kovacic, J. Association between quantitative bone ultrasound and self-reported physical activity in nursing homes residents. Eur Geriatr Med 10, 659–666 (2019). https://doi.org/10.1007/s41999-019-00183-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-019-00183-3