Abstract
Introduction
There are very few published studies on osteoporosis among the institutionalized elderly in Asian countries, where the incidence of osteoporosis is increasing rapidly. Our objectives were to determine both the prevalence and risk factors of osteoporosis, as assessed by calcaneal bone mineral density (BMD) measurements, in a Thai nursing home.
Methods
Activities of daily living, the Mini-Mental State Examination, blood chemistry, body composition analysis, calcaneal quantitative ultrasound (QUS) and serum C-terminal telopeptides of type I collagen (serum β-CTx) were assessed in 108 older people living in the largest nursing home for the elderly in Bangkok. Calcaneal BMD was measured by dual-energy X-ray absorptiometry (DXA).
Results
The prevalence of osteoporosis, as defined by a calcaneal BMD T-score <1.6, was 79.6%. The prevalence of low bone mass, as defined by a T-score of broadband ultrasound attenuation <1.0, was 80.6%. The prevalence of osteoporosis detected by these two methods was not significantly different (p=1.00). The prevalence of increased bone turnover [with the cutoff point being the mean + 2 standard deviation (SD) of the serum β-CTx level of a sex- and age-matched control group] was 13.9%. In multiple linear regression analysis, five risk factors – serum β-CTx, mental health, mobility index, height and lean body mass – were able to predict calcaneal BMD at a coefficient of determination R2) of 0.54.
Conclusions
These results indicate the importance of mental health and self-care ability as factors associated with osteoporosis. Increased bone turnover was also a significant risk factor of low bone mass. Calcaneal QUS was a useful screening tool for diagnosing osteoporosis in this population and was comparable to calcaneal DXA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of hip fractures is increasing rapidly in developing countries, and it has been predicted that by the year 2050, 51% of all hip fractures in the world will occur in Asia [1]. Although there have been studies investigating the risk factors of osteoporosis among elderly Asian people residing in the community [2, 3], there is a paucity of information on the risk factors of this disease among elderly Asian residents of institutions. In addition, the results of studies on the elderly of Western countries who live in institutionalized settings have been indirectly conflicting in some cases. For example, one study found that cognitive impairment was not strongly associated with low bone mineral density (BMD), while the cognitive scale score was part of a scoring algorithm for identifying those at increased risk for fracture [4, 5]. Consequently, there is a need for obtaining a better understanding of the risk factors of osteoporosis in older Asian people living in nursing homes.
The higher prevalence of osteoporosis in institutionalized older people compared to their counterparts in the community has already been highlighted. The prevalence of the former ranges from 67% by total hip BMD to 85.7% by calcaneal BMD and 95% by calcaneal quantitative ultrasound (QUS) [6–8]. Since the outcome of osteoporosis is fracture, the laboratory diagnosis of osteoporosis may not pose immediate concern to either medical personnel or the older people when the diagnosis is made. Osteoporosis might be overlooked or placed in a lower priority due to the other common, perceivable health problems caused by co-existing degenerative disorders and chronic illnesses. One study found that osteoporosis had been documented in the records of only 17% of those who had calcaneal osteoporosis [9]. Another study revealed that 45.5% of physicians caring for older people in long-term care facilities did not routinely assess their patients for the disease and 26.8% routinely did not treat it [10]. One possibility to remedy this situation is to increase awareness and prevent such a crippling medical condition; therefore, a study revealing not only the extent but also the risk factors of osteoporosis in an institutionalized setting where the disease is commonly found is of utmost importance.
It is not practical to employ central dual-energy x-ray absorptiometry (DXA) for all institutionalized older people since it requires transporting the elderly individual to a radiological facility and a degree of competency and cooperation on the part of this same individual. QUS is an ideal screening tool for osteoporosis and can also predict osteoporosis-related fractures [11, 12]. In addition, the correlation between calcaneal BMD and QUS calcaneal parameters is statistically satisfactory [13]. However, the correlation between calcaneal DXA and calcaneal QUS in elderly residents of an institution is scarcely covered in the literature.
The objectives of this study were, therefore, to determine the extent and risk factors of osteoporosis in institutionalized elderly people. The appropriateness of calcaneal QUS as a practical and safe screening method for osteoporosis was also investigated.
Materials and methods
Setting and subjects
This cross-sectional study was approved by the Faculty of Medicine, Siriraj Hospital, Mahidol University, and the Bangkhae Home for the Aged, Ministry of Social Development and Human Security, Bangkok, Thailand. The admission criteria of this, the largest state-owned nursing home in Bangkok are: those aged 60 years and older, live alone and do not have any relatives or care-giver, and those meeting the age criterium who are homeless. Therefore, the residents are generally younger and healthier than most of those admitted to a nursing home in Western societies. A minority of the residents have the freedom to go outside the nursing home but they must return to it on the same day; otherwise they will be discharged from the nursing home. However, for most of the elderly people the nursing home represents their final residence, consequently, there is a large population of very old residents who tend to suffer from ill health and frailty. All of the residents in the nursing home were eligible for the study. There were three nurses and 28 paramedical personnel routinely caring for the residents. All the candidate-participants and, where available, their relatives were informed of the objectives of the study. The exclusion criteria were those who were unwilling to join the study, unable to give consent, mildly demented without a legal guardian to sign a consent form. Of the 223 residents of the nursing home, 108 were ultimately recruited into the study. The study started in September 2004 and finished in January 2005.
Data collection and measurements
Two of the nursing team (W.A. and P.P.) were responsible for direct interview and completion of the questionnaire. The basic medical data were extracted from the medical records of each subject. Since walking was the only exercise routinely practiced by all residents, the time expending in walking as an exercise was derived from the frequency of this exercise in 1 week multiplied by the walking time on each occasion (minutes per week). All the recruited subjects were also asked to fast for at least 10 h before the biochemical and hematological blood tests, which along with bone marker analysis were carried out in the morning. Quantitative ultrasound and BMD measurement by DXA were sequentially done at the left os calcis.
The Thai Mini-Mental State Examination, a Thai version equivalent to Mini-Mental State Examination, was used to assess mental status [14]; the cutoff point denoting impaired mental status was <24 points [15]. The activities of daily living (ADL) designed by the ‘Survey in Europe on Nutrition and the Elderly, A Concerted Action (SENECA)’ was also used as a diagnostic tool [16]. The ADL consists of 16 items of daily living activities, with each item measured on a 4-point scale, namely, being unable to do the activity completely (4 points); can do it only with help (3 points); can do it with difficulty but without help (2 points); can do it independently without difficulty (1 point). On the basis of the total score obtained from these 16 ADL items, two indices can be derived, i.e., the mobility index (MI) and the self-care index (SI). MI was calculated by summing up the following four items, namely, going outdoors, using stairs, walking at least 400 m and carrying a heavy object for at least 100 m. The possible range of the MI is then 4–16 points. The SI was calculated when the following items were added together: walking between rooms, toilet use, grooming and bathing, dressing, getting in and out of bed, cutting toe-nails and eating. The possible range of the SI is then 7–28 points.
The basic blood tests included the analysis of serum cholesterol, triglyceride, creatinine, glucose and complete blood count. Elecsys β-CrossLaps was used to measure the serum isomerized C-terminal telopeptides of type I collagen (serum β-CTx). An elevated serum level indicates increased bone turnover [17]. All blood tests were carried out around 8–9:00 a.m. and sent to the Department of Clinical Pathology, Siriraj Hospital for laboratory measurement before 10:30 a.m.
Calcaneal DXA was performed by PIXI (GE Lunar Corp., Madison, Wis.) using a cone-beam x-ray and area detector. An aluminum os calcis equivalent phantom was used for daily quality assurance. T-score analysis was based on the Asian ethnic data contained in the manufacturer’s database. The short-term reproducibility of BMD was performed by three consecutive measurements of ten subjects with repositioning of the left foot. The coefficient of variation of BMD was 1.89%. Since the optimal T-score of calcaneal BMD that defines the same prevalence of osteoporosis at any central site is −1.6 [18, 19], this value was adopted for osteoporosis classification in the study. This value is also similar to the manufacturer’s recommendations.
Ultrasonographic measurement of the os calcis was performed using the Achilles Plus system (GE Lunar Corp.), which is a water-based system that uses fluid coupled through transmission in a temperature-controlled water bath (37°C). A quarter wave-matched, broadband single-element transducer technique was used. A single ultrasonometer was used throughout the study, and all measurements were carried out by the same operator (P.A.). Quality assurance with the phantom provided by Lunar was done every day before the tests. The short-term reproducibility of broadband ultrasound attenuation (BUA) was performed by three consecutive measurements of ten subjects with repositioning of left foot. The coefficient of variation was 2.78%. The normative data of BUA in young Thai people were obtained by a survey of young Thai adults. The mean + standard deviations (SD) of BUA of normal young male and female subjects were 118.8+14.3 dB/MHz and 108.2+13.9 dB/MHz, respectively [20]. It has been recommended that subjects with a BUA below the mean −1.0 SD of the young people should receive further investigation for osteoporosis as a fracture risk group [21]. Therefore, the cut-off points of 104.5 and 94.3 dB/MHz were adopted for osteoporosis classification in male and female subjects, respectively.
Body composition analysis was done using the Bioimpedance Analyzer Model 450 apparatus (Biodynamics Corp., Seattle, Wash.). This machine assesses electrical tissue conductivity and is used to analyze the composition of the human body. It provides lean body mass, fat mass and total body water measurements. The subjects were told to lie down, facing upwards, relax and be as still as possible with their hands at least 8 inches from their sides, palms down; their feet were also at least 8 inches apart. The sensor pads were placed on the right wrist and the right ankle before the test.
Statistical analyses
Quantitative data that were and were not normally distributed were expressed as mean values + standard deviation (SD) and median values (minimum, maximum) respectively. The chi-square test was used to test the association between two qualitative variables. The unpaired t-test and Mann-Whitney test were employed to test the difference between two groups with respect to a quantitative variable that was and was not normally distributed, respectively. The Pearson correlation coefficient (r) and Spearman rank correlation (r s ) were used to establish a relationship between two variables that did and did not satisfy normality assumptions, respectively.
To determine the effect of each independent variable on the outcome after controlling for the effect of others, we performed multivariable analysis. Multiple linear regression analysis was employed to determine factors affecting calcaneal BMD assessed by DXA.
To compare the prevalence of low bone mass detected by QUS (defined by a T-score of BUA <1.0) and osteoporosis detected by calcaneal BMD (defined by a T-score of BMD <1.6), McNemar’s test was performed.
The statistical package SPSS for Windows ver. 10.0 (serial number: 3607592; SPSS Inc., Chicago, Ill.) was used to analyze the data. The level of statistical significance was set at 0.05.
Results
Of the 108 elderly participants recruited, 87 were women and 21 were men. The mean ages of the women and men were 78.2±6.9 and 74.7±8.7 years, respectively (range: 61–98 years). The mean duration of admission in the nursing home was 8.7±6.7 years (range: 1–30 years, median: 7 years). The mean body mass indices (BMI) of the women and men were 23.9±5.8 and 22.0±3.3 kg/m2, respectively. Only 6.5% did not have any underlying chronic disease, while up to 50% had three or more chronic medical problems. The most common medical problems were joint pain (49.1%), memory complaint (48.1%), hypertension (39.8%) and diabetes mellitus (13.0%). Anemia was prevalent in 45.3% of the women (hemoglobin <12.0 g/dl) and 23.8% of the men (hemoglobin <13.0 gram/dl). Only 26.9% of all the residents or 26.7% of those who had osteoporosis took calcium tablets on a regular basis.
The prevalence of calcaneal osteoporosis (defined by a T-score of BMD <1.6) was 71.4% (95%CI: 47.8–88.7%) in men and 81.6% (95%CI: 71.9–89.1%) in women, with an overall prevalence of 79.6% (95%CI: 70.8–86.8%). A comparison of the prevalence of osteoporosis identified by QUS and DXA revealed that a 80.6% prevalence was identified by QUS compared to a 79.6% prevalence by calcaneal BMD; there was no statistically significant difference in the prevalence rate detected by the two methods (p=1.00). Of the 108 subjects, both QUS and DXA agreed on an osteoporosis prevalence of 72.2% and a normal bone mass prevalence of 12.0%. Therefore, the concordance between the two methods was 84.2%, with the remaining 15.8% being discordant. However, only calcaneal BMD assessed by DXA was used for subsequent analysis.
On the basis of the Mini-mental state examination, the prevalence of abnormal mental status was 70.4%. Those with impaired mental status did not differ from those with normal mental health with respect to age [mean ± SD: 77.9±7.7 vs. 76.8±6.7; p=0.474], years since admission [median (min, max): 6.5 (1, 30) vs. 11.5 (1, 26); p=0.214] and BMI [median (min, max): 22.8 (12.5, 37.9) vs. 22.3 (17.4, 40.6); p=0.532]. However, those with impaired mental status were more functionally impaired in terms of the MI [median (min, max): 12 (4, 16) vs. 8 (4, 16); p<0.001] and SI [median (min, max): 16 (7, 28) vs. 13.5 (7, 24); p<0.001]. At the same time, those with impaired mental status also differed from those with normal mental health with respect to calcaneal BMD [mean ± SD: 0.26±0.10 vs. 0.35±0.14; p=0.001] and serum β-CTx [median (min, max): 0.55 (0.11, 1.58) vs. 0.35 (0.09, 1.45); p=0.002].
The prevalence of increased bone turnover (defined by mean + 2SD of sex- and age-matched value of serum β-CTx) was 17.2% (95%CI: 10.0–26.8%) in women, while none of the male residents had increased bone turnover. The magnitude of correlation between serum β-CTx and the following variables was quite poor, as expressed by a Spearman rank correlation of less than 0.35: age (r s =0.06, p=0.558), mobility index (r s =0.15, p=0.136) and SI (r s =0.19, p=0.050). However, there was a mild degree of correlation between serum β-CTx and the other two variables, namely, hemoglobin (r s =−0.43, p<0.001) and lean body mass (r s =−0.35, p<0.001).
Although the MI and SI were based on different activities, the magnitude of correlation between the SI and MI was quite high (r s =0.90, p<0.001). Both the MI and SI were also significantly correlated to time expended in walking exercise, with r s values of −0.52 and −0.51, respectively. (p<0.001 for both correlations).
The magnitude of correlation between lean body mass and the other variables was as follows: BMI (r=0.44, p<0.001), age (r=−0.28, p=0.003), hemoglobin (r=0.23, p=0.016), years since admission (r s =−0.22, p=0.021), mobility index (r s =−0.05, p=0.596), SI (r s =−0.09, p=0.382) and walking exercise time (r s =−0.001, p=0.993).
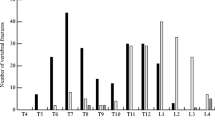
Multiple linear regression was performed to reveal factors determining calcaneal BMD. Backward selection was applied with eight significant independent variables from the univariable analysis (Tables 1, 2): body weight (in kilograms), height (in centimeters), MI (points), SI (points), lean body mass (in kilograms), hemoglobin (in grams per deciliter), serum β-CTx (in micrograms per liter) and mental group (0 = good, 1 = poor). The analysis showed that five variables were significantly associated with BMD: height, lean body mass, MI, mental status and serum β-CTx. The coefficient of determination R2) was 0.535 (Table 3). The unstandardized regression coefficients describing the change in BMD (in grams per square centimeter) for a unit change of each risk factor was 0.003, 0.003, −0.008, −0.037 and −0.122 for height, lean body mass, mobility index, poor mental health and serum β-CTx, respectively. Residual diagnosis showed that the assumptions for regression analysis were satisfied.
Discussion
Low peripheral BMD has been found to be a significant predictor of osteoporotic fracture in nursing home residents [22, 23]. Furthermore, the high degree of correlation shown by BMD values among various skeletal sites has indicated that measuring a single site may be practical in this setting [24]. We therefore selected the measurement of BMD at the left os calcis as our predictor of osteoporotic fracture. Since the prevalence of osteoporosis varies depending on the laboratory technique and the level of T-score used, the prevalence of osteoporosis, as determined by calcaneal BMD measurement, can range from 51% (T-score of <1.6) to 85.7% (T-score of <2.5) [7, 25]. The prevalence of 79.6% from our study is, therefore, comparable to those values previously reported and was much higher than those found in a community setting (around 20%) [26]. A study in a nursing home for older Caucasian people also showed a higher prevalence of osteoporosis than those found for their community-based age-specific counterparts [27]. Because years since admission was not statistically different between those who had and did not have osteoporosis, this might support the hypothesis that a majority of the individuals entering a nursing home were already osteoporotic [28].
Some main risk factors of osteoporotic fractures among the nursing home residents were revealed by two large studies [5, 29]. Cognitive impairment, a risk factor found in both studies, was also an independent factor determining BMD in our results. This indicates the significance of poor mental health on the prevalence of osteoporosis in older Caucasian and Asian residents of nursing homes. Although bone loss was found to predict subsequent cognitive decline in older women, further investigation is needed to determine the mechanisms that link osteoporosis and cognitive decline [30]. Despite the fact that the residents who suffered from cognitive impairment had a poor score for the ADL, MI still existed as an independent determinant of BMD (Table 3), suggesting the significance of poor mobility upon BMD in older people [31]. Additionally, both MI and SI were significantly correlated to each other and to walking exercise time. A more active daily life style would encourage older residents to walk freely indoors, do walking exercise and, hence, enhance BMD.
Height was also an independent factor determining BMD. It was also found to be a factor predicting fracture [5]. This could be explained by the increased likelihood of vertebral fracture leading to a lower height in the diseased cases.
We found serum bone marker to be a significant predictor of BMD. This result is supported by a study showing that circulating parathyroid hormone level is a key determinant of low BMD and osteoporosis in nursing homes [32]. Hyperparathyroidism secondary from hypovitaminosis D is prevalent among elderly residents, and it appears that increased bone turnover is found in those with circulating 25(OH)D levels below 50 nmol/l [9, 28]. In addition, malnutrition is quite common in institutionalized older persons, even in developed countries, where a correlation between nutritional assessment and BUA was found [33]. Therefore, nutritional improvement, especially vitamin D intake, should be of concern to prevent increased bone turnover and osteoporosis in an institutionalized setting.
In an equivalent study in another Asian country, a study in Japan found that serum albumin was a significant predictor of forearm BMD [34]. Our study indirectly showed the same result, thereby suggesting that lean body mass is also a significant predictor of calcaneal BMD. Lean body mass is also significantly correlated to other nutritional indices, namely, body mass index and hemoglobin.
Since osteoporosis is a silent disease and will not be of concern until fracture occurs, this issue may explain the under-diagnosis and under-treatment of the disease in an institutionalized setting [9, 10]. However, the prevalence of low bone mass identified by QUS and of osteoporosis identified by calcaneal DXA were not significantly different (p=1.00), and the agreement between the two methods was 84.2%. Therefore, QUS could be used as a screening tool in an institutionalized setting due to its advantages, i.e., radiation-free, low cost, portability and ease of use.
In conclusion, the older nursing home residents who participated in this study had higher risk of osteoporosis. Disease prevention should start when they first enter the nursing home. This includes early detection, such as by QUS and serum bone marker analysis, and nutritional assessment, especially for low vitamin D and calcium intake as well as protein energy malnutrition. The promotion of good health as the means to delay cognitive impairment and maintain an active lifestyle is also crucially important.
References
Cooper C, Campion G, Melton LJ (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Lau EM, Suriwongpaisal P, Lee JK, Das De S, Festin MR, Saw SM, Khir A, Torralba T, Sham A, Sambrook P (2001) Risk factors for hip fracture in Asian men and women: the Asian osteoporosis study. J Bone Miner Res 16:572–580
Suzuki T (2001) Risk factors for osteoporosis in Asia. J Bone Miner Metab 19:133–141
Zimmerman Itkin S, Hawkes W, Chandler J, Custis Buie V, Hebel JR, Sloanes PD, Martin A, Magaziner J, Holder L, CJ Girman (1999) Correlates of bone mineral density in nursing home residents. J Nutr Health Aging 3:140–145
Girman CJ, Chandler JM, Zimmerman SI, Martin AR, Hawkes W, Hebel JR, Sloane PD, Magaziner J (2002) Prediction of fracture in nursing home residents. J Am Geriatr Soc 50:1341–1347
Greenspan SL, Myers ER, Kiel DP, Parker RA, Hayes WC, Resnick NM (1998) Fall direction, bone mineral density, and function: risk factors for hip fracture in frail nursing home elderly. Am J Med 104:539–545
Sallin U, Mellstrom D, Eggertsen R (2005) Osteoporosis in a nursing home, determined by the DEXA technique. Med Sci Monit 11:67–70
Ekman A, Michaelsson K, Ljunghall S, Mallmin H (2001) Almost all institutionalized women are osteoporotic, when measured by heel and finger ultrasound. J Intern Med 249:173–180
Elliott ME, Binkley NC, Carnes M, Zimmerman DR, Petersen K, Knapp K, Behlke JM, Ahmann N, Kieser MA (2003) Fracture risks for women in long-term care: high prevalence of calcaneal osteoporosis and hypovitaminosis D. Pharmacotherapy 23:702–710
McKercher HG, Crilly RG, Kloseck M (2000) Osteoporosis management in long-term care. Survey of Ontario physicians. Can Fam Physician 46:2228–2235
Bauer DC, Gluer CC, Cauley JA, Vogt TM, Ensrud KE, Genant HK, Black DM (1997) Broadband ultrasound attenuation predicts fractures strongly and independently of densitometry in older women. Arch Intern Med 157:629–634
Hans D, Dargent-Molina P, Schott AM, Sebert JL, Cormier C, Kotzki PO, Delmas PD, Pouilles JM, Breart G, Meunier PJ (1996) Ultrasonographic heel measurements to predict hip fracture in elderly women: the EPIDOS prospective study. Lancet 348:511–514
Langton CM, Langton DK (2000) Comparison of bone mineral density and quantitative ultrasound of the calcaneus: site-matched correlation and discrimination of axial BMD status. Br J Radiol 73:31–35
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Train the brain forum (Thailand) (1993) Thai mental state examination (TMSE). Siriraj Hosp Gaz 45:359–374
Euronut SENECA investigators (1991) Life-style: physical activities and activities of daily living. Eur J Clin Nutr 45[Suppl.3]:139–151
Huber F, Traber L, Roth HJ, Heckel V, Schmidt-Gayk H (2003) Markers of bone resorption-measurement in serum, plasma or urine? Clin Lab 49:203–207
Pearson D, Masud T, Sahota O, Earnshaw S, Hosking D (2003) A comparison of calcaneal dual-energy X-ray absorptiometry and calcaneal ultrasound for predicting the diagnosis of osteoporosis from hip and spine bone densitometry. J Clin Densitom 6:345–352
Faulkner KG (1997) Bone densitometry: choosing the proper skeletal site to measure. J Clin Densitom 1:279–285
Sriussadaporn S, Siritanaratkul N, Ploybutr S, Tanlakij M, Komoltree C, Assantachai P, Leowattana W (2000) Assessment of bone mineral density and factors influencing bone mineral density in Thalassemic diseases in Thailand. Report to the National Research Council of Thailand, Bangkok
Hartl F, Tyndall A, Kraenzlin M, Bachmeier C, Guckel C, Senn U, Hans D, Theiler R (2002) Discriminatory ability of quantitative ultrasound parameters and bone mineral density in a population-based sample of postmenopausal women with vertebral fractures: results of the Basel Osteoporosis Study. J Bone Miner Res 17:321–330
Chandler JM, Zimmerman SI, Girman CJ, Martin AR, Hawkes W, Hebel JR Sloane PD, Holder L, Magaziner J (2000) Low bone mineral density and risk of fracture in white female nursing home residents. JAMA 284:972–977
Broe KE, Hannan MT, Kiely DK, Cali CM, Cupples LA, Kiel DP (2000) Predicting fractures using bone mineral density: a prospective study of long-term care residents. Osteoporos Int 11:765–771
Elliott ME, Drinka PJ, Krause P, Binkley NC, Mahoney JE (2004) Osteoporosis assessment strategies for male nursing home residents. Maturitas 15:225–233
Toofanny N, Maddens ME, Voytas J, Kowalski D (2004) Low bone mass and postfall fracture risk among elderly nursing home men. J Am Med Dir Assoc 5:367–370
Pongchaiyakul C, Kosulwat V, Rojroongwasinkul N, Charoenkiatkul S, Chotmongkol R, Rajatanavin R (2002) Bone mineral density in rural Thai adults living in Khon Kaen province. J Med Assoc Thai 85:235–244
Zimmerman SI, Girman CJ, Buie VC, Chandler J, Hawkes W, Martin A, Holder L, Hebel JR, Sloane PD, Magaziner J (1999) The prevalence of osteoporosis in nursing home residents. Osteoporos Int 9:151–157
Komar L, Nieves J, Cosman F, Rubin A, Shen V, Lindsay R (1993) Calcium homeostasis of an elderly population upon admission to a nursing home. J Am Geriatr Soc 41:1057–1064
Colon-Emeric CS, Biggs DP, Schenck AP, Lyles KW (2003) Risk factors for hip fracture in skilled nursing facilities: who should be evaluated? Osteoporos Int 14:484–489
Lui LY, Stone K, Cauley JA, Hillier T, Yaffe K (2003) Bone loss predicts subsequent cognitive decline in older women: the study of osteoporotic fractures. J Am Geriatr Soc 51:38–43
Ooms ME, Lips P, Van Lingen A, Valkenburg HA (1993) Determinants of bone mineral density and risk factors for osteoporosis in healthy elderly women. J Bone Miner Res 8:669–675
Reginster JY, Deroisy R, Pirenne H, Frederick I, Dewe W, Albert A, Collette J, Zheng SX, Gosset C (1999) High prevalence of low femoral bone mineral density in elderly women living in nursing homes or community-dwelling: a plausible role of increased parathyroid hormone secretion. Osteoporos Int 9:121–128
Gerber V, Krieg MA, Cornuz J, Guigoz Y, Burckhardt P (2003) Nutritional status using the Mini Nutritional Assessment questionnaire and its relationship with bone quality in a population of institutionalized elderly women. J Nutr Health Aging 7:140–145
Nakamura K, Nashimoto M, Matsuyama S, Hatakeyama M, Yamamoto M (2002) Correlates of bone mineral density in elderly women living in nursing homes for the disabled in Japan. Aging Clin Exp Res 14:485–490
Acknowledgements
The authors thank all of the personnel in Bangkhae Home for the Aged who facilitated data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was financially supported by funding from the Faculty of Medicine, Siriraj Hospital, Mahidol University.
Rights and permissions
About this article
Cite this article
Assantachai, P., Angkamat, W., Pongpim, P. et al. Risk factors of osteoporosis in institutionalized older Thai people. Osteoporos Int 17, 1096–1102 (2006). https://doi.org/10.1007/s00198-006-0099-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0099-9