Abstract
Various surgical procedures are used for the management of gingival recession defects. The gold standard approach for gingival recession coverage is the use of autogenous ‘connective tissue grafts (CTG) in combination with a coronally advanced flap. To prevent the complications associated with the use of CTG, several treatment alternatives using soft tissue substitutes are now available for the coverage of gingival recession defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Quick reference/description
Various surgical procedures are used for the management of gingival recession defects. The gold standard approach for gingival recession coverage is the use of autogenous connective tissue grafts (CTG) in combination with a coronally advanced flap (CAF). To prevent the complications associated with the use of CTG, several treatment alternatives using soft tissue substitutes are now available for the coverage of gingival recession defects.
Overview
Soft tissue substitutes | Indications | Applications |
|---|---|---|
Barrier membranes (Guided tissue regeneration) | Single gingival recession defects | To avoid morbidity associated with a second surgical site |
To facilitate regeneration of periodontal tissues on the previously exposed root surfaces | ||
Enamel matrix derivative | Single and multiple gingival recession defects | As a substitute for CTG in root coverage procedures |
To enhance periodontal regeneration on the previously exposed root surfaces | ||
Collagen matrices | ||
Acellular dermal matrices | Coverage of single and multiple gingival recession defects | As a substitute for palatal donor tissue to eliminate the disadvantages associated with autogenous grafts |
Xenogeneic collagen matrices | Coverage of single and multiple gingival recession defects | As an alternative to autogenous tissue and acellular dermal matrices in recession coverage procedures |
Materials/instruments
-
Resorbable membranes
-
Non-resorbable membranes
-
Enamel matrix derivative
-
Acellular dermal matrices (AlloDerm®, Puros® Dermis, PerioDerm™, and Epiflex®)
-
Xenogeneic collagen matrices (Mucoderm®, Mucograft®, Osteobiol® Derma, MucoMatrixX®, and DynaMatrix®)
Procedure
Several surgical treatment approaches have been proposed for the management of gingival recession defects. The gold standard procedure for gingival recession coverage is the use of autogenous CTG along with a CAF. Various soft tissue substitutes are now available for the coverage of gingival recession defects to prevent the complications associated with the use of CTG.
To prevent the morbidity associated with a second surgical site as observed with the use of CTG, the CAF procedure alone is considered simple to perform and effective in achieving recession coverage. However, the CAF alone approach is associated with an apical relapse of the gingival margin corresponding to an inadequate amount and thickness of keratinized tissue in the long term. Therefore, other approaches including the use of various soft tissue substitutes are aimed at substituting the use of CTG and improving the outcome of the CAF procedure.
Barrier membranes
An alternative approach for the coverage of gingival recession defects is guided tissue regeneration (GTR) using resorbable and non-resorbable barrier membranes. The rationale of GTR is to circumvent the creation of a second surgical site and to enhance periodontal regeneration on the previously exposed root surface. Periodontal regeneration with the formation of new alveolar bone, periodontal ligament and cementum is observed when barrier membranes are used in combination with a CAF procedure. The GTR technique has good predictability regarding clinical attachment gain and root coverage.
The GTR technique is associated with several disadvantages limiting its clinical benefits as compared to other root coverage treatment modalities. Therefore, GTR-based root coverage procedures are not recommended for routine use.
Enamel matrix derivative
Another treatment alternative for substituting CTG in root coverage procedures is the use of enamel matrix derivative (EMD). EMD can effectively facilitate regeneration of the periodontal tissues on previously exposed root surfaces. The use of EMD in conjunction with CAF is considered safe and has superior results than the use of CAF alone in terms of keratinized tissue gain, recession reduction and complete root coverage (Fig. 1).
Use of EMD and collagen matrix in conjunction with CAF for root coverage procedures. a Multiple gingival recessions affecting the maxillary left anterior area. b Flap elevation using a split-full-split approach with a short vertical incision distal to the canine. c Application of EMD on the root surface. d Collagen matrix was rehydrated in sterile saline and sutured in place. e Flap coronally advanced and fixed with 6/0 polypropylene sutures to cover the entire collagen matrix. f Clinical outcome 3 months after surgery. g Clinical outcome 9 months after surgery. h Clinical outcome 2 years after surgery (reproduced from Kasaj A, Quintessence Int 2016;47:775–783, courtesy Quintessence Publishing)
The main advantages of the combined use of EMD and CAF are:
Simplicity of the procedure
Avoidance of a second surgical site
Improved early healing
Less postoperative discomfort
As the combination of EMD and CAF has the ability to improve clinical outcomes and promote periodontal regeneration, EMD is a safe substitute for autogenous grafts in root coverage procedures.
Soft tissue graft substitutes
Acellular dermal matrices
Acellular dermal matrices (ADM) can be used as a substitute for autogenous CTG in periodontal plastic surgery to overcome the disadvantages associated with autogenous tissue harvesting. The ADM allograft is obtained from donated human skin. It is treated to remove all viable cells that can be responsible for developing an inflammatory or immunogenic response. The residual connective tissue matrix imparts a collagen structure that acts as a scaffold for ingrowth and subsequent replacement by host tissues.
The advantages of the use of ADM grafts in root coverage procedures are:
Avoidance of palatal tissue harvesting
Decreased morbidity as compared to autogenous grafts
Unlimited tissue availability
Decreased surgery time
Increased patient treatment acceptance
Although the use of ADM is beneficial for the clinician and the patient, its use in root coverage procedures is more complicated than autogenous graft. ADM is an avascular and acellular material, and its function depends on the revascularization and nutrition received from the recipient site. Therefore, full coverage of the ADM by the overlying flap in a tensionless approach is mandatory, predominantly in regions of high muscle activity. Due to the specific properties of healing associated with ADM use, the predictability, efficacy and outcome of ADM are closely related to the implemented surgical technique. Several surgical techniques have been proposed for using ADM in root coverage procedures.
The selection of an appropriate surgical technique for the use of ADM should be aimed at preserving the vascular supply of the overlying flap to allow adequate revascularization and nutrition of the graft material. Commonly, using a flap technique with vertical releasing incisions facilitates good control over the procedure because of improved visibility and easier repositioning of the flap as compared to more technique-sensitive approaches like the tunnel technique.
The use of ADM in recession coverage procedures is associated with less keratinized tissue formation than autogenous grafts. Another matter of concern associated with ADM use is the variability in long-term stability of clinical outcomes. In conclusion, the use of ADM in root coverage procedures is a safe and patient-friendly treatment alternative to autogenous CTG. ADM is commercially available as AlloDerm® (BioHorizons), Puros® Dermis (Zimmer Biomet), PerioDerm™ (Dentsply), and Epiflex® (DIZG).
Xenogeneic collagen matrices
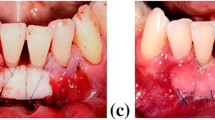
Xenogeneic collagen matrices can be used as an alternative to autogenous donor tissue and ADM in root coverage procedures (Fig. 2). The collagen matrices are of porcine origin. After procurement of porcine dermal tissue, all the antigenic cellular components are removed by processing, while the structure of the source tissue is preserved. Porcine dermal tissue as a source of the collagen matrices is favorable as it is structurally and immunologically similar to human dermal tissue and can reduce some disadvantages associated with the use of human cadaver-derived ADM.
Use of xenogeneic collagen matrix in conjunction with CAF for root coverage procedures. a Multiple gingival recessions affecing the maxillary right quadrant. b Flap elevation using a split-full-split approach without vertical releasing incisions. c Collagen matrix was rehydrated in sterile saline and sutured in place. d Flap coronally advanced and sutured with polypropylene 6/0 to cover the entire collagen matrix. e Clinical outcome 3 months after surgery. f Clinical outcome 18 months after surgery
The rationale of using porcine collagen matrices is that it can act as a temporary 3D scaffold and allow host cell infiltration and tissue ingrowth without eliciting an immunogenic or foreign body response (Figs. 3, 4). Porcine-derived collagen matrices are commercial available as Mucoderm® (Botiss biomaterials), Mucograft® (Geistlich), Osteobiol® Derma (Tecnoss), MucoMatrixX® (Dentegris), and DynaMatrix® (Keystone).
Use of EMD and xenogeneic collagen matrix in conjunction with CAF for root coverage procedures using the tunneling technique. a Preoperative gingival recession on a mandibular left lateral incisor. b Tunnel flap preparation and adjustment of dimensions of the collagen matrix. c Application of EMD on the root surface. d Placement of the rehydrated collagen matrix into the prepared tunnel. e Flap coronally advanced and sutured with polypropylene 6/0. f Clinical outcome 3 months after surgery
Use of EMD and xenogeneic collagen matrix in conjunction with CAF for root coverage procedures. a Gingival recession affecting the maxillary right canine. b Flap elevation using a split-full-split approach and deepithelialization of the anatomical papillae. c Application of EMD on the root surface. d Collagen matrix rehydrated in sterile saline and sutured in place. e Flap coronally advanced and fixed with polypropylene sutures 6/0 to cover the entire collagen matrix. f Clinical outcome 2 years after surgery
Postoperative instructions
Postoperative instructions include the following:
- 1.
Avoid mechanical manipulation of the surgical area (no brushing, no flossing).
- 2.
Maintenance of normal oral hygiene measures in areas not affected by the surgical procedure.
- 3.
Use of 0.12% chlorhexidine mouthrinse twice a day for 2 weeks.
- 4.
Pain control with 600 mg ibuprofen directly after surgery; additional use only if required.
Pitfalls and complications
Soft tissue substitutes are associated with inferior clinical outcomes than connective tissue grafts.
The drawbacks of using connective tissue grafts for recession coverage are:
Requirement of a second surgical procedure for graft harvesting leading to potential donor site morbidity
Increased operative time
Limited availability of donor tissue
The drawbacks and complications of GTR are:
Frequent membrane exposure resulting in a risk of site contamination, infection and procedure failure
Requirement of a second surgical procedure for membrane retrieval, if non-resorbable membranes are used, causing iatrogenic trauma to the regenerating tissue
Use of barrier membranes for recession coverage is associated with a limited ability in increasing thickness of gingival tissue
Use of collagen matrices is a technique-sensitive procedure as flap shrinkage leading to graft exposure during healing can impede graft material revascularization resulting in graft disintegration.
Collagen matrices compared to autogenous grafts are associated with a longer healing period as non-vital materials require additional time for resorption and substitution by host tissue.
The more widespread use of ADM in root coverage procedures can be limited due to ethical concerns and the possible risk of disease transmission as ADM is a human-derived material.
Further Reading
Kasaj A (ed) Gingival recession management. Recession coverage using soft tissue substitutes. https://doi.org/10.1007/978-3-319-70719-8_9
Tatakis DN, Chambrone L, Allen EP, Langer B, McGuire MK, Richardson CR, Zabalegui I, Zadeh HH (2015) Periodontal soft tissue root coverage procedures: a consensus report from the AAP regeneration workshop. J Periodontol 86:S52–S55
Chambrone L, Tatakis DN (2015) Periodontal soft tissue root coverage procedures: a systematic review from the AAP regeneration workshop. J Periodontol 86:S8–S51
Ozenci I, Ipci SD, Cakar G, Yilmaz S (2015) Tunnel technique versus coronally advanced flap with acellular dermal matrix graft in the treatment of multiple gingival recessions. J Clin Periodontol 42:1135–1142
Kasaj A (2016) Gingival recession coverage: do we still need autogenous grafts? Quintessence Int 47:775–783
Atieh MA, Alsabeeha N, Tawse-Smith A, Payne AG (2016) Xenogeneic collagen matrix for periodontal plastic surgery procedures: a systematic review and meta-analysis. J Periodontal Res 51:438–452
McGuire MK, Scheyer ET (2016) Long-term results comparing xenogeneic collagen matrix and autogenous connective tissue grafts with coronally advanced flaps for treatment of dehiscence-type recession defects. J Periodontol 87:221–227
Zucchelli G, Mounssif I (2000) Periodontal plastic surgery. Periodontol 2015(68):333–368
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kasaj, A. Gingival recession coverage using soft tissue substitutes. Clin Dent Rev 3, 23 (2019). https://doi.org/10.1007/s41894-019-0062-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41894-019-0062-8