Abstract
Aim
To evaluate the role of serum HE4 in predicting surgical outcome and platinum response in advanced stage EOC patients and to compare the results with those found for CA125 and radiological response.
Methods
Patients with stage III/IV EOC planned for IDS after 3–4 cycles of NACT between May 1, 2017 and April 31, 2019 were included in the study. Pre-chemotherapy and pre-IDS CA125, HE4 and CT response were used to calculate accuracy, sensitivity, specificity, PPV, and negative predictive value for optimal cytoreduction. Nonparametric receiver operating characteristic analyses were performed to determine the optimal threshold of HE4 levels and CA125 levels for predicting optimal surgery. p-value of < 0.05 was considered statistically significant.
Results
82 women were enrolled and 65 of them (79.3%) had optimal interval debulking surgery. Serum CA125 and HE4 values used together correlated with surgical outcome and achieved higher sensitivity (90.7%) in predicting optimal cytoreduction than either of them alone. The best factor in predicting cytoreduction was the combination of CA125 ≤ 63.94 UI/ml, HE4 ≤ 97.82 pmol/L and CT response, with a sensitivity of 93.85%
Conclusion
Serum HE4 had comparable performance with CA125 as a prognostic marker for predicting surgical outcome after NACT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Epithelial ovarian cancer (EOC) is the leading cause of death among women with gynecological cancers (1). Primary debulking surgery (PDS) followed by adjuvant platinum-based chemotherapy has been considered the standard of care for advanced ovarian cancer, and the complete tumor removal with no gross residual disease (NGR) and platinum response are the most important prognostic factors for overall survival in EOC(2, 3).
Among tumor markers for EOC, cancer antigen 125 (CA125) is commonly used to predict optimal debulking and evaluate platinum sensitivity and monitor disease after treatment (4, 5). Human epididymis protein 4 (HE4) has recently emerged as a valuable biomarker for EOC (6). Serum HE4 is more specific than CA125 in discriminating benign ovarian tumours from malignant ones and its expression is independent of CA125 (7, 8). Serum HE4 may also be important for evaluating treatment response, predicting optimal cytoreduction and monitoring patients with ovarian cancer (8).
Upfront cytoreductive surgery may not always be feasible in advanced EOCs and neoadjuvant chemotherapy (NACT) followed by surgery is an alternative option in them (9,10,11). At present, there is no reliable clinical strategy to predict the possibility of achieving a total resection and determining tumor response to NACT in EOC. Few studies have attempted to use preoperative computed tomography (CT) and CA125 levels for the same with a low sensitivity and low positive predictive value (PPV) (12). Preoperative HE4 profile may also play a role in the same. Vallius et al. were the first to compare the HE4 profile to CA125 and radiologic response as predictors of optimal debulking surgery after NACT and also evaluated HE4 values as a prognostic factor in terms of progression-free interval and overall survival (OS) (12).
In this study, we aimed to evaluate the role of serum HE4 in predicting surgical outcome and platinum response in advanced stage EOC patients and to compare the results with those found for CA125 and radiological response.
Material and Methods
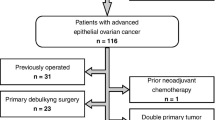
All patients admitted in the department of gynecologic oncology at our institute with histologically confirmed diagnosis of stage III/IV EOC and having received 3–4 cycles of NACT before getting operated between May 1, 2017 and April 31, 2019 were included in the study. NACT followed by IDS was the preferred option when the extent/localization of the disease would likely preclude optimal cytoreduction and/ or the patient would not tolerate extensive surgery due to age and/or comorbidities. Optimal debulking surgery was defined as no visible residual tumor after cytoreduction. The study protocol was approved by internal review board. All these patients received 3–4 cycles of NACT every 3 weeks according to the scheme carboplatin and paclitaxel. Institute review board (IRB) approval was taken for the study.
All patients had preoperative computed tomography (CT) of the chest, abdomen and pelvis with intravenous contrast at the time of diagnosis and before IDS at our center. Results of the CT imaging were interpreted and compared. Evaluation of response took into account RECIST 1.1 criteria (12). Complete response was defined as the disappearance of all target lesions. Partial response (PR) was defined as at least a 30% decrease in the sum of diameters of target lesions, and stable disease is indicated by neither sufficient shrinkage to qualify for PR nor sufficient increase to qualify for progressive disease (12). A CT score of ‘0’ was given to stable disease or PR and a score of ‘1’ to a significant reduction in the CT findings or no or only minimal presence of ascitic fluid (less stringent than complete response according to RECIST). Patients with progressive disease after NACT were not included in the study.
All patients had serum CA125 and HE4 collected at diagnosis, i.e., before first chemotherapy cycle, and before debulking surgery. The intent of surgery was tumor debulking to no macroscopic residual disease. The measurement of serum CA125 was made with the standard radioimmunoassay (normal limit, < 35 IU/mL) during the entire study period. HE4 levels were determined using the HE4 EIA assay. The HE4 EIA is a solid phase, non-competitive immunoassay based upon the direct ‘sandwich’ technique using 2 monoclonal antibodies, 2H5 and 3D8, directed against 2 epitopes in the C-WFDC domain of HE4 (12).
All data were entered in a Microsoft Excel spreadsheet and analyzed using a mathematical model to produce receiver operating characteristic (ROC) curves using MedCalc statistical software ver.19.0.7. Standard mathematic formulas were used to calculate accuracy, sensitivity, specificity, PPV, and negative predictive value (NPV) of CA125, HE4, and CT response alone and in combination. Nonparametric receiver operating characteristic (ROC) analyses were performed to determine the optimal threshold of HE4 levels and CA125 levels for predicting optimal surgery. To calculate the misclassification error rates, we defined the best predictor using the Youden point on the ROC curve. The Youden index (YI) is defined as the maximum (sensitivity (YP) + specificity (YP) – 1) that occurs at the optimum threshold, the Youden point (YP) (12). The diagnostic accuracy of the test was measured by the area under the curve (AUC). The bootstrap method was used to calculate 95% confidence intervals. For all statistical comparisons, a p-value of < 0.05 was considered statistically significant (Table 1).
Results
A total of 82 women were enrolled in the study period of two years. The mean age of the women was 51.44 years (range 29–78 years). Most of these women had serous ovarian cancer (79 women—96.3%). Majority of them were poorly differentiated serous cancers (55 women—67.1%). After three-four cycles of NACT, all these patients underwent surgery and 65 of these 82 women (79.3%) had optimal surgery after interval debulking surgery (IDS). Reasons for suboptimal debulking included presence of multiple serosal deposits over small bowel (7), excessive disease burden over visceral peritoneum (5), disease at porta hepatis with retroperitoneal nodes (1) and excessive overall tumor burden (4).
A categorization of these women based on surgical outcomes–group A (optimal debulking to no gross residual disease) and group B (suboptimal debulking) was done. The mean tumor marker values pre NACT and pre surgery are listed in Table 2.
A pre-IDS CA125 value of 63.94 U/L was considered to be an optimal cutoff value with a sensitivity of 86.15%, a specificity of 64.71%, and an AUC of 0.715 in identifying patients who would attain an optimal debulking (p value 0.0136). The AUC for predicting residual disease based on preoperative HE4 values was 0.720 with a cutoff value at 97.82 pmol/L and sensitivity of 73.85% (p value 0.0036). The difference of AUC between HE4 and CA125 (0.715 vs. 0.720) indicated that HE4 was not a better biomarker to predict surgical outcome of IDS (p value 0.9444). The combination of CA125, HE4, and CT imaging resulted in the best combination to predict optimal debulking surgery with a sensitivity of 93.85% and a specificity of 52.94%.
Discussion
Ovarian cancers are usually diagnosed at an advanced stage and upfront surgical debulking is not always possible especially in women with extensive disease and multiple comorbidities (13). NACT appears to be a valuable option for these patients to avoid extensive perioperative morbidity and delay of adjuvant chemotherapy (9,10,11). Selection of patients for surgery after NACT is crucial, since patients who can be cytoreduced to no macroscopic residual disease may be the only ones gaining a survival benefit from surgery at IDS. Despite several studies focusing on these predictors over the two decades, till now no accurate or reliable preoperative predictors or parameters have been established that may help predict the surgical outcome (12, 14).
Several studies have evaluated the role of CA125 in predicting cytoreduction in ovarian cancers and have suggested that higher CA125 values may suggest larger tumor burden (12, 14). For patients receiving NACT, different cutoffs have been published, ranging from 20 to 100 UI/ml (15). However, the utility of a single tumor marker in predicting optimal cytoreduction is not accurate and should be used keeping in context the other preoperative features. Our results indicate that a pre-IDS CA125 level of 63.94 IU/ml could help identify patients in whom optimal cytoreduction will be achieved with a high sensitivity of 86.15%. Plotti et al. did a similar type of study and found that CA 125 cutoff of 89 U/ml had a sensitivity of 70% (16). However, CA125 is not expressed in all women, and its levels are also correlated with peritoneal inflammation. Therefore, studies are now exploring the additional role of HE4 during NACT in a primarily inoperable ovarian cancer patient cohort (16, 17).
Preoperative HE4 value of 97.82 pmol/L was found to be an optimal cutoff for predicting surgical outcome in our study. Plotti et al. observed that an HE4 value of 226 pmol/L after NACT might be an optimal cutoff value in identifying patients who would not benefit from IDS (16). Shen et al. (154.3 pmol/L), Pelissier et al. (115 pmol/L) and Chudecha-Glaz et al. (218.43 poml/L) presented HE4 cutoff values that were different from ours (18, 19). At the same time, they showed that HE4 is a better predictor than CA125 of the feasibility of optimal cytoreduction. However, in our study, HE4 and CA125 showed similar performance in predicting surgical cytoreduction. Both CA125 and HE4 values had a high negative predictive value which represents a very important clinical parameter and represents the proportion of patients who may be unresectable and may achieve suboptimal cytoreduction. Identifying such cases may help avoid unnecessary negative laparotomies. Imaging studies like CT scan may be used to determine whether a tumor can be completely resected after NACT; however, they have a poor sensitivity in detecting peritoneal metastases of 1 cm or smaller in maximum diameter. A very poor sensitivity of 43.08% for CT response in predicting surgical outcome was found in our study (Table 3).
In our study, CA125 and HE4 values used together correlated with surgical outcome and achieved higher sensitivity (90.7%) in predicting optimal cytoreduction than either of them alone. Angioli et al. showed similar results with a sensitivity of 88.8% and specificity of 89.5% (PPV = 94% and NPV = 80%) for the combination CA125 and HE4 (20). However, the best factor in predicting cytoreduction was the combination of CA125 ≤ 63.94 UI/ml, HE4 ≤ 97.82 pmol/L and CT response, which had a sensitivity of 93.85%. Similar results were observed in a study by Plotti et al. with a high sensitivity of 96% (16). Till now, there is no predefined HE4 cutoff for predicting surgical outcome after NACT. For this reason, in this study, we calculated new CA125 and HE4 cutoff values to improve sensitivity and specificity and used them to establish the best association for pre-IDS evaluation of residual tumor burden.
This study, such as most of the studies on ovarian cancer surgery, could have bias due to the individual experience and different skills of different surgeons. The decision of pursuing surgical treatment can not only be based on laboratory results but a combined approach which also includes physical examination, imaging and general conditions of patients. Surely, the usage of HE4, in addition to CA125 and CT scan, creates a new combination that is able to better predict the residual tumor after debulking surgery, thus providing more accurate information on the prognosis of patients.
Conclusion
Serum HE4 had comparable performance with CA125 as a prognostic marker for predicting surgical outcome after NACT. Based on our results and the literature, the introduction of HE4, alone or combined with CA125 and CT response as a new tool for predicting interval optimal cytoreduction is promising and should be investigated further.
References
Reid BM, Permuth JB, Sellers TA. Epidemiology of ovarian cancer: a review. Cancer Biol Med. 2017;14(1):9.
Chi DS, Eisenhauer EL, Lang J, Huh J, Haddad L, Abu-Rustum NR, et al. What is the optimal goal of primary cytoreductive surgery for bulky stage IIIC epithelial ovarian carcinoma (EOC). Gynecol Oncol. 2006;103(2):559–64.
Chang SJ, Bristow RE, Chi DS, Cliby WA. Role of aggressive surgical cytoreduction in advanced ovarian cancer. J Gynecol Oncol. 2015;26(4):336–42.
Gupta D, Lis CG. Role of CA125 in predicting ovarian cancer survival - a review of the epidemiological literature. J Ovarian Res. 2009;2(1):13.
Charkhchi P, Cybulski C, Gronwald J, Wong FO, Narod SA, Akbari MR. CA125 and ovarian cancer: a comprehensive review. Cancers (Basel). 2020;12(12):1–29.
Fujiwara H, Suzuki M, Takeshima N, Takizawa K, Kimura E, Nakanishi T, et al. Evaluation of human epididymis protein 4 (HE4) and risk of ovarian malignancy algorithm (ROMA) as diagnostic tools of type I and type II epithelial ovarian cancer in Japanese women. Tumour Biol. 2015;36(2):1045.
Dochez V, Caillon H, Vaucel E, Dimet J, Winer N, Ducarme G. Biomarkers and algorithms for diagnosis of ovarian cancer: CA125, HE4, RMI and ROMA, a review. J Ovarian Res. 2019;12(1):1–9.
Pelissier A, Roulot A, Guéry B, Bonneau C, Bellet D, Rouzier R. Serum CA125 and HE4 levels as predictors for optimal interval surgery and platinum sensitivity after neoadjuvant platinum-based chemotherapy in patients with advanced epithelial ovarian cancer. J Ovarian Res. 2016;9(1):1–6.
Kehoe S, Hook J, Nankivell M, Jayson GC, Kitchener H, Lopes T, et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. Lancet. 2015;386(9990):249–57.
Feng Z, Wen H, Li R, Liu S, Fu Y, Chen X, et al. Comparison of survival between primary debulking surgery versus neoadjuvant chemotherapy for ovarian cancers in a personalized treatment cohort. Front Oncol. 2021;10(10):3352.
Vergote I, Amant F, Kristensen G, Ehlen T, Reed NS, Casado A. Primary surgery or neoadjuvant chemotherapy followed by interval debulking surgery in advanced ovarian cancer. Eur J Cancer. 2011;47:S88–92.
Rema P, John ER, Samabasivan S, Prahladan A, George P, Ranjith JS, et al. Evaluation of computed tomography scan and CA 125 response in predicting operability in advanced ovarian cancer and assessing survival outcome in interval cytoreductive surgery. Indian J Surg Oncol. 2019;10(3):426–34.
Schorge JO, Mccann C, Del CMG. Surgical debulking of ovarian cancer: what difference does it make? Rev Obs Gynecol. 2010;3(3):111–7.
Vallius T, Hynninen J, Auranen A, Carpén O, Matomäki J, Oksa S, Grénman S. Serum HE4 and CA125 as predictors of response and outcome during neoadjuvant chemotherapy of advanced high-grade serous ovarian cancer. Tumor Biology. 2014;35:12389–95.
Merlo S, Besic N, Drmota E, Kovacevic N. Preoperative serum CA-125 level as a predictor for the extent of cytoreduction in patients with advanced stage epithelial ovarian cancer. Radiol Oncol. 2021;55(3):341.
Plotti F, Scaletta G, Capriglione S, Montera R, Luvero D, Lopez S, et al. The role of HE4, a novel biomarker, in predicting optimal cytoreduction after neoadjuvant chemotherapy in advanced ovarian cancer. Int J Gynecol Cancer. 2017;27(4):696–702.
Pelissier A, Roulot A, Guéry B, Bonneau C, Bellet D, Rouzier R. Serum CA125 and HE4 levels as predictors for optimal interval surgery and platinum sensitivity after neoadjuvant platinum-based chemotherapy in patients with advanced epithelial ovarian cancer. J Ovarian Res. 2016;9(1):16–21.
Chudecka-Głaz A, Cymbaluk-Płoska A, Wȩaowska M, Menkiszak J. Could HE4 level measurements during firstline chemotherapy predict response to treatment among ovarian cancer patients? PLoS ONE. 2018;13(3):1–16.
Shen Y, Li L. Serum HE4 superior to CA125 in predicting poorer surgical outcome of epithelial ovarian cancer. Tumor Biol. 2016;37(11):14765–72.
Angioli R, Plotti F, Capriglione S, Aloisi A, Montera R, Luvero D, et al. Can the preoperative HE4 level predict optimal cytoreduction in patients with advanced ovarian carcinoma? Gynecol Oncol. 2013;128(3):579–83.
Acknowledgements
NIL
Funding
No funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Poddar, P., Patel, S. & Arora, R. Role of Serum CA125 and HE4 in Predicting Optimal Cytoreduction in Advanced Epithelial Ovarian Cancer After Neoadjuvant Chemotherapy. Indian J Gynecol Oncolog 21, 68 (2023). https://doi.org/10.1007/s40944-023-00750-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-023-00750-4