Abstract
Laparoscopic radical hysterectomy (LRH) is being performed for cervical cancer treatment in many centres worldwide for last three decades. Since the results of LACC trial came out, a number of centres are reverting back to conventional open radical hysterectomy. In this study, we compared the surgical and oncological outcomes of LRH and ORH performed in our centre.
Patients and methods
This is a retrospective study in which we included 171 cancer cervix patients who underwent LRH or ORH in our centre from December 2012 to march 2018. We included FIGO (2009 edition) stages IB1 to IIB cervical cancer. Patients with stages IB2, IIA2 and IIB received neo-adjuvant therapy with either chemotherapy alone or concurrent chemoradiotherapy. Their demography, surgical morbidity, recurrence and survival data were collected and analysed. The survival data for patients who had upfront surgery and those with surgery after neo-adjuvant therapy were compared separately.
Results
There was significant difference between the two arms only in the estimated blood loss during surgery (p = 0.03). The duration of surgery, post-operative length of hospital stay and lymph node harvest were similar between LRH and ORH. The incidence of intraoperative bladder injuries (p = 0.1) and post-operative vesico-vaginal and uretero-vaginal fistulas were higher (p = 0.3) in LRH; there was no statistical significance. There was a non-significant increase in the post-operative bladder dysfunction rates in the LRH arm. The progression-free survival and overall survival were similar (both in upfront surgery and surgery after neo-adjuvant therapy) for LRH and ORH.
Conclusion
Our results are analogous to some of the previous retrospective studies showing comparable oncological outcomes of LRH to conventional open surgery. LRH confers the benefits of less blood loss, early recovery and shorter hospital stay. Further randomised trials with modifications in techniques are needed, and minimally invasive surgery should prosper.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer of the cervix stands as fourth most common cancer among women worldwide, and the incidence is much higher in developing countries with lesser Human Development Index (HDI) [1]. In India, it is the second most common cancer and second common cause of cancer death among women, with 96,922 new cases and 60,078 deaths in 2018 [3]. Of the total cancer cervix deaths in the world, India accounts for 15.2% [3]. Though the incidence of cervical cancer has decreased in the urban areas, it is still high in rural areas [4]. This can be attributed to poor hygienic conditions, early age at marriage and multiple pregnancies in the socio-economically weak population [5]. Further, lesser access to medical facilities and awareness programmes leads to higher incidence and presentation at later stages in majority [6].
For cervical cancer stages IB1 and IIA1, radical hysterectomy with pelvic lymph node dissection is the preferred treatment; however, concurrent chemoradiation (CRT) can also be given [7]. For bulky stage I (IB2), stage IIA2 and IIB concurrent CRT is the treatment of choice [8]. Brachytherapy is an integral part of definitive CRT for locally advanced cervical cancer, which is not available in most parts of developing countries such as India. Hence, many researchers have used multimodality treatment protocols using neo-adjuvant chemotherapy and CRT along with surgery and showed good oncologic outcomes, as achieved with definitive concurrent CRT [9, 10]. Neo-adjuvant therapy helps to downsize the tumour and make the tumour operable, with the additional benefits of treating micro-metastatic disease and reducing the risk of distant failure [11].
Having achieved good survival outcomes with the current treatment strategies, there is an enthusiasm to adopt novel surgical techniques into cancer treatment to reduce the morbidity of open surgery. Minimally invasive surgical techniques have been proven to reduce post-operative morbidity including wound complications, reduce major cardiovascular and pulmonary complications, reduce the length of hospital stay, help early recovery and more cost effective [12, 13]. Many retrospective studies have compared the laparoscopic and open approaches for radical hysterectomy and found that laparoscopic surgery was as good as open technique in terms of oncological outcomes and survival [13,14,15]. But the unexpected results of the laparoscopic approach to carcinoma of the cervix (LACC) trial [16], which is the only randomised control trial till date comparing the two approaches, proving that minimally invasive surgery had significantly higher recurrence rates and poor survival compared to open surgery, is a major setback in taking forward minimally invasive surgery for the treatment of cervical cancer.
Almost all radical hysterectomies are done laparoscopically in our centre for the past 5 years. We analysed the morbidity, oncological and survival outcomes of this technique with the standard open surgery done previously in our centre.
Patients and Methods
This is a retrospective study in which we included all cancer cervix patients who underwent surgery either laparoscopic or open Querleu-Morrow type C1 radical hysterectomy [17], from December 2012 to March 2018 in our centre. Pre-operative chemotherapy and radiation therapy (RT) were given to patients presenting with FIGO stage IB2, IIA2 and IIB as a part of clinical trial conducted in our centre. These patients were also included in this study, and separate comparisons of survival and oncological outcomes for different stages were done. The patients’ characteristics including age, stage of disease, pre-operative therapy, type and duration of surgery, intra-operative blood loss, complications, post-operative histopathology reports, morbidity, survival and recurrence data were collected from the cancer department master case-sheets, operative records, pathology registers and follow-up records. We defined the overall survival from the date of surgery to the last follow-up or death due to cancer cervix.
Inclusion Criteria
Patients with biopsy confirmed cancer of the cervix with histologies including squamous, adenosquamous and adenocarcinoma. FIGO staging (2009 edition) was used and stages IB1, IB2, IIA1, IIA2 and IIB were included. All patients had ECOG performance status ≤ 2 with age between 18 and 70 years.
Exclusion Criteria
Patients treated for some other malignancy previously or with synchronous second malignancy. Recurrent disease after definitive chemoradiation (CRT).
The patients were evaluated routinely with computed tomography of the pelvis and abdomen, and MRI pelvis was done in some patients. Examination under anaesthesia was done by senior surgical oncologists, for patients with bulky tumours > 4 cm on clinical examination, to accurately stage the disease, and cystoscopy was done to rule out bladder involvement.
The neo-adjuvant chemotherapy given for stage IB2 to IIB cancers was 3 cycles of cisplatin 75 mg/m2 and paclitaxel 175 mg/m2 in 21 day cycles. In pre-operative CRT arm, 50 Gy pelvic RT (external beam radiation) including the pelvic nodal basins along with 2 cycles of cisplatin 75 mg/m2 and paclitaxel 175 mg/m2 in 21-day interval. The entire treatment including surgery was completed in a period of 8 to 10 weeks. Patients who had prior abdominal surgery were not considered a contraindication for laparoscopic surgery. The patients in each group were similar in age, stage of disease, pathological type and pre-operative therapies.
Laparoscopic radical hysterectomy (LRH) was done in an exactly similar way as the conventional open radical hysterectomy (ORH) without any oncological compromise. Querleu-Morrow type C1 nerve sparing hysterectomy was the standard procedure of radical hysterectomy done in our centre. For all patients, intra-corporeal colpotomy IC) was done laparoscopically using a harmonic scalpel no one had a vaginal colpotomy(VC). Bilateral pelvic lymphadenectomy was done for all patients removing common iliac, external iliac, internal iliac and obturator nodes, and in LRH the nodes were retrieved through an endobag inserted per vaginally. We never used an uterine manipulator during laparoscopic hysterectomy. The estimated blood loss was measured from the number of fully and partially soaked pads in open surgery and the difference between the total volume of fluid in suction bottle and the amount of fluid used for irrigation both in ORH and LRH. The Foley’s catheter was removed on the 10th post-operative day for both ORH and LRH, and the adequate functioning of the urinary bladder was identified with subjective normal sensation of filling and satisfactory emptying and residual urine volume < 100 ml measured with an ultrasound. The catheter was reinserted and kept for 2 more weeks if the residual volume was > 100 ml. The length of hospital stay was calculated from the first post-operative day to discharge from hospital. The progression-free survival (PFS) and overall survival (OS) were calculated from the date of surgery to the first recurrence and death due to cancer, respectively.
The patients who had early cervical cancer received adjuvant CRT if they had parametrial involvement, nodal involvement or margin positivity after definitive histopathological examination. In node negative, margin negative patients, Sedlis criteria [18] were used for administering adjuvant treatment.
Statistical analysis
Statistical analysis was done using IBM SPSS Statistic Data Editor version 20. We used Person’s Chi-square test for categorical variables, independent samples T test for continuous variables and Kaplan–Meier Survival analysis with log-rank test to compare PFS and OS. A value of p < 0.05 was considered statistically significant.
Results
A total of 171 patients’ data were analysed, of them 82 patients underwent LRH and 84 patients had ORH. In 14 patients, laparoscopic surgery was converted to open for various reasons, most commonly for control of excessive bleeding in six patients, repair of bladder injury (n = 2), rectal injury (n = 1) and in five patients to overcome difficulty of laparoscopic dissection due to extensive fibrosis. All these conversions except one were before September 2016 during the initial period after commencing laparoscopic surgeries in our centre. For survival analysis, the three patients converted for repair of bladder and rectal injuries in whom the dissections were completely laparoscopic were included in LRH and others in the ORH arm. The patients who lost follow-up and died due to other causes were censored for survival analysis. The mean age at presentation was 51.4 years (LRH-52.5, ORH-50.3). Majority of our patients 42.7% (LRH n = 28, ORH n = 45) presented with FIGO stage IIB cervical cancer, 25.1% (LRH n = 24, ORH n = 19) with stage IB1, 12.9% with stage IB2, 10.5% stage IIA2 and 8.8% with stage IIA1. 33.9% of patients (n = 58) underwent primary surgery, 30.4% (n = 52) received pre-operative RT, 27.5% patients (n = 47) had pre-operative chemotherapy and 8.2% (n = 14) received definitive RT, but had residual disease. The demographic details of the patients are listed in Table 1. Squamous cell carcinoma was the most common histological type (n = 153, 89.5%). Eighteen (31.1%) patients in the primary surgery arm received adjuvant radiation for various indications which are listed in detail in Table 2.
Surgical Outcomes
The average blood loss was significantly lower in LRH group 169.2 ml versus 187.2 ml for ORH (p = 0.03). There was no significant difference in the operating times between the two groups, 151.7 min and 143.1 min for LRH and ORH, respectively (p = 0.3). The average length of hospital stay was similar between the two groups, 11.8 days for LRH and 12.2 days for ORH, respectively (p = 0.1). The surgical outcomes of two groups are listed in Table 3. The total number of lymph nodes harvested was compared separately for primary surgery and surgery after chemotherapy or RT. For patients who underwent primary surgery, the average lymph node harvests were 9.6 and 10.2 (p = 0.37) for LRH and ORH, respectively, and 8.2 versus 9.3 (p = 0.4) for surgery after either chemotherapy or RT. Resection with negative margins resection was achieved in all patients irrespective of the surgical approach. Among the patients who received pre-operative therapy, 62.2% (n = 23) in the LRH arm and 55% (n = 33) in the ORH arm had pathological complete response. During laparoscopic surgery two patients had bladder injury (1 in primary surgery and 1 in pre-op RT) and 1 rectal injury (pre-op RT), while there was 1 bladder injury (pre-op RT) and no rectal injury in the open group. There were no intra-operative ureteric injuries in both groups. Overall, the number of injuries was higher in the LRH group but without statistically significant difference (p = 0.1). Early post-operative morbidities including bladder dysfunction and vesico-vaginal and uretero-vaginal fistulas were higher with laparoscopic surgery. In LRH 15.9% (n = 13, 3 in primary surgery, 7 in pre-op RT, 2 in pre-op chemo) had temporary bladder dysfunction, which was seen in 8.9% (n = 8, 1 in primary surgery, 5 in pre-op RT, 2 in pre-op chemo) in ORH arm. However, the bladder dysfunction improved with pelvic floor exercises along with medical management, and only 2 patients in the former group and 1 patient in the latter had prolonged bladder morbidity that needed long-term catherisation (p = 0.3). Vesico-vaginal fistula occurred in four patients and uretero-vaginal fistula in three patients following laparoscopic surgery, and three patients had vesico-vaginal fistula, and one patient had uretero-vaginal fistula after open surgery. All patients were managed conservatively with prolonged catherisation for vesico-vaginal fistula, and four patients had DJ stenting for uretero-vaginal fistula (p = 0.3). The rates of inadvertent intra-operative injuries and post-operative morbidity were high in the patients who received pre-operative CRT; however, there were no statistical differences between the two arms when only the patients who received pre-operative CRT were compared. The surgical complications and recurrences in the two arms are shown in Table 4.
Survival Outcomes
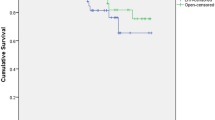
The median follow-up time was 33.5 months (range 24 to 65 months) for LRH and 57 months (range 28 to 85 months) for ORH groups. There were 15 recurrences totally, 6 in LRH and 9 in ORH group. The overall recurrence rate was 7.05% for LRH and 9.47% for ORH group; for primary surgery, it was 2.9% and 4.3%, and for surgery after neo-adjuvant therapy recurrence was 9.8% and 11.2% for LRH and ORH, respectively. The recurrences were 1 in each group after primary surgery, and both were local recurrences. Surgery after neo-adjuvant therapy resulted in 5 recurrences in LRH and 8 in ORH arm. In LRH 1 was local recurrence, 1 nodal recurrence, 2 distant recurrences and 1 port site recurrence. In the ORH arm, three local recurrences, two nodal and three distant recurrences occurred. The majority of patients who underwent primary surgery had stage IB1 disease, and stage IIB was most common in surgery of neo-adjuvant therapy. Hence, the survival for these two stages was compared between the two arms. Survival analysis by Kaplan–Meier method showed similar PFS and OS between the two groups. For stage IB1, the OS was 100% at the end of 2 years in both arms, and PFS was 100% and 95.9% for LRH and ORH, respectively. The survival outcomes for stage IIB were also similar between the groups, with OS 92.8% and 93.4% and PFS 89.3% and 88.9% for LRH and ORH arms, respectively. Stage for stage comparison of survival outcomes showed no significant difference. The outcomes of Kaplan–Meier analysis are shown in Fig. 1a–d. For all stages combined, the 2-year survival was 97.1% and 95.8% after primary surgery, and after posts neo-adjuvant therapy it was 90.2% and 88.7%, for LRH and ORH, respectively (Figs. 2, 3 and 4).
Discussion
Laparoscopic radical hysterectomy (LRH) was first reported by Nezhat et al. in 1992; since then many centres are performing LRH, and the rates have steeply gone up in the last decade [19]. In this retrospective study, we found that there is no significant difference in the recurrence rates and 2-year survival between LRH and open radical hysterectomy (ORH). LRH had significantly less blood loss; the other factors including duration of surgery, length of hospital stay, lymph node harvest, rate of negative margin resection and post-operative morbidity were similar between the two groups. The number of intra-operative complications was higher in the LRH group but did not reach statistical significance.
Many previous retrospective studies have compared LRH and ORH and reported that LRH was non-inferior to ORH in oncological outcomes and survival. The LACC trial, a multi-centre trial, that randomised 319 patients to minimally invasive surgery and 312 to ORH. Ramirez et al. reported a significantly less disease-free survival at 4.5 years compared to open (86.0% versus 96.5%; 95% CI, − 16.4 to − 4.7) and overall survival (3-year rate, 93.8% vs. 99.0%; HR- 6.00; 95% CI, 1.77 to 20.30). The higher incidence of recurrence in LRH have been hypothesised due to the CO2 pneumoperitoneum causing tumour dissemination, steep Trendelenberg position during LRH and the use of uterine manipulator [16]. We had never used an uterine manipulator in any of our laparoscopic surgeries. There are some controversies upon these results like lower recurrence rates compared to other studies and the proficiency of the surgeons have been questioned [20, 21], with the rate of minimally invasive surgery being 11.5% in the USA, and it is close to 50% in many high volume centres in Asia [22, 23]. However, this is the only randomised trial available to compare the efficacy of these two approaches. The results of LACC trial were supported by a retrospective analysis by Melamed et al. including 2461 patients, at a median follow-up of 45 months; the 4-year mortality was 9.1% in minimally invasive surgery cohort and 5.3% in open surgery (HR, 1.65; 95% CI, 1.22 to 2.22; p = 0.002) [24]. In our centre, the recurrence rates and survival were similar between the two groups. This may be due to the fact that many of our patients received pre-operative therapy either chemotherapy or CRT which would have influenced the local and distant failures. After the LACC trial results, Kim and colleagues did a retrospective analysis and found that LRH had a poorer progression-free survival (PFS; 5-year rate, 78.5% vs. 89.7%; p < 0.001), and LRH was an independent poor prognostic factor for PFS (adjusted HR, 2.883; 95% CI, 1.711–4.859; p < 0.001). However, the analysis of a subset of patients with tumour size < 2 cm in pre-operative MRI displayed that LRH does not influence PFS in tumours < 2 cm. They concluded that LRH can still be safely done in patients with smaller tumours [25]. In this study, they showed no difference in recurrence between IC and VC, but various retrospective studies have shown IC to be a strong prognostic factor of recurrence for stage IB to IIA cancers [26, 27]. IC was the only method used in all our surgeries, and hence, there was no separate comparison of IC and VC.
Centina et al. compared the outcomes of pre-operative CRT with radical surgery to definitive CRT which included intrcavitary brachytherapy. The PFS and OS were similar with a projected 5-year survival of 78% for both groups. The patients who had surgery as a part of their treatment suffered acute and late surgical complications including wound infection, dehiscence and uretero-vaginal fistula, intra-abdominal abscess, lymph cyst and a statistically significant increase in hydronephrosis in surgical patients. Nevertheless, the patients who received definitive CRT suffered from proctitis more frequently [28]. In another retrospective comparison of LRH and ORH by Wang et al. for patients with stages IB2, IIA1, IIA2 and IIB, the DFS and OS was poor in LRH for stage IB2, but there was no difference in survival outcomes for stage IIA and IIB disease [29]. Sananes et al. compared neo-adjuvant chemotherapy followed by radical hysterectomy to standard CRT and showed that neo-adjuvant chemotherapy with radical surgery similar oncologic outcomes for locally advanced cervical cancer with complete clinical response and residual tumour < 2 cm after neo-adjuvant therapy [30]. Various other studies have reported the effectiveness of neo-adjuvant chemotherapy or CRT followed by radical surgery in locally advanced cervical cancers [31,32,33]. In our centre, neo-adjuvant chemotherapy and CRT were used in bulky stage I and stage II tumours, and we compared the oncologic outcomes to definitive CRT. The interim results showed equivalent therapeutic response and better toxicity profile and better quality of life for pre-operative CRT compared to definitive CRT.
In a retrospective study by Nam et al., in early-stage cervical cancer [34], LRH (n = 263) and ORH (n = 263), even in patients with tumours > 2 cm in diameter, the risks of recurrence (HR = 0.82; 95% CI 0.31–2.16) or death (HR = 1.01; 95% CI 0.35–2.95) were not higher for LRH than for ORH. The LRH and ORH group had 5-year recurrence-free survival rates of 92.8% and 94.4%, respectively (p = 0.499). LRH resulted in significantly lower estimated blood loss (379.6 versus 541.1 ml, p < 0.001) and shorter post-operative hospital stay (12.5 versus 20.3 days, p < 0.001). Intraoperative complication rates were similar in the two groups (6.8% versus 5.7%, p = 0.711), but post-operative complication rate was lower in the LRH than in the ORH group (9.2% versus 21%, p < 0.001). The average blood loss was significantly less in the LRH in our study, but the mean operating time, lymph node harvest, duration of hospital stay were similar between the two arms. Bogani et al. compared the outcomes of LRH and ORH and found LRH had lower blood loss and shorter hospital stay and had higher 30 day pelvic floor dysfunction rates compared to ORH [35]. Wang et al. has reported the outcomes of LRH and ORH in locally advanced cervical cancers and showed that the LRH resulted in significantly less blood loss, lesser transfusion rates and shorter hospital stay [29]. Various studies have reported higher wound complications and other post-operative complications with ORH. The duration of hospital stay was similar between LRH and ORH, in contrast to the results of other studies may be due to the fact that we retained the Foley’s catheter till day 10 and patients in both arms were discharged at similar times. The duration of surgery was also not significantly different, and the mean durations of both approaches were lesser that that reported in previous studies. The duration of surgery in LRH plummeted after 2 years of starting compared to the initial periods in the learning curve.
The incidence of bladder injury was higher in LRH but without statistical significance. Intra-operative bladder and ureteric injuries and post-operative uretero-vaginal and vesico-vaginal fistulas are the major urologic complications of radical hysterectomy [36]. Bladder injuries usually occur during separation of bladder from the vagina to obtain adequate margin, and ureteric injuries are common while separating the ureter to identify the uterine artery and during de-roofing of the ureter [37]. A recent meta-analysis of 38 studies by Hwang et al. found that LRH was associated with higher intra-operative (OR 1.40, 95% CI 1.05–1.87) and post-operative urologic complications (OR 1.35, 95% CI 1.01–1.80) compared to ORH. The incidence of bladder injuries was significantly higher than the ureteric injuries, and obesity was found to be associated with increased risk of intra-operative urologic complications. In the same study, a sub-group analysis of studies published after 2012 showed that there were no increased urologic complications in LRH compared to ORH [38]. The surgical complications reported in different studies, particularly fistulas, lymphocysts and hydronephrosis were higher for surgery following CRT compared to primary surgery or after chemotherapy. The number of patients with post-operative complications was higher after pre-operative CRT, in our study, irrespective of the type of surgical approach [39, 40].
The incidence of bladder dysfunction was 16.3% in LRH and 9.2% in ORH group in our study, and this improved with treatment and only 3 patients in LRH and 1 patient in ORH had prolonged bladder dysfunction. There was no significant difference between the two arms. The injury to the hypogastric nerves, inferior hypogastriac plexus or the pelvic splanchnic nerves lead to bladder and bowel dysfunction, and they account for 76% to 85% of post-operative morbidity [41, 42]. With the introduction nerve sparing radical hysterectomy, the rates of these complications have come down, but still 37% of patients develop bladder dysfunction, which affects the quality of life [43]. Further the investigators have suggested that the magnified view in laparoscopy helps in nerve preservation better than open surgery [35]. The benefit of nerve sparing LRH is not only in improving bladder function, but also has been shown to improve bowel and sexual function [44]. Nerve sparing LRH results in earlier recovery of bowel function and in long term significantly decreased the incidence of constipation [45, 46].
The oncological and surgical outcomes of a procedure varies significantly between centres depending upon the type of institution, whether it is a teaching hospital, dedicated cancer institute or a tertiary care hospital and the volume of cases treated in that particular centre [47, 48]. This has been proved in a recent study by Haog et al. [49]. Applying the results of a RCT for a surgical procedure to all patients and surgeons worldwide may not be appropriate and should be done cautiously, considering various factors. Even in the LACC trial, sub-optimal outcomes for LRH were observed only in 14 of the 33 participating centres [16]. The equivalent outcomes observed in our study can be construed based on the fact that our patients and conditions are dissimilar to other studies.
The limitations of our study are firstly it is a retrospective study with its inherent biases, and the number and characteristics of patients in different stages of cancer in the two arms were not exactly matched. LRH is being done only for the past 5 years, and the duration of follow-up is very different between the two arms which cannot be matched. We have reached similar oncological outcomes for LRH with a median follow-up of 33.5 months. Almost two-thirds of our patients had received some form of pre-operative therapy, which can be attributed to the good survival outcomes obtained in both forms of surgical approaches.
In this analysis, we have showed that the oncological outcomes and survival after LRH was similar to ORH, and LRH had significantly lesser blood loss. The intra-operative and post-operative complications were not significantly different. Even though the only randomised trial is against the practice of LRH, many retrospective studies have shown LRH to be safe at least in early stages of disease. The reason for failure of LRH in the LACC trial has to be studied and further studies with modification of techniques and including newer technologies may confer better outcomes. Any hypothesis has to be put under repeated testing, to have a scientific discovery. With all the limitations and observations from our study, we can state that there is enough evidence to further evaluate the usefulness of minimally invasive techniques in the treatment of cervical cancer, and Laparoscopy should not be given up all over.
References
Arbyn M, Weiderpass E, Bruni L, Sanjosé S, Saraiya M, Ferlay J, Bray F. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2019. https://doi.org/10.1016/S2214-109X(19)30482-6.
Globocan India 2018. Population fact sheets, p. 1–2. http://www.gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Programme NCR. Time trends and cancer incidence rates: 1982–2005. Bangalore: National Cancer Registry Programme; 2009.
Srivastava AN, Misra JS, Srivastava S, Das BC, Gupta S. Cervical cancer screening in rural India: status and current concepts. Indian J Med Res. 2018;148:687–96.
Badwe RA, Dikshit R, Laversanne M, Bray F. Cancer incidence trends in India. Jpn J Clin Oncol. 2014;44:401–7.
American College of Obstetricians and Gynecologists ACOG Practice Bulletin. Diagnosis and treatment of cervical carcinomas. Number 35, May 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002;78(1):79–91. https://doi.org/10.1016/s0020-7292(02)90092-5.
Gaffney DK, Erickson-Wittmann BA, Jhingran A, et al. ACR appropriateness criteria® on advanced cervical cancer expert panel on radiation oncology-gynecology. Int J Radiat Oncol Biol Phys. 2011;81(3):609–14. https://doi.org/10.1016/j.ijrobp.2010.11.005.
Houvenaeghel G, Lelievre L, Gonzague-Casabianca L, et al. Long-term survival after concomitant chemoradiotherapy prior to surgery in advanced cervical carcinoma. Gynecol Oncol. 2006;100:338–43.
Touboul E, Lefranc JP, Blondon J, et al. Preoperative radiation therapy and surgery in the treatment of ‘“bulky”’ squamous cell carcinoma of the uterine cervix (stage IB, IIA, and IIB operable tumors). Radiother Oncol. 1992;24:32–40.
Neoadjuvant Chemotherapy for Cervical Cancer Meta-Analysis Collaboration (NACCCMA) Collaboration. Neoadjuvant chemotherapy for locally advanced cervix cancer. Cochrane Database Syst Rev. 2004. https://doi.org/10.1002/14651858.CD001774.pub2.
Wang W, Chu HJ, Shang CL, Gong X, Liu TY, Zhao YH, et al. Long-term oncological outcomes after laparoscopic versus abdominal radical hysterectomy in stage IA2to IIA2 cervical cancer: a matched cohort study. Int J Gynecol Cancer. 2016;26:1264–73.
Jin YM, Liu SS, Chen J, Chen YN, Ren CC. Robotic radical hysterectomy is superior to laparoscopic radical hysterectomy and open radical hysterectomy in the treatment of cervical cancer. PLoS ONE. 2018;13:e0193033.
Magrina JF, Kho RM, Weaver AL, Montero RP, Magtibay PM. Robotic radical hysterectomy: comparison with laparoscopy and laparotomy. Gynecol Oncol. 2008;109:86–91.
Abu-Rustum NR, Gemignani ML, Moore K, Sonoda Y, Venkatraman E, Brown C, et al. Total laparoscopic radical hysterectomy with pelvic lymphadenectomy using the argon beam coagulator: pilot data and comparison to laparotomy. Gynecol Oncol. 2003;91:402–9.
Ramirez PT, Frumovitz M, Pareja R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895–904.
Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncol. 2008;9(3):297–303.
Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: a gynecologic oncology group study. Gynecol Oncol. 1999;73(2):177–83. https://doi.org/10.1006/gyno.1999.5387.
Nezhat CR, Burrell MO, Nezhat FR, Benigno BB, Welander CE. Laparoscopic radical hysterectomy with paraaortic and pelvic node dissection. Am J Obstet Gynecol. 1992;166(3):864–5.
Leitao MM Jr. The LACC trial: has minimally invasive surgery for early-stage cervical cancer been dealt a knockout punch? Int J Gynecol Cancer. 2018;28:1248–50.
Kanao H, Aoki Y, Takeshima N. Unexpected result of minimally invasive surgery for cervical cancer. J Gynecol Oncol. 2018;29:e73.
Wright JD, Herzog TJ, Neugut AI, Burke WM, Lu YS, Lewin SN, et al. Comparative effectiveness of minimally invasive and abdominal radical hysterectomy for cervical cancer. Gynecol Oncol. 2012;127:11–7.
Kim JH, Kim K, Park SJ, et al. Comparative effectiveness of abdominal versus laparoscopic radical hysterectomy for cervical cancer in the post dissemination era. Cancer Res Treat. 2019;51(2):788–96. https://doi.org/10.4143/crt.2018.120.
Melamed A, Margul DJ, Chen L, et al. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med. 2018;379(20):1905–14. https://doi.org/10.1056/NEJMoa1714923.
Kim SI, Cho JH, Seol A, et al. Comparison of survival outcomes between minimally invasive surgery and conventional open surgery for radical hysterectomy as primary treatment in patients with stage IB1-IIA2 cervical cancer. Gynecol Oncol. 2019;153(1):3–12. https://doi.org/10.1016/j.ygyno.2019.01.008.
Kong TW, Chang SJ, Piao X, Paek J, Lee Y, Lee EJ, et al. Patterns of recurrence and survival after abdominal versus laparoscopic/robotic radical hysterectomy in patients with early cervical cancer. J Obstet Gynaecol Res. 2016;42:77–86.
Choi CH, Lee JW, Lee YY, Kim HJ, Song T, Kim MK, et al. Comparison of laparoscopic-assisted radical vaginal hysterectomy and laparoscopic radical hysterectomy in the treatment of cervical cancer. Ann Surg Oncol. 2012;19:3839–48.
Cetina L, Garcia-Arias A, Candelaria M, et al. Brachytherapy versus radical hysterectomy after external beam chemoradiation: a non-randomized matched comparison in IB2–IIB cervical cancer patients. World J Surg Oncol. 2009;7:19. https://doi.org/10.1186/1477-7819-7-19.
Wang W, Li L, Wu M, Ma S, Tan X, Zhong S. Laparoscopic versus abdominal radical hysterectomy for locally advanced cervical cancer. Front Oncol. 2019;9:1331. https://doi.org/10.3389/fonc.2019.01331.
Sananes C, Giaroli A, Soderini A, Guardado N, Snaidas L, Bermudez A, Ferreira M, di Paola G, Sardi J. Neoadjuvant chemotherapy followed by radical hysterectomy and postoperative adjuvant chemotherapy in the treatment of carcinoma of the cervix uteri: long-term follow-up of a pilot study. Eur J Gynaecol Oncol. 1998;19(4):368–73 (PMID: 9744728).
Behtash N, Nazari Z, Ayatollahi H, Modarres M, Ghaemmaghami F, Mousavi A. Neoadjuvant chemotherapy and radical surgery compared to radical surgery alone in bulky stage IB–IIA cervical cancer. Eur J Surg Oncol. 2006;32:1226–30.
Monk BJ, Solh S, Johnson MT, Montz FJ. Radical hysterectomy after pelvic irradiation in patients with high risk cervical cancer or uterine sarcoma: morbidity and outcome. Eur J Gynaecol Oncol. 1993;14:506–11.
Morice P, Haie-Meder C, Rey A, Pautier P, Lhommé C, Gerbaulet A, Duvillard P, Castaigne D. Radiotherapy and radical surgery for treatment of patients with bulky stage IB and II cervical carcinoma. Int J Gynecol Cancer. 2000;10:239–46.
Nam JH, Park JY, Kim DY, et al. Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: long-term survival outcomes in a matched cohort study. Ann Oncol. 2012;23:903–11.
Bogani G, Ditto A, Martinelli F, et al. Investigating the role of minimally invasive radical hysterectomy in cervical cancer. J Invest Surg. 2020;33(4):387–8. https://doi.org/10.1080/08941939.2018.1505010.
Hwang JH, Lim MC, Joung JY, Seo SS, Kang S, Seo HK, et al. Urologic complications of laparoscopic radical hysterectomy and lymphadenectomy. Int Urogynecol J. 2012;23(11):1605–11.
Limon Luque LM, Alva Trujillo HN, Delgado UJ. Urologic lesions in gynecologic and uro-gynecologic surgery. Two years of hospital experience. Ginecol Obstet Mex. 1995;63:410–3.
Hwang JH, Kim BW. Laparoscopic radical hysterectomy has higher risk of perioperative urologic complication than abdominal radical hysterectomy: a meta-analysis of 38 studies. Surg Endosc. 2020;34(4):1509–21. https://doi.org/10.1007/s00464-020-07366-1.
Hatch KD, Parham G, Shingleton H. Ureteral strictures and fistulae following radical Wertheim hysterectomy. Gynecol Oncol. 1984;19:17–23. https://doi.org/10.1016/0090-8258(84)90152-5.
Lopez-Graniel C, Reyes M, Chanona G, Robles E, Mohar A, Lopez-Basave H, De La Garza JG, Dueñas-Gonzalez A. Type III radical histerectomy after induction chemotherapy for patients with locally advanced cervical carcinoma. Int J Gynecol Cancer. 2001;11:210–7. https://doi.org/10.1046/j.1525-1438.2001.01012.x.
Manchana T, Prasartsakulchai C, Santingamkun A. Long-term lower urinary tract dysfunction after radical hysterectomy in patients with early postoperative voiding dysfunction. Int Urogynecol J. 2010;21:95–101.
Scotti RJ, Bergman A, Bhatia NN, et al. Urodynamic changes in urethrovesical function after radical hysterectomy. Obstet Gynecol. 1986;68:111–20.
Yang L, Cai J, Dong W, et al. Laparoscopic radical hysterectomy and pelvic lymphadenectomy can be routinely used for treatment of early-stage cervical cancer: a single-institute experience with 404 patients. J Minim Invasive Gynecol. 2015;2:199–204.
Bogani G, Rossetti DO, Ditto A, et al. Nerve-sparing approach improves outcomes of patients undergoing minimally invasive radical hysterectomy: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2018;25:402–10.
Lucidi A, Windemut S, Petrillo M, et al. Self-reported long-term autonomic function after laparoscopic total mesometrial resection for early-stage cervical cancer: a multicentric study. Int J Gynecol Cancer. 2017;27:1501–7.
Bogani G, Cromi A, Uccella S, et al. Nerve-sparing versus conventional laparoscopic radical hysterectomy: a minimum 12 months’ follow-up study. Int J Gynecol Cancer. 2014;24:787–93.
Pfister DG, Rubin DM, Elkin EB, Neill US, Duck E, Radzyner M, Bach PB. Risk adjusting survival outcomes in hospitals that treat patients with cancer without information on cancer stage. JAMA Oncol. 2015;1:1303–10.
Matsuo K, Shimada M, Yamaguchi S, Matoda M, Nakanishi T, Kikkawa F, Ohmichi M, Okamoto A, Sugiyama T, Mikami M. Association of radical hysterectomy surgical volume and survival for early-stage cervical cancer. Obstet Gynecol. 2019;133:1086–98.
Hoag JR, Resio BJ, Monsalve AF, Chiu AS, Brown LB, Herrin J, Blasberg JD, Kim AW, Boffa DJ. Differential safety between top-ranked cancer hospitals and their affiliates for complex cancer surgery. JAMA Netw Open. 2019;2(4):e191912. https://doi.org/10.1001/jamanetworkopen.2019.1912.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shanmugam, S., Susikar, S., Hussain, S.A. et al. A Retrospective Comparison of the Outcomes of Laparoscopic and Open Radical Hysterectomy for Early and Advanced Cancer of the Cervix, in the Post-LACC Era. Indian J Gynecol Oncolog 18, 122 (2020). https://doi.org/10.1007/s40944-020-00473-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-020-00473-w