Abstract
There has been conflicting evidence on the impact of bilateral breast cancer (BBC) on the survival and management of patients. The objectives of this study were to address the incidence of BBC and to investigate its characteristics and outcome compared to unilateral cancer. Data were acquired from the prospectively maintained NUIG breast cancer database between 1988 and 2008. BBC were then categorized as synchronous (within 12 months) or metachronous (after 12 months of first tumour). SPSS was used for data analysis. The incidence of BBC in our population was 4.4% (112 of 2,524). Of those 2.1% were synchronous while 2.3% were metachronous. Compared to unilateral cases, bilateral cancer patients were younger (P = 0.021) and had smaller size (P = 0.001) and earlier stage (P < 0.001) tumours at diagnosis. We identified the HER2/neu positivity as a risk factor for developing contralateral breast tumour and ER negativity as a risk factor for developing metachronous tumours. While there was no significant difference in survival for patients with bilateral compared to unilateral tumour (P > 0.05), the synchronous tumour was associated with poorer survival (P = 0.010) in comparison to metachronous tumour. This large single-institutional experience does not support the increasing practice of prophylactic mastectomy but does justify regular follow-up with mammography for early detection of contralateral tumour.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common malignancy and second only to lung cancer as the major cause of cancer-related deaths among women in the western world [1]. Increasing breast cancer incidence rates, improved diagnosis and management modalities and growing life expectancy have resulted in increasing numbers of women at risk of developing contralateral primary breast cancer. The incidence of clinically observed bilateral breast cancer (BBC) is reported to range from 1.4 to 11.8% [2–5]. There is uncertainty in the literature whether developing a contralateral tumour influences the outcome as some studies suggest poor survival while others report similar survival compared to unilateral disease. Women diagnosed with breast cancer are at increased risk of developing contralateral breast tumour. This represents two to six times greater relative risk than developing a first breast cancer in general population [6]. Other factors including family history of breast cancer, initial tumour diagnosed at an early age, lobular histology of the first tumour, treatment received for the first tumour and nulliparity all contribute to the risk [5, 7–10].
There has been conflicting evidence on the impact of BBC on management of patients with regard to surgical treatment options, bilateral prophylactic mastectomy and role of magnetic resonance imaging (MRI) in patients’ screening. The best management of patients with BBC is still uncertain. Patients are often treated with bilateral mastectomy rather than breast conserving treatment although some reports confirm its efficiency in management of BBC as for unilateral tumours [11, 12]. Secondly, there has been a dramatic increase in rates of contralateral prophylactic mastectomy after technical advances in surgical procedures and improved satisfaction with breast reconstruction, especially in the US [13]. This is because of the perception of increased risk of BBC and related mortality, allowing patients to avoid the physical, emotional and financial costs associated with second tumour detection and treatment. However, the potential benefit of prophylactic mastectomy in reducing the rates of BBC diagnoses and improving survival rate is controversial [14, 15]. Finally, multiple reports demonstrate increased sensitivity of MRI for detection of breast cancer compared to conventional methods particularly in patients suspected or known to have cancer [16, 17]. Nevertheless, its role in screening settings has not yet been outlined. This might be, in part, related to the moderate specificity of MRI and the associated deficiencies of cost, anxiety and benign biopsies and perhaps over-diagnosis.
The objectives of this study were to examine a defined group of breast cancer patients with a view to addressing the incidence, clinicopathological characteristics and outcome of BBC amongst these patients to study its outcome and survival compared to unilateral tumours and to analyze the disease clincopathological characteristics in order to identify the risk group. Moreover, we aimed to give context to our management of patients with BBC based on a prospectively maintained database which captures all such patients referred to our institution.
Materials and methods
Patient cohort
The prospectively updated Galway university hospital breast cancer database was queried for all cases of primary breast cancer from 1988 to 2008. The resulting data were further queried for cases of BBC. The distinction between bilateral cancers and metastatic cancer in the contralateral breast was established by Chaudary’s criteria [6] which are the demonstration of in situ disease, different histological types and grades of cancer between the two breasts and no evidence of local, regional or distant metastasis. Patients with disseminated disease elsewhere in the body would be at high risk of having metastatic disease in the contralateral breast rather than a primary cancer and are not included in the group of BBC unless the two breasts have different histopathological features. In our series, 2 patients had metastatic disease when breast cancer was originally diagnosed without documented differences in histopathological features; hence, they were not considered to have BBC. The bilateral cancers were categorized as synchronous when a contralateral breast cancer was diagnosed within 12 months and metachronous when contralateral breast cancer was diagnosed after 12 months of the initial tumour diagnosis. The term contralateral tumour is used in this study to describe the second primary tumour to arise on the other breast following an initial breast cancer diagnosis. First breast is defined as the breast in which the initial tumour diagnosed while second breast is the breast in which the contralateral tumour developed.
All patients were treated according to local protocols and followed every 3 months for 1 year, 6 months for 2 years and then annually. They also have an annual mammographic review.
Data collected included age and year of presentation for both initial and contralateral tumours, tumour size, grade, stage, histological type, extent of tumour invasion and lymph node involvement, presence or absence of local or distant metastasis, and time between initial tumour diagnosis and presentation of contralateral breast tumour. The estrogen, progesterone and HER-2/neu receptor status were also noted when data were available as was local therapy and the use of hormonal therapy, chemotherapy and radiotherapy.
Statistical analysis
The risk factors for developing contralateral primary breast cancer were investigated comparing histopathological parameters of unilateral breast cancer and the first tumour of the bilateral cancers while the bilateral disease characteristics were determined comparing the unilateral cancer to the second tumour of the bilateral disease and further analyzing the synchronous and metachronous tumours. Survival studies were performed from the date of diagnosis of the first cancer and disease-free survival (DFS) was regarded as zero if the patient presented with metastatic disease.
The SPSS® 16.0 software package (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Mann–Whitney U test and t test were used, as appropriate, for comparison of continuous variables and Chi-square test for categorical variables. All tests were two sided and a result was considered significant if the calculated P value was <0.05. Survival distributions were analyzed by the method of Kaplan–Meier. The statistical significance of differences in survival between groups was determined by log rank which compares differences along all points of the curve. Multivariate analysis was done using Cox regression while for categorical data, logistic regression was used.
Results
There were 2,524 cases of breast cancer identified in the 20-year study period. Of those, 112 women had BBC (4.4%). Among the patients with BBC, 52 (46.4%) had synchronous cancers and 60 (53.6%) had metachronous breast cancers. Although the annual risk of breast cancer was increasing in our population during this study period especially from 2005 to 2008, the risk of BBC remained constant for both synchronous and metachronous tumours (Fig. 1). The mean interval between the development of metachronous cancers was 5.9 years while the median was 3.9 years. Women with BBC were younger than the unilateral group at the time of the diagnosis of their initial tumours (P = 0.021). Contralateral tumours of BBC patients measured significantly smaller than contemporary unilateral tumours (P = 0.001) and their associated initial tumour of BBC (P = 0.006). This difference was also present for synchronous tumours as the second primary was significantly smaller than the initial tumour (P = 0.003).
No significant differences were found between the study groups for histological patterns and grades of tumours. The distribution of histopathological patterns was similar for all groups of patients with more than 70% of unilateral and bilateral patients having ductal carcinoma. Nevertheless, contralateral tumours of BBC patients were diagnosed at earlier stage than the initial tumours (P < 0.001), a difference that is also noted for both synchronous (P = 0.001) and metachronous (P = 0.004) tumours. Contralateral primaries of BBC, synchronous and metachronous tumours were found to be stage 0 or I more frequently than initial tumours and stage II and III less often. A similar significant difference was also seen when comparing the contralateral tumours to unilateral breast cancer (P < 0.001).
Moreover, contralateral tumours were significantly more likely to be associated with negative axillary lymph nodes than initial tumours of BBC (P = 0.005) and unilateral breast carcinoma (P < 0.001). Again, this difference was noted to occur in synchronous (P = 0.028) but not the metachronous cancers. Seventy-nine percent of BBC patients who underwent axillary lymph node dissection were lymph node negative, 11.1% had 1–3 positive lymph nodes and 9.7% had more than 3 positive lymph nodes.
Regarding receptors status, there were significant differences in the rates of progesterone receptors (PR) positivity (P = 0.002) and HER2/neu expression (P = 0.018) but not the rate of estrogen receptor (ER) positivity (P = 0.712) between the unilateral and contralateral tumours of BBC (Tables 1, 2). Approximately 72% of unilateral tumours were PR positive and 20% were HER2/neu positive compared to 56 and 33%, respectively. In the case of BBC no significant differences were noted in any of the receptors status when comparing initial and contralateral tumours.
Risk factors
Many of the previously described risk factors for BBC were identified in our series of patients. More than 43% of patients who developed BBC have family history of breast cancer, 33% were using oral contraceptive and 14.3% were on postmenopausal hormones. The characteristics of the first tumour of BBC were analyzed in order to identify the risk factors for developing synchronous or metachronous tumours. Patients who presented with stage IV PR positive initial tumour were more likely to develop synchronous tumours (Table 3).
Detection methods
Details of methods of diagnosis for both tumours of BBC were available for 81 cases. The initial tumours were detected during screening in 16% of cases compared to 64% of contralateral tumours. The sensitivity of mammography was 86 and 87.3% for initial and contralateral tumours, respectively. 57% of initial tumours were detected by mammography compared with 74.3% of contralateral tumours. Only one case (1.4%) of contralateral tumours required MRI scan to diagnose cancer (Table 4).
Management of BBC in our institution
Thirty-three (30.6%) patients with contralateral tumours and 777 (42.7%) of the unilateral cancer patients received adjuvant chemotherapy. Hormonal therapy was prescribed to 92% of unilateral cancer group, 86% of bilateral cancer patients when got the initial tumour and 74% of them when developed the contralateral tumour. Patients with BBC were more likely to have bilateral mastectomy (64.7%). Breast conserving surgery of both breasts was performed in 11.3% and in combination with mastectomy of the other breast in 24.1% of BBC patients. Of those who had mastectomy of contralateral breast, 19.4% had breast reconstruction performed (13.3% immediate, 6.1% delayed). No significant differences were noted in both surgical treatment (P = 0.280) and radiation treatment (P = 0.093) when comparing initial and contralateral tumours of BBC. On the other hand, adjuvant hormonal and chemotherapy were differentially prescribed with P values of 0.036 and 0.006, respectively. When comparing contralateral tumours of BBC with unilateral carcinoma, there were no differences in all management modalities received by patients.
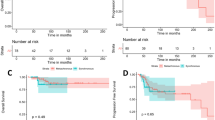
Disease-free survival
Disease-free survival was calculated as the number of months from the diagnosis of the initial tumour to recurrence (local and distant), death or last follow-up. Recurrence occurred in 42% of patients with synchronous tumours, 55% of patients with metachronous and 21% of patients with unilateral breast carcinoma. The difference in DFS was significant between the bilateral cancer patients (P = 0.013) as was the difference between the bilateral and unilateral cancer patients (P < 0.001) (Fig. 2). Median time for DFS was 52 months for synchronous tumours, 148 months for metachronous and 169 months for unilateral tumours. On Cox regression analysis, initial tumours grade (P = 0.021), stage (P = 0.020) and nodal status (P = 0.001), contralateral tumours grade (P = 0.035) and PR status (P = 0.018); and adjuvant chemotherapy for both tumours (P = 0.007) were independent predictors of DFS in BBC patients. After adjustment for these variables both groups did not differ significantly with P value of 0.157 for bilateral and unilateral tumours and 0.284 for synchronous and metachronous tumours.
Disease-free survival (DFS) analysis. (A) Although log-rank test by Kaplan–Meier was significant (P = 0.001), the difference in DFS between bilateral and unilateral cancer patients was not confirmed by Cox-regression analysis (P = 0.157). (B) Significant difference in DFS between bilateral cancer groups was determined by Kaplan–Meier (P = 0.013) but not the Cox-regression analysis (P = 0.284)
Overall survival
There was no significant difference in the overall survival of patients with bilateral and unilateral breast carcinoma (P = 0.073); however, comparison of patients with synchronous disease to those with metachronous disease yielded a significant difference with P value of 0.010 (Fig. 3). Women with synchronous tumours had a high mortality from breast cancer with median survival of 62 months compared to 148 months in metachronous and 154 months in unilateral cancer patients. A multivariate Cox regression analysis was used to determine the prognostic factors for the overall survival for all groups. ER (P < 0.001) and PR (P = 0.018) positivity, lymph nodes negativity (P = 0.001) and radiotherapy (P = 0.002) for the second primary tumour were found to be by far the most important factors. After simultaneous adjustment of all these variables, there continues to be a significant difference in the survival between synchronous and metachronous tumours (P = 0.026).
Overall survival analysis. (A) In bilateral compared to unilateral breast cancer patients. No significant difference in the overall survival between both groups as determined by Kaplan–Meier survival analysis (χ2 = 3.2, P = 0.073) and Cox-regression (P = 0.639). (B) In synchronous compared to metachronous bilateral breast cancer. The significantly reduced overall survival in synchronous tumours was confirmed by both Kaplan–Meier analysis (χ2 = 6.6, P = 0.010) and Cox-regression (P = 0.026)
Discussion
The reported incidence of BBC is variable and may reach up to 20% in patients in whom breast cancer diagnosis has been made by contralateral biopsy and mastectomy in clinically negative breasts [18]. The variations in reported incidence could be explained by the use of different analysis methods, variations in intensity of screening for contralateral tumours and differences in duration of follow-up. In accordance with previous reports, the incidence of BBC in this study was 4.4% of which 2.1% were synchronous and 2.3% were metachronous. However, as no minimum length of follow-up was defined in this study to classify patients into unilateral breast cancer group, some unilateral cases would become bilateral cases with longer follow-up. The annual risk of breast cancer was noticed to increase markedly in 2005 and after in our population. This observation not necessarily indicates an increase incidence of breast cancer but may be due to the fact that the screening programme was started in that year.
Numerous studies have found that patients with BBC were significantly younger at the time of diagnosis of their initial cancer and considered age as the most important predictor for contralateral breast cancer [5, 18–20]. The earlier a woman develops a first breast cancer, the higher the risk of developing a contralateral tumour [21]. This finding was also observed in our series of patients. Increased risk in younger group might be due to increased life expectancy and the fact that patients with family history of breast cancer develop their cancer at an early age. Furthermore, we demonstrated smaller contralateral tumour size and earlier stage when compared with unilateral tumours and the initial tumours of BBC. These differences were also observed for both synchronous and metachronous diseases. Some studies described similar differences between initial and contralateral tumours of BBC [7, 9, 22, 23] while others reported conflicting results [8, 20, 24, 25]. These findings might be related to increased compliance with screening after development of the initial tumour.
Estrogen receptor positivity was found to be predictive of bilateral disease previously [26, 27]; however, Coradini et al. [28] described no differences in ER and PR positivity of the initial and contralateral tumours. In this study, there was low rate of PR positivity in patients with bilateral tumours compared to those with unilateral disease. Examining the HER2 status, we found that initial tumours of bilateral cancers significantly overexpress HER2/neu rather than unilateral tumours (P = 0.018). Based on this we can postulate that HER2 over-expressers are more likely to develop contralateral tumour.
With regard to risk factors for developing BBC in our study, there was significant association of early stage (stage 0 and I) and PR negative initial tumours and the development of metachronous tumours. The breast conservative surgery (BCS) for the initial tumour is a confounding factor as it usually performed in early stage disease.
Multiple reports in the literature demonstrated the increased sensitivity of MRI for detection of breast cancer compared with mammography and ultrasound, with MRI sensitivity approaching 100% [16, 29–32]. However, most of these reports evaluated MRI in diagnostic settings. Lehman et al. [29] investigated the role of MRI in detecting cancer in the contralateral breast that is missed by mammography and clinical examination at the time of initial tumour diagnosis. They were able to detect cancer in only 3.1% of the women who were enrolled in the study with biopsy performed depending on MRI results on 12.5%. Furthermore, Moore et al. [33] concluded that the use of breast MRI compared to mammography for screening in young women at high risk does not appear to be cost-effective. In this study we showed that mammography is still a valid and convenient method of screening for breast cancer in women with initial breast cancer and MRI was able to detect only one mammography and clinically occult contralateral tumour. Although MRI can improve the detection of contralateral tumours, its use should be preserved for high-risk patients and in conjunction with thorough clinical examinations and mammographic evaluation.
Adjuvant therapy generally is given to improve the survival and to reduce the incidence of contralateral breast cancer. Both chemotherapy and tamoxifen were found to be associated with reduced risk of contralateral breast cancer. Both Bertelsen et al. [34] and Vogel et al. [35] observed a significant reduction of incidence of contralateral primary breast cancer among women receiving adjuvant hormonal therapy. Adjuvant hormonal therapy also reported to reduce the incidence of BBC by 40% in both ER positive and ER negative patients [36]. Consistent with what was previously stated, in this study, adjuvant therapy was significantly associated with improved disease-free and overall survival. Furthermore, adjuvant hormonal therapy was significantly more prescribed in unilateral cancer group compared to initial tumours of BBC, which might indicate its role in reducing the risk of developing a contralateral tumour.
The surgical management of BBC patients is an area for debate. The controversy is due to the conflicting data regarding the role of contralateral prophylactic mastectomy in preventing BBC, the belief of superiority of mastectomy over breast conserving surgery for management of contralateral tumours and the increasing risk of developing contralateral tumour after conserving breast surgery and radiotherapy for the initial cancer. Bedrosian et al. [37] in their study using SEER database showed that contralateral prophylactic mastectomy is associated with small improvement in 5-year survival, mainly in young women with stages I–II disease ER-negative breast cancer. However, most of previous reports confirmed that contralateral prophylactic mastectomy is unlikely to be beneficial in improving disease-specific survival when performed outside of the existing recommendations [15, 38]. Moreover, measurable morbidity rates and negative psychological impacts were found to be associated with prophylactic mastectomy [39, 40]. Secondly, BCT was described as a safe and efficacious treatment option for treating early stage cancer [11, 27, 41, 42]. Yamauchi et al. [42] demonstrated no local recurrence or distant metastasis in patients who underwent bilateral BCT after a median follow-up of 95 months. Lee et al. [11] also noticed no differences in survival in bilateral and unilateral caner patients treated with BCT. In addition, Rochefordiere et al. [27] found no significant difference in survival comparing 51 patients with synchronous BBC treated with bilateral BCT to a group of patients treated with either bilateral mastectomy or unilateral BCT. Finally, most studies have demonstrated no significant increase risk of contralateral breast cancer after radiation treatment for initial tumour [43–45], while others documented the opposite [46–48]. We observed no significant association between initial tumour radiation and the development of contralateral cancer. Also we noticed that the second tumours were less likely to get radiation therapy compared to the unilateral tumours due to the fact that most of the contralateral cancer patients end up with mastectomy rather than BCT.
Previous studies comparing survival between women with bilateral versus unilateral breast cancer have yielded inconsistent results. Some studies found that BBC had a poorer prognosis than unilateral cancer [12, 22, 24], whereas others showed similar prognosis for both types [7, 8, 25, 49, 50]. These variations might be related to the small number of patients, variable definitions of synchronous and metachronous cancers and the use of different methods as calculation of survival from the time of the initial or the second tumour development. Carrying out multivariate analysis, we were unable to identify significant differences in both disease-free and overall survival between bilateral and unilateral breast cancer patients, while in BBC patients synchronous tumours were significantly associated with poor overall survival. One of the reasons metachronous tumours seem to do better is because they are smaller and detected earlier by surveillance. We also identified factors like adjuvant chemotherapy, PR and ER positivity, degree of invasion and grade of the contralateral tumour as important prognostic indicators in BBC patients. In contrast, factors like histological types have no effect on BBC survival. This finding is in accordance with Mhuircheartaigh et al. [51] who found no difference in the outcome of invasive ductal and lobular breast cancer in our unit.
Conclusion
Significant differences in some characteristics of bilateral compared to unilateral breast cancer were identified in this study. However, BBC does not appear to have a major impact on the outcome beyond the initial primary tumour. The increasing practice of bilateral mastectomy is not supported by this large single-institutional experience which allows confident prediction of outcome based on accurate follow-up.
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ (2008) Cancer statistics, 2008. CA Cancer J Clin 58:71–96
Donovan AJ (1990) Bilateral breast cancer. Surg Clin N Am 70:1141–1149
Michowitz M, Noy S, Lazebnik N, Aladjem D (1985) Bilateral breast cancer. J Surg Oncol 30:109–112
Gogas J, Markopoulos C, Skandalakis P, Gogas H (1993) Bilateral breast cancer. Am Surg 59:733–735
Chen Y, Thompson W, Semenciw R, Mao Y (1999) Epidemiology of contralateral breast cancer. Cancer Epidemiol, Biomark Prev 8:855–861
Chaudary MA, Millis RR, Hoskins EO, Halder M, Bulbrook RD, Cuzick J, Hayward JL (1984) Bilateral primary breast cancer: a prospective study of disease incidence. Br J Surg 71:711–714
Heron DE, Komarnicky LT, Hyslop T, Schwartz GF, Mansfield CM (2000) Bilateral breast carcinoma: risk factors and outcomes for patients with synchronous and metachronous disease. Cancer 88:2739–2750
Newman LA, Sahin AA, Cunningham JE, Bondy ML, Mirza NQ, Vlastos GS, Whitman GJ, Brown H, Buchholz TA, Lee MH, Singletary SE (2001) A case-control study of unilateral and bilateral breast carcinoma patients. Cancer 91:1845–1853
Mertens WC, Hilbert V, Makari-Judson G (2004) Contralateral breast cancer: factors associated with stage and size at presentation. Breast J 10:304–312
Hartman M, Czene K, Reilly M, Bergh J, Lagiou P, Trichopoulos D, Adami H-O, Hall P (2005) Genetic implications of bilateral breast cancer: a population based cohort study. Lancet Oncol 6:377–382
Lee MM, Heimann R, Powers C, Weichselbaum RR, Chen LM (1999) Efficacy of breast conservation therapy in early stage bilateral breast cancer. Breast J 5:36–41
Jobsen JJ, Jvd Palen, Ong F, Meerwaldt JH (2003) Synchronous, bilateral breast cancer: prognostic value and incidence. Breast 12:83–88
Tuttle TM, Jarosek S, Habermann EB, Arrington A, Abraham A, Morris TJ, Virnig BA (2009) Increasing rates of contralateral prophylactic mastectomy among patients with ductal carcinoma in situ. J Clin Oncol 27:1362–1367
Hartmann LC, Schaid DJ, Woods JE, Crotty TP, Mayers JL, Arnold PG, Petty PM, Sellers TA, Johnson JL, McDonnell SK, Frost MH, Jenkins RB (1999) Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med 340:77–84
Quan G, Pommier SJ, Pommier RF (2008) Incidence and outcomes of contralateral breast cancers. Am J Surg 195:645–650
Lee SG, Orel SG, Woo IJ, Cruz-Jove E, Putt ME, Solin LJ, Czerniecki BJ, Schnall MD (2003) MR imaging screening of the contralateral breast in patients with newly diagnosed breast cancer: preliminary results. Radiology 226:773–778
Boetes C, Veltman J (2005) Screening women at increased risk with MRI. Cancer Imaging 23:S10–S15
Carmichael AR, Bendall S, Lockerbie L, Prescott R, Bates T (2002) The long-term outcome of synchronous bilateral breast cancer is worse than metachronous or unilateral tumours. Eur J Surg Oncol 28:388–391
Adami HO, Bergstrom R, Hansen J (1985) Age at first primary as a determinant of the incidence of bilateral breast cancer: cumulative and relative risks in a population-based case-control study. Cancer 55:643–647
Brenner H, Engelsmann B, Stegmaier C, Ziegler H (1993) Clinical epidemiology of bilateral breast cancer. Cancer 72:3629–3635
Rauschecker HF, Sauerbrei W, Gatzemeier W, Sauer R, Schauer A, Schmoor C, Schumacher M (1998) Eight-year results of a prospective non-randomized study on therapy of small breast cancer. The German Breast Cancer Study Group (GBSG). Eur J Cancer 34:315–323
Abdalla I, Thisted RA, Heinmann R (2000) The impact of contralateral breast cancer on the outcome of breast cancer patients treated by mastectomy. Cancer 6:266–272
Samant RS, Olivotto IA, Jakson ISH, Mates D (2001) Diagnosis of metachronous contralateral breast cancer. Breast J 7:405–410
Gajalakshmi CK, Shanta V, Hakama M (1999) Survival from contralateral breast cancer. Breast Cancer Res Treat 58:115–122
Irvine T, Allen DS, Gillett C, Hamed H, Fentiman IS (2009) Prognosis of synchronous bilateral breast cancer. Br J Surg 96:376–380
Lesser ML, Rosen PP, Kinne DW (1982) Multicentricity and bilaterality in invasive breast carcinoma. Surgery 91:234–240
de la Rochefordiere A, Asselain B, Scholl S, Campana F, Ucla L, Vilcoq JR, Durand JC, Pouillart P, Fourquet A (1994) Simultaneous bilateral breast carcinoma: a retrospective review of 149 cases. Int J Radiat Oncol Biol Phys 30:35–41
Coradini D, Oriana S, Mariani L, Miceli R, Bresciani G, Marubini E, Di Fronzo G (1998) Is steroid receptor profile in contralateral breast cancer a marker of independence of the corresponding primary tumour? Eur J Cancer 34:825–830
Lehman CD, Gatsonis C, Kuhl CK, Hendrick RE, Pisano ED, Hanna L, Peacock S, Smazal SF, Maki DD, Julian TB, DePeri ER, Bluemke DA, Schnall MD (2007) MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med 356:1295–1303
Kriege M, Brekelmans CT, Boetes C, Besnard PE, Zonderland HM, Obdeijn IM, Manoliu RA, Kok T, Peterse H, Tilanus-Linthorst MM, Muller SH, Meijer S, Oosterwijk JC, Beex LV, Tollenaar RA, de Koning HJ, Rutgers EJ, Klijn JG (2004) Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med 351:427–437
Viehweg P, Rotter K, Laniado M, Lampe D, Buchmann J, Kölbl H, Heywang-Köbrunner S (2004) MR imaging of the contralateral breast in patients after breast-conserving therapy. Eur Radiol 14:402–408
Lehman CD, Blume JD, Thickman D, Bluemke DA, Pisano E, Kuhl C, Julian TB, Hylton N, Weatherall P, O’loughlin M, Schnitt SJ, Gatsonis C, Schnall MD (2005) Added cancer yield of MRI in screening the contralateral breast of women recently diagnosed with breast cancer: results from the International Breast Magnetic Resonance Consortium (IBMC) trial. J Surg Oncol 92:9–15
Moore SG, Shenoy PJ, Fanucchi L, Tumeh JW, Flowers CR (2009) Cost-effectiveness of MRI compared to mammography for breast cancer screening in a high risk population. BMC Health Serv Res 9:9
Bertelsen L, Bernstein L, Olsen JH, Mellemkjaer L, Haile RW, Lynch CF, Malone KE, Anton-Culver H, Christensen J, Langholz B, Thomas DC, Begg CB, Capanu M, Ejlertsen B, Stovall M, Boice JD Jr, Re S, Women’s Environment CaRESCG, Bernstein JL (2008) Effect of systemic adjuvant treatment on risk for contralateral breast cancer in the Women’s Environment, Cancer and Radiation Epidemiology Study. J Natl Cancer Inst 100:32–40
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, Bevers TB, Fehrenbacher L, Pajon ER Jr, Wade JL III, Robidoux A, Margolese RG, James J, Lippman SM, Runowicz CD, Ganz PA, Reis SE, McCaskill-Stevens W, Ford LG, Jordan VC, Wolmark N (2006) Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA 295:2727–2741
Early Breast Cancer Trialists’ Collaborative Group (1998) Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet 351:1451–1467
Bedrosian I, Hu CY, Chang GJ (2010) Population-based study of contralateral prophylactic mastectomy and survival outcomes of breast cancer patients. J Natl Cancer Inst 102(6):401–409
Peralta EA, Ellenhorn JD, Wagman LD, Dagis A, Andersen JS, Chu DZ (2000) Contralateral prophylactic mastectomy improves the outcome of selected patients undergoing mastectomy for breast cancer. Am J Surg 180:439–445
Zion SM, Slezak JM, Sellers TA, Woods JE, Arnold PG, Petty PM, Donohue JH, Frost MH, Schaid DJ, Hartmann LC (2003) Reoperations after prophylactic mastectomy with or without implant reconstruction. Cancer 98:2152–2160
Frost MH, Slezak JM, Tran NV, Williams CI, Johnson JL, Woods JE, Petty PM, Donohue JH, Grant CS, Sloan JA, Sellers TA, Hartmann LC (2005) Satisfaction after contralateral prophylactic mastectomy: the significance of mastectomy type, reconstructive complications, and body appearance. J Clin Oncol 23:7849–7856
Gollamudi SV, Gelman RS, Peiro G, Schneider LJ, Schnitt SJ, Recht A, Silver BJ, Harris JR, Connolly JL (1997) Breast-conserving therapy for stage I–II synchronous bilateral breast carcinoma. Cancer 79:1362–1369
Yamauchi C, Mitsumori M, Nagata Y, Kokubo M, Inamoto T, Mise K, Kodama H, Hiraoka M (2005) Bilateral breast-conserving therapy for bilateral breast cancer: results and consideration of radiation technique. Breast Cancer 12:135–139
Bernstein JL, Thompson WD, Risch N, Holford TR (1992) Risk factors predicting the incidence of second primary breast cancer among women diagnosed with a first primary breast cancer. Am J Epidemiol 136:925–936
Gajalakshmi CK, Shanta V, Hakama M (1998) Risk factors for contralateral breast cancer in Chennai (Madras), India. Int J Epidemiol 27:743–750
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347:1233–1241
Boice JD Jr, Harvey EB, Blettner M, Stovall M, Flannery JT (1992) Cancer in the contralateral breast after radiotherapy for breast cancer. N Engl J Med 326:781–785
Storm HH, Andersson M, Boice JD Jr, Blettner M, Stovall M, Mouridsen HT, Dombernowsky P, Rose C, Jacobsen A, Pedersen M (1992) Adjuvant radiotherapy and risk of contralateral breast cancer. J Natl Cancer Inst 84:1245–1250
Gao X, Fisher SG, Emami B (2003) Risk of second primary cancer in the contralateral breast in women treated for early-stage breast cancer: a population-based study. Int J Radiat Oncol Biol Phys 56:1038–1045
Takahashi H, Watanabe K, Takahashi M, Taguchi K, Sasaki F, Todo S (2005) The impact of bilateral breast cancer on the prognosis of breast cancer: a comparative study with unilateral breast cancer. Breast Cancer 12:196–202
Verkooijen HM, Chatelain V, Fioretta G, Vlastos G, Rapiti E, Sappino AP, Bouchardy C, Chappuis PO (2007) Survival after bilateral breast cancer: results from a population-based study. Breast Cancer Res Treat 105:347–357
Mhuircheartaigh JN, Curran C, Hennessy E, Kerin MJ (2008) Prospective matched-pair comparison of outcome after treatment for lobular and ductal breast carcinoma. Br J Surg 95:827–833
Acknowledgments
The authors would like to acknowledge the National Breast Cancer Research Institute (NBCRI) for their financial support of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kheirelseid, E.A.H., Jumustafa, H., Miller, N. et al. Bilateral breast cancer: analysis of incidence, outcome, survival and disease characteristics. Breast Cancer Res Treat 126, 131–140 (2011). https://doi.org/10.1007/s10549-010-1057-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-010-1057-y