Abstract
Skeletal muscle is made up of hundreds of multinucleated, aligned fibers that work together during contraction. While smaller injuries are typically able to be repaired by the body, large volumetric muscle loss (VML) typically results in loss of function. Tissue engineering (TE) applications that use cells seeded onto hydrogels are one potential option for regenerating the lost tissue. Hydrogels are described as soft crosslinked polymeric networks with high water content that simulates the body’s natural aqueous environment. They can be formulated from many different starting materials into biocompatible, biodegradable systems. Fabrication methods such as electrospinning, freeze-drying, molding, and 3D printing can be used with the hydrogel solution to form 3D structures. In this review, natural, semi-synthetic, synthetic, and composite hydrogels for skeletal muscle regeneration are discussed. It was ascertained that the majority of the current research focused on natural polymeric hydrogels including collagen, gelatin, agarose, alginate, fibrin, chitosan, keratin, and combinations of the aforementioned. This category was followed by a discussion of composite hydrogels, defined in this review as at least one synthetic and one natural polymer combined to form a hydrogel, and these are the next most favored materials. Synthetic polymer hydrogels came in third with semi-synthetic polymers, chemically modified natural polymers, being the least common. While many of the hydrogels show promise for skeletal muscle regeneration, continued investigation is needed in order to regenerate a functional muscle tissue replacement.
Lay Summary
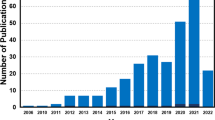
Skeletal muscle tissue engineering focuses on regenerating large amounts of skeletal muscle tissue lost due to tumor removal, traumatic injuries, and/or disease. Neither natural repair processes by the body nor current medical interventions are able to completely restore function after volumetric muscle loss. Thus, scientists are investigating alternative approaches to regenerate the lost muscle, restore function, and increase patient quality of life. This review paper summarizes the research from 2013 to early 2018 using hydrogels, a soft material with a high water content, as a tool to regenerate muscle. The review is categorized into hydrogels made from natural materials, semi-synthetic materials, synthetic materials, and composite materials (at least one natural and one synthetic material combined).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Skeletal muscle accounts for 30–40% of a human’s total body mass, and its functions include stabilization and movement of the skeleton, guarding entrances/exits to the digestive, respiratory, and urinary systems, generating heat, and protecting internal organs [1,2,3,4,5]. It consists of hundreds of multinucleated, unidirectional fibers that work together with the nervous system to coordinate movement of the entire musculoskeletal system [2,3,4]. After injury, adult skeletal muscle stem cells called satellite cells proliferate, differentiate, and fuse at the site of the injury to fill in and close the gap created by the injury. Satellite cells only account for about 1–5% of muscle cells, and if not enough are not able to accumulate at the injury site, scar tissue may form. In the case of smaller injuries, scar tissue formation may not interfere with the function of the muscle tissue [5,6,7,8,9]. However, traumatic injuries, congenital abnormalities, tumor ablation, and/or denervation lead to larger muscle loss termed volumetric muscle loss (VML) that the body is unsuccessful at repairing leading to muscle weakness [5, 8, 10,11,12,13,14,15].
VML injuries result in a change in muscle architecture and muscle strength. Garg et al. determined that VML loss after a fracture resulted in functional defects that depend on the joint angle and muscle length after inducing an osteotomy and removal of part of the tibialis anterior (TA) muscle [12]. Corona et al. evaluated 450 military service members for VML service-disqualifying disabilities following battlefield trauma from 2001 to 2005. Out of the 450 service members, 39 individuals were reported as discharged due to a muscle disabling condition with 36 of these service members having confirmed VML and/or residual muscle weakness [11]. Autologous tissue transfer is one replacement option but, is limited by donor tissue availability, results in donor site morbidity, and has poor engraftment [5,6,7, 16]. Other potential treatment options include cell transplantation, gene therapy, and growth factors just to name a few; however, none of these treatments result in functional restoration of the muscle tissue [5, 16].
An alternative treatment option, tissue engineering (TE), uses cells seeded onto biomaterials to create a viable, functional replacement tissue. The chosen biomaterial should be biocompatible, biodegradable, and have correct chemical and mechanical properties to encourage cellular growth and fusion to form parallel, aligned muscle fibers to better mimic native architecture and have contractile strength consistent with that of native skeletal muscle [10, 16]. Additionally, this cellularized biomaterial should not invoke an immune response; it should incorporate with the surrounding tissue and have integrated vasculature and peripheral nerves in vivo. Since this process focuses on regenerating tissues via a process that mimics neoorganogenesis, it already meets many of the requirements for success.
Hydrogels are a soft biomaterial characterized by high water content, biodegradability, biocompatibility, and ability to release drugs [10, 17,18,19]. Their mechanical properties are tunable due to the amount of chemical, temperature, or photocrosslinking [17, 20,21,22,23]. By tuning the hydrogel’s mechanical properties such as elastic modulus to be similar to those of native skeletal muscle, it can aid in mature skeletal muscle development. In addition, 3D structures can be created using a variety of methods such as freeze drying, molding, electrospinning, 3D printing, and injection directly into a defect [10, 17, 19,20,21, 24,25,26,27]. It is for these reasons that hydrogels are an attractive option for muscle regeneration. Skeletal muscle TE is a relatively new field with the overall goal to replace the damaged muscle with a functional scaffold that is engineered to regenerate new tissue with properties similar to the native one. In this review, we focus on natural, semi-synthetic, synthetic, and composite hydrogels, herein defined as a combination of at least one natural and one synthetic polymer, advancements for skeletal muscle regeneration from 2013 into early 2018.
Natural Hydrogels
Hydrogels made from natural materials are a popular choice as they induce a limited inflammatory response and are often components of the extracellular matrix (ECM) which has been shown to encourage skeletal muscle regeneration [10]. Some of the most investigated materials include collagen, gelatin, fibrin, alginate, and keratin. Pollet et al. screened collagen, agarose, alginate, fibrin, and collagen-chitosan hydrogels for their tensile mechanical properties and ability to grow skeletal muscle in vitro. Collagen, fibrin, and collagen-chitosan hydrogels had average elastic moduli ranging from 2.7 to 3.7 MPa. Agarose hydrogels were much stiffer with an elastic modulus of 87.3 ± 32.6 MPa, and the alginate hydrogels at the densities and dimensions used in the study were unable to be measured due to poor handability. They propose that collagen, fibrin, and collagen-chitosan hydrogels could be implanted and once stretched, activate satellite cells, since they elongate at least twofold without failing. Primary rat satellite cells seeded onto the constructs were assessed for the genetic RNA expression of MyoD, myogenin, and myosin heavy chain (MHC) which indicate maturation into contractile units. MyoD expression decreased over the 14-day period while myogenin expression peaked on day 7 before decreasing for all five hydrogel types. Only fibrin had significantly greater MHC expression on days 7 and 14. Based on these patterns of gene expression, the authors conclude that fibrin has the best potential as a scaffold for skeletal muscle regeneration, followed by collagen [10].
Fibrin hydrogels are made by combining thrombin and fibrinogen [28], which are involved in blood clotting. Matthias et al. suspended muscle derived stem cells (MDSCs) in fibrin gel and cast the solution directly into a murine TA–induced injury. One month after implantation, little fibrosis and myosin heavy chain 1 (MYH1) positive muscle fibers were present, indicating myofiber maturation in the defect [29]. Neal et al. added C2C12, murine myoblasts, into fibrin hydrogels using a sacrificial outer mold to form elongated fascicles. After subjecting, the cellularized fibrin hydrogels to axial stress for 14 days, more myotubes with a higher level of maturity were formed compared with only one side being anchored [28]. Heher et al. also applied tension to C2C12 embedded fibrin hydrogels using the MagneTissue system. After 9 days in culture, the elongated myotube diameter and length were significantly greater compared with the unstrained hydrogels and floating control [18]. These studies highlight that fibrin has had successful outcomes when formulated into hydrogels for muscle development, especially when coupled with mechanical stimulation.
Marcinczyk et al. added the ECM protein laminin (LM-111) to fibrinogen scaffolds prior to seeding with C2C12 cells. They found that incorporation of 450 μg/mL of LM-111 increased myoblast proliferation and secretion of pro-regenerative growth factors such as insulin growth factor-1 (IGF-1), human growth factor (HGF), vascular endothelial growth factor (VEGF), and interleukin-6 (Il-6). They also applied tensile and electrical stimulation to the C2C12-seeded fibrin-LM-111 hydrogels. The combination of mechanical and electrical stimulation improved cellular alignment and had an increase in both VEGF and IGF-1 secretion, but Il-6 levels were decreased compared with electrical stimulation alone. The authors conclude that the fibrin-LM-111 hydrogel is promising and should be investigated further [30].
In contrast to Pollet et al., Ansari et al. created an injectable RGD–coupled alginate scaffold–containing Forskolin (FSK), 6-Bromo-methylindirubin-3’oxime (MeBIO), and basic fibroblast growth factor (bFGF) to deliver gingival mesenchymal stem cells (GMSCs) to promote differentiation into skeletal muscle once implanted. These specific growth factors were chosen as they support cell self-renewal and can induce cell differentiation. In comparison to the alginate encapsulated human bone marrow mesenchymal stem cells (hBMMSCs), the alginate encapsulated GMSCs expressed larger amounts of the myogenic markers, MyoG, Myf5, and MyoD, after 4 weeks in vitro indicating that the cells delivered in the alginate scaffold differentiated into mature muscle cells. Both encapsulated hBMMSCs and GMSCs in alginate were implanted subcutaneously in immunocompromised mice. After 8 weeks, the GMSCs encapsulated in alginate had a significantly larger number of cells expressing MF20 and MyoD compared with the hBMMSCs in alginate. In addition, the alginate scaffolds with GMSCs had a significantly larger number of blood vessels compared with the alginate scaffolds containing hBMMSCs. It was concluded that the RGD-alginate scaffolds were able to delivery stem cells, differentiate the stem cells into muscle, and show potential for muscle tissue regeneration [31].
Collagen is a major component of the ECM and its denatured, cost-effective counterpart, gelatin, has also been investigated for skeletal muscle regeneration. Fischer, McGaughey, and Wolyniak combined 10% (w/v) gelatin solutions, 1% microbial transglutaminase (mTG), and 0.02% (v/v) chloroform to created crosslinked hydrogels [32, 33]. One million C2C12 cells were combined with the gelatin solution prior to crosslinking and a 10% static tension applied for 7 days. They found that the cellularized gelatin scaffolds under tension had significantly greater elongated cells with projections compared with the control (Fig. 1). Bettadapur et al. compared micro-molded gelatin hydrogels with micro-printed polydimethylsiloxane (PDMS) scaffolds that were coated with a layer of fibronectin. The gelatin hydrogels had significantly higher C2C12 myotube width, myotube length, and myogenic index 3 weeks after initiating differentiation. They theorize that because these hydrogels have a large amount of protein that more cell adhesion sites become available as the cells remodel or degrade the gelatin hydrogel, but more investigation is need to fully understand this mechanism [1].
In addition to cell delivery, gelatin can also be used for drug delivery. Ma et al. combined osteoactivin (OA), a transmembrane glycoprotein that can prevent atrophy, with gelatin hydrogels prior to implantation in rats [34]. While no muscle formed within the defect, it is possible that a different OA concentration should be used or that it should be delivered with cells to the defect. Hagiwara et al. compared myoblasts, myoblasts with empty gelatin microspheres, and myoblasts with gelatin microspheres containing bFGF on repairing an induced muscular defect, created by removing a bulk sample of muscle from the thigh. While bFGF is commonly used to induce angiogenesis, the authors concluded that combining myoblasts with encapsulated bFGF improved cell survival and promoted muscle regeneration rather than angiogenesis [35].
Keratin promotes cell attachment and growth; however, the body may not possess the proper enzymes to degrade the resulting hydrogel. Tomblyn et al. assessed whether keratose (KOS) hydrogels, oxidation of cysteine residues on human hair, or kerateine (KTN) hydrogels, reduction of cysteine residues, had the ability promote muscle cell maturation and deliver growth factors. KOS hydrogels had significantly more multinucleated human muscle cells compared with Matrigel™, collagen, and uncoated tissue culture polystyrene (TCPS) while KTN hydrogels were only significantly greater compared with uncoated TCPS after 4 days. The KOS hydrogels did degrade quicker and release growth factors faster than the KTN hydrogels [36]. Baker et al. and Passipieri et al. built on this work by combining KTN hydrogels with combinations of IGF-1, bFGF, and muscle precursor cells (MPCs) prior to induced VML injury in either mice or rat TA muscles. Their results determined that KTN hydrogels alone had the same functional outcome as the KTN hydrogel with IGF-1 and bFGF. The authors do conclude that more work is required to better understand how keratin implantation is positively affecting muscle regeneration [16, 37].
Several manuscripts have also combined two or more natural polymers to create hydrogels. Yi et al. combined alginate with gelatin and heparin (Alg-G-H) to form a hydrogel that was then coated with muscle ECM to increase cell adherence. Human skeletal muscle progenitor cells (hSMPCs) were cultured on these hydrogels and assessed for myogenic protein expression and myotube formation. The ECM-coated Alg-G-H hydrogels had enhanced skeletal myogenic protein expression and myotube formation [38]. Ding et al. combined chitosan, β-glycerophosphate, and collagen (C/GP/Co) to form an injectable, thermosensitive hydrogel to carry skeletal muscle satellite cells (SMSCs). In vitro experiments of the C/GP/Co solution with SMSCs had greater cell viability by day 3 compared to the control of collagen type I alone. When myogenic differentiating media was added, the fusion index, the number of nuclei in multinucleate myotubes divided by the total number of nuclei, of the SMSCs on C/GP/Co hydrogels was significantly greater compared to the control. Then, C/GP/Co encapsulated SMSCs were injected dorsally into nude mice and after four weeks, histological analysis showed viable SMSCs with blood vessels. They concluded that the C/GP/Co hydrogel could deliver SMSCs via injection, but more research is needed on differentiation of the SMSCs post-injection [39].
Semi-synthetic Hydrogels
Semi-synthetic hydrogels utilize at least one natural polymer that has been chemically modified with gelatin being a common natural polymer choice for this category of hydrogels [21, 40,41,42,43,44]. Kim et al. showed that C2C12 cellularized gelatin hydroxyphenylpropionic acid (GHPA) hydrogels supported cell proliferation and MHC was expressed indicating maturation into myofibers [41]. Costantini et al. synthesized gelatin methacryloyl hydrogels with elastic moduli ranging from 1 to 10 kPa. C2C12 encapsulated hydrogels with lower elastic moduli showed greater myotube formation compared with ones with higher elastic moduli [21]. Ramón-Azcón et al. combined gelatin methacrylate (GelMA) with carbon nanotubes (CNTs) and exposed the hydrogels to dielectrophoresis (DEP) to create aligned CNTs. C2C12 cells were cultured on groove-ridge patterned GelMA–aligned CNTs, GelMA-random CNTs, and pristine GelMA hydrogels. Sarcomeric actin, MRF4, α-actinin, and myogenin were all significantly higher when cultured on GelMA-aligned CNT scaffolds when exposed to electrical stimulation indicating increased maturation compared with GelMA-random CNTs and pristine GelMA hydrogels with and without electrical stimulation [42].
Hong et al. encapsulated C2C12 cells in GelMA hydrogels and investigated the effects of compression and compression with shear to simulate the effects of deep tissue injuries (DTIs). Their results show that both the level and duration of the strain play a role in C2C12 cell death and should be taken into account for implantation of soft materials focused on regenerating skeletal muscle [43]. Agrawal et al. sandwiched a C2C12 GelMA hydrogel in between two polyacrylamide (PAm) hydrogels that was then anchored between two PAm pillars. Cell alignment and cellular interaction were observed on day 2 with a dense microtissue formed by day 5 and continuation of hydrogel compaction until day 12. C2C12 GelMA hydrogels cultured without the pillars ending up collapsing into a ball of cells by day 5 rather than forming multinucleated myotubes, thus showing that tension on the hydrogel is an important component of muscle development [44].
Hyaluronan and hyaluronic acid have also been investigated for skeletal muscle regeneration. Goldman et al. combined hyaluronic acid and laminin-111 (HA + LMN) to take advantage of the anti-adhesive and anti-inflammatory properties to protect the encapsulated minced muscle tissue once implanted. VML of the TA muscle in rats was created by removing a 6-mm diameter section and then implanting the HA + LMN containing minced muscle graft (MG), the HA + LMN hydrogel with no muscle tissue, or no repair to the defect. Histological analysis showed that the no repair region was filled mostly with ECM, the HA + LMN hydrogel had minimal cellular infiltration and was mostly degraded, and the MG + HA + LMN treated defect had a mixture of regenerated myofibers and ECM [14]. Davoudi et al. combined hyaluronan with methylcellulose (HAMC) as a way to deliver muscle stem cells (MuSCs) after injury to the TA muscle in mice via injection of barium chloride (BaCl2). From their data, they inferred that the HAMC scaffolds may delay MuSC differentiation and allow the proliferation period to occur for longer thus leading to better engraftment [45].
Synthetic Hydrogels
Synthetic only hydrogels are a less popular choice for skeletal muscle tissue engineering compared with natural polymeric hydrogels. Some advantages of synthetic polymers are their tunable degradation and mechanical properties, ease of manufacturing and functionality, high availability, and lower cost. Poly(ethylene glycol) diacrylate (PEGDA), N-isopropylacrylamide (NIPAAm), acrylic acid (AA), and polyacrylamide (PAAm) have all been investigated [22, 23, 27, 46,47,48,49].
Vannozzi et al. combined a low molecular weight PEGDA (575 and 700) layer with a higher molecular weight layer (6,000 and 20,000). The scaffolds underwent self-folding into a tube due to the different mechanical properties and degree of swelling between the layers. A starting size of 2 × 5 mm2 was found to achieve a complete 3D tube. Iron oxide nanoparticles (50 nm diameter) were embedded in the lower PEGDA molecular weight layer to allow for better guidance and control over the folding process using a magnetic field. Since PEGDA does not allow for much cellular attachment, a thin layer of gelatin methacryloyl, Irgacure 2959, fibronectin, and laminin in phosphate buffered saline (PBS) was added and photo-crosslinked to allow for C2C12 attachment prior to folding. After 72 h, C2C12 viability was high and cells displayed a spindle-like morphology. After 20 days, the C2C12 cells had spread and covered the entire tube. The authors conclude that this self-folding PEGDA system is similar to a muscle fascicle and can deliver cells while allowing for nutrient and oxygen exchange [47].
Browe et al. combined PEGDA with AA to form a biocompatible, electroactive hydrogel to be used as an actuator while promoting mature skeletal muscle tissue. Figure 2 shows the actuation of a PEGDA-AA hydrogel before electrical stimulation and after 20 V was applied for 60 s. Hydrogels with a 1:16 ratio of PEGDA to AA swelled to more than 200% of their original size. No significant differences in elastic moduli were measured, but an increase was seen when the overall polymer concentration was increased [27]. These elastic moduli values are similar to ones measured for rat and pig leg muscles [50]. C2C12 cells survived and were metabolically active on 100% PEGDA, 1:4, 1:8, 1:12, and 1:16 PEGDA to AA hydrogels over a 10-day period, but the 1:4 PEGDA:AA hydrogel had significantly greater values. Although there were no significant differences in contractile strength of the PEGDA containing scaffolds, it was determined that AA was necessary for actuation and that as the AA amount increased, so did the contractile strength. Browe et al. successfully created a biocompatible, actuating hydrogel for skeletal muscle where this response was reversible and repeatable [27].
Conductive elements can be added to polymers to act as electrical signals that influence skeletal muscle cell communication and behavior that can be critical to development [23, 49]. Hosseinzadeh et al. combined PAA with the conductive polymer polyaniline (PANi) to form a hydrogel with pores ranging from 20 to 30 μm and an average fiber size of 108 ± 0.009 nm. Mouse muscle satellite cells were more aligned in the patterned PAA-PANi hydrogels compared with non-patterned ones after 10 days of flow perfusion culture [49]. Jo et al. also investigated conductive hydrogels by incorporating graphene oxide (GO) into PAAm. The elastic modulus increased from 18 ± 1 kPa to 54 ± 10 kPa as the amount of GO increased. C2C12 cells were unable to adhere to PAAm hydrogels alone, but when GO was added, the amount of cells increased over 72 h. Conductivity also increased when GO was incorporated and even more so when reduced graphene oxide (rGO) was utilized. The C2C12 cells also matured on the GO/PAAm scaffolds as evidenced by expression of MHC, MyoD, and myogenin. The r(GO/PAAm) scaffolds at 24 h expressed more MyoD, myogenin, and MHC at 7 days when electrically stimulated compared with an unstimulated control [23]. Both Hosseinzadeh et al. and Jo et al. successfully created soft, hydrophilic, and conductive scaffolds that supported skeletal muscle growth.
Xu et al. studied the effect of NIPAAm, AA, and 2-hydroxyethyl methacrylate (HEMA) oligoester on the differentiation of rat bone marrow mesenchymal stem cells (MSCs). Several different compositions of these hydrogels were formulated with the express purpose of delivering MSCs and being able to differentiate the MSCs into muscle tissue. The MSCs grew and differentiated after 14 days in culture, but the highest differentiation amount occurred in the hydrogels with a 20 kPa elastic modulus [48]. In contrast, Villa et al. combined poly(NIPAAm) with HEMA to culture C2C12 cells to form a detachable muscle sheet for implantation. Initially, cell studies showed that three out of the five hydrogels treated with plasma and coated with laminin had cells that exhibited the typically spindle-shaped morphology after 24 h. However, only the hydrogel with the 1.50 HEMA:NIPAAM displayed the best thermoresponsive, optical, and cellular properties. In addition, C2C12 cells cultured on this hydrogel expressed desmin and a muscle cell sheet was successfully detached after 15 min. When the amount of crosslinker used with the 1.50 HEMA:NIPAAM hydrogel was doubled, the time for C2C12 confluence decreased and the detached cell sheet was easier to handle [22]. Thus NIPAAm combined with HEMA can be used as both a cellular delivery device and a manufacturing device.
Composite Hydrogels
For this paper, composite hydrogels are defined as at least one synthetic and one natural polymer making up the hydrogel. Ideally, by combining natural and synthetic polymers into a hydrogel, the best attributes of both can be utilized for skeletal muscle regeneration. Poly(ethylene glycol) (PEG) as the synthetic component of the composite hydrogel is a popular choice [19, 51,52,53,54,55]. For example, Hwang et al. encapsulated bFGF and human adipose-derived stem cells (h-ADSCs) inside a gelatin-PEG-tyramine (GPT) hydrogel. After determining the bFGF release profile and biocompatibility, an in vivo study involving the laceration of a mouse gastrocnemius muscle was completed. The authors found that treatment with GPT, h-ADSCs, and bFGF resulted in low fibrosis, regained muscle contractility, and more regenerated myofibers after 4 weeks [19].
Mulyasasmita et al. utilized protein-PEG hydrogels to deliver human induced pluripotent stem cell-derived endothelial cells (hiPSC-ECs) and vascular endothelial growth factor (VEGF) after an ischemic injury in the gastrocnemius muscle of non-obese diabetic severe combined immune deficient (NOD SCID) mice. After 2 weeks, the muscle tissue showed reduced necrosis and more myofibers compared with delivery of the hydrogel alone or PBS injection as a control [51]. Salimath and García combined PEG with maleimide (MAL) and RGD to increase cellular attachment before crosslinking with a peptide. Viable C2C12 cells cultured on the PEG-MAL-RGD were significantly greater compared with PEG-MAL hydrogels containing RDG, a scrambled sequence of RGD. In addition, cell encapsulated hydrogels were placed into a contractile solution and the change in length was 18.4 ± 2.75% compared with a change in length of 7.2 ± 3.15% for hydrogels placed in PBS as a control [52].
Several authors have investigated PEG combined with fibrinogen (PF) for skeletal muscle regeneration. Fuoco et al. mixed swine muscle-derived pericytes (MP) into the PF hydrogel and immediately added growth medium to support the encapsulated cells. Immunofluorescent staining and Western blotting showed myotube formation and expression of MHC. Cellularized PF constructs were implanted subcutaneously on the back in immunocompromised mice and explanted after 30 days. Histological analysis showed MHC positive myofibers and blood vessels [53]. A follow-up study by Fuoco et al. implanted the PF hydrogels containing mesoangioblasts either into the cavity left after ablation of the TA muscle or subcutaneously on the back. PF hydrogels implanted in both areas resulted in new artificial muscle similar to native muscle [54]. More recently, Constantini et al. 3D printed the PF solution containing C2C12 cells into aligned hydrogel fibers. After 3 weeks, C2C12 cells formed myotubes, expressed MHC and laminin, and underwent sarcomerogenesis. The cellularized PF hydrogel fibers were implanted subcutaneously in the back of immunocompromised SCID mice after culturing in vitro for 7 days. The implants were explanted after 28 days, and histological analysis showed more aligned, striated, and MHC-positive myofibers compared with the cellularized bulk-hydrogel controls [55].
Several synthetic polymers have also been combined with the natural material alginate. Rich et al. combined alginate methacrylate (AM) with PEGDA prior to freeze-drying to make microporous hydrogels with average ice crystal diameters ranging from 20 to 60 μm. AM-PEGDA hydrogels with RGD seeded with primary mouse myoblasts showed proliferation, expression of muscle creatine kinase (MCK), and expression of MHC [24]. Bootsma et al. 3D printed alginate-polyacrylamide hydrogels with mechanical properties specifically for soft tissues like skeletal muscle [17]. Mozetic et al. 3D printed alginate with Pluronic®, a thermoresponsive block copolymer, with C2C12 cells into a tightly packed, aligned hydrogel. After 1 week in differentiating media, the C2C12 cells in 3D-printed hydrogel expressed higher levels of myogenin, α-sarcomeric actin, and MyoD compared with the 2D control [56].
Wang et al. created a nanofiber yarn with a hydrogel core to better emulate skeletal muscle native structure. They combined poly(caprolactone), silk fibroin, and polyaniline (PC/SF/PANI) together to form the nanofiber yarn using a dry-wet electrospinning method. Yarns were placed into poly(dimethylsiloxane) (PDMS) tubes and a poly(ethylene glycol)-co-poly(glycerol sebacate) (PEGS-M) solution was injected inside. After photocrosslinking, each yarn had a hydrogel outer shell surrounding it. C2C12 cells aligned along the direction of the yarn, and after 7 days, the cells expressed MHC [26]. De France et al. combined poly(oligoethylene glycol methacrylate) (POEGMA) and magnetic cellulose nanocrystals (CNCs) to create an injectable hydrogel that crosslinks using hydrazine in situ. C2C12 cells proliferated and spread on the POEGMA-CNC hydrogel surface with and without a magnetic field applied, but the POEGMA-CNC hydrogels with a magnetic field displayed a greater degree of myotube orientation compared with the tissue culture polystyrene (TCPS) control and unaligned hydrogels after 8 days in differentiation media [20].
Conclusions and Future Directions
Skeletal muscle TE aims to regenerate functional muscle tissue after VML injuries that the body is unable to repair. Hydrogels are an attractive option when developing scaffolds for TE as they are an aqueous environment similar to the body and the amount of crosslinking can be tuned for mechanical properties similar to skeletal muscle. In addition, a multitude of fabrication methods can be used including injection, microsphere fabrication, electrospinning, 3D printing, molding, and freeze-drying. As skeletal muscle TE is a newer area of research, researchers are currently investigating a multitude of hydrogels to determine the best material, concentration of polymer, and crosslinking method that can best restore skeletal muscle function. The majority of hydrogel papers had good cellular compatibility and, in some cases, were able to differentiate stem cells into muscle cells and/or induce skeletal muscle maturation. We determined that natural polymers were the most popular choice for making hydrogels comprising 42.5% of the papers reviewed, composite hydrogels made up 25%, synthetic polymer hydrogels made up 17.5%, and semi-synthetic hydrogels were the least common choice at 15%. Composite and semi-synthetic hydrogels have the potential to increase in popularity as it may be possible to combine the advantageous properties of natural hydrogels with those of synthetic ones while reducing or eliminating the disadvantageous ones. Although this review focused on different compositions of hydrogels, mechanical, chemical, and electrical cues also play important roles in the successful development of muscle within or on the hydrogels. Future work should focus on mechanical property analysis and creating larger, more 3D scaffolds that form more mature, aligned skeletal muscle to better match the native skeletal muscle anatomy.
References
Bettadapur A, Suh GC, Geisse NA, Wang ER, Hua C, Huber HA, et al. Prolonged culture of aligned skeletal myotubes on micromolded gelatin hydrogels. Sci Rep. 2016;6:1–14. https://doi.org/10.1038/srep28855.
Guyton AC, Hall JE. Textbook of medical physiology. 11th ed. Philadelphia: Elsevier Saunders; 2006.
Martini F, Nath J, Batholomew E. Fundamentals of anatomy and physiology. 10th ed. San Francisco: Pearson/Benjamin Cummings; 2015.
Marieb EN, Hoehn K. Human anatomy & physiology. 8th ed. San Francisco: Benjamin Cummings; 2010.
Scott JB, Ward CL, Corona BT, Deschenes MR, Harrison BS, Saul JM, et al. Achieving acetylcholine receptor clustering in tissue-engineered skeletal muscle constructs in vitro through a materials-directed Agrin delivery approach. Front Pharmacol. 2017;7. https://doi.org/10.3389/fphar.2016.00508.
Fan C, Jiang P, Fu L, Cai P, Sun L, Zeng B. Functional reconstruction of traumatic loss of flexors in forearm with gastrocnemius myocutaneous flap transfer. Microsurgery. 2008;28(1):71–5. https://doi.org/10.1002/micr.20449.
Vekris MD, Beris AE, Lykissas MG, Korompilias AV, Vekris AD, Soucacos PN. Restoration of elbow function in severe brachial plexus paralysis via muscle transfers. Injury. 2008;39:S15–22. https://doi.org/10.1016/j.injury.2008.06.008.
Baniasadi H, Mashayekhan S, Fadaoddini S, Haghirsharifzamini Y. Design, fabrication and characterization of oxidized alginate-gelatin hydrogels for muscle tissue engineering applications. J Biomater Appl. 2016;31(1):152–61. https://doi.org/10.1177/0885328216634057.
Bach AD, Beier JP, Stern-Staeter J, Horch RE. Skeletal muscle tissue engineering. J Cell Mol Med. 2004;8(4):413–22.
Pollot BE, Rathbone CR, Wenke JC, Guda T. Natural polymeric hydrogel evaluation for skeletal muscle tissue engineering. J Biomed Mater Res B Appl Biomater. 2018;106(2):672–9. https://doi.org/10.1002/jbm.b.33859.
Corona BT, Rivera JC, Owens JG, Wenke JC, Rathbone CR. Volumetric muscle loss leads to permanent disability following extremity trauma. J Rehabil Res Dev. 2015;52(7):785–92. https://doi.org/10.1682/jrrd.2014.07.0165.
Garg K, Ward CL, Hurtgen BJ, Wilken JM, Stinner DJ, Wenke JC, et al. Volumetric muscle loss: persistent functional deficits beyond frank loss of tissue. J Orthop Res. 2015;33(1):40–6. https://doi.org/10.1002/jor.22730.
Grogan BF, Hsu JR. Skeletal trauma Res C. Volumetric muscle loss. J Am Acad Orthop Surg. 2011;19:S35–S7.
Goldman SM, Henderson BEP, Walters TJ, Corona BT. Co-delivery of a laminin-111 supplemented hyaluronic acid based hydrogel with minced muscle graft in the treatment of volumetric muscle loss injury. PLoS One. 2018;13(1). https://doi.org/10.1371/journal.pone.0191245.
Kim JT, Kasukonis BM, Brown LA, Washington TA, Wolchok JC. Recovery from volumetric muscle loss injury: a comparison between young and aged rats. Exp Gerontol. 2016;83:37–46. https://doi.org/10.1016/j.exger.2016.07.008.
Baker HB, Passipieri JA, Siriwardane M, Ellenburg MD, Vadhavkar M, Bergman CR, et al. Cell and growth factor-loaded keratin hydrogels for treatment of volumetric muscle loss in a mouse model. Tissue Eng A. 2017;23(11–12):572−+. https://doi.org/10.1089/ten.tea.2016.0457.
Bootsma K, Fitzgerald MM, Free B, Dimbath E, Conjerti J, Reese G, et al. 3D printing of an interpenetrating network hydrogel material with tunable viscoelastic properties. J Mech Behav Biomed Mater. 2017;70:84–94. https://doi.org/10.1016/j.jmbbm.2016.07.020.
Heher P, Maleiner B, Pruller J, Teuschl AH, Kollmitzer J, Monforte X, et al. A novel bioreactor for the generation of highly aligned 3D skeletal muscle-like constructs through orientation of fibrin via application of static strain. Acta Biomater. 2015;24:251–65. https://doi.org/10.1016/j.actbio.2015.06.033.
Hwang JH, Kim IG, Piao S, Jung AR, Lee JY, Park KD, et al. Combination therapy of human adipose-derived stem cells and basic fibroblast growth factor hydrogel in muscle regeneration. Biomaterials. 2013;34(25):6037–45. https://doi.org/10.1016/j.biomaterials.2013.04.049.
De France KJ, Yager KG, Chan KJW, Corbett B, Cranston ED, Hoare T. Injectable anisotropic nanocomposite hydrogels direct in situ growth and alignment of myotubes. Nano Lett. 2017;17(10):6487–95. https://doi.org/10.1021/acs.nanolett.7b03600.
Costantini M, Testa S, Fornetti E, Barbetta A, Trombetta M, Cannata SM, et al. Engineering muscle networks in 3D gelatin methacryloyl hydrogels: influence of mechanical stiffness and geometrical confinement. Front Bioeng Biotechnol. 2017;5:22. https://doi.org/10.3389/fbioe.2017.00022.
Villa C, Martello F, Erratico S, Tocchio A, Belicchi M, Lenardi C, et al. P(NIPAAM-co-HEMA) thermoresponsive hydrogels: an alternative approach for muscle cell sheet engineering. J Tissue Eng Regen Med. 2017;11(1):187–96. https://doi.org/10.1002/term.1898.
Jo H, Sim M, Kim S, Yang S, Yoo Y, Park JH, et al. Electrically conductive graphene/polyacrylamide hydrogels produced by mild chemical reduction for enhanced myoblast growth and differentiation. Acta Biomater. 2017;48:100–9. https://doi.org/10.1016/j.actbio.2016.10.035.
Rich MH, Lee MK, Marshall N, Clay N, Chen JR, Mahmassani Z, et al. Water hydrogel binding affinity modulates freeze-drying-induced micropore architecture and skeletal myotube formation. Biomacromolecules. 2015;16(8):2255–64. https://doi.org/10.1021/acs.biomac.5b00652.
McKeon-Fischer KD, Rossmeisl JH, Whittington AR, Freeman JW. In vivo skeletal muscle biocompatibility of composite, coaxial electrospun, and microfibrous scaffolds. Tissue Eng A. 2014;20(13–14):1961–70. https://doi.org/10.1089/ten.tea.2013.0283.
Wang L, Wu YB, Guo BL, Ma PX. Nanofiber yarn/hydrogel core-shell scaffolds mimicking native skeletal muscle tissue for guiding 3D myoblast alignment, elongation, and differentiation. ACS Nano. 2015;9(9):9167–79. https://doi.org/10.1021/acsnano.5b03644.
Browe DP, Wood C, Sze MT, White KA, Scott T, Olabisi RM, et al. Characterization and optimization of actuating poly(ethylene glycol) diacrylate/acrylic acid hydrogels as artificial muscles. Polymer. 2017;117:331–41. https://doi.org/10.1016/j.polymer.2017.04.044.
Neal D, Sakar MS, Ong L-LS, Asada HH. Formation of elongated fascicle-inspired 3D tissues consisting of high-density, aligned cells using sacrificial outer molding. Lab Chip. 2014;14(11):1907–16. https://doi.org/10.1039/c4lc00023d.
Matthias N, Hunt SD, Wu JB, Lo J, Callahan LAS, Li Y, et al. Volumetric muscle loss injury repair using in situ fibrin gel cast seeded with muscle-derived stem cells (MDSCs). Stem Cell Res. 2018;27:65–73. https://doi.org/10.1016/j.scr.2018.01.008.
Marcinczyk M, Elmashhady H, Talovic M, Dunn A, Bugis F, Garg K. Laminin-111 enriched fibrin hydrogels for skeletal muscle regeneration. Biomaterials. 2017;141:233–42. https://doi.org/10.1016/j.biomaterials.2017.07.003.
Ansari S, Chen C, Xu XT, Annabi N, Zadeh HH, Wu BM, et al. Muscle tissue engineering using gingival mesenchymal stem cells encapsulated in alginate hydrogels containing multiple growth factors. Ann Biomed Eng. 2016;44(6):1908–20. https://doi.org/10.1007/s10439-016-1594-6.
Chen P-Y, Yang K-C, Wu C-C, Yu J-H, Lin F-H, Sun J-S. Fabrication of large perfusable macroporous cell-laden hydrogel scaffolds using microbial transglutaminase. Acta Biomater. 2014;10(2):912–20.
Paguirigan AL, Beebe DJ. Protocol for the fabrication of enzymatically crosslinked gelatin microchannels for microfluidic cell culture. Nat Protoc. 2007;2(7):1782–8.
Ma J, Baker AR, Calabro A, Derwin KA. Exploratory study on the effect of osteoactivin on muscle regeneration in a rat volumetric muscle loss model. PLoS One. 2017;12(4). https://doi.org/10.1371/journal.pone.0175853.
Hagiwara K, Chen G, Kawazoe N, Tabata Y, Komuro H. Promotion of muscle regeneration by myoblast transplantation combined with the controlled and sustained release of bFGFcpr. J Tissue Eng Regen Med. 2016;10(4):325–33. https://doi.org/10.1002/term.1732.
Tomblyn S, Kneller ELP, Walker SJ, Ellenburg MD, Kowalczewski CJ, Van Dyke M, et al. Keratin hydrogel carrier system for simultaneous delivery of exogenous growth factors and muscle progenitor cells. J Biomed Mat Res B. 2016;104(5):864–79. https://doi.org/10.1002/jbm.b.33438.
Passipieri JA, Baker HB, Siriwardane M, Ellenburg MD, Vadhavkar M, Saul JM, et al. Keratin hydrogel enhances in vivo skeletal muscle function in a rat model of volumetric muscle loss. Tissue Eng A. 2017;23(11–12):556−+. https://doi.org/10.1089/ten.tea.2016.0458.
Yi HL, Forsythe S, He YY, Liu Q, Xiong G, Wei SC, et al. Tissue-specific extracellular matrix promotes myogenic differentiation of human muscle progenitor cells on gelatin and heparin conjugated alginate hydrogels. Acta Biomater. 2017;62:222–33. https://doi.org/10.1016/j.actbio.2017.08.022.
Ding K, Yang Z, Zhang YL, Xu JZ. Injectable thermosensitive chitosan/−glycerophosphate/collagen hydrogel maintains the plasticity of skeletal muscle satellite cells and supports their in vivo viability. Cell Biol Int. 2013;37(9):977–87. https://doi.org/10.1002/cbin.10123.
Pepelanova I, Kruppa K, Scheper T, Lavrentieva A. Gelatin-Methacryloyl (GelMA) hydrogels with defined degree of functionalization as a versatile toolkit for 3D cell culture and extrusion bioprinting. Bioengineering. 2018;5(3):55.
Kim MJ, Shin YC, Lee JH, Jun SW, Kim C-S, Lee Y, et al. Multiphoton imaging of myogenic differentiation in gelatin-based hydrogels as tissue engineering scaffolds. Biomater Res. 2016;20:2. https://doi.org/10.1186/s40824-016-0050-x.
Ramon-Azcon J, Ahadian S, Estili M, Liang X, Ostrovidov S, Kaji H, et al. Dielectrophoretically aligned carbon nanotubes to control electrical and mechanical properties of hydrogels to fabricate contractile muscle myofibers. Adv Mater. 2013;25(29):4028–34. https://doi.org/10.1002/adma.201301300.
Hong Y, Yao Y, Wong S, Bian L, Mak AFT. Change in viability of C2C12 myoblasts under compression, shear and oxidative challenges. J Biomech. 2016;49(8):1305–10. https://doi.org/10.1016/j.jbiomech.2016.03.014.
Agrawal G, Aung A, Varghese S. Skeletal muscle-on-a-chip: an in vitro model to evaluate tissue formation and injury. Lab Chip. 2017;17(20):3447–61. https://doi.org/10.1039/c7lc00512a.
Davoudi S, Chin C-Y, Cooke MJ, Tam RY, Shoichet MS, Gilbert PM. Muscle stem cell intramuscular delivery within hyaluronan methylcellulose improves engraftment efficiency and dispersion. Biomaterials. 2018;173:34–46. https://doi.org/10.1016/j.biomaterials.2018.04.048.
Cha SH, Lee HJ, Koh W-G. Study of myoblast differentiation using multi-dimensional scaffolds consisting of nano and micropatterns. Biomater Res. 2017;21(1):1. https://doi.org/10.1186/s40824-016-0087-x.
Vannozzi L, Yasa IC, Ceylan H, Menciassi A, Ricotti L, Sitti M. Self-folded hydrogel tubes for implantable muscular tissue scaffolds. Macromol Biosci. 2018;18(4):1700377. https://doi.org/10.1002/mabi.201700377.
Xu Y, Li Z, Li X, Fan Z, Liu Z, Xie X, et al. Regulating myogenic differentiation of mesenchymal stem cells using thermosensitive hydrogels. Acta Biomater. 2015;26:23–33. https://doi.org/10.1016/j.actbio.2015.08.010.
Hosseinzadeh S, Rezayat SM, Giaseddin A, Aliyan A, Soleimani M. Microfluidic system for synthesis of nanofibrous conductive hydrogel and muscle differentiation. J Biomater Appl. 2018;32(7):853–61. https://doi.org/10.1177/0885328217744377.
McKeon-Fischer KD, Flagg DH, Freeman JW. Coaxial electrospun poly(epsilon-caprolactone), multiwalled carbon nanotubes, and polyacrylic acid/polyvinyl alcohol scaffold for skeletal muscle tissue engineering. J Biomed Mater Res A. 2011;99A(3):493–9. https://doi.org/10.1002/jbm.a.33116.
Mulyasasmita W, Cai L, Dewi RE, Jha A, Ullmann SD, Luong RH, et al. Avidity-controlled hydrogels for injectable co-delivery of induced pluripotent stem cell-derived endothelial cells and growth factors. J Control Release. 2014;191:71–81. https://doi.org/10.1016/j.jconrel.2014.05.015.
Salimath AS, García AJ. Biofunctional hydrogels for skeletal muscle constructs. J Tissue Eng Regen Med. 2016;10(11):967–76. https://doi.org/10.1002/term.1881.
Fuoco C, Sangalli E, Vono R, Testa S, Sacchetti B, Latronico MV, et al. 3D hydrogel environment rejuvenates aged pericytes for skeletal muscle tissue engineering. Front Physiol. 2014;5:203. https://doi.org/10.3389/fphys.2014.00203.
Fuoco C, Rizzi R, Biondo A, Longa E, Mascaro A, Shapira-Schweitzer K, et al. In vivo generation of a mature and functional artificial skeletal muscle. Embo Mol Med. 2015;7(4):411–22. https://doi.org/10.15252/emmm.201404062.
Costantini M, Testa S, Mozetic P, Barbetta A, Fuoco C, Fornetti E, et al. Microfluidic-enhanced 3D bioprinting of aligned myoblast-laden hydrogels leads to functionally organized myofibers in vitro and in vivo. Biomaterials. 2017;131:98–110. https://doi.org/10.1016/j.biomaterials.2017.03.026.
Mozetic P, Giannitelli SM, Gori M, Trombetta M, Rainer A. Engineering muscle cell alignment through 3D bioprinting. J Biomed Mater Res A. 2017;105(9):2582–8. https://doi.org/10.1002/jbm.a.36117.
Funding
Dr. Fischer, Mr. McGaughey, and Dr. Wolyniak would like to acknowledge the Virginia Academy of Sciences for their Small Research Project Grant.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fischer, K.M., Scott, T.E., Browe, D.P. et al. Hydrogels for Skeletal Muscle Regeneration. Regen. Eng. Transl. Med. 7, 353–361 (2021). https://doi.org/10.1007/s40883-019-00146-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-019-00146-x