Abstract
Suicide is the second leading cause of death among youth aged 10–25 years and approximately 1-in-6 adolescents reported serious suicidal ideation in the past year. Schools are a unique environment in which to identify and respond to youth suicide risk. Although there are screening tools for identifying which youth are at risk and assessment measures for establishing the severity of suicide risk, an essential aspect of risk management is excluded: monitoring youth suicide risk. It is likely that this gap exists because most of the development and research on screening and assessment is in settings such as outpatient mental health clinics or hospitals where routine monitoring is difficult. The Suicide Risk Monitoring Tool (SMT) was developed so that school mental health professionals could quickly track changes in youth already identified at-risk for suicide, including youth who are assessed but remain in school, or those who are re-entering school after a hospitalization. The SMT includes factors known to correlate with youth suicide risk. This paper will review the research on suicide screening and risk assessment, identify and describe the empirical and theoretical basis for the SMT, relate monitoring to the comprehensive risk assessment within a school’s overall framework for suicide risk assessment procedures, and provide a detailed case study that demonstrates how the SMT can be used with students in a school setting. Implications for research and practice are included.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
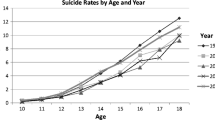
Suicide is the second leading cause of death among youth aged 10–25 years and approximately 1-in-6 adolescents reported serious suicidal ideation in the past year (Centers for Disease Control and Prevention 2017; Kann et al. 2016). Although rates of suicidal ideation and attempt are unknown in elementary-aged youth, national surveys suggest rates of ideation are highest among middle school students (19.6 per 100,000), and suicide attempts and death are highest among high school students (Centers for Disease Control and Prevention 2017; Kann et al. 2016). Rates of suicidal ideation and planning, but not suicide attempt, increased among high school students between 2009 and 2015 (Kann et al. 2016).
Schools are an ideal setting in which to identify and respond to youth suicide risk. Students spend more waking hours in schools than any other setting, including home. Students are in contact with peers, staff, and skilled mental health professionals, all of whom can be trained to identify and respond to youth suicide risk. Indeed, the President’s New Freedom Commission on Mental Health stated that identifying and assessing youth suicide risk was an essential function of schools (Mills et al. 2006). Nearly half of youth identified at risk for suicide are identified in schools, compared to 16% for community mental health agencies, 4.3% for juvenile justice settings, 2.7% for hospitals, and 1.9% for police (Stiffman et al. 2004). Recent research using data from the Garrett Lee Smith Memorial suicide prevention grants found that identification and referral reduce suicide attempts and death (Condron et al. 2015; Garraza et al. 2015; Walrath et al. 2015). School staff who received longer gatekeeper trainings were more successful identifying and referring youth to services (Condron et al. 2015).
Despite the risk that suicide poses and the evidence that suicide prevention programs save lives, school mental health professionals and administrators face a daunting task when it comes to addressing suicide risk in the schools, including time constraints, limited research, and entrenched myths. Even when administrators are able to carve out the time needed for school mental health professionals to receive specialized training, much of the research on identifying and intervening with suicidal youth has been conducted primarily in medical settings (e.g., primary care, emergency departments, or inpatient settings), or community mental health, rather than school settings. For example, most of the research on universal screening, which has been shown to be a safe and effective way of identifying youth at risk for suicide (Gould et al. 2005; Scott et al. 2010), has been done in hospital and primary care settings (see Horowitz et al. 2009 for a review; Wintersteen 2010). Further, parents and professionals alike believe the myth that screening for suicide risk will make kids want to kill themselves (Erbacher et al. 2015; Joiner 2011), despite research that has shown that asking students about suicide does not increase suicide risk (i.e., there is no iatrogenic effect of screening, Gould et al. 2005).
Suicide Risk Screening and Assessment
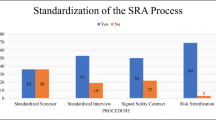
The current standard for identifying and responding to suicide risk is screening followed by a suicide risk assessment. Universal screening involves asking all youth a few questions about suicide risk. For example, the Columbia-Suicide Severity Rating Scale brief screener for schools (http://cssrs.columbia.edu/documents/c-ssrs-screener-triage-schools/) asks about suicidal ideation and attempt in the past month or year. Youth who answer “yes” to past-month suicidal ideation or attempt are referred for a more comprehensive suicide risk assessment (SRA). The more comprehensive assessment is necessary for several reasons: (1) all screeners (not just those for suicide) will misidentify some youth as suicidal who are not (i.e., false positive) and the SRA provide data as to a youth’s actual risk (Eack et al. 2008); (2) a comprehensive SRA will provide information about level of risk and provide support for decisions to maintain the youth in the community or refer to a hospital.
Best practice recommendations for youth SRA includes assessing for suicidal ideation, intent, and planning; identifying risk factors, warning signs, and protective factors; identifying lethal means; assessing the guardians’ capacity to provide an emotionally and physically safe environment; and gathering information from multiple sources including parents, teachers, and other collateral contacts (Barrio 2007; Erbacher et al. 2015; Ribeiro et al. 2013). Although the SRA is essentially atheoretical, there has been growing empirical support for assessing the three constructs in Joiner’s Interpersonal Theory of Suicide: thwarted belonging, burdensomeness, and acquired capacity (Joiner 2007; Ribeiro et al. 2013).
The majority of suicide screening and SRA protocols have been developed for hospitals or community mental health centers, not schools. These protocols assume access to resources (including family members, medical records, and more time than is typically available to school-based mental health professionals), exclude information (such as school-specific stressors like standardized testing or social events) that is essential to suicide risk assessment in schools, and assume that youth are residential (e.g., hospitals) or are seen weekly (e.g., outpatient therapy) rather than daily as is possible in a school setting. Despite these limitations, most schools have adopted the screen–assess protocol with established screeners such as the Columbia-Suicide Severity Rating Scale brief screener for schools (http://cssrs.columbia.edu/documents/c-ssrs-screener-triage-schools/) and Erbacher et al.’s (2015) suicide risk assessment protocol. In some cases, one school staff member might do the screening and refer the comprehensive risk assessment to a school-based mental health professional, a mobile crisis support person, or refer directly out to an outpatient therapist, crisis center, or psychiatric hospital. In other cases, the school mental health professional completes both the screening and the assessment.
The Gap in Managing Suicide Risk
Recent research suggests that the screen–assess model leaves a gap in managing suicide risk. While many elements of a suicide attempt are planned in advance (Smith et al. 2008), research on adult suicide attempt survivors found that the final details, including identifying a method and where/when the suicide would occur, most often occurred just days or hours prior to the suicide attempt (Kleiman et al. 2017; Millner et al. 2017). Suicidal thoughts and behaviors are episodic as they ebb and flow (Erbacher et al. 2015); with episodes for adolescents fluctuating more rapidly than for adults (Pisani et al. 2016). Mental health clinicians therefore need an effective way to monitor the fluid nature of suicide risk and uncover increasing fluctuations before a suicidal crisis or attempt occurs (Erbacher et al. 2015; Millner et al. 2017). Further, information on fluctuations in risk is clinically valuable and can be shared among the systems with which the youth is involved, including community mental health, hospitals, juvenile court, and child welfare.
Development of the Suicide Monitoring Tool
In order to address the gap in the suicide prevention continuum, the authors (TAE and JBS) developed a suicide monitoring tool (SMT) specifically designed for use in school settings and shareable across service delivery systems. Screeners are not intended to be used with youth already at risk for suicide, and it is impractical and excessive to conduct multiple comprehensive SRAs with the same youth in a short period of time. The SMT is neither a screening tool like the C-SSRS screener nor a comprehensive suicide risk assessment. Screeners like the C-SSRS brief screener ask about past month and past year ideation and attempt; they identify youth who would benefit from a comprehensive suicide risk assessment. Screeners are not useful in collecting and tracking clinically relevant information with youth who are already at known risk for suicide. For example, the C-SSRS screener is designed to be administered by an adult no more than once-a-month. Even if industrious school professionals engaged in “off-label” use of the C-SSRS (which nullifies the C-SSRS’s psychometric evaluations), it does not provide clinically useful information such as reasons for living, sources of support, and Joiner’s concepts of burdensomeness and belonging. On the other hand, comprehensive SRAs are not designed to be completed quickly nor track short-term changes in suicide risk.
The SMT fills the gap between brief screeners and comprehensive SRAs. It is intended to be used with youth already identified at risk for suicide, such as youth who reported thoughts of suicide but were deemed safe to remain in the community or youth returning to school after a hospitalization. It is a brief (3–5-minute) self- or staff-administered tool that gathers data on suicidal ideation, intent, plan, protective factors, and incorporates key concepts related to suicide. The SMT is designed so that information can be graphed in order for changes in suicide risk to be quickly identified. In the case of unexpected increases in risk, the SMT will alert the professional so they can initiate appropriate intervention and referral. In cases where youth are involved in multiple systems, the SMT enables school staff to quickly gather information that can be shared and understood by providers in other systems. The development of a risk monitoring tool that can quickly identify changes in suicide risk and be shared across service delivery systems meets the first goal of the Revised National Strategy for Suicide Prevention (2012), which is to integrate and coordinate suicide prevention activities across multiple sectors and settings. The SMT is also consistent with recent research noted above which found that suicidal ideation can fluctuate significantly within a matter of hours (Kleiman et al. 2017). The SMT is an important advance in gathering and sharing potentially life-saving information across sectors and settings. Next, we briefly describe the SMT and the relevant conceptual and empirical support.
Ideation
The first section asks if the student is having thoughts of suicide, and if so when (four options including “right now”, “past 24 hour”, “past week” and “past month.”). We also assess for frequency, duration, and intensity. We included the timeframe for suicide risk for several reasons: (1) It is impossible to monitor changes without gathering information on when ideation occurs; (2) The most widely used protocol for assessing ideation and intent—Shea’s Chronological Assessment of Suicide Events (CASE; Shea 2002) uses these timeframes in assessment; and (3) Recent research on adults indicated that the intensity of suicidal ideation fluctuates significantly over the course of a day (Kleiman et al. 2017). Frequency, duration, and intensity are standard concepts used in establishing diagnostic categories, such as those in the DSM-5 (American Psychiatric Association 2013).
Intent
We ask how much the student wants to live and die on a five-point scale. This question acknowledges and assesses the ambivalence of suicide, which is the contradiction that part of you wants to live and part of you wants to die. Monitoring changes in the degree to which a student wants to live or die is essential to understanding risk for suicide. Prior research has found that people with intense suicidal ideation but low or no intent are at low risk for suicide (Joiner et al. 2003). Our use of a five-point scale is consistent with best practice recommendations that encourage the use of a scale to measure intent (Chu et al. 2015), and a developmentally appropriate elementary school three-point version of the scale is also available.
Plan
This section gathers information on plan, including writing a note, identifying and having access to the method and whether or not the student has made a recent attempt. Despite the media’s fascination with suicide notes, approximately 70% of people do not leave notes, and the majority of those who do are adults not youth. People who leave notes are different from most people who die of suicide (Stack and Rockett 2016). Compared to adult notes, which tend to be more functional when written by men (e.g., “my will is located in the top file cabinet drawer in the basement”) and tend to express more hopelessness and failure when written by women (Lester and Leenaars 2016), youth notes also express love for others and express vindictiveness (Freuchen and Grøholt 2015). The advent of social media, however, has changed the way we use and understand suicide notes (Barrett et al. 2016). A text, Facebook post, or tweet could serve as a suicide “note” in that it provides a final documentation of intent prior to the death (Chhabra and Bryant 2016). If a student indicates that they have written a note, providers should find out if they used traditional media (e.g., paper) or new media (e.g., text).
Assessing for method is key in monitoring suicide risk (Shea 2017). For example, if a student’s response to the question “have you identified a method” changes from “no” to “yes,” that would indicate an increase in risk. Identifying the specific method enables the provider to engage in means restriction, which is suggested for any suicidal adolescent, particularly with regard to firearms (Brent et al. 1993). Finally, we include a single question to ask about a recent attempt. Research by Hom et al. (2016) suggested that assessing for prior attempt using a single survey question might be misleading. Therefore, if a student checks “yes” to this question, providers should follow up and ask more questions about the nature of the attempt, including lethality, timeframe, and desire to attempt again using the same method. Even though the SMT is intended for repeated use, repeated “yes” answers could refer to the same past incident, or it could refer to a new attempt and should be queried further.
Warning Signs
Warning signs are indicators of immediate risk. Student answers to prior questions about ideation, intent, and plan can serve as warning signs. Additionally, we ask students about hopelessness, burdensomeness, sadness, and disconnection. Hopelessness and sadness are symptoms of depression, and burdensomeness and disconnection are two of three required states in Joiner’s Interpersonal Theory of Suicide (Joiner 2007). Feeling like a burden and not feeling like you belong (i.e., disconnection) are short-term predictors of increased suicide risk in adults (Kleiman et al. 2017).
Protective Factors
In the final section, we ask students about protective factors, including their reasons for living (Miller et al. 2007), people whom they identify as support (Stanley and Brown 2012), and a final question, “What could change about your life that would make you no longer want to die?” These three questions lead to a mini safety plan for the student, though providers should follow up to get more detailed information about how and when students would use the resources listed. Elements of a comprehensive safety plan, identified as an effective best practice stand-alone intervention to mitigate suicide risk, can be found in Stanley and Brown (2012).
Instructions for Providers
The back page of the SMT is a checklist of actions that providers should take after reviewing the content of the monitoring tool, including establishing current level of risk, contacting parents/guardian, removing means, etc.
In conclusion, the SMT is intended to be used with youth already known to be at risk for suicide. Although some of the questions and categories are the same as providers will find in screening and assessment, the SMT serves a different purpose; it tracks changes in key domains of risk, identifies protective factors, and facilitates continuity of care with collaborating agencies. In the next section, we will demonstrate how data gathering and graphing work with the SMT.
Case Study: Using the SMT as Part of Comprehensive Suicide Prevention in Schools
Tianna had trouble making friends after transferring into a new school junior year. Despite being an honor roll student and athlete, she quickly earned a reputation of being a flirt and a liar. Tianna’s boyfriend of six months, Kyle, was part of her reason for transferring to this particular school. While he loved her, Kyle often got frustrated with Tianna’s behaviors. Tianna always seemed to seek admiration and want to be the center of attention, whether in class, during sports, or at parties. Their relationship could be described as rocky, at best.
Tianna first came to the attention of the school guidance department as a referral from her special education teacher who noted that Tianna seemed to suffer from “emotional distress.” Tianna met criteria for an individualized education plan (IEP) as an emotionally disturbed student. At intake, Tianna reported that she had been admitted to partial hospitalization for three weeks the year prior (October of tenth grade) due to suicidal thoughts after the death of her uncle. Tianna identified that a major life stressor at that time was a concussion that resulted in her no longer being able to play basketball. She had always identified as an athlete and her closest friends had been her teammates, who were continuing to bond without her since she could no longer play. She also reported that she had previously been in an abusive relationship throughout much of ninth grade. Tianna had therefore received individual counseling since ninth grade along with ongoing family therapy and monthly psychiatry appointments. Treatment methods have included cognitive-behavioral therapy as well as eye movement desensitization and reprocessing (EMDR) due to the trauma of her abusive relationship. Her current medication regime included Zoloft and Abilify, though she was admittedly inconsistent in taking them as prescribed, expressing that she could not drink alcohol while on them. Tianna reported having been diagnosed with anxiety and depression as well as trichotillomania. She continues to have no eyebrows or eyelashes. She has a history of nonsuicidal self-injury (NSSI): cutting or scratching herself multiple times weekly. This was particularly concerning for Tianna as NSSI can be a contributing factor toward building capacity for suicide (Joiner 2007; Klonsky et al. 2013). Positively, Tianna is currently achieving strong grades and has returned to the basketball team as a star athlete in her new school. Tianna also started a new anti-bullying campaign on campus, advocating for those who are vulnerable.
While Tianna shared all of the above with the examiner, rapport had initially been difficult to establish. Tianna immediately reported that she did not trust counselors. The counselor validated Tianna’s distrust, saying “I understand. You have no reason to trust me. But I’m going to do everything I can to earn your trust. Is there anything you’d like to ask me?” After spending the time needed to build a therapeutic alliance, the counselor gently asked Tianna to talk about her prior suicidal ideation. In addition to being a useful way to gather information, having students talk about previous suicidal crises eases them into disclosing current thoughts and behaviors in real time. As her apprehension with trust was explored further, Tianna disclosed that she was afraid of being sent to the hospital. Tianna then shared what happened late last year:
Tianna: I understand I needed partial hospitalization in October; my suicidal thoughts were strong. But, in April, I made the mistake of telling a friend that I was just thinking about suicide. I got called down to the guidance office and the guidance counselor freaked out. She barely asked me any questions, but told me she was calling my mother and I had to go to the hospital. I had been to the hospital before—once—when I ASKED to go. I knew I didn’t need it this time. But, the counselor didn’t listen and she sent me anyway. It was awful. I didn’t dare to mention my thoughts again.
Tianna lost her trust when the counselor recommended a more restrictive setting than Tianna thought she needed. While Tianna had some suicidal thoughts at that time, they were consistent with her own baseline. The hospital also noted this and she was not admitted after waiting for nearly seven hours to see a psychiatrist. Tianna expressed frustration at feeling the counselor just reacted without fully understanding Tianna’s mental state at that time. Tianna felt that the counselor just wanted to make sure she wasn’t liable for anything and Tianna felt the counselor did not act in her best interest.
In order to better understand her current state, the school social worker and school psychologist conducted a comprehensive SRA. After spending two and a half hours with Tianna, the SRA team determined that Tianna was again at high risk for suicide. During the SRA, Tianna disclosed that she planned to take an overdose of pills (which she had access to) and identified the time and place in which she intended to take them. Tianna’s parents were notified and they transported her to a local adolescent psychiatric hospital. During her seven-day hospitalization Tianna received milieu group, individual therapy sessions, medication review by the psychiatrist, and one family therapy session. Rather than being discharged immediately back into the community, a step-down procedure allowed Tianna to transition from the hospital to partial hospitalization, which she attended for ten school days. After missing three full weeks of school, Tianna transitioned back to school and a re-entry meeting was conducted. At this meeting, a change in medication was noted as Tianna had additionally been prescribed Lexapro for her trichotillomania. Her follow-up plan included intensive outpatient therapy (IOP) four days a week after school from 3:00 PM to 5:00 PM along with psychiatrist appointments on Friday afternoons and family-based services on Saturday mornings; insurance did not allow for more than one mental health appointment in any given day. Tianna decided to openly share with her teachers and peers that her absences were due to “depression and anxiety,” which she felt was an easier response than making something up to cover the truth. She then began attending classes.
As part of the re-entry meeting, it was agreed that Tianna’s suicide risk would be monitored by the school psychologist on a frequent basis, who would collaborate with the school team and Tianna’s community-based mental health professionals as needed. The Suicide Monitoring Tool (Erbacher et al. 2015) was first completed on April 30th, the day of re-entry back to school, in order establish current risk and a baseline. The SMT is constructed so that higher scores indicate higher risk for suicide.
As illustrated in Fig. 1, Tianna’s highest scores were “lack of connection” and “parental relationship.” When asked about this, she told the counselor that she did not feel connected to her new teammates and missed the bonds she felt with her old teammates. Tianna also described ongoing tumultuous relationships with both parents, believing that she could never do right by them, and that “nothing was ever good enough.” Because parental relationships were identified in the first meeting as strongly related to her suicidal thoughts, we included it on the form as an individualized stressor. At school, interventions were implemented including getting Tianna involved in the school’s spirit club to establish connections, providing support for her anti-bullying efforts to build her sense of purpose, providing a tutor from the National Honor Society to catch her up on school work, and meeting with the school psychologist to work on cognitive-behavioral strategies focusing on her anxiety and decreasing her negative thought patterns. It was also determined that Tianna’s suicidal thoughts and behaviors would be monitored daily, particularly throughout the first four weeks upon her return to school from hospitalization as this is a particularly high risk time (Kleiman et al. 2017). Over the next few weeks, Tianna’s SMT scores were relatively unchanged.
On the morning of May 15th, Tianna came into the guidance office reporting significant stress due to the expectations of her Honors course load and the demands of making up work she missed when hospitalized, even though teachers were asked to require only the “essential” material (similar to the school’s concussion policy). Tianna expressed concern with making up missed assignments and keeping up with new assignments while attending therapy 6 days per week and managing the side effects of medication (exhaustion and nausea). While it was clear that she was stressed (she had said as much), she did not volunteer that she was having more frequent thoughts of suicide. As illustrated in Fig. 2, that morning’s SMT indicated a two point increase in the frequency of suicidal ideation and a one point increase in lack of connection, and sadness and depression.
Tianna shared with the counselor that she was feeling stressed and overwhelmed about school. The school team (which included the school social worker, school psychologist, nurse, principal, and vice principal) agreed that Tianna would attend her morning classes, Honors Chemistry and Honors History, and would check in with the counselor after lunch. As illustrated in Fig. 3, Tianna’s post-lunch SMT scores were much higher than they were that morning.
The benefits of charting were clear when Tianna’s mental health team saw the rapid escalation in her suicidal thoughts and behaviors (Kleiman et al. 2017). As seen in Fig. 3, the levels of stress she was experiencing with school work (specifically the demands of her morning honors classes), continued familial discord, and unrelenting feelings of disconnection were of significant concern. By the time she finished lunch, Tianna was considering a suicide plan with stated intent to carry out her plan that evening when her parents went out to dinner. By attending to Tianna’s expressed overwhelm and monitoring her suicidal thoughts and behaviors again within hours, the team was able to uncover the rapid increase in her suicide intent and plan. Because of her history of suicidal thoughts and the increased ratings, the team met with Tianna and her parents to discuss returning to the hospital for evaluation and another round of inpatient treatment. Tianna’s agreed that she could not be safe in the community and needed a higher level of care. Tianna was admitted for five days, followed by two more weeks in a partial hospital.
Due to school policy, school administrators came to the team noting that Tianna could not attend prom because of her absences, and could not walk in graduation because of her incompletes. The school psychologist, however, was able to argue that Tianna was diligent in attending the partial hospital’s school program and that Tianna was an Honor student who had proven herself academically throughout her high school career. While she would not yet receive her diploma, administrators allowed Tianna to walk in graduation if she agreed to attend school in the summer with the resource room teacher (funding was found to finance this option) until all of her work was finished. Tianna successfully completed her work, earned her diploma, and attended the college of her choice with a major in Accounting.
Case Study: Appendix
Data above show real-time suicidal thoughts and behaviors for Tianna, and the SMT allowed school professionals to uncover the dramatic spike in her suicidal thoughts and behaviors that occurred quickly (within hours). The SMT can be used to show trends in suicide risk by graphing data over time and allows clinicians to catch even subtle changes early. As illustrated in Fig. 4, frequency, duration, and intensity of Tianna’s suicidal thoughts waxed and waned, as is common, until May 15th (session 13) when there was a significant increase in intent (see Fig. 3) and the team decided she would be safest in the hospital.
Figure 4 also provides insight into the nature of Tianna’s suicidal ideation. Although she continued to have frequent thoughts of suicide, the duration and intensity of those thoughts decreased. This information is invaluable for school personnel and collateral contacts. Figures 1, 2, 3, and 4 were created with a fillable Excel spreadsheet created by Erbacher et al. (2015), and available on the eResource page of the Routledge website. The spreadsheet makes graphing data simple and it can be done in any of the assessment categories included on the SMT. Graphing makes it easy to see fluctuations in real-time and provides rationale for starting, stopping, or continuing an intervention. For example, Tianna’s “Parent Relationship” score remained high, which provided her community-based therapist a rational for keeping it as a focus of treatment. And, when this worsened on the SMT, the school-based professional was readily able to communicate with Tianna’s outside therapist (a release of information was signed by her parents) in order to share concerns and alter treatment goals, allowing for a collaborative team approach. Her outside therapist would also extend Tianna’s therapy appointments at these times. Through frequent monitoring, Tianna became more aware of her own triggers and feelings. Although not an explicit goal of the form, the team hoped that Tianna would learn to recognize her triggers and be able to independently seek help when needed.
Summary: Applications and Future Directions
The Suicide Monitoring Tool was developed to fill a gap in managing suicide risk. In this case study, a screening tool would have been insufficient as Tianna had already been identified as being at risk for suicide. Likewise, a comprehensive suicide risk assessment would have been excessive, time consuming, and would not have been easy to graph and track. Frequent monitoring can help practitioners uncover changes in a student’s suicidal thoughts and behaviors before reaching crisis levels. Though Tianna required re-hospitalization, in many cases frequent monitoring of suicidal thoughts can prevent the need for future hospitalizations as increasing thoughts can be caught early. The SMT can be used with any child or adolescent presenting with suicidal thoughts or behaviors and both an elementary/middle and high school form exist. Optimally, the form is administered frequently and shared with outside mental health professionals. Once a student stabilizes, frequency of SMT administration can be decreased to biweekly, then monthly through the end of the school year. Administering again at the beginning of the following school year is suggested in order to ensure no triggers and increased suicidal thoughts occurred over summer months.
Future directions include schools ensuring protocols and administrative directives include set procedures for suicide screening, assessment, and risk monitoring along with safety planning and collaboration with community mental health. The SMT currently lacks scale validation and data regarding user satisfaction, ease of use, and reliability and validity.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington: American Psychiatric Association.
Barrett, J. R., Shetty, H., Broadbent, M., Cross, S., Hotopf, M., Stewart, R., & Lee, W. (2016). “He left me a message on Facebook”: comparing the risk profiles of self-harming patients who leave paper suicide notes with those who leave messages on new media. BJ Psych Open, 2(3), 217–220. https://doi.org/10.1192/bjpo.bp.116.002832.
Barrio, C. A. (2007). Assessing suicide risk in children: guidelines for developmentally appropriate interviewing. Journal of Mental Health Counseling, 29(1), 50–66.
Brent, D. A., Perper, J. A., Moritz, G., Baugher, M., Schweers, J., & Roth, C. (1993). Firearms and adolescent suicide: a community case-control study. American Journal of Diseases of Children, 147(10), 1066–1071. https://doi.org/10.1001/archpedi.1993.02160340052013.
Centers for Disease Control and Prevention. (2017). Web-based Injury Statistics Query and Reporting System (WISQARS) (Fatal Injury Reports, 1999–2015, for National, Regional, and States [RESTRICTED]). National Center for Injury Prevention and Control. Retrieved from http://webappa.cdc.gov/cgi-bin/broker.exe
Chhabra, N., & Bryant, S. M. (2016). Snapchat toxicology: social media and suicide. Annals of Emergency Medicine, 68(4), 527. https://doi.org/10.1016/j.annemergmed.2016.05.031.
Chu, C., Klein, K. M., Buchman-Schmitt, J. M., Hom, M. A., Hagan, C. R., & Joiner, T. E. (2015). Routinized assessment of suicide risk in clinical practice: an empirically informed update. Journal of Clinical Psychology, 71(12), 1186–1200. https://doi.org/10.1002/jclp.22210.
Condron, D. S., Garraza, L. G., Walrath, C. M., McKeon, R., Goldston, D. B., & Heilbron, N. S. (2015). Identifying and referring youths at risk for suicide following participation in school-based gatekeeper training. Suicide & Life-Threatening Behavior, 45(4), 461–476. https://doi.org/10.1111/sltb.12142.
Eack, S. M., Singer, J. B., & Greeno, C. G. (2008). Screening for anxiety and depression in community mental health: the Beck Anxiety and Depression Inventories. Community Mental Health Journal, 44(6), 465–474. https://doi.org/10.1007/s10597-008-9150-y.
Erbacher, T. A., Singer, J. B., & Poland, S. (2015). Suicide in schools: a practitioner’s guide to multi-level prevention, assessment, intervention, and postvention. New York: Routledge.
Freuchen, A., & Grøholt, B. (2015). Characteristics of suicide notes of children and young adolescents: an examination of the notes from suicide victims 15 years and younger. Clinical Child Psychology and Psychiatry, 20(2), 194–206. https://doi.org/10.1177/1359104513504312.
Garraza, L., Walrath, C., Goldston, D. B., Reid, H., & McKeon, R. (2015). Effect of the Garrett Lee Smith Memorial Suicide Prevention Program on suicide attempts among youths. JAMA Psychiatry, 72(11), 1143–1149. https://doi.org/10.1001/jamapsychiatry.2015.1933.
Gould, M. S., Marrocco, F. A., Kleinman, M., Thomas, J. G., Mostkoff, K., Cote, J., & Davies, M. (2005). Evaluating iatrogenic risk of youth suicide screening programs: a randomized controlled trial. JAMA: The Journal of the American Medical Association, 293(13), 1635–1643. https://doi.org/10.1001/jama.293.13.1635.
Hom, M. A., Joiner, T. E., & Bernert, R. A. (2016). Limitations of a single-item assessment of suicide attempt history: implications for standardized suicide risk assessment. Psychological Assessment, 28(8), 1026–1030. https://doi.org/10.1037/pas0000241.
Horowitz, L. M., Ballard, E. D., & Pao, M. (2009). Suicide screening in schools, primary care and emergency departments. Current Opinion in Pediatrics, 21(5), 620–627. https://doi.org/10.1097/MOP.0b013e3283307a89.
Joiner, T. E. (2007). Why people die by suicide. Cambridge: Harvard University Press.
Joiner, T. E. (2011). Myths about suicide. Cambridge: Harvard University Press.
Joiner, T. E., Steer, R. A., Brown, G., Beck, A. T., Pettit, J. W., & Rudd, M. D. (2003). Worst-point suicidal plans: a dimension of suicidality predictive of past suicide attempts and eventual death by suicide. Behaviour Research and Therapy, 41(12), 1469–1480.
Kann, L., McManus, T., Harris, W. A., Shanklin, S. L., Flint, K. H., Hawkins, J., et al. (2016). Youth risk behavior surveillance—United States, 2015. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C.: 2002), 65(6), 1–174. 10.15585/mmwr.ss6506a1.
Kleiman, E. M., Turner, B. J., Fedor, S., Beale, E. E., Huffman, J. C., & Nock, M. K. (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. Journal of Abnormal Psychology. https://doi.org/10.1037/abn0000273.
Klonsky, E. D., May, A. M., & Glenn, C. R. (2013). The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. Journal of Abnormal Psychology, 122(1), 231–237.
Lester, D., & Leenaars, A. (2016). A comparison of suicide notes written by men and women. Death Studies, 40(3), 201–203. https://doi.org/10.1080/07481187.2015.1086449.
Miller, A. L., Rathus, J. H., & Linehan, M. (2007). Dialectical behavior therapy with suicidal adolescents. New York: Guilford Press.
Millner, A. J., Lee, M. D., & Nock, M. K. (2017). Describing and measuring the pathway to suicide attempts: a preliminary study. Suicide & Life-Threatening Behavior, 47(3), 353–369. https://doi.org/10.1111/sltb.12284.
Mills, C., Stephan, S. H., Moore, E., Weist, M. D., Daly, B. P., & Edwards, M. (2006). The President’s New Freedom Commission: capitalizing on opportunities to advance school-based mental health services. Clinical Child and Family Psychology Review, 9(3–4), 149–161. https://doi.org/10.1007/s10567-006-0003-3.
Pisani, A. R., Murrie, D. C., & Silverman, M. M. (2016). Reformulating suicide risk formulation: from prediction to prevention. Academic Psychiatry, 40, 623–629. https://doi.org/10.1007/s40596-015-0434-6.
Ribeiro, J. D., Bodell, L. P., Hames, J. L., Hagan, C. R., & Joiner, T. E. (2013). An empirically based approach to the assessment and management of suicidal behavior. Journal of Psychotherapy Integration, 23(3), 207–221. https://doi.org/10.1037/a0031416.
Scott, M., Wilcox, H., Huo, Y., Turner, J. B., Fisher, P., & Shaffer, D. (2010). School-based screening for suicide risk: balancing costs and benefits. American Journal of Public Health, 100(9), 1648–1652. https://doi.org/10.2105/AJPH.2009.175224.
Shea, S. C. (2002). The practical art of suicide assessment: a guide for mental health professionals and substance abuse counselors. Lexington: Mental Health Presses.
Shea, S. C. (2017). Uncovering a patient’s hidden method of choice for suicide: insights from the Chronological Assessment of Suicide Events (CASE approach). Psychiatric Annals, 47(8), 421–427. https://doi.org/10.3928/00485713-20170708-01.
Smith, A. R., Witte, T. K., Teale, N. E., King, S. L., Bender, T. W., & Joiner, T. E. (2008). Revisiting impulsivity in suicide: implications for civil liability of third parties. Behavioral Sciences & the Law, 26(6), 779–797. https://doi.org/10.1002/bsl.848.
Stack, S., & Rockett, I. R. H. (2016). Are suicide note writers representative of all suicides? Analysis of the National Violent Death Reporting System. Suicide & Life-Threatening Behavior. https://doi.org/10.1111/sltb.12320.
Stanley, B., & Brown, G. K. (2012). Safety planning intervention: a brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256–264. https://doi.org/10.1016/j.cbpra.2011.01.001.
Stiffman, A. R., Pescosolido, B., & Cabassa, L. J. (2004). Building a model to understand youth service access: the Gateway Provider Model. Mental Health Services Research, 6(4), 189–198.
Walrath, C., Garraza, L. G., Reid, H., Goldston, D. B., & McKeon, R. (2015). Impact of the Garrett Lee Smith Youth Suicide Prevention Program on suicide mortality. American Journal of Public Health, 105(5), 986–993. https://doi.org/10.2105/AJPH.2014.302496.
Wintersteen, M. B. (2010). Standardized screening for suicidal adolescents in primary care. Pediatrics, 125(5), 938–944. https://doi.org/10.1542/peds.2009-2458.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with human participants or animals performed by any of the authors. Informed consent is therefore not applicable.
Conflict of Interest
Both authors of this manuscript receive royalties from the sale of their 2015 text, Suicide in schools: A practitioner’s guide to multi-level prevention, assessment, intervention, and postvention, through which the suicide monitoring tool noted in this article is made available.
Rights and permissions
About this article
Cite this article
Erbacher, T.A., Singer, J.B. Suicide Risk Monitoring: the Missing Piece in Suicide Risk Assessment. Contemp School Psychol 22, 186–194 (2018). https://doi.org/10.1007/s40688-017-0164-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40688-017-0164-8