Abstract
Introduction
Hypertension is a burden for most kidney transplant recipients. Whether respect of hypertension guidelines results in better outcomes is unknown.
Methods
In this multicenter study, office blood pressure at 12 months following transplantation (i.e., after > 20 outpatient visits), and survival were assessed over 35 years among 2004 consecutive kidney transplant recipients who received a first kidney graft from 1985 to 2019 (follow-up: 26,232 patient-years).
Results
Antihypertensive medications were used in 1763/2004 (88.0%) patients. Renin-angiotensin-system blockers were used in 35.6% (47.1% when proteinuria was > 0.5 g/day) and calcium-channel blockers were used in 6.0% of patients. Combined treatment including renin-angiotensin-system-blockers, calcium-channel blockers and diuretics was used in 15.4% of patients receiving ≥ 3 antihypertensive drugs.
Blood pressure was controlled in 8.3%, 18.8% and 43.1%, respectively, depending on definition (BP < 120/80, < 130/80, < 140/90 mmHg, respectively) and has not improved since the year 2001. Two-thirds of patients with uncontrolled blood pressure received < 3 antihypertensive classes. Low sodium intake < 2 g/day (vs ≥ 2) was not associated with better blood pressure control.
Uncontrolled blood pressure was associated with lower patient survival (in multivariable analyses) and graft survival (in univariate analyses) vs controlled hypertension or normotension. Low sodium intake and major antihypertensive classes had no influence on patient and graft survival.
Conclusions
Pharmacological recommendations and sodium intake reduction are poorly respected, but even when respected, do not result in better blood pressure control, or patient or graft survival. Uncontrolled blood pressure, not the use of specific antihypertensive classes, is associated with reduced patient, and to a lesser extent, reduced graft survival, even using the 120/80 mmHg cut-off.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is common among kidney transplant recipients (KTRs) and is recognized as a major risk factor for graft failure and death [1]. Over the last 25 years, international guidelines indicated that office blood pressure (BP) should be controlled in all hypertensive patients [1]. However, not all of them mentioned specific BP targets for KTRs, and when they did, various systolic and diastolic BP goals have been proposed (systolic BP: 120–140 mmHg; diastolic: 80–90 mmHg) [2,3,4,5,6,7]. A BP target < 120 mmHg for systolic BP was advocated following the publication of the SPRINT trial but whether this target was possible or even desirable is still debated with regard to patients with chronic kidney disease and in KTRs [1, 8, 9].
It has been largely acknowledged that BP control is difficult in this population and often requires combination therapy [1, 2]. Causes of hypertension are probably multifactorial with an important contribution of reduced renal function, diabetes mellitus and older age [2]. Most guidelines indicate repeating BP measurements, reducing sodium intake < 2 g/day and preferentially using renin-angiotensin-system blockers (RAS-blockers) at least in patients with proteinuria [2,3,4,5,6,7]. The European Society of Hypertension (ESH) guidelines proposed an “optimal treatment strategy” (RAS-blockers, calcium-channel blockers (CCBs) and diuretics) when 3 or more anti-hypertensive medications are necessary in hypertensive non-transplanted populations [5]. However, this strategy has not been evaluated in KTRs.
Finally, many uncertainties remain regarding management of hypertension in KTRs including BP target, optimal antihypertensive pharmacological treatments, and long-term effect of reduced sodium diet on BP. The long-term benefits of adopting the guidelines should be assessed not only on BP control but also on patient survival and graft survival, and the clinical utility and implementation of guidelines including the latest ones [3, 6] must be addressed [10]. Randomized clinical trials are difficult to organize over the long term (> 10 years), but careful analyses of BP management and guidelines implementation in large cohorts provide important information [1]. In the present multicenter study, we assessed BP management and control as well as patient and graft survival in 2004 KTRs over a 35-year period in the Centre-Val-de-Loire Area, France.
Methods
Patient selection and management
We conducted a retrospective analysis of 2440 consecutive kidney transplant recipients who received a first kidney transplantation from October 1985 to December 2019 at the Tours university hospital (Indre-et-Loire, France). After discharge from hospital for kidney transplantation, medical consultations were organized from 1985 to 1997 as follows: twice a week for 4 months, every week between the 4th and 9th month, every other week until the first post-transplant period. From 1997 to 2000, consultations were scheduled 3 times a week for 6 weeks, twice a week until the 5th month, every week in the 5th and 6th month, every other week between the 6th and 10th month, every month between the 11th and 18th month, every 2 months between the 19th and 24th months, then every 3 months. Since 2001, outpatient visits were less frequent, but patients had at least 21 programmed medical consultations during the first year. These patients were followed-up in 12 nephrology centers, including 90.4% in the 10 nephrology centers from the Centre-Val-de-Loire area (a 2.6 million inhabitant area): Indre-et-Loire: 33.2%, Loir-et-Cher: 12.3%, Eure-et-Loir: 13.0%, Indre: 8.1%, Cher: 16.7% and Loiret: 16.6%. During these medical consultations, weight was recorded, thorough medical examination was performed, systolic and diastolic BP were measured in a standard way with the patient in a supine position after a few minutes’ rest (specifically, reported BP was measured on the arm without arteriovenous fistula and one measurement was performed as is usual in real-life conditions). Modification of their treatments were prescribed by the nephrologists. Patients had additional medical consultations whenever necessary. Blood pressure guidelines were known by all nephrologists, and regular meetings were organized with all nephrologists from these 12 nephrology centers to standardize patient management.
Within the first year after kidney transplantation, 396 patients returned to dialysis, died or had missing data. Thus, 2004/2440 (82.1%) patients were included in the present study.
Collected data
At the time of transplantation, the following variables were available: age, gender, diabetes status before transplantation and initial immunosuppression. At 12 months, the following variables were recorded: systolic and diastolic BP, body mass index (BMI), serum creatinine level (estimated glomerular filtration rate (eGFR) using CKD-EPI equation was calculated), urinary sodium excretion (since 2010) and proteinuria (both using a 24-h urine collection), immunosuppressive drugs and antihypertensive medications.
Ethics
Data were collected from our prospectively maintained institutional database of transplant patients and the ASTRE database [“commission nationale informatique et liberté” (CNIL) agreement number: DR-2012–518]. The study protocol was approved by the Ethics Committee in Human Research (Hôpital Bretonneau, CHU Tours, France) and is in accordance with the Helsinki declaration of 1975, as revised in 2013. Results are reported according to the STROBE Statement.
Statistical analyses
Results are expressed as percentages or means ± standard deviations or median and interquartile range (IQR). Qualitative variables were compared using Chi-square test. Continuous variables were compared between two groups using Student’s t test and between multiple groups using analysis of variance (ANOVA).
Patients were considered normotensive if they received no antihypertensive medications during the first year after transplantation. To ensure that patients without antihypertensive drugs during the first year were really normotensive, we retrieved their BP values at 3 and 6 months. Patients were considered hypertensive if they were taking any antihypertensive medication at the 12-month visit. Among hypertensive patients, we analyzed whether (1) office BP was controlled using different target BP values (120/80 mmHg, 130/80 mmHg and 140/90 mmHg). The 130/80 mmHg cut-off value was our main analysis as this target BP value has been chosen by most contemporary guidelines (KDIGO 2012, AHA 2017 and KDIGO 2019 guidelines [1, 4, 11, 12]. However, as other cut-off BP values (120/80 mmHg and 140/90 mmHg) are used in the European guidelines [13,14,15], we assessed the association between these 2 cut-off BP values and the outcomes (as sensitivity analyses); we also assessed whether «appropriate» antihypertensive medications according to guidelines were used among hypertensive patients; we assessed whether salt intake was limited (i.e., urinary sodium excretion < 2 g/day–90 mmol/day, corresponding to 5 g/day of sodium chloride) [6]. These analyses were performed in the whole cohort, and in patients with proteinuria ≥ 0.5 g/day and in patients receiving at least 3 antihypertensive classes [5]. In this latter group, we assessed whether the combination therapy recommended by the ESH (“optimal treatment” i.e., RAS-blockers, CCB and diuretics) was preferentially used [5].
During follow-up, events of interest for survival analyses were patients’ death with a functioning graft and graft loss (dialysis or new transplantation). As graft loss and death with a functioning graft (DWFG) are competing events, we used the cumulative incidence competing risk (CICR) method to evaluate the predicted probability of death and graft loss. Hazard ratios and 95% confidence intervals were estimated with the subdistribution hazard approach proposed by Fine and Gray [16]. Schoenfeld residuals confirmed proportional hazard assumption.
We analyzed the risk of patient and graft survival in the whole cohort, in patients with proteinuria ≥ 0.5 g/day, in patients receiving at least 3 antihypertensive classes. We analyzed whether sodium intake < 2 g/day (vs ≥ 2/day) and RAS-blockers (vs no RAS-blockers) were associated with better patient and graft survival among patients with proteinuria, and whether the combination therapy recommended by the European Society of Hypertension was associated with better patient and graft survival (vs other treatment combinations). Finally, we compared the risk of death and graft loss among the 4 main antihypertensive classes (RAS-blockers, CCBs, diuretics and beta-blockers (BBs)) in multivariable analyses. Analyses were performed using the statistical software RStudio (RStudio Team, 2015, v1.4.1103, Boston, MA, USA).
Results
Patient characteristics
Among the 2004 included patients, median age was 54.7 [IQR: 41.8–63.9], two-thirds of patients were male and 17.0% had diabetes (Table 1). Estimated GFR at 12 months was < 45 mL/min/1.73 m2 in one third of patients. Proteinuria values were available in 1652 patients, and mean proteinuria was 0.47 ± 1.35 g/day. Urinary sodium excretion was available in 810/2004 patients. Mean sodium intake was 165 ± 80 mmol/day (i.e., mean sodium intake was 4.4 ± 1.8 g/day or mean sodium chloride intake was 9.2 ± 4.4 gday). Most patients received calcineurin inhibitors (CNIs) and 64.3% were still on steroids at the 12-month visit (Table 1).
Anti-hypertensive medications were used in 1763/2004 (88.0%) patients at 12 months (median number of antihypertensive medications: 2 [interquartile range: 1–3]). Beta blockers (BBs); 66.6%), calcium channel blockers (CCBs) (61.0%), diuretics (20.8%) and renin-angiotensin-system (RAS)-blockers (35.6%) were mostly used (Table 1). SBP/DBP values in 241 normotensive patients (i.e., patients without antihypertensive drugs at 12 months) were 127 ± 15/76 ± 11 mmHg, and 178 (73.8%) had a BP < 140/90 mmHg. The SBP/DBP of the 63 (26.2%) remaining patients was 144 ± 12/85 ± 10 mmHg. Their SBP/DBP at 3 and 6 months was 131 ± 12/77 ± 10 mmHg and 132 ± 13/79 ± 12 mmHg, respectively.
Office BP control at the 12-month visit according to baseline characteristics and BP control definition among treated patients
Office BP control was 8.3% (BP < 120/80 mmHg), 18.2% (BP < 130/80 mmHg) and 43.1% (BP < 140/90 mmHg), respectively, depending on the definition of BP control in the 1763 treated patients. Blood pressure control significantly improved from the 1985–2000 to the 2001–2020 period. However, during the 2001 to 2020 period, there was no significant improvement (Table 2).
Office BP control was significantly lower in patients with diabetes (vs no diabetes), eGFR < 45 (vs ≥ 45), proteinuria > 0.5 g/day (vs ≤ 0.5 g/day), higher BMI (obesity vs lean or overweight), patients aged > 65 (vs ≤ 65) (Table 2). No significant difference in BP control was found for use of steroid (vs no steroid), CNI (vs no CNI), mTOR inhibitor (vs no mTOR inhibitor), and men (vs women) (Table 2).
Office BP control at the 12-month visit according to management
All treated patients (n = 1763)
Sodium intake was < 2 g/day (urinary sodium excretion < 90 mmol/day) in 15.6% of patients. There was no significant difference in BP control in patients with sodium intake < 2 g/day (vs ≥ 2 g/day) (Table 3). As expected, BP control was lower in patients needing more antihypertensive classes (Table 3). Among the antihypertensive classes, RAS-blockers and CCBs (vs diuretics and BBs) were significantly associated with better BP control in univariate analyses (Table 3).
Treated patients with proteinuria (n = 365)
Proteinuria ≥ 0.5 g/day was present in 365 patients (mean ± standard deviation: 1.56 ± 2.57 g/day). Among them, RAS-blockers were used in 45.2% and sodium intake was < 2/day in 8.5%, respectively (Table 3). There was no significant difference in BP control according to RAS-blockade (vs no RAS-blockade) and sodium intake < 2 g/day (vs ≥ 2 g/day) (Table 3).
Patients with ≥ 3 antihypertensive classes (n = 537)
Overall, 537/1763 (30.5%) patients received at least 3 antihypertensive drugs; among them, optimal pharmacological treatment according to the ESH guidelines was achieved in 13.2% and sodium intake was < 2 g/day in 10.9%. No significant difference in BP control was observed in patients receiving ESH optimal pharmacological treatment (vs other combination therapies) and in those with sodium intake < 2 (vs ≥ 2 g/day) (Table 3).
Survival over the 35-year period according to office BP control at the 12-month visit
Survival models according to BP control groups were adjusted on sex, age > 65 years, diabetes, proteinuria, eGFR > 45 ml/min.1.73m2, graft vintage, steroids, CNIs, mycophenolate mofetil, donor age, donor sex, and donor diabetes (patient survival), and BMI (patient survival) or acute rejection at 1 year (graft survival). The same analyses were also performed with age as a continuous variable. Survival models according to antihypertensive medications (RAS-blockers, diuretics, beta-blockers, number of antihypertensive classes) were adjusted on sex, age > 65 years, diabetes, proteinuria, eGFR > 45 ml/min.1.73m2, graft vintage, acute rejection at 1 year, steroids, CNI, mycophenolate mofetil, donor age, donor sex, donor diabetes and other antihypertensive medications (patient survival), and acute rejection at 1 year (graft survival). Doses of antihypertensive medications were not collected and could not be added to our model.
Patient survival in the whole population (n = 2004)
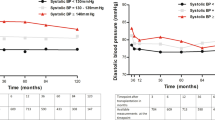
During follow-up (26,232 patient-years (range: 1.4–35.2 years)), 379 patients died while 403 patients returned to dialysis or had a new kidney graft. Uncontrolled vs controlled BP, and controlled BP vs normotension were associated with reduced patient survival over the 35-year period, irrespective of BP control definition (Fig. 1). After adjustments, uncontrolled BP remained significantly associated with worse patient survival (supplemental Table 1a). Analyses were also performed with age as a continuous variable and confirmed the association between uncontrolled BP and worse patient survival (target 120/80: HR = 2.16 [CI95% 1.23–3.79]; target 130/80 mmHg: HR = 1.72 [CI95% 0.99–3.01]; target 140/80: HR 2.38 [CI95% 1.34–4.21]). No significant association was demonstrated between specific antihypertensive classes used and the risk of patient death in multivariable analyses (Supplemental Table 2). Sodium intake < 2 g/day (vs ≥ 2 g/day) was not associated with better patient survival (Fig. 2).
Patient survival according to BP groups (uncontrolled BP, controlled BP, normotension) and BP control definition in 2004 kidney transplant recipients (crude analysis). < 120/80 mmHg (BP control definition): controlled BP vs normotension: hazard ratio (HR): 3.40 [1.74–6.65], p < 0.0001; uncontrolled vs normotension: HR: 3.87 [2.22–6.72], p < 0.0001; uncontrolled vs controlled BP: HR: 2.05 [1.47–2.86], p < 0.0001. < 130/80 mmHg (BP control definition): controlled BP vs normotension: hazard ratio (HR): 3.08 [1.68–5.66], p < 0.0001; uncontrolled vs normotension: HR: 3.99 [2.29–6.93], p < 0.0001; uncontrolled vs controlled BP: HR: 1.84 [1.21–2.41], p < 0.0001. < 140/90 mmHg (BP control definition): controlled BP vs normotension: hazard ratio (HR): 3.00 [1.70–5.32], p < 0.0001; uncontrolled BP vs normotension: HR: 4.42 [2.54–7.71], p < 0.0001; uncontrolled vs controlled BP: HR: 1.76 [1.43–2.17], p < 0.0001
Graft survival in the whole population (n = 2004)
Uncontrolled BP was associated with reduced graft survival over the 35-year period, irrespective of BP control definition in univariate analysis (Fig. 3) but not after adjustments (supplemental Table 1b). No significant association was demonstrated between use of specific antihypertensive classes and the risk of graft survival in multivariable analyses (Supplemental Table 2). Sodium intake < 2 g/day (vs ≥ 2 g/day) was not associated with better graft survival (Fig. 2).
Graft survival according to BP groups (uncontrolled BP, controlled BP, normotension) and BP control definition in 2004 kidney transplant recipients (crude analysis). 120/80 mmHg (BP control definition): controlled BP vs normotension: hazard ratio (HR): 1.27 [0.75–2.16], p = 0.380; uncontrolled vs normotension: HR: 1.55 [1.07–2.22], p = 0.019; uncontrolled vs controlled BP: HR: 1.40 [1.05–1.85], p = 0.02. 130/80 mmHg (BP control definition): controlled BP vs normotension: hazard ratio (HR): 1.32 [0.85–2.04], p = 0.220; uncontrolled vs normotension: HR: 1.57 [1.09–2.26], p = 0.016; uncontrolled vs controlled BP: HR: 1.33 [1.05–1.68], p = 0.02. 140/90 mmHg (BP control definition): controlled BP vs normotension: hazard ratio (HR): 1.28 [0.87–1.89], p = 0.210; uncontrolled BP vs normotension: HR: 1.69 [1.17–2.45], p = 0.005; uncontrolled vs controlled BP: HR: 1.39 [1.14–1.69], p = 0.001
Patient and graft survival among patients with proteinuria
There was no significant difference in patient or graft survival according to RAS-blocker use (vs no RAS-blockers) (supplemental Fig. 1a and 1b) and sodium intake < 2 g/day (vs ≥ 2 g/day) (supplemental Fig. 2a and 2b).
Patient and graft survival among patients receiving at least 3 antihypertensive classes
There was no significant difference in patient or graft survival according to the ESH optimal pharmacological treatment (vs other antihypertensive treatment combinations) (4) (supplemental Fig. 3a and 3b) and sodium intake < 2 g/day vs (≥ 2 g/day) (supplemental Fig. 4a and 4b).
Discussion
In the present multicenter study conducted in 2004 KTRs over a 35-year period, hypertension defined as the use of one or more antihypertensive medications was present in 88.0% at 12 months, sodium intake was < 2 g/day in 1 out of 6 patients, less than half of patients with proteinuria received RAS-blockers, and 1 patient out of 7 had optimal treatment according to the ESH guidelines when 3 or more antihypertensive classes were used [5]. At the 12-month visit (i.e., after more than 21 outpatient visits), office BP control varied from 8.3% to 43.1% depending on BP control definition, and these results have not improved since 2001. Only a third of patients with uncontrolled BP received 3 or more antihypertensive classes. Office BP control was not significantly influenced by sodium intake and specific antihypertensive classes. Uncontrolled BP was associated with reduced patient survival and graft survival (in univariate analysis), irrespective of BP control definition. In contrast, respect of the recommendations and use of specific antihypertensive classes had no measurable impact on patient and graft survival.
First, guidelines that we were able to test were respected in only a minority of patients [2,3,4,5,6,7]. These guidelines shared the importance of lowering sodium intake [2,3,4,5,6,7]. Sodium intake was assessed in the whole population, in patients with proteinuria, and in those with multiple antihypertensive classes, and very disappointing results were found. In the literature, similar results regarding sodium intake were observed in 610 KTRs in a study from the Netherlands [17]. In the Dutch study, 95% of KTRs had a sodium intake > 70 mmol/day [17]. In 270 KTRs from Spain, 87% of patients had an excessive sodium intake [18]. Furthermore, in our study, sodium intake ≥ 2 g/day was not associated with worse BP control (vs sodium intake < 2 g/day) in the whole population, in patients with proteinuria and in those with 3 or more antihypertensive classes, suggesting that lowering sodium intake was not better implemented in patients at high renal and cardiovascular risk. Although excessive sodium intake is universally cited as a cause of resistant hypertension, data regarding this issue are scarce in KTRs. In a study involving 38 KTRs, reduction of sodium intake for 14 days resulted in lower BP values [19]. In another study, sodium excretion was independently associated with higher BP values [18]. Other short-term interventions on dietary sodium restriction resulted in BP decrease [20]. Our own findings suggest that sodium intake likely does not play a major role over the long-term as compared to other important factors such as obesity, low eGFR, diabetes and older age. As developed in a recently published consensus paper [1], mechanisms of hypertension in KTRs included (among others) extra-cellular fluid expansion, increased sympathetic nerve activity and arterial stiffness. Arterial stiffness may play a major role in uncontrolled BP in KTRs, and low sodium diet does correct arterial stiffness. Accordingly, older patients > 65 who are at the highest risk of increased arterial stiffness had a very high risk of uncontrolled BP in the present study. The absence of beneficial long-term effects of low sodium diet on patient and graft survival also deserves comment. Low sodium diets may improve extra-cellular fluid expansion, but can also enhance angiotensin II and aldosterone secretion, which could have deleterious effects on kidney and patient survival.
Second, we assessed the implementation of international guidelines regarding pharmacological management of BP [2,3,4,5,6,7]. Half of the patients with proteinuria ≥ 0.5 g/day (corresponding to severely increased albuminuria (A3)) [21] were not treated by RAS-blockers. Obstacles to the use of RAS-blockers have been extensively studied and they include increase in serum creatinine and hyperkalemia [22, 23]. Hyperkalemia is frequently present in KTRs due to low GFR, diabetes mellitus, congestive heart failure, CNI use and acidosis). RAS-blockers may reduce hemoglobin levels, and therefore are avoided during the first months following transplantation. It was not possible to identify the exact date of the initiation of RAS-blockers, and the percentage (and reasons) of RAS-blocker withdrawal before 1 year in our study. These obstacles play a major role in RAS-blocker withdrawal or avoidance, even in these high-risk patients. We also assessed whether the optimal treatment proposed in ESC/ESH guidelines for patients treated with at least 3 antihypertensive medications could result in better BP control [5]. Less than 1 in 5 received the combination of RAS-blockers, CCBs and diuretics among these patients, and BP control was not better achieved using this strategy vs other antihypertensive medications. To the best of our knowledge, this strategy has not been tested in randomized clinical trials or in large cohorts among KTRs. Our present results do not support a superiority of this strategy vs other therapeutic combinations regarding BP control in KTRs.
Third, uncontrolled BP had a more significant impact on patient than graft survival, irrespective of BP control definition. Multivariable analyses indicated that uncontrolled BP (vs controlled BP or normotension) was associated with worse patient survival but not graft survival. However, less than 10% of patients had a BP < 120/80 mmHg in our study. Due to the design of our study, our findings do not prove that uncontrolled BP or the use of specific classes of antihypertensive medications cause decreased patient or graft survival, and the risk of unknown bias has to be considered. In addition, uncontrolled BP itself could be a marker of renal parenchymal damage due to many parameters including chronic rejection, donor age or donor characteristics. We did not measure the Kidney Donor Profile Index. However, we entered donor age, donor sex and donor diabetes as covariates in our models and our results were qualitatively unchanged. Patient and graft survival appeared as a priority for patients and physicians in the Standardized Outcomes in Nephrology— Kidney Transplantation (SONG-Tx) project [24, 25], and therefore our results support the view that systolic BP should be lowered towards 120 mmHg whenever possible. Sadly, two-thirds of patients with uncontrolled BP received only 1 or 2 antihypertensive classes, highlighting the prominent role of therapeutic inertia in most patients [10].
Fourth, implementation of guidelines regarding sodium intake and specific pharmacological treatments was not associated with better survival over a 35-year period in our cohort. However, we did not find any relationship between low sodium intake and graft and patient survival in this cohort. This does not mean that sodium reduction does not have favorable effects on cardiovascular and renal outcomes in KTRs. Furthermore, we did not assess drug adherence, and it is noteworthy that excessive sodium intake may also be a marker of poor therapeutic adherence. It is largely acknowledged that most guidelines regarding pharmacological management are not based on hard data. Latest recommendations clearly indicate that « the most important recommendation for future research for BP management in KTRs is adequately powered randomized trials evaluating the cardiovascular, kidney, and survival effects of targeting SBP»[26]. However, it is probably impossible to organize long-term (> 10 years) randomized clinical trials to assess the optimal BP target and treatment in KTRs.
The limits of our multicenter study are numerous: it is a retrospective study, and allocation of treatments was not randomized. Office BP measurement was not unattended. In this study, BP was measured in a supine position; this position was in accordance with the French Recommendations up to 2005 [27]. Blood pressure values may be influenced by body position, from supine to seated position, and thus may constitute a limitation in our study. However, in the large study of Privsek et al., SBP was higher in the seated position than in supine position in 39% of patients; SBP was higher in the supine position than in seated position in 34% and was similar regardless of the positions in the remaining 27% patients [28]. Of note, other parameters can contribute to inaccurate BP measurement in KTRs including dialysis vintage [29] and vascular calcification[30].
The BP value at 12 months was considered, although it is well known that BP may vary over time. To overcome this issue, we used 3 different cut-off values defining « BP control» (from 120 to 140 mmHg for SBP and from 80 to 90 mmHg for DBP). However, although these sensitivity analyses are important, this effort may not be sufficient as one single BP measurement at a fixed time may not represent the usual BP of the patients. A single BP measurement was used and may not reflect BP values during the whole follow-up of these patients and may have limited predictive value with regard to long-term patient outcome. Causes of death (CV vs non-CV) were not analyzed. Although BP was measured using automated devices adapted for arm size, recalibration of these devices was probably not systematically done during the 35-year follow-up period. In addition, BP was measured by many physicians enhancing the heterogeneity of BP measurement.
The use of ambulatory BP monitoring was not considered as it is not mandatory even in most recent guidelines despite a systematic review supporting it [31]. The use of office BP was relevant as it is still the most frequently used method for BP measurement. Importantly, masked hypertension was more frequent than white-coat hypertension in KTRs, so the absence of ambulatory BP monitoring could have led to BP control underestimation rather than overestimation in our study [31]. The dose of antihypertensive medications was not analyzed. Coronary artery disease rather than hypertension could be the indication of beta-blockers when used alone in some patients.
Our study also has some strengths. It is probably the largest study focused on BP control in KTRs, and it is also the study with the longest duration in this population. No other study has analyzed BP management, implementation of pharmacological and nonpharmacological guidelines and patient and graft survival in relation to BP control over a 35-year period. Nephrologists of all centers involved were aware of guidelines regarding BP measurement and control and were properly trained. Blood pressure values were considered at 12 months after transplantation, that is, at least after 21 outpatient visits with systematic BP measurement.
In conclusion, respect of the guidelines concerns only a minority of KTRs. Office BP control is poor, and has not improved since 2001. Implementation of the guidelines that we analyzed did not lead to better results. Uncontrolled BP was associated with reduced patient survival, and to a lesser extent, with reduced graft survival, even when the 120/80 mmHg cut-off was used, with no clear benefit of one class of antihypertensives over the others. These data, based on one of the largest multicenter studies in KTRs and with the longest follow-up, could help refine international guidelines regarding BP control and management in this population. They support the view that home or ambulatory BP monitoring should be recommended, and that it is now time to organize randomized clinical trials using home ambulatory BP monitoring in KTRs [1, 10, 31].
Availability of data and material
The data are held by the nephrology department of the university hospital of Tours and are available on request according to the procedures in place.
References
Halimi J-M, Ortiz A, Sarafidis PA et al (2021) Hypertension in kidney transplantation: a consensus statement of the ‘hypertension and the kidney’ working group of the European society of hypertension. J Hypertens 39:1513–1521. https://doi.org/10.1097/HJH.0000000000002879
Chobanian AV, Bakris GL, Black HR et al (2003) Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42:1206–1252. https://doi.org/10.1161/01.HYP.0000107251.49515.c2
Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group (2021) KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int 99:S1–S87. https://doi.org/10.1016/j.kint.2020.11.003
Whelton PK, Carey RM, Aronow WS et al (2018) ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the american college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. https://doi.org/10.1161/HYP.0000000000000065
Williams B, Mancia G, Spiering W et al (2018) 2018 Practice guidelines for the management of arterial hypertension of the European society of cardiology and the european society of hypertension. Blood Press 27:314–340. https://doi.org/10.1080/08037051.2018.1527177
Drawz PE, Beddhu S, Bignall ONR et al (2022) KDOQI US commentary on the 2021 KDIGO clinical practice guideline for the management of blood pressure in CKD. Am J Kidney Dis 79:311–327. https://doi.org/10.1053/j.ajkd.2021.09.013
Blacher J, Halimi J-M, Hanon O et al (2014) Management of hypertension in adults: the 2013 French society of hypertension guidelines. Fundam Clin Pharmacol 28:1–9. https://doi.org/10.1111/fcp.12044
Dasgupta I, Zoccali C (2022) Is the KDIGO systolic blood pressure target <120 mm Hg for chronic kidney disease appropriate in routine clinical practice? Hypertension 79:4–11. https://doi.org/10.1161/HYPERTENSIONAHA.121.18434
(2017) A randomized trial of intensive versus standard blood-pressure Control. N Engl J Med 377:2506–2506. Doi: https://doi.org/10.1056/NEJMx170008
Halimi J-M, Persu A, Sarafidis PA et al (2017) Optimizing hypertension management in renal transplantation: a call to action. Nephrol Dial Transplant 32:1959–1962. https://doi.org/10.1093/ndt/gfx283
Verbeke F, Lindley E, Van Bortel L et al (2014) A European renal best practice (ERBP) position statement on the kidney disease: improving global outcomes (KDIGO) clinical practice guideline for the management of blood pressure in non-dialysis-dependent chronic kidney disease: an endorsement with some caveats for real-life application. Nephrol Dial Transplant 29:490–496. https://doi.org/10.1093/ndt/gft321
Cheung AK, Chang TI, Cushman WC et al (2019) Blood pressure in chronic kidney disease: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int 95:1027–1036. https://doi.org/10.1016/j.kint.2018.12.025
Williams B, Mancia G, Spiering W et al (2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 39:3021–3104. https://doi.org/10.1093/eurheartj/ehy339
Unger T, Borghi C, Charchar F et al (2020) 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension 75:1334–1357. https://doi.org/10.1161/HYPERTENSIONAHA.120.15026
Visseren FLJ, Mach F, Smulders YM et al (2021) 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 42:3227–3337. https://doi.org/10.1093/eurheartj/ehab484
Hsu JY, Roy JA, Xie D et al (2017) Statistical Methods for Cohort studies of CKD: survival analysis in the setting of competing risks. Clin J Am Soc Nephrol 12:1181–1189. https://doi.org/10.2215/CJN.10301016
van den Berg E, Geleijnse JM, Brink EJ et al (2012) Sodium intake and blood pressure in renal transplant recipients. Nephrol Dial Transplant 27:3352–3359. https://doi.org/10.1093/ndt/gfs069
Rodrigo E, Monfá E, Albines Z et al (2015) Sodium Excretion pattern at 1 year after kidney transplantation and high blood pressure. Ann Transplant 20:569–575. https://doi.org/10.12659/AOT.893862
Soypacaci Z, Sengul S, Yıldız EA et al (2013) Effect of daily sodium intake on post-transplant hypertension in kidney allograft recipients. Transplant Proc 45:940–943. https://doi.org/10.1016/j.transproceed.2013.02.050
de Vries LV, Dobrowolski LC, van den Bosch JJON et al (2016) Effects of Dietary Sodium Restriction in Kidney transplant recipients treated with renin-angiotensin-aldosterone system blockade: a randomized clinical trial. Am J Kidney Dis 67:936–944. https://doi.org/10.1053/j.ajkd.2015.11.026
Levey AS, Eckardt K-U, Dorman NM et al (2020) Nomenclature for kidney function and disease: report of a kidney disease: improving global outcomes (KDIGO) consensus conference. Kidney Int 97:1117–1129. https://doi.org/10.1016/j.kint.2020.02.010
Cross NB, Webster AC, Masson P et al (2009) Antihypertensive treatment for kidney transplant recipients. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003598.pub2
Pisano A, Bolignano D, Mallamaci F et al (2020) Comparative effectiveness of different antihypertensive agents in kidney transplantation: a systematic review and meta-analysis. Nephrol Dial Transplant 35:878–887. https://doi.org/10.1093/ndt/gfz092
Sautenet B, Tong A, Manera KE et al (2017) Developing consensus-based priority outcome domains for trials in kidney transplantation: a multinational delphi survey with patients, caregivers, and health professionals. Transplantation 101:1875–1886. https://doi.org/10.1097/TP.0000000000001776
Tong A, Gill J, Budde K et al (2017) Toward establishing core outcome domains for trials in kidney transplantation: report of the standardized outcomes in nephrology—kidney transplantation consensus workshops. Transplantation 101:1887–1896. https://doi.org/10.1097/TP.0000000000001774
Cheung AK, Chang TI, Cushman WC et al (2021) Executive summary of the KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int 99:559–569. https://doi.org/10.1016/j.kint.2020.10.026
Prise en charge des patients adultes atteints d’hypertension artérielle essentielle. In: Haute Autorité de Santé France. 2005.
Privšek E, Hellgren M, Råstam L et al (2018) Epidemiological and clinical implications of blood pressure measured in seated versus supine position. Medicine (Baltimore) 97:e11603. https://doi.org/10.1097/MD.0000000000011603
Sarafidis PA, Persu A, Agarwal R et al (2017) Hypertension in dialysis patients: a consensus document by the European renal and cardiovascular medicine (EURECA-m) working group of the European renal association-european dialysis and transplant association (ERA-EDTA) and the hypertension and the kidney working group of the European society of hypertension (ESH)*. Nephrol Dial Transplant 32:620–640. https://doi.org/10.1093/ndt/gfw433
Arroyo D, Betriu A, Martinez-Alonso M et al (2014) Observational multicenter study to evaluate the prevalence and prognosis of subclinical atheromatosis in a Spanish chronic kidney disease cohort: baseline data from the NEFRONA study. BMC Nephrol 15:168. https://doi.org/10.1186/1471-2369-15-168
Pisano A, Mallamaci F, D’Arrigo G et al (2022) Assessment of hypertension in kidney transplantation by ambulatory blood pressure monitoring: a systematic review and meta-analysis. Clin Kidney J 15:31–42. https://doi.org/10.1093/ckj/sfab135
Acknowledgements
We wish to thank Lise Binet for her precious help.
Funding
The authors report no specific funding in relation to this research.
Author information
Authors and Affiliations
Contributions
J-MH: design, data analysis and writing. J-MH, J-BF and LTW: data management, data analysis and writing. GP, SB, MB, HL, TB-A: writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
None directly related to the matter of this article. JMH has received fees for lectures or consulting from Alexion, Sanofi, AstraZeneca, Bayer, Boehringer-Ingelheim France, MSD, and Servier, and a grant from AstraZeneca.
Ethical approval
The study was approved by the regional ethic committee (“Espace de reflexion éthique region Centre”: research project no. 2017-003).
Human and Animal rights
This study does not contain any studies with animals.
Informed consent
For this type of study, informed consent is not required by French law.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wangueu, L.T., de Fréminville, JB., Gatault, P. et al. Blood pressure management and long-term outcomes in kidney transplantation: a holistic view over a 35-year period. J Nephrol 36, 1931–1943 (2023). https://doi.org/10.1007/s40620-023-01706-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-023-01706-9