Abstract
Background
Intradialytic hypotension is a clinically relevant complication in haemodialysis patients. Pre-dialysis diastolic blood pressure is routinely measured. However, the association between pre-dialysis diastolic blood pressure and intradialytic hypotension is not well understood.
Methods
Patient-level (N = 545) and haemodialysis session-level (N = 3261) data were collected; the exposure variable was pre-dialysis diastolic blood pressure. The primary outcome of interest was the development of intradialytic hypotension, defined as any nadir < 100 mmHg if the pre-dialysis systolic blood pressure was ≥ 160 mmHg, or any nadir < 90 mmHg if the pre-dialysis systolic blood pressure was < 160 mmHg. Odds ratios (ORs) with 95% confidence intervals (CIs) were estimated using mixed-effects logistic regression for the association between pre-dialysis diastolic blood pressure and intradialytic hypotension, after adjusting for potential confounders.
Results
Intradialytic hypotension occurred in 14.4% of the sessions. All sessions were divided into five categories according to pre-dialysis diastolic blood pressure. The adjusted ORs for intradialytic hypotension were 2.72 (95% CI 1.64–4.51), 1.07 (95% CI 0.68–1.66), 1.68 (95% CI 1.08–2.62), and 1.81 (95% CI 1.05–3.14) in sessions with pre-dialysis diastolic blood pressure of < 60 mmHg, ≥ 60 to < 70 mmHg, ≥ 80 to < 90 mmHg, and ≥ 90 mmHg, respectively, compared with the reference pre-dialysis diastolic blood pressure of ≥ 70 to < 80 mmHg. Cubic spline analyses revealed a reverse J-shaped association between pre-dialysis diastolic blood pressure and intradialytic hypotension.
Conclusions
Low and high pre-dialysis diastolic blood pressure levels were associated with intradialytic hypotension. This may help identify patients at a high risk of developing intradialytic hypotension.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intradialytic hypotension (IDH) is a clinically relevant complication in patients undergoing haemodialysis (HD). Previous studies have noted that IDH is associated with high mortality and incidence of cardiovascular events, vascular failure, loss of residual renal function, intradialytic symptoms, and intradialytic cardiac arrhythmias [1,2,3,4,5,6,7,8]. Nevertheless, there is only weak evidence of a strategy for the prevention and treatment of IDH, which is an area of high unmet need [9,10,11]. It might be important to identify the factors that predict IDH.
Diastolic blood pressure (DBP) is measured simultaneously with systolic blood pressure (SBP). Previous studies have shown a J-shaped association between DBP and cardiovascular events in the general population and in patients with stable coronary artery disease [12,13,14,15]. Low DBP may decrease coronary perfusion to the myocardium, which leads to subclinical myocardial damage [16], whereas high DBP is associated with coronary artery stenosis, which may contribute to cardiovascular events [17]. Therefore, DBP is clinically used as a risk factor and predictor of cardiovascular events.
To our knowledge, the association between pre-dialysis DBP and IDH is not well understood. We hypothesised that high and low pre-dialysis DBP levels are associated with IDH. Given the key role of DBP in the coronary artery, a history of ischaemic heart disease (IHD) may strongly affect this association. Hence, to clarify the relationship between pre-dialysis DBP and IDH, we conducted a retrospective study using data from a dialysis centre in Japan.
Methods
Study design and population
This was a retrospective cohort study at Rakuwakai Otowa Kinen Hospital, a high-volume dialysis centre in the Yamashina region of Kyoto, Japan. This study included patients undergoing maintenance HD who had data available on pre-dialysis DBP and medical information in December 2017. This study excluded patients with pre-dialysis SBP < 90 mmHg because these patients were not at risk for IDH. The study design was approved by the Rakuwakai Otowa Hospital Ethics Committee (approval number: Rakuoto-Rin-21-022) and conducted according to the Helsinki Declaration of 1975, as revised in 2013.
Exposure
Pre-dialysis DBP was measured in the dorsal position after a few minutes of rest. All HD sessions were divided into five categories according to pre-dialysis DBP (< 60 mmHg, ≥ 60 mmHg to < 70 mmHg, ≥ 70 mmHg to < 80 mmHg, ≥ 80 mmHg to < 90 mmHg, and ≥ 90 mmHg). A pre-dialysis DBP of ≥ 70 mmHg to < 80 mmHg was used as a reference in our model for categorical variable analysis, as per a previous study [14]. Similarly, for continuous variable analysis, a pre-dialysis DBP of 80 mmHg was used as a reference [14].
Outcomes
The primary outcome of interest was the development of IDH, defined as any nadir < 100 mmHg if the pre-dialysis SBP was ≥ 160 mmHg, or any nadir < 90 mmHg if the pre-dialysis SBP was < 160 mmHg [1]. Pre-dialysis SBP was measured in the dorsal position after a few minutes of rest, and intradialytic blood pressure was measured every 30 min (IDHnadir).
Statistical analysis
Regarding the session-level characteristics categorised by pre-dialysis DBP, continuous data with a normal distribution were summarised as means (standard deviation [SD]), continuous variables with skewed data were presented as medians (interquartile range [IQR]), and dichotomous data were presented as proportions. Unadjusted and adjusted odds ratios (ORs) with 95% confidence intervals (CIs) for IDHnadir according to the categories of pre-dialysis DBP were calculated using a mixed-effects logistic regression model. A random intercept was included to account for repeated measures within the subjects, imposing a compound symmetric covariance structure. This model was adjusted for age, sex, body mass index (BMI), diabetes as the primary cause of end-stage renal disease (ESRD), haemodialysis vintage, vascular access, dialysate temperature, interdialytic weight gain (IDWG), ultrafiltration rate (UFR), pre-dialysis SBP, treatment modality, use of antihypertensive drugs, use of antihypotensive drugs, IHD, serum albumin level, and C-reactive protein (CRP) level. These variables were based on a priori clinical judgement and existing studies [2, 3, 9,10,11,12,13,14,15]. Serum albumin and CRP levels were not available at every dialysis session. Therefore, these values were obtained from the data of the first session.
Furthermore, we analysed the relationship nonlinearly by modelling pre-dialytic DBP as a continuous variable rather than a categorical value using a restricted cubic spline. We used four knots located at the 5th, 35th, 65th, and 95th pre-dialytic DBP, as recommended [18].
The history of IHD as an effect modifier was analysed to assess potential differences in the pattern of association of pre-dialytic DBP categories with IDHnadir. IHD was defined as acute myocardial infarction, unstable angina, and/or revascularisation. ORs were estimated using mixed-effects logistic regression adjusted for the same confounding factors. The reference was non-IHD and pre-dialysis DBP categories of ≥ 70 mmHg to < 80 mmHg. The tests for interactions were assessed using the Wald test.
Two sensitivity analyses were performed to examine the robustness of the association. In sensitivity analysis 1, unadjusted and adjusted incidence rate ratios (IRRs) with 95% CIs were calculated using a Poisson mixed-effects model. A random intercept was included to account for repeated measures within the subjects. In sensitivity analysis 2, unadjusted and adjusted ORs with 95% CIs were calculated using generalised estimating equations with robust variance estimation. Sensitivity analyses of the association between IDHnadir and continuous variables of pre-dialysis DBP were also conducted. In addition, the interaction between pre-dialysis DBP and IHD on IDHnadir was also examined in the two models.
All analyses were performed using Stata Ver. 15.0 software (Stata Corp., College Station, TX, USA). Statistical significance was set at P < 0.05.
Results
Session-level characteristics by pre-dialysis DBP categories
A total of 3261 HD sessions from 545 patients were analysed in this study (Supplementary Fig. 1). Table 1 shows the overall session-level characteristics and pre-dialysis DBP categories. The median age was 71.1 years; males, 58.0%; diabetes as the primary cause of ESRD, 42.0%; arteriovenous fistula (AVF), 88.7%; and median haemodialysis vintage, 5.0 years. The patients with low pre-dialysis DBP tended to be older, had a higher proportion of females, had a lower BMI, had a higher history of IHD, and a lower serum albumin level. The patients with high pre-dialysis DBP tended to have a higher proportion of AVF and haemodiafiltration (HDF) as treatment modalities, with higher IDWG, UFR, and pre-dialysis SBP.
Distributions of pre-dialysis DBP
A histogram of the pre-dialysis DBP is shown in Supplementary Fig. 2. This shows a normal distribution (mean, 77.0 mmHg [16.7] mmHg).
Association between pre-dialysis DBP and IDHnadir
Categorical variable analysis
IDHnadir occurred in 14.4% (470/3,261) of all sessions. Table 2 shows the association between the pre-dialysis DBP categories and IDHnadir. The unadjusted ORs for IDHnadir were 4.22 (95% CI 2.63–6.78), 1.29 (95% CI 0.84–2.00), 1.32 (95% CI 0.86–2.04), and 1.07 (95% CI 0.65–1.75) in sessions with a pre-dialysis DBP of < 60 mmHg, ≥ 60 mmHg to < 70 mmHg, ≥ 80 mmHg to < 90 mmHg, and ≥ 90 mmHg, respectively, compared with the reference pre-dialysis DBP of ≥ 70 mmHg to < 80 mmHg. Furthermore, after adjustment for potential confounders, the adjusted ORs for IDHnadir were 2.72 (95% CI 1.64–4.51), 1.07 (95% CI 0.68–1.66), 1.68 (95% CI 1.08–2.62), and 1.81 (95% CI 1.05–3.14) in sessions with a pre-dialysis DBP of < 60 mmHg, ≥ 60 mmHg to < 70 mmHg, ≥ 80 mmHg to < 90 mmHg, and ≥ 90 mmHg, respectively, compared with the reference pre-dialysis DBP of ≥ 70 mmHg to < 80 mmHg.
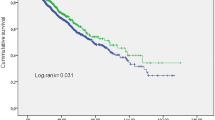
Continuous variable analysis
Figure 1 shows the association between pre-dialysis DBP as a continuous variable and IDHnadir. Restricted cubic spline analysis revealed a reverse J-shaped association between pre-dialysis DBP and IDHnadir.
OR for IDHnadir by pre-dialysis DBP. Note: Restricted cubic spline plots of the ORs for IDHnadir according to pre-dialysis DBP. The solid line represents the OR, and the dotted line represents the 95% confidence interval. The horizontal grey line corresponds to a normal reference OR of 1.0. A pre-dialysis DBP of 80 mmHg was used as the reference in this study. ORs were estimated using mixed-effects logistic regression for the association between pre-dialysis DBP and IDHnadir adjusted for age, sex, BMI, cause of ESRD, haemodialysis vintage, vascular access, dialysate temperature, IDWG, ultrafiltration rate, pre-dialysis SBP, treatment modality, use of antihypertensive drugs, use of antihypotensive drugs, IHD, serum albumin level, and CRP level. IDHnadir was defined as any nadir < 100 mmHg if the pre-dialysis SBP was ≥ 160 mmHg, or any nadir < 90 mmHg if the pre-dialysis SBP was < 160 mmHg. OR odds ratio, IDH intradialytic hypotension, DBP diastolic blood pressure, BMI body mass index, ESRD end-stage renal disease, IDWG interdialytic weight gain, SBP systolic blood pressure, IHD ischaemic heart disease, CRP C-reactive protein
Interaction between pre-dialysis DBP and history of IHD and IDHnadir
Table 3 shows that the IHD categories modified the association between pre-dialysis DBP and IDHnadir. A history of IHD and pre-dialysis DBP of < 60 mmHg, ≥ 80 mmHg to < 90 mmHg, and ≥ 90 mmHg were more closely associated with IDHnadir than non-IHD and a pre-dialysis DBP of ≥ 70 mmHg to < 80 mmHg (adjusted ORs 3.55 [95% CI 1.58–7.95], 4.11 [95% CI 1.80–9.39], and 6.22 [95% CI 2.44–15.82], respectively). A significant interaction between both IHD and pre-dialysis DBP categories and IDHnadir was observed (P for interaction < 0.001).
Sensitivity analysis
In sensitivity analysis 1, adjusted IRRs for IDHnadir were 1.95 (95% CI 1.36–2.80), 1.14 (95% CI 0.82–1.59), 1.39 (95% CI 0.99–1.95), and 1.48 (95% CI 0.99–2.21) in sessions with a pre-dialysis DBP of < 60 mmHg, ≥ 60 mmHg to < 70 mmHg, ≥ 80 mmHg to < 90 mmHg, and ≥ 90 mmHg, respectively, compared with the reference pre-dialysis DBP of ≥ 70 mmHg to < 80 mmHg (Supplementary Table 1). Similar results were obtained for the continuous association between pre-dialysis DBP and IDHnadir (Supplementary Fig. 3). A history of IHD and pre-dialysis DBP of < 60 mmHg, ≥ 80 mmHg to < 90 mmHg, and ≥ 90 mmHg were more closely associated with IDHnadir than non-IHD and a pre-dialysis DBP ≥ 70 mmHg to < 80 mmHg (adjusted IRR 2.39 [95% CI 1.42–4.01], 2.44 [95% CI 1.40–4.25], and 2.91 [95% CI 1.57–5.40], respectively). A significant interaction between both IHD and pre-dialysis DBP categories and IDHnadir was observed (P for interaction < 0.001) (Supplementary Table 2).
In sensitivity analysis 2, adjusted ORs for IDHnadir were 2.06 (95% CI 1.45–2.94), 1.03 (95% CI 0.74–1.43), 1.47 (95% CI 1.08–2.00), and 1.59 (95% CI 1.09–2.34) in sessions with a pre-dialysis DBP of < 60 mmHg, ≥ 60 mmHg to < 70 mmHg, ≥ 80 mmHg to < 90 mmHg, and ≥ 90 mmHg, respectively, compared with the reference pre-dialysis DBP of ≥ 70 mmHg to < 80 mmHg (Supplementary Table 3). Similar results were obtained for the continuous association between pre-dialysis DBP and IDHnadir (Supplementary Fig. 4). A history of IHD and pre-dialysis DBP of < 60 mmHg, ≥ 80 mmHg to < 90 mmHg, and ≥ 90 mmHg were more closely associated with IDHnadir than non-IHD and a pre-dialysis DBP of ≥ 70 mmHg to < 80 mmHg (adjusted OR 2.56 [95% CI 1.37–4.77], 2.87 [95% CI 1.58–5.23], and 3.91 [95% CI 2.08–7.36], respectively). A significant interaction between both IHD and pre-dialysis DBP categories and IDHnadir was observed (P for interaction < 0.001) (Supplementary Table 4).
Discussion
In the present study, we observed that both high and low pre-dialysis DBP levels were associated with IDH. Continuous variable analysis revealed a reverse J-shaped association between pre-dialysis DBP and IDH. This association differs across the history of IHD. Additionally, similar results regarding these associations were obtained from the sensitivity analyses.
As with the association of cardiovascular events with both high and low DBP in previous studies [12,13,14,15], the present study revealed that both high and low pre-dialysis DBP levels were associated with IDH. However, the difference was that a low pre-dialysis DBP had a much higher risk of IDH than a high pre-dialysis DBP. As a mechanism, it was considered that low DBP decreased coronary perfusion to the myocardium, which may lead to a potential ischaemic state, and cause IDH [16].
In addition, a history of IHD had an effect on the association between pre-dialysis DBP and IDH, which is reasonable considering the mechanism. On the other hand, a combination of a high pre-dialysis DBP and a history of IHD was associated with the highest risk of IDH. This result is similar to previous studies about the association between DBP and cardiovascular events in patients with stable coronary disease [12,13,14,15]. A previous study showed that high DBP was associated with arteriosclerosis of the coronary arteries [17]. Arteriosclerosis of the coronary arteries reduces coronary flow reserve (CFR), which is the ratio of the maximal or hyperaemic flow down coronary arteries to the resting flow [19]. CFR represents the capacity of increasing coronary flow to dilate following an increase in myocardial metabolic demands. Therefore, we presumed that the present state of vulnerability to ischaemia and a history of IHD may synergistically lead to IDH under the load of haemodialysis that reduces myocardial perfusion itself [20].
The clinical implication is that DBP is a routinely measured vital sign that makes it easy to identify high-risk patients with IDH. Although effective treatments for IDH are limited, pre-dialysis DBP and a history of IHD may identify high-risk patients with IDH development, which may allow for close monitoring of target patients.
The major strengths of this study are as follows. This is the first study to reveal the association between pre-dialysis DBP and IDH, and the first study to evaluate the interaction between pre-dialysis DBP and a history of IHD and IDH. Additionally, pre-dialysis DBP is routinely measured, and a combination of pre-dialysis DBP and history of IHD may help identify patients at high risk of developing IDH. Lastly, using various statistical models, the association between pre-dialysis DBP and IDH was consistent, which showed the robustness of the results.
This study has several limitations. First, this was a single-centre study, leading to limited generalisability. Second, there were unknown and unmeasured confounding factors as this was a retrospective cohort study. This study lacked information on cardiac function. Low cardiac function is associated with both low DBP and IDH [21]. Therefore, we might have overestimated the association between low DBP and IDH. However, we minimised the effects by excluding patients with low pre-SBP and adjusting for pre-SBP. Third, this study was observational; therefore, it could not directly show cause-and-effect associations.
In conclusion, our study revealed that low and high pre-dialysis DBP levels were associated with IDH, and the association differed across the history of IHD. This may help identify patients at a high risk of developing IDH.
References
Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM (2015) Association of mortality risk with various definitions of intradialytic hypotension. J Am Soc Nephrol 26:724–734. https://doi.org/10.1681/ASN.2014020222
Shoji T, Tsubakihara Y, Fujii M, Imai E (2004) Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int 66:1212–1220. https://doi.org/10.1111/j.1523-1755.2004.00812.x
Tislér A, Akócsi K, Borbás B, Fazakas L, Ferenczi S, Görögh S, Kulcsár I, Nagy L, Sámik J, Szegedi J, Tóth E, Wágner G, Kiss I (2003) The effect of frequent or occasional dialysis-associated hypotension on survival of patients on maintenance haemodialysis. Nephrol Dial Transplant 18:2601–2605. https://doi.org/10.1093/ndt/gfg450
Burton JO, Jefferies HJ, Selby NM, McIntyre CW (2009) Hemodialysis-induced cardiac injury: determinants and associated outcomes. Clin J Am Soc Nephrol 4:914–920. https://doi.org/10.2215/CJN.03900808
Chang TI, Paik J, Greene T, Desai M, Bech F, Cheung AK, Chertow GM (2011) Intradialytic hypotension and vascular access thrombosis. J Am Soc Nephrol 22:1526–1533. https://doi.org/10.1681/ASN.2010101119
Jansen MA, Hart AA, Korevaar JC, Dekker FW, Boeschoten EW, Krediet RT, NECOSAD Study Group (2002) Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int 62:1046–1053. https://doi.org/10.1046/j.1523-1755.2002.00505.x
Correa S, Pena-Esparragoza JK, Scovner KM, Mc Causland FR (2020) Predictors of intradialytic symptoms: an analysis of data from the hemodialysis study. Am J Kidney Dis 76:331–339. https://doi.org/10.1053/j.ajkd.2020.01.004
Mc Causland FR, Tumlin JA, Roy-Chaudhury P, Koplan BA, Costea AI, Kher V, Williamson D, Pokhariyal S, Charytan DM, MiD Investigators and Committees* (2020) Intradialytic hypotension and cardiac arrhythmias in patients undergoing maintenance hemodialysis: results from the monitoring in dialysis study. Clin J Am Soc Nephrol 15:805–812. https://doi.org/10.2215/CJN.06810619
Sars B, van der Sande FM, Kooman JP (2020) Intradialytic hypotension: mechanisms and outcome. Blood Purif 49:158–167. https://doi.org/10.1159/000503776
Reeves PB, Mc Causland FR (2018) Mechanisms, clinical implications, and treatment of intradialytic hypotension. Clin J Am Soc Nephrol 13:1297–1303. https://doi.org/10.2215/CJN.12141017
Kanbay M, Ertuglu LA, Afsar B, Ozdogan E, Siriopol D, Covic A, Basile C, Ortiz A (2020) An update review of intradialytic hypotension: concept, risk factors, clinical implications and management. Clin Kidney J 13:981–993. https://doi.org/10.1093/ckj/sfaa078
McEvoy JW, Chen Y, Rawlings A, Hoogeveen RC, Ballantyne CM, Blumenthal RS, Coresh J, Selvin E (2016) Diastolic blood pressure, subclinical myocardial damage, and cardiac events: implications for blood pressure control. J Am Coll Cardiol 68:1713–1722. https://doi.org/10.1016/j.jacc.2016.07.754
Flint AC, Conell C, Ren X, Banki NM, Chan SL, Rao VA, Melles RB, Bhatt DL (2019) Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N Engl J Med 381:243–251. https://doi.org/10.1056/NEJMoa1803180
Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, Tendera M, Tavazzi L, Bhatt DL, Steg PG, CLARIFY Investigators (2016) Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet 388:2142–2152. https://doi.org/10.1016/S0140-6736(16)31326-5
Vidal-Petiot E, Greenlaw N, Ford I, Ferrari R, Fox KM, Tardif JC, Tendera M, Parkhomenko A, Bhatt DL, Steg PG (2018) Relationships between components of blood pressure and cardiovascular events in patients with stable coronary artery disease and hypertension. Hypertension 71:168–176. https://doi.org/10.1161/HYPERTENSIONAHA.117.10204
Messerli FH, Panjrath GS (2009) The J-curve between blood pressure and coronary artery disease or essential hypertension: exactly how essential? J Am Coll Cardiol 54:1827–1834. https://doi.org/10.1016/j.jacc.2009.05.073
Saleh M, Alfaddagh A, Elajami TK, Ashfaque H, Haj-Ibrahim H, Welty FK (2018) Diastolic blood pressure predicts coronary plaque volume in patients with coronary artery disease. Atherosclerosis 277:34–41. https://doi.org/10.1016/j.atherosclerosis.2018.07.031
Harrell FE (2001) General aspects of fitting regression models. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis, 2nd edn. Springer, New York, pp 13–44
Gould KL, Lipscomb K, Hamilton GW (1974) Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am J Cardiol 33:87–94. https://doi.org/10.1016/0002-9149(74)90743-7
McIntyre CW, Burton JO, Selby NM, Leccisotti L, Korsheed S, Baker CS, Camici PG (2008) Hemodialysis-induced cardiac dysfunction is associated with an acute reduction in global and segmental myocardial blood flow. Clin J Am Soc Nephrol 3:19–26. https://doi.org/10.2215/CJN.03170707
Böhm M, Ferreira JP, Mahfoud F, Duarte K, Pitt B, Zannad F, Rossignol P (2020) Myocardial reperfusion reverses the J-curve association of cardiovascular risk and diastolic blood pressure in patients with left ventricular dysfunction and heart failure after myocardial infarction: insights from the EPHESUS trial. Eur Heart J 41:1673–1683. https://doi.org/10.1093/eurheartj/ehaa132
Acknowledgements
We would like to thank the patients and medical staff at the Otowa Kinen Hospital, for their cooperation in this study.
Funding
The authors did not receive support from any organisation for the submitted work.
Author information
Authors and Affiliations
Contributions
Research idea and study design: TH, YK, and TN; data acquisition: TH, YK, and TN; data analysis/interpretation: TH and YK; statistical analysis: TH and YK; supervision or mentorship: TN. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Takashi Hara, Yuto Kasahara, and Takahiko Nakagawa declare no competing interests.
Ethical disclosures
This study was performed in accordance with the ethical standards, the Declaration of Helsinki and its later amendments; IRB approval April 7 2021, approval number: Rakuoto-Rin-21-022, Rakuwakai Otowa Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hara, T., Kasahara, Y. & Nakagawa, T. Pre-dialysis diastolic blood pressure and intradialytic hypotension in patients undergoing maintenance haemodialysis. J Nephrol 35, 1419–1426 (2022). https://doi.org/10.1007/s40620-022-01292-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-022-01292-2