Abstract
Background
Abnormalities of bone mineral parameters are associated with increased mortality in patients on dialysis, but their effects and the optimal range of these biomarkers are less well characterized in non-dialysis chronic kidney disease (CKD).
Methods
PECERA (Collaborative Study Project in Patients with Advanced CKD) is a 3-year, prospective multicenter, open-cohort study of 966 adult patients with non-dialyzed CKD stages 4–5 enrolled from 12 centers in Spain. Associations between levels of serum calcium (Ca) (corrected for albumin), phosphate (P), and intact parathyroid hormone (iPTH) with all-cause mortality (primary outcome) and cardiovascular mortality (secondary outcome) were examined using time-dependent Cox proportional hazards models and penalized splines analysis adjusted by demographics and comorbidities, treatments and biochemical values collected every 6 months for 3 years.
Results
After a median follow-up of 29 months (IQR: 13–36 months) there were 181 deaths (19%). The association of calcium with all-cause mortality was J-shaped, with an increased risk for all-cause mortality at levels > 10.5 mg/dL. For phosphate and iPTH levels, the association was U-shaped. The serum values associated with the minimum risk of mortality were 3.8 mg/dL for phosphate and 70 pg/mL for iPTH, being the lowest risk ranges between 2.8 and 5.0 mg/dL, and between 38 and 112 pg/mL for phosphate and iPTH, respectively.
Conclusions
Our study provides evidence on the non-linear association of serum calcium, phosphate and iPTH levels with mortality in stage 4 and 5 CKD patients, and suggests potential survival benefits for controlling bone mineral parameters in this population, as previously reported for dialysis patients.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abnormalities in serum calcium (Ca), phosphate (P) and parathyroid hormone (PTH), bony derangements and vascular calcification are progressively more common in patients with chronic kidney disease (CKD) stages 4 and 5 and are collectively referred to as CKD-mineral and bone disorders (CKD-MBD) [1,2,3].
Epidemiological studies associate these disturbances with the risk of both all-cause and cardiovascular mortality of patients with CKD [4,5,6,7]. Accordingly, the international Kidney Disease: Improving Global Outcomes (KDIGO) guidelines for CKD-MBD suggest (2C) maintaining serum calcium, phosphate and PTH within different target ranges for each CKD stage, making the assessment and control of theses biochemical parameters an integral component of the routine care of these patients [8].
These recommendations have been challenged and criticized for being based on observational studies [9,10,11]. However, it is unlikely that large clinical trials evaluating target ranges of CKD-MBD biomarkers will be conducted. Prospective, well-designed observational studies may instead contribute to provide the strength of evidence needed to inform practice [12]. While some prospective cohorts in dialysis have described “optimal” risk ranges for calcium, phosphate and PTH levels based on mortality risk prediction [13, 14], no evidence on the matter exists for persons with non-dialysis-dependent (NDD) CKD stages 4 and 5 [8]. Using data from the PECERA study, we prospectively investigated the longitudinal associations of serum CKD-MBD biomarkers with mortality in patients with CKD stages 4–5 undergoing routine clinical care, and evaluated clinical ranges associated to lowest mortality risks.
Methods
Study design and population
The PECERA (Collaborative Study Project In patients with Advanced Renal Failure) is a multi-center, prospective, observational cohort of NDD patients with CKD stages 4–5 undergoing repeated clinical assessments during a maximum of 3 years. Patients were enrolled from 12 centers in the Valencian Community of Spain. All centers were ascribed to the Spanish National Healthcare system, providing universal and government-subsidized healthcare. The study was conducted in accordance with the Declaration of Helsinki, and the Hospital Ethics Committees approved the study.
Patient inclusion and data collection
Prospective enrollment occurred between January 2007 and August 2009. All adult patients (equal to or older than 18 years), who were referred to nephrologist-care and had Stage 4 or 5 CKD not receiving dialysis therapy were eligible. After signing informed consent, all patients underwent a baseline examination, and were re-examined after 6, 12, 24 and 36 months.
At each examination, a thorough clinical assessment and routine testing of laboratory markers was performed. The clinical assessment included the recording of demographics, smoking and body size, comorbidity history and ongoing medication. During the follow-up examinations, patient status and hospitalizations were also recorded. Follow-up continued until death, commencement of dialysis or pre-emptive transplantation, loss to follow-up or 36 months from study entry. Patients who started dialysis therapy or were transplanted or lost to follow-up were included in analyses to the point of study discontinuation. As per protocol, all patients starting chronic renal replacement therapy were followed over the first 30 days of dialysis initiation, recalculating their final status as “death” if it occurred during that period.
Standardized data collection was ensured and conducted by nephrologists using internet-based electronic case report forms. The data collected in each center was anonymized and then centralized by the study coordinators. When inconsistencies were identified, the coordinators contacted the reporting centers for verification and/or correction. Each investigator was advised to adhere strictly to best practice guidelines and clinical recommendations.
Study exposure
The study exposure was the serum levels of calcium, phosphate and intact PTH (iPTH), both at baseline and as a time-dependent exposure with repeated measures every 6 months. Calcium levels were corrected using the following formula: Corrected calcium (mg/dL) = measured total calcium (mg/dL) + 0.8 [4.0 − serum albumin (g/dL)], according to KDIGO guideline recommendations [8]. All laboratory evaluations were performed according to the routine methods of the laboratory departments at each center. iPTH levels were assessed by an automated 2nd generation electrochemiluminescence immunoassay. The Elecsys assay (Roche Diagnostic) was used in 10 of the 12 centers, accounting for 91% (n = 866) of the patients included in the study. The Advia Centaur (Bayer) and the Immulite 2500 Intact PTH (Siemens) assays were used in two centers, which enrolled 6% (n = 55) and 3% (n = 28) of patients, respectively.
Study outcomes
The primary outcome was all-cause mortality. The secondary outcome was cardiovascular mortality, defined as death attributable to myocardial ischemia and infarction, heart failure, cardiac arrest because of other or unknown cause, cerebrovascular disease (stroke), or peripheral vascular disease.
Study covariates
Other study covariates were age, sex, comorbidities, ongoing medications, anthropometric measurements, and laboratory tests. Comorbidities registered in our study forms were diabetes mellitus, smoking status, and cardiovascular disease history prior to enrollment. Current medication recorded during each study visit included phosphate binding agents (PBAs), vitamin D compounds, erythropoiesis stimulating agents (ESAs), oral or i.v. iron, and antihypertensives. Other retrieved laboratory parameters were: serum levels of creatinine, sodium, potassium, bicarbonate, albumin, C reactive protein (CRP), and blood cell count. 24-h urine tests included urinary volume, urea, creatinine, sodium, and protein. Estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI formula [15].
Statistics
According to the information obtained from the literature, annual mortality in patients with non-dialysis CKD stages 4 and 5 is around 8% [16]. Approximately 45% of this population is estimated to show hyperphosphatemia, defined by phosphate levels higher than 4.6 mg/dL [17]. Several studies have analyzed the influence of phosphate levels on the mortality of non-dialysis CKD patients, showing an 80% increase in mortality in the group of patients with hyperphosphatemia [18]. With a minimum follow-up of three years, assuming losses of 20% and considering an error of beta = 0.8, it is estimated that the initial inclusion of at least 918 patients is required in order to find significant mortality differences between groups with and without hyperphosphatemia.
Categorical variables are presented as percentage and continuous variables as mean ± SD or median (interquartile range), where appropriate. Missing values were replaced by the last measured value (last observation carried forward) [14]. Differences in the characteristics of patients were assessed with one-way analysis of variance for continuous variables and chi-squared test for categorical variables.
Time-dependent Cox proportional hazards regressions were used to assess the association between Ca, P and PTH on all-cause and cardiovascular mortality. The exposure variables (serum levels of phosphate, calcium and PTH at each visit) were introduced in the Cox models as continuous variables and fitted by using non-linear p-splines [19]. All Cox models were stratified by center. The optimal degree of smoothness was selected using the Akaike Information Criterion.
Three different multivariate models were used for adjustment: Model 0 (crude) included each of the parameters, calcium, phosphate and iPTH, separately. Model 1 included adjustment for demographic, anthropometric characteristics and co-morbidities: age, sex, BMI, waist circumference, cardiovascular comorbidity, diabetes, and blood pressure. Model 2 included the variables of Model 1 plus medications: prescription of vitamin D, PBAs, iron and ESAs. Similarly, Model 3 (full model) was adjusted for all previous variables plus laboratory parameters: serum levels of calcium, phosphate, iPTH, eGFR, albumin, hemoglobin, CRP and potassium, and proteinuria. All variables included were modeled as time-varying throughout every six-month patient visits, including the patient identifier as a cluster variable to account for correlated observations within each patient.
The serum values of calcium, phosphate and PTH with the minimum log hazard ratio (HR) were used as reference (HR = 1.0). Following previous studies [13, 14], the lowest mortality risk ranges were estimated as serum ranges with a hazard ratio ≤ 1.1 (≤ 10% increase in the relative risk of mortality). Afterwards, the serum values of all patients were categorized as below, within and above the lowest mortality risk ranges, and the association of these categories with mortality was assessed. Serum categories were used as time-varying variables, and the reference (HR = 1.0) was the serum values within the estimated ranges. Crude and adjusted relative mortality risks were calculated by using the same three multivariate models described above.
Finally, taking the baseline risk ranges categories as reference, we additionally evaluated the potential survival benefits of remaining or moving across risk ranges categories during follow-up. To this end, categorical changes from the minimal risk range at baseline to another risk category (moving to below or above the minimal risk range) were analyzed in the same manner as above. Because of the limited number of patients with phosphate levels above minimal risk range at baseline (n = 76), analysis of phosphate category changes was only adjusted for age, using a restricted adjustment model [14]. Due to the low number of patients with phosphate (n = 25) and iPTH (n = 34) below minimal risk range at baseline, we did not perform analyses of changes from these categories.
A p value of < 0.05 was considered significant. All statistical analyses were done using R Statistical Software version 3.0.1 with the “survival” packages (R Foundation for Statistical Computing, Vienna, Austria) [19].
Results
Patient characteristics at enrollment, overall and by CKD-MBD biomarker categories
Of the 995 patients enrolled, 966 had non-missing values for demographics, comorbidity history, ongoing medication, and at least one available value for serum phosphate, total calcium and iPTH, and were included in the analysis (Supplementary Figure S1). No differences between included and excluded patients were observed at baseline (Supplementary Table S1). At inclusion, 707 (73%) patients had CKD Stage 4 and 259 (27%) had CKD Stage 5. Mean age was 69.6 ± 13.7 years, and 61% were men. The baseline characteristics by CKD stage are summarized in Table 1.
Supplementary Tables S2–S4 show the characteristics of patients categorized into terciles of distribution according to baseline serum calcium, phosphate and iPTH levels. Patients in the highest tercile of calcium were older, had lower body mass index (BMI) and albumin levels compared to patients in the lowest tercile, who showed the lowest levels of iPTH. The proportion of patients treated with vitamin D and calcium-free PBAs was higher among patients in the highest calcium tercile (Supplementary Table S2). Patients in the highest tercile of phosphate showed lower eGFR and hemoglobin levels, with a higher proportion of diabetes and treatment with PBAs and ESAs (Supplementary Table S3). Many baseline comorbidities and laboratory parameters varied among the different terciles of serum iPTH (Supplementary Table S4). Patients in the highest tercile were older and showed lower eGFR, albumin and hemoglobin levels, with higher proteinuria. proportion of diabetes and treatment with PBAs and ESAs. The proportion of patients treated with active vitamin D and calcium-free PBAs was higher among patients in the highest iPTH tercile.
Follow-up and outcomes
During median follow-up of 29 months (interquartile range: 13–36 months), a total of 3,183 subsequent 6-month patient visits were recorded (mean: 3.3 visits per patient), together with 181 deaths (19%) and 305 (32%) events of kidney replacement therapy initiation. Most deaths were attributed to cardiovascular causes (n = 95; 53%), followed by infections (n = 25; 14%), tumors (n = 20; 11%), renal death (n = 13; 7%), other (n = 10; 6%) and unknown causes (n = 18; 10%). 297 (31%) patients initiated chronic dialysis and 8 (1%) underwent pre-emptive kidney transplantation. Only 67 (7%) patients were lost to follow-up, and censored at the time point of discontinuation.
Association between calcium levels and risk of mortality
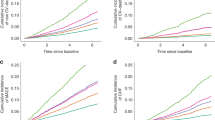
In both crude and minimally adjusted analyses (models 1 and 2), high and low values of calcium were associated with a higher risk for death (Supplementary Figure S2). In the fully adjusted models, however, the association of calcium with all-cause mortality was J-shaped, and only high values were significantly associated with the risk of mortality (Fig. 1a).
Hazard ratios (HR) and 95% confidence intervals (CI) for the risk of mortality associated with time-dependent measurements of a albumin-corrected calcium, b phosphate and c iPTH in patients with CKD stages 4–5. The upper panels at each graph graphically depict the output of a restricted cubic spline analysis with time-dependent exposures. Multivariable adjustment considered demographic and anthropometric characteristics, co-morbidities, medications, and laboratory parameters at each repeated patient visit (full list in the legend of Table 2). Grey boxes show the serum concentration (with 95% CI) associated with the lowest risk of mortality. Horizontal dashed lines indicate the minimal risk range of mortality (HR ≤ 1.1). The lower panels show the distribution of calcium, phosphate and iPTH measurements
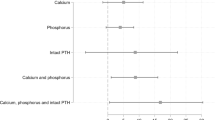
The calcium levels associated with the minimum relative risk of mortality (HR = 1.0) was found at 9.5 mg/dL, being ≤ 10.5 mg/dL the calcium range associated with the lowest risk (HR ≤ 1.1) in the fully adjusted model (p = 0.043 for the joint significance of the polynomial terms) (Table 2). The 95% CI for high serum calcium was wide (Fig. 1a), and only 2% of patients were above the lowest risk range for calcium (Fig. 2), not allowing to detect a significant association between survival and calcium values above the > 10.5 mg/dL threshold (Table 2). For cardiovascular mortality, the lowest mortality risk in the fully adjusted model was 9.3 mg/dL, with the lowest risk ranging from 8.5 to 10.0 mg/dL (p = 0.007), although values below or above this threshold only tended to be associated with a higher cardiovascular mortality risk (Supplementary Table S5).
Association between phosphate levels and risk of mortality
In both crude and adjusted models, the association between phosphate levels and mortality was U-shaped (Fig. 1b and Supplementary Figure S3). The serum values associated with the minimum risk of mortality were 3.8 mg/dL, being the lowest risk range between 2.8 and 5.0 mg/dL (p = 0.027) (Table 2). At baseline, 3%, 89% and 8% of patients were found to be below, within and above this range, respectively (Fig. 2). Phosphate values above the lowest risk range were associated with a higher relative risk of mortality, whereas serum levels below this range did not reach statistical significance (Table 2). For cardiovascular mortality, the phosphate levels associated with the minimum relative risk were reduced to 2.1 mg/dL, being the lowest risk range between 2.1 and 4.4 mg/dL (p < 0.001) in the fully adjusted model. As shown with all-cause mortality, only phosphate values above these ranges were associated with a higher relative risk of cardiovascular mortality (Supplementary Table S5).
Association between iPTH levels and risk of mortality
In both crude and adjusted models, high and low values of iPTH were associated with a higher risk for all-cause mortality (Fig. 1c and Supplementary Figure S4). The minimum risk of mortality was found at 70 pg/mL, with the lowest mortality risk ranging from 38 to 112 pg/mL (p = 0.008) (Table 2). At baseline, 4%, 36% and 61% of patients were found to be below, within and above this range, respectively (Fig. 2). iPTH values above the lowest risk range were associated with a higher relative risk of mortality (Table 2). An increased risk was also observed for iPTH values below the lowest risk range, but this did not reach statistical significance.
Lowest risk ranges for cardiovascular mortality did not differ markedly, being 62 pg/mL the iPTH value associated with the minimum relative risk of mortality, with a lowest range between 34 and 109 pg/mL (p = 0.008) in the fully adjusted model. As for all-cause mortality, only iPTH values above these ranges were associated with a higher relative risk of cardiovascular mortality (Supplementary Table S5).
Association between changes in serum calcium, phosphate and iPTH categories and risk of mortality
Figure 2 summarizes the percentage of patients within the lowest mortality risk ranges for each serum biochemical parameter at baseline. Maintaining optimal ranges for both phosphate and PTH levels was related to better survival. In patients with baseline serum phosphate and iPTH values above the lowest mortality risk ranges (> 5.0 mg/dL for serum phosphate, > 112 mg/dL for iPTH levels), the reduction in serum phosphate or iPTH towards the lowest range (2.8–5.0 mg/dL for serum phosphate, 38–112 pg/mL for iPTH levels), was associated with a subsequent lower risk of mortality (Table 3). Conversely, in patients with baseline serum phosphate or iPTH values within the lowest mortality range, increases in the phosphate or iPTH levels were associated with a higher risk of mortality, although statistical significance was not reached for iPTH. The proportion of patients outside the minimal risk range for calcium at baseline (> 10.5 mg/dL) was very low (Fig. 2), and no survival associations were observed when moving to lower calcium categories (Table 3). Similarly, in patients with baseline serum calcium within the lowest mortality range (≤ 10.5 mg/dL), increases in serum calcium did not show significant association with the mortality risk.
Discussion
We believe this is the largest and longest prospective study evaluating the association between CKD-MBD parameters and survival in patients with non-dialysis dependent CKD stages 4–5. In line with what has been reported for patients on dialysis [13, 14], we found that high calcium levels, as well as low and high phosphate and iPTH levels, were associated with the risk of mortality. We report ranges in which the lowest mortality risk was observed, and that transitioning to a higher or a lower risk range over time consequently predicted the risk of mortality. In the absence of trial evidence, our results may inform clinical decisions on when to initiate or intensify therapeutic strategies to control CKD-MBD disorders in advanced CKD.
The lowest risk value and minimal risk range observed for serum calcium (9.5 mg/dL, range ≤ 10.5 mg/dL) agree with those suggested by KDIGO guidelines [8], where avoidance of hypocalcemia is advocated, and with previous studies. In a historic cohort of 1,243 men with NDD-CKD, Kovesdi et al. observed non-linear associations between time-averaged serum calcium and mortality, with higher risk seen with higher calcium levels. [20]. However, most of the patients included in the study (67%) were in CKD stages 1–3 and hypercalcemia is typically uncommon at that early stage, limiting their inferences on risk associations at high calcium ranges.
Our observed lower risk value and minimal risk range for phosphate (3.8 mg/dL, range 2.8–5.0 mg/dL) are also consistent with KDIGO recommendations of lowering serum phosphate “towards normal” (i.e. 2.8–4.7 mg/dL) [8], while they largely confirm previous studies on phosphate as an independent risk factor for mortality in NDD-CKD patients [4,5,6,7, 21, 22].
This said, the observed lower risk value and minimal risk range for iPTH (70 pg/mL, range 38–112 pg/mL) are novel. Due to a dearth of data on clinical outcomes, current KDIGO guidelines indicate that the optimal PTH level in patients with CKD 4–5 not on dialysis is not known, and suggest, somewhat ambiguously, that patients with levels of iPTH progressively rising or persistently above the upper normal limit for the assay be evaluated for modifiable factors. However, they do suggest maintaining iPTH levels in the range of approximately 2–9 times the upper normal limit for the assay in dialysis patients [8], whereas we know that higher iPTH levels are associated with cardiovascular events in the general population, in those whose optimal iPTH levels should be below the upper limit of normal (in the laboratory) [23]. Thus, somewhere around CKD stages 3 to 5 there should be a transition point between these recommendations [24]. Our data can contribute to fill this void of evidence and they correspond well with the ranges recommended by other guidelines [25, 26], which conclude that a modest degree of hyperparathyroidism represents an appropriate adaptive response to declining kidney function, due to its phosphaturic effects and increasing bone resistance to PTH to maintain a normal bone remodeling rate in the setting of CKD. The association between higher iPTH levels and mortality agrees with a recent cohort study of 536 CKD patients with eGFR between 89 and 15 ml/min/1.73 m2 [27]. In contrast, Fouque et al. failed to show a relationship between serum iPTH and mortality in a prospective study which included 719 adult patients with non-dialysis Stage 4 or 5 CKD [28], which we attribute to the fact that those analyses assumed the association to be linear. Because of that, we regard our use of penalized splines smoothing analyses as a strength in our report [29].
Another key finding of our study is the independent association between maintaining biochemical parameters towards lowest risk ranges during the 3-year follow-up with a lower relative risk of mortality. It was especially demonstrated for the group of patients above the lowest risk ranges for serum phosphate and iPTH above ranges, which also represented the two conditions associated with a higher risk of mortality. Although no survival benefit could be observed when patients with hypercalcemia at baseline moved into the minimal risk category, we speculate that the limited number of subjects in this group of patients may have reduced the statistical power for detecting significant associations with mortality, as previously noted [13, 14]. Taken together, our data illustrate the potential benefits of controlling these three main CKD-MBD biochemical parameters in patients with NDD-CKD, and provide clinicians with a rationale to guide their routine clinical practice in the absence of randomized clinical trials which may be unlikely to be performed [10].
The assessment of CKD-MBD as a factor for cardiovascular mortality was a secondary aim of this study. Lowest risk ranges for this outcome did not differ markedly for all three parameters, showing a mild reduction in the levels associated with the minimum relative mortality risk. Several mechanisms might explain the increased mortality associated with abnormalities in CKD-MBD biochemical markers. High calcium levels have been linked to vascular calcification, adynamic bone disease and immobility [17, 30, 31]. In addition to the calcification-inducing effects on the vessels [4, 32, 33], phosphate could increase mortality by other mechanisms, such as through fibroblast Growth Factor-23 that has been implicated in the pathogenesis of atherosclerosis and myocardial hypertrophy [34, 35]. Lastly, abnormal levels of iPTH have been implicated in the pathogenesis of left ventricular myocardial function, cardiac fibrosis, vascular calcification, and bone remodeling [36].
The strengths of PECERA reside in the relatively large sample size, prospective data collection and long period of follow-up, with high events rate and minimal loss of follow-up. However, we are limited by the observational nature of our analysis and may still be unpowered for evaluating minimal risk ranges. Thus, confirmation in other independent and preferably geographically and ethnically diverse cohorts is necessary to increase generalizability. The low proportion of patients not receiving CKD-MBD related medications prevented us from investigating the association between spontaneous changes in the laboratory parameters and mortality. Although laboratory parameters were evaluated at each center, most iPTH levels were assessed by the same assay, improving the comparability of the results of the study.
To conclude, we found a non-linear association of serum calcium, phosphate and iPTH levels with mortality in stage 4 and 5 CKD patients. Whereas the ranges of calcium and phosphate associated with the lowest mortality in the study were consistent with the current KDIGO targets, our observed PTH thresholds were lower than currently recommended. All these data suggest potential survival benefits for controlling bone mineral parameters in thispopulation, as previously reported for dialysis patients.
References
Bellorin-Font E, Vasquez-Rios G, Martin KJ (2019) Controversies in the management of secondary hyperparathyroidism in chronic kidney disease. Curr Osteoporos Rep 17(5):333–342. https://doi.org/10.1007/s11914-019-00533-x
Bover J, Ureña-Torres P, Mateu S et al (2020) Evidence in chronic kidney disease-mineral and bone disorder guidelines: is it time to treat or time to wait? Clin Kidney J. https://doi.org/10.1093/ckj/sfz187 ([published online ahead of print, 2020 Jan 15])
Evenepoel P, Rodriguez M, Ketteler M (2014) Laboratory abnormalities in CKD-MBD: markers, predictors, or mediators of disease? Semin Nephrol 34(2):151–163. https://doi.org/10.1016/j.semnephrol.2014.02.007
Evenepoel P, Bover J, Ureña-Torres P (2016) Parathyroid hormone metabolism and signaling in health and chronic kidney disease. Kidney Int 90(6):1184–1190
Felsenfeld AJ, Levine BS, Rodriguez M (2015) Pathophysiology of calcium, phosphorus, and magnesium dysregulation in chronic kidney disease. Semin Dial 28(6):564–577
Fernández-Martín JL, Martínez-Camblor P, Dionisi MP et al (2015) Improvement of mineral and bone metabolism markers is associated with better survival in haemodialysis patients: the COSMOS study. Nephrol Dial Transplant 30(9):1542–1551
Fouque D, Roth H, Darné B et al (2018) Achievement of 2009 and 2017 kidney disease: improving global outcomes mineral and bone targets and survival in a French cohort of chronic kidney disease stages 4 and 5 non-dialysis patients. Clin Kidney J 11(5):710–719
García-Canton C, Bosch E, Ramírez A et al (2011) Vascular calcification and 25-hydroxyvitamin D levels in non-dialysis patients with chronic kidney disease stages 4 and 5. Nephrol Dial Transplant 26(7):2250–2256
Górriz JL, Molina P, Bover J et al (2013) Characteristics of bone mineral metabolism in patients with stage 3–5 chronic kidney disease not on dialysis: results of the OSERCE study. Nefrologia 33(1):46–60
Górriz JL, Molina P, Cerverón MJ et al (2015) Vascular calcification in patients with nondialysis CKD over 3 years. Clin J Am Soc Nephrol 10(4):654–666
Gutiérrez OM, Januzzi JL, Isakova T, Laliberte K, Smith K, Collerone G et al (2009) Fibroblast growth factor 23 and left ventricular hypertrophy in chronic kidney disease. Circulation 119:2545–2552
Hill AB (2015) The environment and disease: association or causation? 1965. J R Soc Med 108(1):32–37
Isakova T, Cai X, Lee J et al (2020) Longitudinal evolution of markers of mineral metabolism in patients with CKD: the chronic renal insufficiency cohort (CRIC) study. Am J Kidney Dis 75(2):235–244. https://doi.org/10.1053/j.ajkd.2019.07.022
Kestenbaum B, Sampson JN, Rudser KD et al (2005) Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol 16(2):520–528
Kestenbaum B, Sampson JN, Rudser KD, Patterson DJ, Seliger SL, Young B, Sherrard DJ, Andress DL (2005) Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol 16(2):520–528. https://doi.org/10.1681/ASN.2004070602
Khan AM, Chirinos JA, Litt H, Yang W, Rosas SE (2012) FGF-23 and the progression of coronary arterial calcification in patients new to dialysis. Clin J Am Soc Nephrol 7:2017–2022
Kidney Disease :Improving Global Outcomes (KDIGO) CKD-MKD Update Work Group (2017) KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 7(1):1–59
Kovesdy CP, Kalantar-Zadeh K (2008) Bone and mineral disorders in pre-dialysis CKD. Int Urol Nephrol 40(2):427–440
Kovesdy CP, Anderson JE, Kalantar-Zadeh K (2010) Outcomes associated with serum phosphorus level in males with non-dialysis dependent chronic kidney disease. Clin Nephrol 73(4):268–275
Kovesdy CP, Kuchmak O, Lu JL, Kalantar-Zadeh K (2010) Outcomes associated with serum calcium level in men with non-dialysis-dependent chronic kidney disease. Clin J Am Soc Nephrol 5(3):468–476
Lamina C, Kronenberg F, Stenvinkel P et al (2020) Association of changes in bone mineral parameters with mortality in haemodialysis patients: insights from the ARO cohort. Nephrol Dial Transplant 35(3):478–487
Levey AS, Stevens LA, Schmid CH, for the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Levin A, Bakris GL, Molitch M et al (2007) Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 71(1):31–38
Malloy EJ, Spiegelman D, Eisen EA (2009) Comparing measures of model selection for penalized splines in Cox models. Comput Stat Data Anal 53:2605–2616
Melamed ML, Buttar RS, Coco M (2016) CKD-mineral bone disorder in stage 4 and 5 CKD: what we know today? Adv Chronic Kidney Dis 23(4):262–269
Menon V, Greene T, Pereira AA et al (2005) Relationship of phosphorus and calcium-phosphorus product with mortality in CKD. Am J Kidney Dis 46(3):455–463. https://doi.org/10.1053/j.ajkd.2005.05.025
O’Hare AM, Bertenthal D, Covinsky KE, Landefeld CS, Sen S, Mehta K, Steinman MA, Borzecki A, Walter LC (2006) Mortality risk stratification in chronic kidney disease: one size for all ages? J Am Soc Nephrol 17(3):846–853
Palmer S, Hayen A, Mackaskill P et al (2011) Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA 305(11):1119–1127
Seiler-Mussler S, Limbach AS, Emrich IE et al (2018) Association of nonoxidized parathyroid hormone with cardiovascular and kidney disease outcomes in chronic kidney disease. Clin J Am Soc Nephrol 13(4):569–576. https://doi.org/10.2215/CJN.06620617
Seng JJB, Tan YLC, Lim RW et al (2018) Prevalence and risk factors for hypercalcemia among non-dialysis patients with chronic kidney disease-mineral and bone disorder. Int Urol Nephrol. 50(10):1871–1877
Therneau TM, Grambsch PM (2000) The cox model. In: Modeling survival data: extending the cox model statistics for biology and health. Springer, New York, p 39–77. . https://doi.org/https://doi.org/10.1007/978-1-4757-3294-8_3(ISBN 0-387-98784-3)
Torregrosa JV, Cannata-Andia J, Bover J et al (2008) Recommendations of the Spanish Society of Nephrology for managing bone-mineral metabolic alterations in chronic renal disease patients. Nefrologia 28(Suppl 1):S1-22
van Ballegooijen AJ, Reinders I, Visser M, Brouwer IA (2013) Parathyroid hormone and cardiovascular disease events: a systematic review and meta-analysis of prospective studies. Am Heart J 165(5):655-664.e6645. https://doi.org/10.1016/j.ahj.2013.02.014
Voormolen N, Noordzij M, Grootendorst DC et al (2007) High plasma phosphate as a risk factor for decline in renal function and mortality in pre-dialysis patients. Nephrol Dial Transplant 22(10):2909–2916. https://doi.org/10.1093/ndt/gfm286
Voormolen N, Noordzij M, Grootendorst DC, PREPARE study group et al (2007) High plasma phosphate as a risk factor for decline in renal function and mortality in pre-dialysis patients. Nephrol Dial Transplant. 22(10):2909–2916. https://doi.org/10.1093/ndt/gfm286
Watanabe R, Lemos MM, Manfredi SR, Draibe SA, Canziani ME (2010) Impact of cardiovascular calcification in nondialyzed patients after 24 months of follow-up. Clin J Am Soc Nephrol 5(2):189–194
Acknowledgements
The PECERA study was sponsored by the Valencian Society of Nephrology, the Spanish Society of Nephrology, and the Tomás de Osma Renal Foundation. Logistics (meetings, developing of Web site for data entry, etc.) were financially supported by Abbott, Hoffmann-La Roche, and Boehringer Ingelheim. The authors wish to thank all the co-investigators and participating centers of the PECERA study: MD Albero (Hospital Virgen de los Lirios. Alcoy), L Álvarez (Hospital Virgen de los Lirios. Alcoy), A Antolín (Hospital Francesc de Borja), MA Aparicio (Hospital de la Ribera), E Bea (Hospital de la Ribera), S Bea (Hospital General Universitario de Valencia), Y Blanco (Hospital de la Ribera), C Climent (Hospital Francesc de Borja), C Del Pozo (Hospital Virgen de los Lirios. Alcoy), JE Fernández-Nájera (Hospital de Manises), C García-Aparicio (Hospital de Villajoyosa), A García Hervás (Hospital Universitari Dr Peset), E Garrigós (Hospital Universitario La Fe), M González-Rico (Hospital Clínico Universitario de Valencia), JL Górriz (Hospital Clínico Universitario de Valencia), JM Graña (Hospital de la Ribera), R López-Menchero (Hospital Virgen de los Lirios), J Martín-Rivas (Hospital de Elda), P Molina (Hospital Universitari Dr Peset), C Montoyo (Hospital de la Marina Alta. Denia), E Muñoz de Bustillo (Hospital de Villajoyosa), LM Pallardó (Hospital Universitari Dr Peset), A Peris (Hospital Universitario La Fe), F Ramos (Hospital de Denia), L Sánchez (Hospital Virgen de los Lirios. Alcoy), MP Sánchez-Pérez (Hospital Universitario La Fe), A Soldevila (Hospital Universitario La Fe), J Torralba (Hospital General Univesitario de Alicante), V Valverde (Hospital de Elda).
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed important intellectual content during manuscript drafting or revision and accept accountability for the overall work. The individual contribution of each co-author is as follows: research idea and study design: JLG, LMP, PM, MPS; patient recruitment and clinical information gathering: PM, JLG, JT, VE, LA, AP, MPS, MG, MJP, JEF, EG, LD; statistical analysis: MDM, PM, JJC; data analysis/interpretation: PM, MDM, JLG, JJC; supervision and mentorship: JLG, LMP, JJC.
Corresponding author
Ethics declarations
Conflicts of interest
The results presented in this paper have not been published previously in whole or part, except in abstract format. JJC acknowledges support from the Swedish Research Council (grant number 2019-01059). The authors declare no other conflicts of interest that might be perceived as affecting the objectivity of this study.
Ethics approval
The study was conducted in agreement with the Declaration of Helsinki, and the Hospital Ethics Committees approved the study.
Consent to participate
All patients provided informed consent.
Consent for publication
All authors consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Molina, P., Molina, M.D., Pallardó, L.M. et al. Disorders in bone-mineral parameters and the risk of death in persons with chronic kidney disease stages 4 and 5: the PECERA study. J Nephrol 34, 1189–1199 (2021). https://doi.org/10.1007/s40620-020-00916-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00916-9