Abstract
Urinary tract infection (UTI) represents the most common infection after kidney transplantation; it is associated with an increased risk for acute kidney rejection and impaired graft function in the early post-transplant period. Kidney transplant recipients with UTIs are often clinically asymptomatic due to the immunosuppressive therapy; however, asymptomatic bacteriuria may progress to acute pyelonephritis, bacteremia and urosepsis, particularly in the early post-transplant period, that are independent risk factors for short and long-term graft and patient survival. This article reviews the definitions, incidence, risk factors and the management of UTI in kidney transplant recipients; furthermore, the main controversial and still unanswered questions, regarding the causes of recurrent UTIs, adequate use of antibiotics to avoid antibiotic resistance, dosing and timing for prophylaxis and treatment of symptomatic infections, are also discussed. The emerging definition of urinary microbiota introduces new concepts in understanding the complexity of the disease and might represent the future target for therapeutic interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A urinary tract infection (UTI) is a pathologic invasion of the urothelium with a consequent inflammatory response which is clinically characterized by specific signs and symptoms and caused by an infectious agent (mainly bacterial agents). UTIs are the most important and frequent infection in adults and represent the most common problem in patients with kidney transplantation (KTX) and the incidence in these patients is significantly higher than in the general population [1,2,3]. UTIs not only impacts on the patient’s well-being but also increase the risk of further complications in transplanted patients, particularly related to potential drug interactions, development of resistant bacteria [4] and severe sepsis and potential effect on long-term graft survival and even death [5, 6]. Even a single episode of UTI during the post-transplant period can cause a decrease in graft function, measured as iothalamate GFR [7]. Hence, prevention and early diagnosis of UTIs are important to minimize the risk of life-threatening complications and graft loss [8]. However, the real impact of UTIs in this setting is still under debate and several aspects, such as morbidity and mortality from UTIs are controversial.
This article reviews and updates the main controversial aspects related to UTIs in kidney transplantation, mainly focusing on the prevalence and risk factors in this specific subset of patients, their potential influence on short and long-term graft outcome, as well as treatment and prophylaxis recommendations.
Definitions and epidemiology of UTI
UTIs after kidney transplantation may occur either as asymptomatic bacteriuria or as symptomatic infection [9]. An asymptomatic bacteriuria is defined as the presence of > 105 bacterial colony forming units per milliliter (CFU/ml) on urine culture without local or systemic signs and symptoms [10]. A symptomatic UTI is defined as uncomplicated (presence of > 105 CFU/ml on urine culture with local urinary symptoms, such as dysuria, urgency, but without systemic symptoms) or complicated if the urinary symptoms are associated with systemic ones (allograft pain, fever, chills) [7, 10, 11]. Guidelines define sporadic (less than three episodes/year) or recurrent (more than three episodes/year) UTIs according to the frequency of episodes [9]. Conventionally, a classification based on the severity of UTIs has been proposed by European Association of Urology and distinguishes six different severity grades of infection [cystitis, mild-moderate pyelonephritis, severe pyelonephritis, systemic inflammatory response syndrome (SIRS), severe urosepsis and uroseptic shock] (Table 1) [9].
The prevalence of UTIs in renal allograft recipients is extremely various among studies, ranging from 23 to 75% [3, 12], and accounting for about 40–50% of all infectious complications [13]. This may be ascribed to differences across studies in terms of population characteristics, definitions and diagnostic criteria, centre-specific antibiotic strategies and duration of follow-up. Likewise, the incidence of UTIs after KTX has been estimated to vary across the studies. Many authors reported that infections are more likely to occur in the early post-transplant period, particularly in the first year (74%) [13], while the incidence of UTIs decreases to about 35% during the second year and further to 21% at four post-transplant years [14]. The development of early UTIs is probably related to the surgical trauma, the placement of urinary catheter and ureteral stent, as well as to the higher level of immunosuppression in this post-transplant period. By contrast, Senger et al. showed that in a prospective cohort of kidney transplant recipients only < 30% developed UTIs within the first 3 months [15]. Similarly, a retrospective study of 28,942 kidney transplant recipients in the USA, described a cumulative incidence of early UTIs of 17% in the initial 3 months [16].
Microbiology
UTIs after KTX is usually caused by gram-negative organisms, accounting for more than 70% and Escherichia coli is the most common causative organism in the general population, as well as in kidney transplantation (30–80%) [14, 17]. Klebsiella, Pseudomonas aeruginosa, and Proteus are other gram-negative bacteria frequently isolated. However, the widespread use of antibiotics in preventing infections or treatment of asymptomatic bacteriuria in kidney transplant recipients has led to a significant increase in resistance to common antibiotics, like trimethoprim-sulfamethoxazole (TMP-SMX) and fluoroquinolones, and caused an increase of infections due to multidrug resistant (MDR) and extensively-drug-resistant (XDR) pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter spp.) [15, 18, 19]. Recently, Korth et al. reported a significant increase in antimicrobial resistence of Klebiella spp. to TMP-SMX, ciprofloxacin and ceftazidime from 2009 to 2012 [20]. Emergence of MDR pathogens, extended-spectrum β-lactamases (ESBL)- and carbapenemase-producting organisms has been the most important threat in KTX and may be associated with a poorer short- and long-term prognosis [21, 22]. Gram-positive pathogens (Streptococcus species, Staphylococcus saprophyticus) are less frequent cause of UTIs. Candida species are the most common fungal cause of UTIs in KTX, occurring in about 11% of renal transplant recipients [23]. Since these infections are often asymptomatic, there are no diagnostic tests to differentiate infection from colonization in patients with candiduria. However, candiduria may uncommonly have serious complications, leading to ascending infections, candidemia and obstructing fungal balls at the ureterovescical junction, with a significant impact on graft and patient survival [24].
Risk factors for UTIs
Risk factors for UTI in KTX are similar to those in the general population as shown in Fig. 1. Female gender is a well-known risk factor for UTIs in the post-transplant period [3, 10, 25] and this is due to the anatomical features of the urinary tract. On the other hand, many authors did not find any gender difference in the incidence and frequency of UTIs in the post-transplant period [18, 26]. Conflicting results have been reported on the association between older age and frequency of UTIs. A higher infection occurrence is generally found in elder kidney transplant recipients [27, 28]; Chaung et al. showed that 55% of patients aged > 60 years developed UTIs compared to only 30% in the younger group [25]. By contrast, other studies did not show significant correlation between age and UTI occurrence [29,30,31]. An impaired immune system, the low tolerance to immunosuppression and other concurrent co-morbidities are the main determinants of the increased risk for UTIs observed in older transplant recipients. A number of recipient co-morbidities and factors, such as diabetes mellitus, polycystic kidney disease, uropathies and poor hygiene, have been indicated as significant risk factors for UTI [3, 16, 25]. Patients with chronic kidney disease (CKD) are typically characterized by alterations in host protective functions and functional disorders of the urinary tract: the loss of antibacterial properties of the urine, the reduction of the production of protective mucosa in the urothelium and the immunosuppression in the setting of uraemia and KTX are the main reasons for the higher risk of UTIs [32].
Transplant-related factors might also be associated with an increased risk for UTI, as for example the type of donor (living or deceased), episodes of delayed graft function (DGF), acute rejection, cytomegalovirus infection, and urological complications (duration of catheterisation and stenting, vescicoureteric reflux) [33]. In a recent meta-analysis of 13 studies that evaluated the prevalence and risk factors for UTIs, more than one-third of patients had at least one episode of UTI after KTX. Female gender, older recipient age, long duration of catheterisation, acute rejection episodes and cadaveric donor were significantly associated with an increased risk for UTI [34].
Finally, the type of immunosuppression is strongly related to the development of UTI. It is well known that immunosuppression may influence the resistance of enterococcal spp. to β-lactam-based antibiotics affecting the expression of penicillin-binding proteins (PBPs). Many studies showed that azathioprine [25], mycophenolate mofetil [25, 31] and anti-thymocyte globulin [3] are associated with higher rate of UTIs in the post-transplant period, while other drugs (calcineurin inhibitors, everolimus) seems not to affect the risk; moreover, steroid withdrawal did not have any effect on the risk of UTI [35]. In a cohort of patients with chronic allograft nephropathy commenced on mycophenolate for calcineurin inhibitors withdrawal, Hanvesakul et al. showed a significant increase in infections after conversion (26.7% vs 66.6%, p < 0.0005), especially for both urinary tract and respiratory tract infections [36]. Although several studies showed no differences between calcineurin inhibitors, β-lactam-based antibiotics seem to be more effective in tacrolimus-based immunosuppression [37].
Pathogenesis of UTIs: bacteria virulence and host defence mechanisms
UTIs are tipically related to the presence of uropathogenic bacteria ascending to the bladder from the urethra (ascending route). Uropathogens initially adhere to and colonize urothelium of the distal urethra; then, up to 50% of infections may ascend into the upper urinary tracts and bacteria reach the renal pelvis, penetrate the renal parenchyma leading to pyelonephritis. The heamatogenous route is more frequent than in healthy individuals because of immunosuppression. Bacteria virulence factors play a significant role in the invasion of the urothelium. Adherence of micro-organisms is related to the presence of specific adhesins found on the surface of bacterial membrane [38]. Adhesins are surface glycoproteins that work as ligands for specific glycoprotein and glycolipid receptors on uroepithelial cells. After penetrating the cell membrane, uropathogens proliferate within the cytosol to form cluster [39]; furthermore, bacteria develop specific protective structures, as biofilm matrix, that allow them to change their phenotypes and avoid host’s immune response [40]. Overall, these processes stimulate epithelial cells to produce proinflammatory factors leading to an inflammatory response.
In this setting, several host defence mechanisms may also play a pathogenic role in UTIs onset, particularly in the transplant setting, including alterations in vaginal mucosa in female recipients, regular bladder emptying, urine flow, specific urine characteristics, such as high concentration of urea, that inhibits bacterial growth [41]. Other urine conditions that increase the susceptibility to pathogens are urinary pH between 6 and 7, glicosuria, idiopathic hypercalciuria and elevated urinary iron [32]. The absence of a sphincter between the transplanted ureter and the native bladder can increase the risk of transplant pyelonephritis: furthermore, ureteral stents placed during transplantation and the presence of renal cysts in patients with history of polycystic disease may predispose patients to develop recurrent UTIs [10, 11, 25]. Innate immunity represents a first line of defence against the invasion of urinary pathogens, counteracting the penetration of microrganisms into urethelial cells. Numerous cell types such as neutrophils, macrophages, natural killer cells are activated as the uropathogen invades, mediating several effects to limit pathogens penetration and damage. Several studies showed that specific genetic backgrounds are implicated in recurrence and persistence of UTIs and genetic variations of innate immunity modifying specific aspects of the immune response can result in a compromised urinary immunity and an higher susceptibility to UTIs [42]. Many of the identified genes are involved in neutrophils function. Interleukin-8 is an inflammatory cytokine promoting neutrophils migration across infected urothelial cells; absence of CXCR1, the interleukin-8 receptor, have been shown to promote bacteremia within the urinary tract. A genetic predisposition to UTIs has been identified in pediatric patients with recurrent pyelonephritis (mutation of CXCR1 gene) and expression of CXCR1 is usually lower in these patients compared with controls [43]. Moreover, patients with asymptomatic bacteriuria carry TLR4 promoter genotype variants that lower TLR4 expression [42]. Finally, a promoter sequence variants that reduce the expression of Irf3, a key transcription factor that controls the TLR4-dependent response to uropathogenic bacteria, has been reported [42].
Impact on short and long-term outcomes
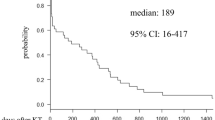
It was long believed that UTIs could be considered “benign” in kidney transplant patients; however, in the recent years, accumulating evidence suggested that UTIs could significantly impact on graft function and long-term outcomes. Although kidney transplant recipients with UTIs are often clinically asymptomatic due to the inability to mount an adequate inflammatory response to infection compared to the general population, UTIs can complicate in acute pyelonephritis (APN) and potential urosepsis, particularly in the early post-transplant period, when the mortality associated to bacteremia is higher [13, 14, 44]. Infections are the main indication for emergency department admission during the early post-transplant period and UTI represents the main cause of sepsis in this setting [45]. While lower UTIs did not affect graft function over the time, post-transplant APN can lead to a decreased graft function and increased mortality [14]. Conflicting results have been reported on late and recurrent post-transplant UTIs; although late UTIs were often considered as benign in the past [46], other studies suggested something different [47]. Abbott et al. found in a large cohort study that the adjusted relative risk for graft failure in patients with late UTIs was 2.35 times higher than in patients without UTI [16]; moreover, recipients who developed septicaemia are at higher risk of death due to cardiovascular events compared to recipients without infections. Pellè et al. confirmed that late UTIs were associated with worse long-term patient survival and APN is an independent risk factor for worse outcomes in KTX [14]. By contrast, in a cohort of kidney transplant recipients with recurrent UTIs, Dupont et al. found that more than 75% of patients have focal renal cortical scarring in a DMSA single-photon emission CT evaluation, independent of the presence of vescicoureteral reflux; however, no significantly different impairment in graft function was found between patients with or without these findings [48]. Recently, in an observational study of 1019 kidney transplant recipients in Kuwait, the Authors found that female gender, older age, thymoglobulin induction, pretransplant urological abnormalities and hepatitis C infection were significant risk factors for recurrent UTIs, but no difference in patient and graft survival was shown between patients with recurrent UTIs and those without UTIs or with no-recurrent UTIs [49]. In both studies, the favorable outcomes for patients with recurrent UTIs have been ascribed to a prompt prophylactic intervention and treatment with intravenous antibiotics to avoid further complications (i.e. sepsis). Finally, in a retrospective study based on 380 patients from our Transplant Center, we demonstrated that recurrent UTIs during the first year post-transplantation is an independent predictor of graft function at 3 years (hazard ratio 2.2; 95% CI 1.3–3.5; p = 0.001) [50]. Hence, the idea of UTIs as “benign” needs to be revised and it seems more reasonable to define each episode of UTI as potentially dangerous for graft and patient survival.
Diagnosis, prophylaxis and treatment of UTI
UTIs can present as either uncomplicated (characterized by urinary signs and symptoms like dysuria, frequency, urgency, hematuria) or complicated UTIs (the signs and symptoms above are associated with those of systemic inflammation, like fever, allograft pain, chills, nausea, fatigue). The diagnosis is based on a positive urine culture with > 105 CFU/ml in presence of clinical symptoms. Patients also present a urine dipstick positive for nitrites, blood, protein, and leukocyte esterase. About 16% of patients with complicated UTIs present also a positive blood cultures [11]. Additional evaluation (renal and bladder ultrasounds, CT scan of urinary tract, cystoscopy, urodynamic studies) should be considered in patients with recurrent UTIs to detect potential structural or functional abnormalities of the urinary tract, stones, complex cysts [51]. Considering the relevant impact on graft outcomes, early detection of UTIs among transplant recipients is important, particularly in the early post-transplant period. Untreated UTIs in the first 3 months post-transplantation have been found to significantly increase the risk of allograft rejection [10]. Most transplant centers routinely screen for asymptomatic bacteriuria and use an antimicrobial prophylaxis within the first 6 months of transplantation to prevent symptomatic UTIs and potential early graft dysfunction [52]. A meta-analysis of six randomized clinical trials in 545 patients, showed that TMP-SMX prophylaxis significantly reduced the risk of sepsis, septicemia by 87% and bacteriuria by 60%, although no differences in graft loss and mortality were reported [53]. However, no consensus is achieved among transplant clinicians on the optimal prophylactic regimen and duration; a prophylaxis with TMP-SMX 160 + 800 mg orally daily is effective and strongly suggested [53]. KDIGO guidelines suggested a prophylaxis based on TMP-SMX for at least 6 months post-transplantation that is helpful even in preventing other opportunistic infections (Pneumocystis) [54]. Long-term prophylaxis has been demonstrated as an effective and inexpensive approach to reduce the incidence of UTIs and sepsis [55]; nevertheless, it is still doubtful whether the long-term antimicrobial prophylaxis could increase the risk of resistance in this subset of patients as already demonstrated in the general population, and consequently affect graft and patient survival [3, 15]. Alternative agents should be used for patients known to be allergic to TMP-SMX (cephalexin, phosphomycin, nitrofurantoin) [53, 54]. Since UTI may not be clinically evident but may evolve to APN, bacteremia, urosepsis and potential risk for allograft rejection [10], a general consensus suggests to treat all transplant recipients with asymptomatic bacteriuria in the first 3 months after transplantation; an initial administration of empiric antibiotics should be followed by a specific antibiotic therapy based on the pathogen and its susceptibility pattern identified in the urine culture. Uncomplicated UTIs may be managed on an outpatient basis and common antibiotics regimes are based on ciprofloxacin 250 mg orally twice daily, levofloxacin 500 mg orally once daily, amoxicillin 500 mg orally three times daily, nitrofurantoin 100 mg orally twice daily [54]. The duration of the therapy should be modulated according to patient’s characteristics and the timing of transplantation (10–14 days treatment in the early post-transplant period, 5–7 days after 6 months) [13] and the dosing must be adjusted in patients with reduced graft function. The suspicion of APN or other complications requires hospitalization and intravenous therapy covering both gram-negative and gram-positive organisms (piperacillin-tazobactam 4.5 g IV every 6 h, meropenem 1 g IV every 8 h, cefepime 1 g IV every 8 h), adjusted for graft function [54]. As for uncomplicated UTI, urine culture samples must be collected before initiating empiric antibiotic treatment and treatment should be modified according to the urine culture results. There is no consensus on optimal duration and general recommendations suggest to treat all patients with complicated UTIs for 14–21 days and a switch to oral treatment may be suggested after the resolution of symptoms [13]. Patients with relapses or recurrent UTIs (more than three episodes in 1 year) should be evaluated for potential predisposing factors (structural and functional abnormalities of the urinary tract) as previously mentioned, and the duration of therapy might be prolonged (up to 3 months); in other cases, patients can be switched to prophylactic antibiotics after a short period of antibiotic treatment [13, 54]. Treatment of patients with asymptomatic candiduria is not universally accepted: many of these patients are treated for the risk of severe graft and patient complications. However, some evidences suggested to discourage this approach, unless the patient is neutropenic or undergoing an urological procedure [24]. The preferred agent is fluconazole, 200–400 mg orally per day per 14 days and adjustment of calcineurin inhibitors dosage may be necessary [21]. Intravenous amphotericin B (0.3–1 mg/kg/day) should be used with caution for its nephrotoxicity, while lipid formulations should be not used given their limited urine concentration. Alternative approaches (flucytosine, voriconazole, echinocandins) can be considered in selected cases, especially in the treatment of transplant pyelonephritis [21].
Challenges in UTIs treatment
Treatment of methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococcus (VRE) infections remain a critical challenge. Pre-transplant colonization is common (about 10%) and transplant recipients are at high risk for MRSA infection due to surgical procedure, ICU stay and immunosuppression [56]. Infection control strategies, including hard hygiene, active surveillance with screening for MRSA before KTX (nasal/cutaneous swab cultures) and decolonization of carriers, are still matter of debate [57]: a typical decolonization protocol includes intranasal application of 2% topical mupirocin twice daily for 5 days combined with chlorhexidine baths for 7 days, while long-term use of antistaphylococcal agents is not recommended for decolonization [57]. Vancomycin is the best choice for the treatment of severe MRSA infections and dosage should be calculated based on actual body weight and renal function: in patients with normal renal function, a dose of 15–20 mg/kg every 8–12 h should be considered with a serum trough concentrations of 15–20 µg/ml. However, vancomycin MIC value ≥ 1.5 µg/ml are strongly predictive of treatment failure; daptomycin, a bactericidal agent, should be considered in complicated MRSA infections and bacteremia at the dose of 6 mg/kg/day in patients with normal renal function [58].
VRE is hystorically considered as low pathogenic; however, VRE colonization and infections have been linked with increased mortality in patients with solid organ transplant [59]. Infection control strategies are pivotal in management of VRE infections; treatment of VRE infections remain a critical clinical situation, as the use of linezolid, quinupristin/dalfopristin (Q/D) and daptomycin is also associated with adverse effects [60]. Meta-analyses showed a modest advantage for linezolid over daptomycin, although the heterogeneity of the studies did not allow definitive conclusions [61].
While MRSA and VRE infections are declining worldwide, MDR/XDR Enterobacteriaceae and MDR/XDR non-fermenters are progressively growing as a cause of infection and represent a global threat [62]. While ESBL-producing E. coli do not need isolation in the majority of cases, ESBL-producing K. pneumoniae and Enterobacteriaceae producing derepressed β-lactamases or carbapenemases may require single-bed isolation and contact precautions: no active surveillance to detect colonization is recommended [63]. Carbapenems are the cornerstone of treatment for MDR Enterobacteriaceae as they are often resistant to quinolones and cotrimoxazole: the use of ertapenem should be preferred as this can downscale the use of imipenem and improve susceptibility of non-fermentative Gram-negative bacteria [64]. A combination of antibiotics is a standard of care in carbapenemase-producing Enterobacteriaceae infections and colistin is the most active agent against these strains [63]. In most cases, combination antibiotic therapy with polymyxin B, tigecycline, aminoglycosides, fosfomycin is an optimal choice [63]. Finally, clinical experience in the treatment of MDR/XDR non-fermatative bacilli (Pseudomonas aeruginosa) is limited; combination therapies using different antibiotic classes on the base of resistance phenotypes (beta-lactam + aminoglycoside ± fluoroquinolone) should be considered for at least 10–14 days [63].
Urosepsis and uroseptic shock
Urosepsis is common in both community-acquired and in hospital associated infections; it is diagnosed when clinical evidence of infection is associated to a systemic inflammatory response (fever, tachycardia, tachypnoea, leukopenia) (Table 1). Severe urosepsis is characterized by the presence of multi organ dysfunction, while uroseptic shock is defined by the persistence of hypotension despite adequate resuscitation approaches and represents the most frequent cause of death for nosocomial infection [9]. Urosepsis treatment requires a combination of adequate life-supporting care, prompt antibiotic therapy and the optimal management of urinary tract disorders; a strong collaboration between urologists, nephrologists, intensive care and infectious disease specialists are required for the best management of these patients [21, 32]. An empirical initial antibiotic treatment should be provided early and adapted on the basis of the culture results later. The antibiotic dosage should be generally higher than in uncomplicated UTIs, but adequately reduced in presence of renal failure. The prompt management of fluid and volume balance, as well as the respiratory support, is crucial in patients with septic shock; the goal is to maintain adequate tissue perfusion, oxygen delivery, stabilization of arterial pressure, effective in reducing mortality among these patients [65]. The most effective preventive measures for urosepsis include isolation of all patients with multi-resistant organisms, early removal of indwelling urethral catheters, reduction of hospital stay, minimization of immunosuppressive therapy. A clinical algorithm for the management of these conditions are reported in Fig. 2. Patients with septic shock are more likely to develop renal failure and require renal replacement therapy in intensive care units: moreover, continuous treatment should be preferred because of the hemodynamic instability. Furthermore, specific extracorporeal therapies for sepsis should be considered: techniques based on adsorption or the combination of plasma filtration and absorption (CPFA) may reduce the deadly systemic inflammatory response in sepsis, improving hemodynamics, stabilizing patients and reducing the severity of disease [66].
Urinary microbiota and non-antibiotic approaches for UTIs
Recent studies suggested that the urinary tract is characterized by a unique specific urinary microbiota, completely different from that of the gut and vagina [41, 67]. As described for the gut, the composition and the balance between certain microbial organisms may have a critical role in the maintenance of health and the development of disease in the urinary tract [67]: in fact, although the urinary microbiota is not fully characterized, differences between patients and healthy volunteers have been linked to several urological diseases [68,69,70]. However, the extent of this relation is still unclear. Several factors have been implicated in changes of urinary microbiota during an individual’s life [71]. Hormonal changes during puberty and adolescence, as well as the sexual activity are associated with changes in the bacterial composition of the urinary microbiota in both men and women [72, 73]. Dietary habits are well known risk factors for UTIs and specific urinary components may have a pivotal role in determining the colonization of the urinary tract. For example, Habash et al. demonstrated that high water intake may lead to the dilution of specific factors that usually inhibits microbial deposition, and this lead to an increased adherence of E. coli and E. faecalis to silicon rubber [74]. Furthermore, drugs, like antibiotics, may significantly alter the microbiota composition, leading to an increased risk for infections [75]. In this scenario, several non-antibiotic options have been proposed for recurrent UTIs in the last years with controversial results [76]. No RCTs supported the utility of urinary alkalinisation with potassium citrate in reducing UTIs symptoms [77]. Probiotic organisms (e.g. Lactobacillus spp.) modulate host defences by reducing pathogen adherence and their ability to cause infections: a Cochrane systematic review did not show significant differences between the probiotic arm and placebo, although the small sample size may limit the significance of this analysis [78]. In post-menopausal women with recurrent UTIs, the use of topical estrogen has been shown to reduce the events of UTIs, improving vaginal atrophia and increasing vaginal lactobacilli [79]. Several evidences suggest the use of cranberry juice for patients with chronic recurrent post-transplant UTIs in order to prevent the adhesion of uropathogenic micro-organisms to the urothelium [80]; however, the role of these products is still controversial, as a recent Cochrane systematic review and meta-analysis points out that cranberry juice is less effective than previously indicated [81]. Moreover, d-mannose have shown promising results in reducing the risk for UTIs, inhibiting the attachment of bacterial type 1 fimbriae to cell surfaces and reducing their ability to infect the host, but its efficacy has not been evaluated in RCTs yet [82].
Finally, it is notable that several UTIs resolve without antibiotic interventions, probably related to the ability to restore the urinary microbiota after the acute infection [83]. If so, why do not all UTIs resolve in this way? Are changes in the urinary microbiota related to this specific pathway and the restore of the urinary microbiota has a pivotal role for IVUs outcomes? These questions are still unanswered and future studies focusing on differences in urinary metabolites in healthy and pathological conditions might help in characterizing urinary microbiota in both conditions and identifying markers of disease. Future alternative therapeutic strategies targeting the urinary microbiota might be useful tools for the correct management of symptoms and reducing the risk for complications.
Conclusions
UTI remains a common and challenging problem in kidney transplantation, affecting both short and long-term outcomes in kidney transplant recipients. Various factors may influence the incidence and severity of UTIs in this particular setting and their recognition is important to identify kidney transplant recipients who are more likely to develop UTIs and therefore minimize the risk with a personalized management (e.g. adequate screening and prophylaxis, avoid overimmunosuppression, etc.). A summary of the current recommendations in the management of UTIs in kidney transplantation is showed in Table 2. However, several issues still need to be addressed: the identification of underlying causes of recurrent UTIs, the role of long-term prophylaxis, the need for treating asymptomatic bacteriuria, careful and selective use of antibiotics to avoid the incidence of MDR/XDR micro-organisms, the dosing and timing for prophylaxis and treatment of symptomatic infections. The lack of definitive answers to these issues strongly highlights the need for future well-planned studies of post-transplant UTIs, focusing on the urinary microbiota and alternative non-antibiotic treatments for UTIs. Due to the complexity of the disease, the identification of a multidisciplinary team (nephrologists, urologists, intensive care and infectious disease specialists) in managing UTIs in transplant centers is strongly recommended.
References
Karuthu S, Blumberg EA (2012) Common infections in kidney transplant recipients. Clin J Am Soc Nephrol 7:2058–2070. https://doi.org/10.2215/CJN.04410512
Rice JC, Safdar N (2009) Urinary tract infections in solid organ transplant recipients. Am J Transplant 9(Suppl 4):S267–S272. https://doi.org/10.1111/j.1600-6143.2009.02919.x
Alangaden GJ, Thyagarajan R, Gruber SA et al (2006) Infectious complications after kidney transplantation: current epidemiology and associated risk factors. Clin Transplant 20:401–409. https://doi.org/10.1111/j.1399-0012.2006.00519.x
Bodro M, Sabe N, Tubau F et al (2013) Risk factors and outcomes of bacteremia caused by drug-resistant ESKAPE pathogens in solid-organ transplant recipients. Transplantation 96:843–849. https://doi.org/10.1097/TP.0b013e3182a049fd
Castaneda DA, Leon K, Martin R et al (2013) Urinary tract infection and kidney transplantation: a review of diagnosis, causes, and current clinical approach. Transplant Proc 45:1590–1592. https://doi.org/10.1016/j.transproceed.2013.01.014
de CR Ferreira, Cristelli F, Paula MP et al (2017) Infectious complications as the leading cause of death after kidney transplantation: analysis of more than 10,000 transplants from a single center. J Nephrol 30:601–606. https://doi.org/10.1007/s40620-017-0379-9
Ariza-Heredia EJ, Beam EN, Lesnick TG et al (2014) Impact of urinary tract infection on allograft function after kidney transplantation. Clin Transplant 28:683–690. https://doi.org/10.1111/ctr.12366
Lorenz EC, Cosio FG (2010) The impact of urinary tract infections in renal transplant recipients. Kidney Int 78:719–721. https://doi.org/10.1038/ki.2010.219
Grabe M, Bjerklund-Johansen TE, Botto H et al (2015) Guidelines on urological infections. European Association of Urology, London
Lee JR, Bang H, Dadhania D et al (2013) Independent risk factors for urinary tract infection and for subsequent bacteremia or acute cellular rejection: a single-center report of 1166 kidney allograft recipients. Transplantation 96:732–738. https://doi.org/10.1097/TP.0b013e3182a04997
Ariza-Heredia EJ, Beam EN, Lesnick TG et al (2013) Urinary tract infections in kidney transplant recipients: role of gender, urologic abnormalities, and antimicrobial prophylaxis. Ann Transplant 18:195–204. https://doi.org/10.12659/AOT.883901
Veroux M, Giuffrida G, Corona D et al (2008) Infective complications in renal allograft recipients: epidemiology and outcome. Transplant Proc 40:1873–1876. https://doi.org/10.1016/j.transproceed.2008.05.065
Saemann M, Horl WH (2008) Urinary tract infection in renal transplant recipients. Eur J Clin Investig 38 (Suppl 2):58–65. https://doi.org/10.1111/j.1365-2362.2008.02014.x
Pelle G, Vimont S, Levy PP et al (2007) Acute pyelonephritis represents a risk factor impairing long-term kidney graft function. Am J Transplant 7:899–907. https://doi.org/10.1111/j.1600-6143.2006.01700.x
Senger SS, Arslan H, Azap OK et al (2007) Urinary tract infections in renal transplant recipients. Transplant Proc 39:1016–1017. https://doi.org/10.1016/j.transproceed.2007.02.060
Abbott KC, Swanson SJ, Richter ER et al (2004) Late urinary tract infection after renal transplantation in the United States. Am J Kidney Dis 44:353–362
Valera B, Gentil MA, Cabello V et al (2006) Epidemiology of urinary infections in renal transplant recipients. Transplant Proc 38:2414–2415. https://doi.org/10.1016/j.transproceed.2006.08.018
Dantas SRPE, Kuboyama RH, Mazzali M, Moretti ML (2006) Nosocomial infections in renal transplant patients: risk factors and treatment implications associated with urinary tract and surgical site infections. J Hosp Infect 63:117–123. https://doi.org/10.1016/j.jhin.2005.10.018
Silva C, Afonso N, Macario F et al (2013) Recurrent urinary tract infections in kidney transplant recipients. Transplant Proc 45:1092–1095. https://doi.org/10.1016/j.transproceed.2013.02.019
Korth J, Kukalla J, Rath P-M et al (2017) Increased resistance of gram-negative urinary pathogens after kidney transplantation. BMC Nephrol 18:164. https://doi.org/10.1186/s12882-017-0580-z
Parasuraman R, Julian K (2013) Urinary tract infections in solid organ transplantation. Am J Transplant 13 (Suppl 4):327–336. https://doi.org/10.1111/ajt.12124
Linares L, Cervera C, Cofan F et al (2007) Epidemiology and outcomes of multiple antibiotic-resistant bacterial infection in renal transplantation. Transplant Proc 39:2222–2224. https://doi.org/10.1016/j.transproceed.2007.06.061
Safdar N, Slattery WR, Knasinski V et al (2005) Predictors and outcomes of candiduria in renal transplant recipients. Clin Infect Dis 40:1413–1421. https://doi.org/10.1086/429620
Fisher JF, Sobel JD, Kauffman CA, Newman CA (2011) Candida urinary tract infections-treatment. Clin Infect Dis 52 (Suppl 6):S457–S466. https://doi.org/10.1093/cid/cir112
Chuang P, Parikh CR, Langone A (2005) Urinary tract infections after renal transplantation: a retrospective review at two US transplant centers. Clin Transplant 19:230–235. https://doi.org/10.1111/j.1399-0012.2005.00327.x
Jung GO, Chun JM, Park JB et al (2008) Clinical significance of posttransplantation vesicoureteral reflux during short-term period after kidney transplantation. Transplant Proc 40:2339–2341. https://doi.org/10.1016/j.transproceed.2008.06.027
Meier-Kriesche HU, Ojo A, Hanson J et al (2000) Increased immunosuppressive vulnerability in elderly renal transplant recipients. Transplantation 69:885–889
Trouillhet I, Benito N, Cervera C et al (2005) Influence of age in renal transplant infections: cases and controls study. Transplantation 80:989–992
Sqalli TH, Laboudi A, Arrayhani M et al (2008) Urinary tract infections in renal allograft recipients from living related donors. Saudi J Kidney Dis Transplant 19:551–553
Memikoglu KO, Keven K, Sengul S et al (2007) Urinary tract infections following renal transplantation: a single-center experience. Transplant Proc 39:3131–3134. https://doi.org/10.1016/j.transproceed.2007.10.005
Kamath NS, John GT, Neelakantan N et al (2006) Acute graft pyelonephritis following renal transplantation. Transplant Infect Dis 8:140–147. https://doi.org/10.1111/j.1399-3062.2006.00148.x
Tandogdu Z, Cai T, Koves B et al (2016) Urinary tract infections in immunocompromised patients with diabetes, chronic kidney disease, and kidney transplant. Eur Urol Focus 2:394–399. https://doi.org/10.1016/j.euf.2016.08.006
Papasotiriou M, Savvidaki E, Kalliakmani P et al (2011) Predisposing factors to the development of urinary tract infections in renal transplant recipients and the impact on the long-term graft function. Ren Fail 33:405–410. https://doi.org/10.3109/0886022X.2011.568137
Wu X, Dong Y, Liu Y et al (2016) The prevalence and predictive factors of urinary tract infection in patients undergoing renal transplantation: a meta-analysis. Am J Infect Control 44:1261–1268. https://doi.org/10.1016/j.ajic.2016.04.222
Pascual J, Galeano C, Royuela A, Zamora J (2010) A systematic review on steroid withdrawal between 3 and 6 months after kidney transplantation. Transplantation 90:343–349. https://doi.org/10.1097/TP.0b013e3181e58912
Hanvesakul R, Kubal C, Jham S et al (2008) Increased incidence of infections following the late introduction of mycophenolate mofetil in renal transplant recipients. Nephrol Dial Transplant 23:4049–4053. https://doi.org/10.1093/ndt/gfn387
Jarzembowski T, Daca A, Witkowski J et al (2013) Changes of PBP5 gene expression in enterococcal isolates from renal transplantation recipients. Biomed Res Int 2013:687156. https://doi.org/10.1155/2013/687156
Mulvey MA (2002) Adhesion and entry of uropathogenic Escherichia coli. Cell Microbiol 4:257–271
Anderson GG, Martin SM, Hultgren SJ (2004) Host subversion by formation of intracellular bacterial communities in the urinary tract. Microbes Infect 6:1094–1101. https://doi.org/10.1016/j.micinf.2004.05.023
Justice SS, Hung C, Theriot JA et al (2004) Differentiation and developmental pathways of uropathogenic Escherichia coli in urinary tract pathogenesis. Proc Natl Acad Sci USA 101:1333–1338. https://doi.org/10.1073/pnas.0308125100
Wolfe AJ, Toh E, Shibata N et al (2012) Evidence of uncultivated bacteria in the adult female bladder. J Clin Microbiol 50:1376–1383. https://doi.org/10.1128/JCM.05852-11
Ragnarsdóttir B, Lutay N, Grönberg-Hernandez J et al (2011) Genetics of innate immunity and UTI susceptibility. Nat Rev Urol 8:449
Lundstedt A-C, McCarthy S, Gustafsson MCU et al (2007) A genetic basis of susceptibility to acute pyelonephritis. PLoS One 2:e825. https://doi.org/10.1371/journal.pone.0000825
Lyerova L, Lacha J, Skibova J et al (2001) Urinary tract infection in patients with urological complications after renal transplantation with respect to long-term function and allograft survival. Ann Transplant 6:19–20
Trzeciak S, Sharer R, Piper D et al (2004) Infections and severe sepsis in solid-organ transplant patients admitted from a university-based ED. Am J Emerg Med 22:530–533
Rao KV, Andersen RC (1988) Long-term results and complications in renal transplant recipients. Observations in the second decade. Transplantation 45:45–52
Schmaldienst S, Dittrich E, Horl WH (2002) Urinary tract infections after renal transplantation. Curr Opin Urol 12:125–130
Dupont PJ, Psimenou E, Lord R et al (2007) Late recurrent urinary tract infections may produce renal allograft scarring even in the absence of symptoms or vesicoureteric reflux. Transplantation 84:351–355. https://doi.org/10.1097/01.tp.0000275377.09660.fa
Tawab KA, Gheith O, Al Otaibi T et al (2017) Recurrent urinary tract infection among renal transplant recipients: risk factors and long-term outcome. Exp Clin Transplant 15:157–163. https://doi.org/10.6002/ect.2016.0069
Pesce F, Martino M, Fiorentino M et al (2019) Recurrent urinary tract infections in kidney transplant recipients during the first-year influence long-term graft function: a single-center retrospective cohort study. J Nephrol. https://doi.org/10.1007/s40620-019-00591-5
Mitra S, Alangaden GJ (2011) Recurrent urinary tract infections in kidney transplant recipients. Curr Infect Dis Rep 13:579–587. https://doi.org/10.1007/s11908-011-0210-z
El Amari EB, Hadaya K, Buhler L et al (2011) Outcome of treated and untreated asymptomatic bacteriuria in renal transplant recipients. Nephrol Dial Transplant 26:4109–4114. https://doi.org/10.1093/ndt/gfr198
Green H, Rahamimov R, Gafter U et al (2011) Antibiotic prophylaxis for urinary tract infections in renal transplant recipients: a systematic review and meta-analysis. Transplant Infect Dis 13:441–447. https://doi.org/10.1111/j.1399-3062.2011.00644.x
(2009) KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant 9 Suppl 3:S1–S155. https://doi.org/10.1111/j.1600-6143.2009.02834.x
Horwedel TA, Bowman LJ, Saab G, Brennan DC (2014) Benefits of sulfamethoxazole-trimethoprim prophylaxis on rates of sepsis after kidney transplant. Transplant Infect Dis 16:261–269. https://doi.org/10.1111/tid.12196
Ziakas PD, Pliakos EE, Zervou FN et al (2014) MRSA and VRE colonization in solid organ transplantation: a meta-analysis of published studies. Am J Transplant 14:1887–1894. https://doi.org/10.1111/ajt.12784
Garzoni C, Vergidis P (2013) Methicillin-resistant, vancomycin-intermediate and vancomycin-resistant Staphylococcus aureus infections in solid organ transplantation. Am J Transplant 13:50–58. https://doi.org/10.1111/ajt.12098
Kullar R, Davis SL, Levine DP et al (2011) High-dose daptomycin for treatment of complicated gram-positive infections: a large, multicenter, retrospective study. Pharmacother J Hum Pharmacol Drug Ther 31:527–536. https://doi.org/10.1592/phco.31.6.527
Russell DL, Flood A, Zaroda TE et al (2008) Outcomes of colonization with MRSA and VRE among liver transplant candidates and recipients. Am J Transplant 8:1737–1743. https://doi.org/10.1111/j.1600-6143.2008.02304.x
Patel R, Gallagher JC (2015) Vancomycin-resistant enterococcal bacteremia pharmacotherapy. Ann Pharmacother 49:69–85. https://doi.org/10.1177/1060028014556879
Chuang Y-C, Wang J-T, Lin H-Y, Chang S-C (2014) Daptomycin versus linezolid for treatment of vancomycin-resistant enterococcal bacteremia: systematic review and meta-analysis. BMC Infect Dis 14:687. https://doi.org/10.1186/s12879-014-0687-9
Yuan X, Liu T, Wu D, Wan Q (2018) Epidemiology, susceptibility, and risk factors for acquisition of MDR/XDR Gram-negative bacteria among kidney transplant recipients with urinary tract infections. Infect Drug Resist 11:707–715. https://doi.org/10.2147/IDR.S163979
Cervera C, van Delden C, Gavaldà J et al (2014) Multidrug-resistant bacteria in solid organ transplant recipients. Clin Microbiol Infect 20:49–73. https://doi.org/10.1111/1469-0691.12687
Sousa D, Castelo-Corral L, Gutierrez-Urbon J-M et al (2013) Impact of ertapenem use on Pseudomonas aeruginosa and Acinetobacter baumannii imipenem susceptibility rates: collateral damage or positive effect on hospital ecology? J Antimicrob Chemother 68:1917–1925. https://doi.org/10.1093/jac/dkt091
Rivers E, Nguyen B, Havstad S et al (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377. https://doi.org/10.1056/NEJMoa010307
Livigni S, Bertolini G, Rossi C et al (2014) Efficacy of coupled plasma filtration adsorption (CPFA) in patients with septic shock: a multicenter randomised controlled clinical trial. BMJ Open 4:e003536. https://doi.org/10.1136/bmjopen-2013-003536
Whiteside SA, Razvi H, Dave S et al (2015) The microbiome of the urinary tract—a role beyond infection. Nat Rev Urol 12:81–90. https://doi.org/10.1038/nrurol.2014.361
Pearce MM, Hilt EE, Rosenfeld AB et al (2014) The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. MBio 5:e01283–e01214. https://doi.org/10.1128/mBio.01283-14
Siddiqui H, Lagesen K, Nederbragt AJ et al (2012) Alterations of microbiota in urine from women with interstitial cystitis. BMC Microbiol 12:205. https://doi.org/10.1186/1471-2180-12-205
Fouts DE, Pieper R, Szpakowski S et al (2012) Integrated next-generation sequencing of 16S rDNA and metaproteomics differentiate the healthy urine microbiome from asymptomatic bacteriuria in neuropathic bladder associated with spinal cord injury. J Transl Med 10:174. https://doi.org/10.1186/1479-5876-10-174
Yatsunenko T, Rey FE, Manary MJ et al (2012) Human gut microbiome viewed across age and geography. Nature 486:222–227. https://doi.org/10.1038/nature11053
Hummelen R, Macklaim JM, Bisanz JE et al (2011) Vaginal microbiome and epithelial gene array in post-menopausal women with moderate to severe dryness. PLoS One 6:e26602. https://doi.org/10.1371/journal.pone.0026602
Gupta K, Hillier SL, Hooton TM et al (2000) Effects of contraceptive method on the vaginal microbial flora: a prospective evaluation. J Infect Dis 181:595–601. https://doi.org/10.1086/315267
Habash MB, Van der Mei HC, Busscher HJ, Reid G (1999) The effect of water, ascorbic acid, and cranberry derived supplementation on human urine and uropathogen adhesion to silicone rubber. Can J Microbiol 45:691–694
Swann JR, Tuohy KM, Lindfors P et al (2011) Variation in antibiotic-induced microbial recolonization impacts on the host metabolic phenotypes of rats. J Proteome Res 10:3590–3603. https://doi.org/10.1021/pr200243t
Barclay J, Veeratterapillay R, Harding C (2017) Non-antibiotic options for recurrent urinary tract infections in women. BMJ 359:j5193. https://doi.org/10.1136/bmj.j5193
O’Kane DB, Dave SK, Gore N et al (2016) Urinary alkalisation for symptomatic uncomplicated urinary tract infection in women. Cochrane Database Syst Rev 4:CD010745. https://doi.org/10.1002/14651858.CD010745.pub2
Schwenger EM, Tejani AM, Loewen PS (2015) Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008772.pub2
Perrotta C, Aznar M, Mejia R et al (2008) Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005131.pub2
Jepson RG, Craig JC (2007) A systematic review of the evidence for cranberries and blueberries in UTI prevention. Mol Nutr Food Res 51:738–745. https://doi.org/10.1002/mnfr.200600275
Jepson RG, Williams G, Craig JC (2012) Cranberries for preventing urinary tract infections. Cochrane Database Syst Rev 10:CD001321. https://doi.org/10.1002/14651858.CD001321.pub5
Kranjcec B, Papes D, Altarac S (2014) d-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial. World J Urol 32:79–84. https://doi.org/10.1007/s00345-013-1091-6
Ferry SA, Holm SE, Stenlund H et al (2004) The natural course of uncomplicated lower urinary tract infection in women illustrated by a randomized placebo controlled study. Scand J Infect Dis 36:296–301
Acknowledgements
The results presented in this study have not been published elsewhere in whole or part. All authors approved the final version of the submitted manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared no competing interests.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fiorentino, M., Pesce, F., Schena, A. et al. Updates on urinary tract infections in kidney transplantation. J Nephrol 32, 751–761 (2019). https://doi.org/10.1007/s40620-019-00585-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-019-00585-3