Abstract
Subclinical rejection (SCR) has been variably associated with reduced graft survival, development and progression of interstitial fibrosis/tubular atrophy and chronic allograft nephropathy, but data are controversial concerning SCR treatment in terms of graft survival improvement. In this single-center retrospective study, we enrolled 174 adult kidney transplant recipients with a protocol biopsy performed at 30 days after transplantation to evaluate the incidence rate and risk factors for early SCR and its impact on 10-year graft survival. Five patients showed primary non function and were excluded. Among 159/169 (94.08 %) patients with stable graft function who underwent protocol biopsy, 17 (10.7 %) showed signs of SCR and were treated with low-dose intravenous (i.v.) steroids. Ten patients showed functional impairment, 8 (4.73 %) resulting as acute rejection. At multivariate analysis, donor age [odds ratio (OR) 1.04, 95 % confidence interval (CI) 1.01–1.09], and delayed graft function (DGF) (OR 1.08, 95 % CI 1.03–1.12) were significantly associated with SCR. The 10-year graft survival rate in the SCR group was similar to that in the normal-findings group (76.5 vs. 74.9 % respectively; p = 0.61). At multivariate Cox regression, acute [hazard ratio (HR) 5.22, 95 % CI 1.70–16.01], but not sub-clinical, rejection was independently associated with long-term graft failure. In conclusion, early protocol biopsy is a useful and safe tool to detect early SCR which seems not to affect the long-term survival. We suggest that this could be, probably, linked to early SCR treatment with low dose i.v. steroids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subclinical rejection (SCR) is histologically defined as an acute rejection [1] characterized by tubulointerstitial mononuclear infiltration identified from a biopsy specimen without the presence of a functional deterioration [2, 3]. SCR is therefore, by definition, diagnosed only on biopsies taken as per protocol at a fixed time after transplantation, rather than driven by clinical indication.
SCR peaks during the two initial months of post-transplantation and declines thereafter [4]. The averaged prevalence of SCR in the first year post renal transplantation depends on protocol biopsy strategy variation between nephrology units [4], ranging from 29 % at 1 month to 17 % at 1 year [2, 5].
The long-term impact of SCR on renal graft function remains poorly understood, notwithstanding it was previously suggested as having a significant impact on allograft outcome [6–9]. Indeed, SCR has been variably associated with impaired renal function at 6 and 12 months after transplantation [8, 10], reduced graft survival [8, 9, 11–13], development and progression of interstitial fibrosis and tubular atrophy (IF/TA) [14], and chronic allograft nephropathy (CAN) [2, 8–10, 15], which is the most common cause of late renal allograft failure. Nevertheless, biopsies with SCR as early as 2 weeks can distinguish survival differences when followed to 10 years [11]. Therefore, early detection and treatment of SCR should reduce the incidence of CAN and increase graft survival, but controversial data exist about SCR treatment efficacy [16, 17] even if the kidney disease/improving global outcomes (KDIGO) guidelines recommend, with a low grade of evidence, to treat subclinical and borderline acute rejection [18].
The aims of our study were, first, to evaluate the incidence of early SCR revealed by protocol biopsy at 1 month post kidney transplantation and the factors potentially involved in this manifestation; and, secondly, to evaluate the association between SCR precociously treated with low-dose intravenous (i.v.) steroids and long-term graft survival.
Materials and methods
This was a single-center retrospective study performed at our Renal Transplant Unit at Annunziata Hospital in Cosenza, Italy. Between July 2000 and December 2013, 174 adult patients received a primary kidney transplant from deceased donors. A protocol biopsy was performed on patients with stable graft function at day 30 after transplantation. Stable graft function in the recipients was defined as an increase between 0 and 15 % in serum creatinine in the 5 days before protocol biopsy. Core renal biopsies were taken using an 18-gauge biopsy gun using ultrasound localization. Primary non function was diagnosed in 5 patients, who were excluded from the analysis. Of the 169 remaining, 159 patients underwent protocol biopsy while 10 patients presented, within the first month post transplantation, a clinically suspected acute rejection episode that was confirmed by a percutaneous graft biopsy in 8 patients, while the other two showed acute cyclosporine toxicity.
Renal biopsy slides were scored by two independent figures (a pathologist and a nephrologist) according to the Banff 97 working classification [1]. To minimize inter-observer variability, every 10th biopsy was scored by both doctors and the findings discussed. All biopsy specimens included five or more glomeruli. Presence of SCR was based on the absence of functional deterioration and histologic findings indicative of rejection on the basis of the tubulitis (‘t’) and mononuclear cell infiltration (‘i’) scores. All findings of ‘t’ score ≥1 and ‘i’ score >0 in the absence of functional deterioration were classified as SCR.
Patients with SCR were treated with i.v. steroid pulse therapy (methylprednisolone (Solu-Medrol, Pharmacia, The Netherlands) 250 mg/day for three consecutive days. An acute rejection episode was treated with methylprednisolone 500 mg/d for three consecutive days or anti-thymocyte globulin as clinically and histologically indicated.
All participants received induction treatment based on basiliximab, steroids, mycophenolate mofetil (MMF) followed by maintenance with calcineurin inhibitors (after day 2 post transplantation), steroids and MMF. Tacrolimus was used in 113 patients and cyclosporine (CsA) in 61. We used the dose of tacrolimus achieving 12-h trough levels of 10 (5–15) ng/ml [18, 19]. Standard-dose CsA may be defined as the dose achieving C0 of 200 (150–300) ng/ml or C2 1400–1800 ng/ml early and 800–1200 ng/ml later after transplantation [20, 21]. The initial dose of MMF was 1.5 g/day, and the dose was modified to minimize adverse effects such as diarrhea or leukopenia.
Delayed graft function (DGF) was defined as necessity for dialysis in the first week after surgery. Cytomegalovirus (CMV) infection was defined as detection of viremia >650 copies/ml of whole blood. All transplant patients were treated according to a preemptive strategy, consisting of the initiation of antiviral treatment upon detection of a viral load (CMV-DNAemia) above 5,000 copies/ml. Anti-CMV preemptive treatment included i.v. administration of ganciclovir (5 mg/kg daily) adjusted for renal function. Antiviral therapy was considered successful when two sequential negative CMV-DNAemia tests were obtained.
Our 174 patients were divided into normal, SCR and acute rejection groups according to the Banff classification. The clinical characteristics observed among three groups were compared with respect to the age and sex of recipients and donors, the duration of dialysis before transplantation, the total number of human leukocyte antigen (HLA) mismatches, types of immunosuppressant used, presence of DGF, incidence of CMV infection and the cold ischemia time. Clinical outcomes of each group were compared with respect to graft survival (10 years). Graft survival was calculated using the Kaplan–Meier method and compared for statistical significance using the log-rank method. Cox proportional hazards regression models were used to evaluate factors associated with graft survival. Chi-Square, Student’s t tests or logistic regression were used for other comparisons. A p value <0.05 was assumed statistically significant.
The design of the study was approved by the local ethical committee. All patients enrolled provided written informed consent, and the study was conducted in conformity with the declaration of Helsinki and guidelines of the local ethical committee.
Results
The main demographic and baseline characteristics at 30 days post transplantation (time point for protocol biopsy) of all 174 participants are shown in Table 1. Five patients showed primary non function due to venous thrombosis in three cases, arterial thrombosis in one case and in one patient both vessels were thrombosed. DGF was diagnosed in 69 (39.7 %) cases. The majority of transplant recipients (127, 74.1 %) exhibited three or four mismatches at the time of transplantation.
Among the 159 out of 169 patients (94.08 %) who showed stable graft function, protocol biopsy revealed normal findings in 142 patients (89.30 %), while 17 patients (10.7 %) showed SCR. Among those with functional alterations, 8 patients (4.73 %) showed acute rejection according to the Banff classification while 2 patients presented acute cyclosporine toxicity and were added to the normal findings group. The comparison of the selective mean Banff scores according to the status of the graft (normal, SCR or acute rejection) is shown in Table 2. The Banff component scores were significantly higher in the groups with SCR and acute rejection than in the normal findings group, without a significant difference between the subclinical and acute rejection groups. Nevertheless, there was no correlation between elementary lesions and renal function at day 30. Incidence of SCR, as well as of acute rejection, did not differ significantly between tacrolimus and cyclosporine treated patients. In terms of complications after the biopsy procedure, we registered only three cases of peri-renal hematoma and one fistula.
A comparison between the clinical characteristics of normal and SCR patients is shown in Table 3. There were no differences between the recipients in terms of age or sex. Serum creatinine levels at the time of graft biopsy did not differ between groups. The duration of dialysis before transplantation, cold ischemia time, number of mismatches, type of calcineurin inhibitors, CMV infection and date of transplantation did not affect the histological findings. However, patients with subclinical rejection showed more DGF events and higher donor age than the normal findings group (p < 0.05).
Table 4 shows the results of the multivariate analysis of factors associated with subclinical rejection. Factors significantly associated with SCR were donor age with an odds ratio (OR) of 1.04 [95 % confidence interval (CI) 1.01–1.09], and DGF with an OR of 1.08 (95 % CI 1.03–1.12).
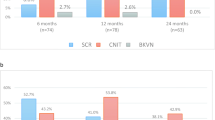
The 10-year graft survival rate in the subclinical rejection group was similar to that of the normal findings group (68.8 vs. 74.9 % respectively; p = 0.27), while the acute rejection group had a significantly lower 10-year graft survival (31.1 %, p < 0.001) (Fig. 1). At multivariate Cox regression, donor age [hazard ratio (HR) 1.03, 95 % CI 1.01–1.05], DGF (1.57, 1.04–2.22) and acute (5.22, 1.70–16.01), but not sub-clinical, rejection were independently associated with 10-year graft failure (Table 5).
We observed 13 (7.5 %) cases of patient death due to cardiovascular accident (61.5 %), neoplasia (23.1 %) and infection (15.4 %).
Discussion
Our study suggests that early protocol biopsy is a useful and safe tool to detect early SCR which seems not to affect the long-term survival, in contrast to acute rejection. Indeed, we did not find any survival difference at 10 years between the steroid-treated SCR group and the normal findings group while the acute rejection group had a significantly lower 10-year graft survival and acute rejection was independently associated with graft survival. We speculate, based on the current literature, that this could be probably linked to our strategy of early SCR treatment with low-dose pulse i.v. methylprednisolone therapy.
Evidence linking SCR with reduced graft survival in children and adults is supported by findings from long-term studies [8, 9, 11–13]. Choi et al. showed a marked 10-year graft survival difference between patients with untreated SCR (obtained from biopsy performed at day 14 after transplantation) and patients with normal histological findings. They clearly demonstrated that the incidence of acute rejection increased and graft survival rate decreased in patients showing untreated subclinical rejection [11]. Thierry et al. reported a similar difference in terms of estimated glomerular filtration rate (eGFR) at 30 months post transplantation [22]. Only a few studies have focused on SCR treatment in terms of graft survival improvement, and in the published literature, to our knowledge, there are few randomized controlled trials (RCTs), reporting conflicting data. In one of these, Rush and colleagues randomized 72 patients to protocol biopsies at 1, 2, 3, 6 and 12 months (biopsy group) or to 6- and 12-month biopsies only (control group), and followed them for a minimum of 2 years. They concluded that the detection and treatment of subclinical acute rejection resulted in better graft function [16]. Conversely, in a multicenter RCT of 218 patients, protocol biopsies and treatment of subclinical acute rejection were not beneficial [23]. In our retrospective cohort, independently of histological score and immunosuppressive strategy, the choice to treat SCR with i.v. pulse steroid could have led to a graft survival improvement in SCR groups, possibly explaining the absence of any significant difference in SCR group graft survival with respect to the normal findings group.
Early SCR treatment could prevent the acute rejection onset and so ameliorate the graft survival. Indeed, Roberts et al. [24] reported that most patients whose day 7 biopsy specimens showed SCR go on to develop clinical rejection if left untreated, and this was confirmed by Park et al. who reported that 20 % of recipients with borderline changes experienced acute rejection within 6 months [25]. Schweitzer et al. [26] reported that borderline changes frequently represent acute rejection, and that anti-rejection treatment is therefore appropriate in most cases. Our results also are in line with previous data reporting that recipients with SCR who were treated with anti-rejection therapy showed significant improvements in graft function compared to patients without anti-rejection treatment [27]. Moreover, in our renal transplantation unit we chose, as therapeutic protocol of SCR, i.v. pulse 250 mg of methylprednisolone which represents a relatively low dose of steroids. This strategy appeared useful to ameliorate long-term graft survival in the SCR group, probably preventing acute rejection onset, without exposing patients to the side effects of a high dose of steroids.
Our findings underlie the usefulness of establishing an early time-point for graft biopsy as part of the protocol biopsy strategy to ameliorate late graft survival. One of the concerns of protocol biopsies is that they may lead to a significant risk of graft failure and that this risk is greater than the potential benefit for the patients. However, several studies [28, 29] have shown that the benefits of protocol biopsy could exceed the risks, and that biopsy is the most accurate tool for detecting subclinical rejection. According to previous reports, in our study we found no major problems caused by biopsy-related complications [11]. With regard to biopsy timing, we chose 1 month after transplantation because graft function is generally normalized within this time-frame and usually at day 30 patients begin the in-hospital follow-up after discharge.
We observed an incidence for SCR of 10.7, and 4.73 % for acute rejection after 1 month post transplantation, data similar to those reported in the literature even if there are few epidemiological reports on the incidence of early acute rejection.
SCR can be sub-classified into ‘acute’ SCR (Banff i2 and t2 or worse) or milder ‘borderline’ SCR (e.g. i1 and t1), synonymously designated as ‘suspicious for acute rejection’ [1]. We chose not to sub-classify SCR because we think that this histological difference should not influence the therapeutic approach. Indeed, also borderline changes should not be regarded as harmless, since previous studies have shown that their presence is associated with an incidence of clinical acute rejection double that of patients without these changes [11] and a worse renal function 5 years after transplantation [6]. In addition, the presence of SCR in protocol biopsies has been consistently associated with the progression of IF/TA, supporting the notion that persistent interstitial inflammation is harmful for the allograft [14]. Even very low-grade inflammation has been associated with progression of chronic tubulointerstitial damage. Thus, it has been proposed that IF/TA will progress in parallel to the intensity and duration of SCR and, consequently, a chronological sequence of events initiated by subclinical inflammation may lead to graft failure.
At multivariate regression analysis, we found donor age and DGF to be predictors of early SCR development. Previous studies also associate HLA mismatches (in particular HLA DR mismatch) with cold ischemia time to SCR development [11, 30]. Rush et al. [30] performed protocol biopsies at 1, 2, and 3 months after renal transplantation, and found that the incidence of subclinical rejection in the first protocol biopsy was 20, 30 and 63 % in patients with zero, one and two HLA-DR mismatches, respectively. Choi et al. reported that, in living donor transplantation, the incidence of subclinical rejection increased with the increase in the number of HLA-DR mismatches (2.7, 15.4 and 20.8 % in patients with zero, one and two HLA-DR mismatches, respectively) [11]. Probably this association is lacking in our cohort because the majority of our patients presented 3–4 mismatches and a short average cold ischemia time.
Our study has several limitations, the chief one being the lack of an SRC group without steroid treatment as control. To overcome this, we used previous study reports even if it is difficult to compare studies of protocol biopsy findings due to the wide variations in patient demographics, utilization of induction therapy, timing of the biopsy and selection of calcineurin inhibitor.
In conclusion, an early protocol biopsy performed 1 month after renal transplantation is a useful tool to detect subclinical rejection and we suggest that anti-rejection treatment for SCR, with low-dose i.v. pulse steroids, could be an appropriate strategy to improve kidney transplant graft survival in the long term even if this therapeutic approach needs to be confirmed through a clinical trial.
References
Racusen LC, Solez K, Colvin RB, Bonsib SM, Castro MC, Cavallo T, Croker BP, Demetris AJ, Drachenberg CB, Fogo AB, Furness P, Gaber LW, Gibson IW, Glotz D, Goldberg JC, Grande J, Halloran PF, Hansen HE, Hartley B, Hayry PJ, Hill CM, Hoffman EO, Hunsicker LG, Lindblad AS, Yamaguchi Y et al (1999) The Banff 97 working classification of renal allograft pathology. Kidney Int 55(2):713–723
Nankivell BJ, Borrows RJ, Fung CL, O’Connell PJ, Allen RD, Chapman JR (2004) Natural history, risk factors, and impact of subclinical rejection in kidney transplantation. Transplantation 78(2):242–249
Rush D, Nickerson P, Gough J, McKenna R, Grimm P, Cheang M, Trpkov K, Solez K, Jeffery J (1998) Beneficial effects of treatment of early subclinical rejection: a randomized study. J Am Soc Nephrol 9(11):2129–2134
Nankivell BJ, Chapman JR (2006) The significance of subclinical rejection and the value of protocol biopsies. Am J Transplant 6(9):2006–2012
Shapiro R, Randhawa P, Jordan ML, Scantlebury VP, Vivas C, Jain A, Corry RJ, McCauley J, Johnston J, Donaldson J, Gray EA, Dvorchik I, Hakala TR, Fung JJ, Starzl TE (2001) An analysis of early renal transplant protocol biopsies–the high incidence of subclinical tubulitis. Am J Transplant 1(1):47–50
Miyagi M, Ishikawa Y, Mizuiri S, Aikawa A, Ohara T, Hasegawa A (2005) Significance of subclinical rejection in early renal allograft biopsies for chronic allograft dysfunction. Clin Transplant 19(4):456–465
Nankivell BJ, Borrows RJ, Fung CL, O’Connell PJ, Allen RD, Chapman JR (2003) The natural history of chronic allograft nephropathy. N Engl J Med 349(24):2326–2333
Rush DN, Jeffery JR, Gough J (1995) Sequential protocol biopsies in renal transplant patients. Clinico-pathological correlations using the Banff schema. Transplantation 59(4):511–514
Shishido S, Asanuma H, Nakai H, Mori Y, Satoh H, Kamimaki I, Hataya H, Ikeda M, Honda M, Hasegawa A (2003) The impact of repeated subclinical acute rejection on the progression of chronic allograft nephropathy. J Am Soc Nephrol 14(4):1046–1052
Seron D, Diaz-Gallo C, Grino JM, Castelao AM, Carrera M, Bover J, Alsina J (1991) Characterization of interstitial infiltrate in early renal allograft biopsies in patients with stable renal function. Transplant Proc 23(1 Pt 2):1267–1269
Choi BS, Shin MJ, Shin SJ, Kim YS, Choi YJ, Kim YS, Moon IS, Kim SY, Koh YB, Bang BK, Yang CW (2005) Clinical significance of an early protocol biopsy in living-donor renal transplantation: ten-year experience at a single center. Am J Transplant 5(6):1354–1360
Kanetsuna Y, Yamaguchi Y, Toma H, Tanabe K (2003) Histological evaluation of renal allograft protocol biopsies in the early period and 1 year after transplantation. Clin Transplant 17(Suppl 10):25–29
Rush D, Jeffery J, Trpkov K, Solez K, Gough J (1996) Effect of subclinical rejection on renal allograft histology and function at 6 months. Transplant Proc 28(1):494–495
Heilman RL, Devarapalli Y, Chakkera HA, Mekeel KL, Moss AA, Mulligan DC, Mazur MJ, Hamawi K, Williams JW, Reddy KS (2010) Impact of subclinical inflammation on the development of interstitial fibrosis and tubular atrophy in kidney transplant recipients. Am J Transplant 10(3):563–570
Nankivell BJ, Fenton-Lee CA, Kuypers DR, Cheung E, Allen RD, O’Connell PJ, Chapman JR (2001) Effect of histological damage on long-term kidney transplant outcome. Transplantation 71(4):515–523
Rush DN, Karpinski ME, Nickerson P, Dancea S, Birk P, Jeffery JR (1999) Does subclinical rejection contribute to chronic rejection in renal transplant patients? Clin Transplant 13(6):441–446
Scholten EM, Rowshani AT, Cremers S, Bemelman FJ, Eikmans M, van Kan E, Mallat MJ, Florquin S, Surachno J, ten Berge IJ, Bajema IM, de Fijter JW (2006) Untreated rejection in 6-month protocol biopsies is not associated with fibrosis in serial biopsies or with loss of graft function. J Am Soc Nephrol 17(9):2622–2632
Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group (2009) KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant 9(Suppl 3):S1–S155
Vincenti F, Friman S, Scheuermann E, Rostaing L, Jenssen T, Campistol JM, Uchida K, Pescovitz MD, Marchetti P, Tuncer M, Citterio F, Wiecek A, Chadban S, El-Shahawy M, Budde K, Goto N (2007) Results of an international, randomized trial comparing glucose metabolism disorders and outcome with cyclosporine versus tacrolimus. Am J Transplant 7(6):1506–1514
Ekberg H, Tedesco-Silva H, Demirbas A, Vitko S, Nashan B, Gurkan A, Margreiter R, Hugo C, Grinyo JM, Frei U, Vanrenterghem Y, Daloze P, Halloran PF (2007) Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med 357(25):2562–2575
Ekberg H, Grinyo J, Nashan B, Vanrenterghem Y, Vincenti F, Voulgari A, Truman M, Nasmyth-Miller C, Rashford M (2007) Cyclosporine sparing with mycophenolate mofetil, daclizumab and corticosteroids in renal allograft recipients: the CAESAR Study. Am J Transplant 7(3):560–570
Thierry A, Thervet E, Vuiblet V, Goujon JM, Machet MC, Noel LH, Rioux-Leclercq N, Comoz F, Cordonnier C, Francois A, Marcellin L, Girardot-Seguin S, Touchard G (2011) Long-term impact of subclinical inflammation diagnosed by protocol biopsy one year after renal transplantation. Am J Transplant 11(10):2153–2161
Rush D, Arlen D, Boucher A, Busque S, Cockfield SM, Girardin C, Knoll G, Lachance JG, Landsberg D, Shapiro J, Shoker A, Yilmaz S (2007) Lack of benefit of early protocol biopsies in renal transplant patients receiving TAC and MMF: a randomized study. Am J Transplant 7(11):2538–2545
Roberts IS, Reddy S, Russell C, Davies DR, Friend PJ, Handa AI, Morris PJ (2004) Subclinical rejection and borderline changes in early protocol biopsy specimens after renal transplantation. Transplantation 77(8):1194–1198
Park JH, Yang CW, Kim YS, Lee SH, Choi YJ, Kim YS, Moon IS, Koh YB, Bang BK (2002) Comparisons of clinicopathological correlations between immediate and slow graft function in renal transplant recipients. Clin Transplant 16(Suppl 8):18–23
Schweitzer EJ, Drachenberg CB, Anderson L, Papadimetriou JC, Kuo PC, Johnson LB, Klassen DK, Hoehn-Saric E, Weir MR, Bartlett ST (1996) Significance of the Banff borderline biopsy. Am J Kidney Dis 28(4):585–588
Park JH, Yang CW, Kim YS, Moon IS, Chang YS, Koh YB, Bang BK (1999) Clinical impact of slow recovery of renal function in renal transplantation. Transplant Proc 31(7):2841–2842
Furness PN, Philpott CM, Chorbadjian MT, Nicholson ML, Bosmans JL, Corthouts BL, Bogers JJ, Schwarz A, Gwinner W, Haller H, Mengel M, Seron D, Moreso F, Canas C (2003) Protocol biopsy of the stable renal transplant: a multicenter study of methods and complication rates. Transplantation 76(6):969–973
Wilczek HE (1990) Percutaneous needle biopsy of the renal allograft. A clinical safety evaluation of 1129 biopsies. Transplantation 50(5):790–797
Rush DN, Grimm P, Gough J, Lipman M, Birk P, McKenna R, Nickerson P (1999) Prediction rejection: is early diagnosis achievable and important? Graft 2(Suppl. 2):s31–s35
Acknowledgements
The authors gratefully acknowledge Armentano Filomena and Greco Angela for their nursing assistance in this study and all our Nephrology staff for their clinical assistance in this study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gigliotti, P., Lofaro, D., Leone, F. et al. Early subclinical rejection treated with low dose i.v. steroids is not associated to graft survival impairment: 13-years’ experience at a single center. J Nephrol 29, 443–449 (2016). https://doi.org/10.1007/s40620-015-0206-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-015-0206-0