Abstract
Background
Monocarboxylate transporter 8 (MCT8) is the first thyroid hormone transporter that has been linked to a human disease. Besides genetic alterations other factors might impair MCT8 activity.
Aim
This study aimed at investigating whether some common drugs having a structural similarity with TH and/or whose treatment is associated with thyroid function test abnormalities, or which behave as antagonists of TH action can inhibit MCT8-mediated T3 transport.
Methods
[125I]T3 uptake and efflux were measured in COS-7 cells transiently transfected with hMCT8 before and after exposure to increasing concentrations of hydrocortisone, dexamethasone, prednisone, prednisolone, amiodarone, desethylamiodarone, dronedarone, buspirone, carbamazepine, valproic acid, and l-carnitine. The mode of inhibition was also determined.
Results
Dexamethasone significantly inhibited T3 uptake at 10 μM; hydrocortisone reduced T3 uptake only at high concentrations, i.e. at 500 and 1000 μM; prednisone and prednisolone were devoid of inhibitory potential. Amiodarone caused a reduction of T3 uptake by MCT8 only at the highest concentrations used (44% at 50 μM and 68% at 100 μM), and this effect was weaker than that produced by desethylamiodarone and dronedarone; buspirone resulted a potent inhibitor, reducing T3 uptake at 0.1–10 μM. l-Carnitine inhibited T3 uptake only at 500 mM and 1 M. Kinetic experiments revealed a noncompetitive mode of inhibition for all compounds. All drugs inhibiting T3 uptake did not affect T3 release.
Conclusion
This study shows a novel effect of some common drugs, which is inhibition of T3 transport mediated by MCT8. Specifically, dexamethasone, buspirone, desethylamiodarone, and dronedarone behave as potent inhibitors of MCT8.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monocarboxylate transporter 8 (MCT8) is the first thyroid hormone (TH) transporter that has been linked to a human disease [1, 2].
Loss-of-function mutations in the MCT8 gene (SLC16A2) are the molecular cause of the Allan–Herndon–Dudley syndrome, a form of X-linked mental retardation and severe neurological impairment, associated with TH abnormalities, consisting of high 3,5,3,-triiodothyronine (T3), low thyroxine (T4) and 3,3,5,-triiodothyronine (rT3) levels, and normal or slightly elevated concentration of the thyroid-stimulating hormone (TSH) [3]. In man MCT8 is expressed at different levels in many tissues including liver, adrenal gland, brain, kidney, placenta, and thyroid [4,5,6].
MCT8 functions as a specific TH transmembrane transporter [7, 8], mediating the uptake as well as the efflux [9]. The precise mechanisms by which MCT8 facilitates TH transport are still unknown, although recently a model has been proposed [10]. It has been demonstrated that this process is Na+ independent, not sensitive to pH and is a facilitated transport [11].
So far, only few drugs (i.e. desipramine and tyrosine kinase inhibitors) and natural compounds (silychristin and some natural kinase inhibitors) have been shown to interfere with MCT8 function through non-competitive and competitive inhibition, respectively [12,13,14,15,16].
Aiming at increasing the knowledge about inhibitors of MCT8 function, in the present work we examined whether some commonly used drugs are able to inhibit MCT8-mediated T3 transport, and potentially interfere with TH action in target tissues. We selected drugs having a somewhat structural similarity with TH and/or whose treatment is associated with thyroid function tests (TFTs) abnormalities, or which behave as antagonists of TH action. Figure 1 shows the chemical formulas of T3 and selected drugs.
Overall, glucocorticoids, as other steroid hormones resemble TH in size, hydrophobic properties, and mechanism of action through binding to members of the nuclear receptor superfamily, and some recent evidence suggests that also for steroids the cell-membrane passage might be carrier-mediated [17]. Moreover, the use of dexamethasone and other synthetic glucocorticoids in prenatal life and in childhood has been associated with adverse effects on the developing brain similar to those induced by hypothyroidism [18,19,20].
Amiodarone is a benzofuran frequently prescribed for the treatment of refractory cardiac arrhythmias, having a structural resemblance to TH. Besides hyper- and hypothyroidism, administration of amiodarone has been also associated with a low T3 syndrome, which has been attributed to the inhibitory effect of amiodarone on type I and II 5′-deiodinase [21, 22]. Furthermore, since a hypothyroidism-like condition of some tissues has been observed during treatment with amiodarone [23], it was demonstrated that this drug and its active metabolite, desethylamiodarone (DEA), block T3 binding to nuclear receptors [24] and decrease expression of some TH-related genes such as alpha-myosin heavy chain and low-density lipoprotein receptor [25, 26]. DEA has been shown to competitively inhibit TRα1 and to noncompetitively TRβ1 [27]. However, it is conceivable that the induction of the local hypothyroid state may be also due to the impaired TH uptake in tissues. Dronedarone is structurally related to amiodarone but lacks iodine moiety. As for amiodarone and DEA, dronedarone was shown to reduce in vitro binding of T3 to TRα1 without affecting TRβ1 receptors, while its metabolite, debutyldronedarone, inhibited T3 binding to both receptors [28].
Thyroid hormones influence mood [29] and there is evidence that some psychotropic medications can reduce TH uptake in brain [12]. Among these agents, we selected buspirone, a drug that, when used in major depression in augmentation with SSRIs or tricyclic antidepressants, shows to be less effective than T3 in improving the response of clinical non responders [30, 31].
The use of carbamazepine and valproic acid is associated with TFTs abnormalities, the underlying mechanisms of which are not yet fully understood [32].
Lastly, basic and clinical studies performed in the late 1950s and mid-1960s suggested that l-carnitine could contrast the effect of TH in both animals and humans [33, 34]. A more recent study on cultures of fibroblasts, hepatic, and neuronal cells showed that l-carnitine dose-dependently inhibits the entry into the cell nuclei of T4 and T3 but not their binding to the cognate nuclear receptors and caused a minimal additional decrease in whole-cell uptake of both hormones [35], suggesting that l-carnitine could be a naturally occurring inhibitor of TH action.
Herein, we show a significant inhibition of MCT8 by dexamethasone, buspirone, desethylamiodarone, and dronedarone. Our findings can help to explain the side effects related to the use of these drugs.
Materials and methods
Plasmid
Human MCT8 gene cloned in pcDNA3 expression vector used for transient transfection of COS-7 was kindly provided by Dr. Dumitrescu, University of Chicago, Chicago, Illinois (USA).
Drugs and concentrations
3,5,3′-Triiodo-l-thyronine, hydrocortisone, BSP, buspirone, dronedarone, amiodarone, desethylamiodarone, carbamazepine, and valproic acid were obtained from Sigma-Aldrich; prednisone, prednisolone, dexamethasone acetate, l-carnitine were obtained from Caelo Caesar & Loretz. As solvents to prepare the stock solutions were used: dimethylsulphoxide (DMSO) for hydrocortisone, amiodarone, desethylamiodarone, prednisone and prednisolone, whereas water for bromsulphthalein (BSP), valproic acid, buspirone and l-carnitine, and ethanol for carbamazepine and dexamethasone; 0.1 M natrium hydroxide was used as solvent of T3.
The non-bile acid organic anion BSP, a potent inhibitor of thyroid hormone transport on the basis of structural similarity [36], was used as positive control at 50 μM concentration.
All the drugs and the concentrations used for the study are shown in Table 1.
Cell culture and transient transfection
COS-7 cells were cultured in 24-well dishes with Dulbecco’s modifed Eagle’s medium supplemented with 10% FBS, 100 IU/mL penicillin, 100 mg/mL streptomycin, 2.5 mg/mL fungizone, and 1 mmol/L sodium pyruvate. For transient expression of hMCT8 gene, COS-7 cells were seeded at the concentration of 100,000 cells/well and subsequently transfected in duplicate with 1 mg empty vector or pcDNA3-hMCT8 using Attractene Reagent (Qiagen).
Tripan blue dye exclusion
48 h after transfection, cells were incubated for 1 h or O/N at 37 °C with different concentrations of the drugs to be tested (Table1). Tripan blue dye exclusion test was used to determine the number of viable cells present in cell suspension as described previously [37].
T3 uptake assay
In order to determine the kinetic characteristics of T3 uptake in COS-7 cells, a time course experiment was performed. Forty-eight hours after transfection, cells were washed with Dulbecco’s Phosphate Buffered Saline (D-PBS) medium and incubated for 5–60 min at 37 °C with 150,000 cpm T3 labelled with 125 I ([125I]-T3 PerkinElmer) in D-PBS medium plus 0.1% BSA (assay buffer). After incubation cells were quickly washed twice with ice-cold assay buffer and lysed with 0.1 M NaOH. Cell-associated radioactivity was determined by counting the cell lysates in γ-counter and data were given in counts per minute (cpm). All subsequent uptake experiments were performed after 15-min incubation with radiolabelled T3.
Effect of drugs on T3 uptake
To study the effect of the selected drugs on MCT8-mediated T3 uptake, transfected cells were incubated at 37 °C for 15’ with 150,000 cpm [125I] T3 in the absence (basal value of uptake) or in the presence of different concentrations of each drug as indicated in Table 1. After incubation, cells were washed, lysed, and the accumulated radioactivity was counted as described above. Results were expressed as percent T3 uptake with respect to value obtained in basal condition. Net uptake levels corrected for background observed in cells transfected with empty vector were used.
In order to obtain the IC50 values for each substance significantly diminishing [125I]T3 uptake, data were fitted by nonlinear regression using the GraphPad version 6.0.
Determination of the mode of inhibition
Transfected cells were incubated for 3 min with [125I]T3 different concentrations in the absence or presence of the IC50 of the different substances to test [13]. After two washes with D-PBS cells were lysed in 0.1 M NaOH, and cell-associated radioactivity was measured with a γ-counter.
To describe the T3 transport across the cell membrane a Michaelis–Menten mechanism was assumed and kinetics data were plotted according to Eadie–Hofstee diagram. In this linearization of the Michaelis–Menten equation, the intersection with the ordinate axis represents the maximum velocity value (Vmax), while the slope of the curve is the negative value of the Michaelis–Menten constant (− Km). Parallel lines in the presence of the inhibitor imply that Km is constant and there is no competition with substrate, while the decrease of Vmax implies a reduction in active molecule concentration and a noncompetitive mode of inhibition.
Efflux of radiolabeled T3
To determine the kinetics of T3 efflux, COS-7 cells transiently transfected as above were preincubated for 30 min at 37 °C with 150,000 cpm [125I] T3 diluted in assay buffer, washed with D-PBS medium plus 0.1% BSA, and incubated for 1–30 min with fresh assay medium with or without 10 μM unlabeled T3. After incubation, both medium and cells were collected and [125I]T3 associated radioactivity was quantified.
Effect of drugs on T3 efflux
To evaluate the ability of the drugs having an effect on T3 uptake to inhibit T3 efflux, after 30 min preincubation with labelled T3, hydrocortisone, amiodarone, dronedarone, desethylamiodarone, dexamethasone, buspirone, l-carnitine, T3, and BSP were added at their respective maximum inhibition concentration for additional 15 min. Hereinafter the radioactive buffer was replaced with fresh assay buffer for 0–2-4–10-15 min; all supernatants were collected, cells were lysed after the last supernatant removal and medium and cell-associated radioactivity was determined. Total radioactivity at the beginning of efflux (100%) was calculated by adding the radioactivity found in each supernatant to that of finally lysed cells. Data of T3 efflux were expressed as percent of cell retained T3 with respect to time.
Statistics
Variables were preliminarily tested for normal distribution and expressed as mean ± SE. To evaluate the difference in T3 uptake in the presence of the different drugs tested compared to the basal uptake values, a one-way ANOVA with Dunnett’s T3 post-hoc test for multiple comparisons was used. A linear-mixed analysis for repeated measures was performed to evaluate the effect of different drugs tested on T3 efflux across all time points. T3 efflux values were log-transformed to correct for heterogeneity of variance and to produce approximately normally distributed data. Means were compared using Fisher’s least square difference post-hoc test. The two-tailed level of statistical significance was set at P less than 0.05. All statistical analyses were performed by using SPSS (IBM SPSS Statistics, version 25).
Results
Tripan blue dye exclusion
The selected drugs were tested at all concentrations showed in Table1 and, also after an O/N incubation of transfected COS-7 cells with the substances, no cytotoxic effect was detected with a cell viability greater than 95% (Supplemental Table 1). Therefore, all the concentrations were used in the following experiments.
Time course of T3 accumulation in COS-7 cells
hMCT8 transfected COS-7 cells showed nearly 2.5-fold higher [125I]T3 uptake compared to cells transfected with empty vector.
In the former, [125I]T3 uptake increased linearly between 0 and 5 min. After 15-min incubation the plateau of the uptake was not yet achieved, and the curve continued to grow even if not linearly as in the first 5 min (Fig. 2). Inhibition studies were then performed at 15 min after coapplying to [125I]T3 increasing concentrations of each drug.
Time course of [125I]T3 accumulation in COS-7 cells transfected with the empty vector (pcDNA3), i.e. with the expression vector not containing human MCT8 gene, and with expression vector containing MCT8 coding sequence (hMCT8). Data are expressed as mean ± SE. All experiments were performed in triplicate
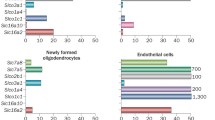
Effect of drugs on MCT8-mediated [125I]T3 uptake
Glucocorticoids
Exposure to each glucocorticoid gave different results. Hydrocortisone dose-dependently inhibited T3 uptake. Low doses of hydrocortisone did not inhibit T3 uptake. A non-significant inhibition with 100 μM (− 21%; P = 0.979) and a significant inhibition at 500 and 1000 μM (− 74% and -77%, respectively) (Fig. 3a) were observed. Dexamethasone had a more pronounced effect on MCT8 transport. In particular, a non-significant inhibition of T3 uptake was obtained at 0.1 and 1 μM (− 21 and − 29%, respectively), while 10 and 100 μM significantly reduced T3 uptake (− 54 and − 65%, respectively; all P < 0.001) (Fig. 3a). Conversely, prednisone and prednisolone did not show inhibitory potential in the statistical modeling used in this study (Fig. 3a).
Effects of the selected drugs on MCT8 mediated [125I]T3 uptake. a Glucocorticoids, b antiarrhythmic drugs, c anxiolytic drug, d anticonvulsant agents, e l-carnitine. Results are the means ± SE of three independent experiments and are expressed as percent [125I]T3 uptake with respect to values obtained without inhibitor (basal condition, set to 100%). Bromsulphthalein (BSP) at 50 μM concentration was used as positive control. [125I]T3 uptake of cells transfected with empty vector (i.e. the expression vector not containing human MCT8 gene) was considered as background and subtracted. *P < 0.05; **P < 0.001 ***P < 0.0001
Antiarrhythmic drugs
Among the antiarrhythmic agents tested, amiodarone caused a significant reduction of MCT8-mediated T3 uptake only at the highest concentrations as follows: − 43% at 50 μM and − 66% at 100 μM. This effect was weaker than that produced by desethylamiodarone and dronedarone. In fact, desethylamiodarone significantly inhibited T3 uptake in COS-7 transfected with hMCT8 starting from 10 μM (− 36.5%) and determined a 72% of inhibition at 100 μM; dronedarone inhibited T3 uptake in the same cells from − 38% at 1 μM concentration to − 86% inhibition at 100 μM (Fig. 3b).
Anxiolytic drug
Buspirone resulted as a potent inhibitor, significantly reducing the uptake of T3 in hMCT8-transfected cells even at low concentrations. After exposure to buspirone (1–125 μM), the reduction of MCT8-mediated T3 uptake ranged between − 38 and − 86% (Fig. 3c).
Anticonvulsant agents
As shown in Fig. 3d, both carbamazepine and valproic acid did not show any inhibitory effect on MCT8-mediated T3 uptake at all concentrations used (all P > 0.05).
l-Carnitine
The widespread dietary supplement l-carnitine behaved as weak inhibitor of MCT8. In fact, when coapplied for 15 min, it significantly inhibited T3 uptake in hMCT8 transfected COS-7 only at very high concentrations that are 500 mM and 1 M (all P < 0.001). At these concentrations baseline T3 uptake was reduced by 51% and 68%, respectively (Fig. 3e).
Mode of inhibition
For each inhibiting drug the concentration determining 50% reduction of T3 uptake (IC50) was evaluated, and the results are reported in Table 2. Thereafter, in order to determine the mode of inhibition, we titrated substrate concentrations in the presence or not of drugs (i.e. 635 μM hydrocortisone, 48.5 μM dexamethasone, 63 μM amiodarone, 53.1 μM desethylamiodarone, 35.7 μM buspirone, 503 mM l-carnitine or 50 μM BSP). Plotting the data according to Eadie–Hofstee diagram, for all drugs tested we observed an essentially parallel shift of the curve in the presence of each inhibitor (Km values remained constant in the order to 10–2 μM, while a decrease of Vmax values was observed), suggesting a predominantly noncompetitive mode of inhibition of MCT8-mediated T3 transport by these substances (Fig. 4a–g). For the positive control BSP a competitive mode of inhibition was observed as also described in literature (Fig. 4h).
Eadie–Hofstee plot of labeled T3 uptake in the presence of the concentration of each substance corresponding to the IC50 value. a Hydrocortisone, b dexamethasone, c amiodarone, d desethylamiodarone, e dronedarone, f buspirone, g l-carnitine, h bromsulphthalein (BSP) 50 µM concentration, positive control
Effects of drugs on T3 efflux
Since MCT8 functions also as a T3 exporter [7], we tested whether the drugs able to reduce T3 uptake could inhibit T3 efflux as well. None of these drugs affected T3 release from cells transfected with hMCT8 at the respective maximal inhibitory concentration (Fig. 5a, b).
Discussion
Interfering effects of drugs on MCT8 function have been so far poorly investigated and proved for only few compounds.
Aiming at identifying new classes of inhibitors, we screened in vitro the effect on MCT8 of a set of common drugs, and we found inhibition of the T3 transport by some of these drugs and at certain concentrations.
Among the glucocorticoids tested, hydrocortisone significantly inhibited T3 uptake by MCT8 only at high concentrations, i.e. 500 and 1000 μM, with an IC50 of 635 μM. These values are far from the therapeutic plasma levels of the drug reached during the replacement therapy of adrenal insufficiency. In fact, after an oral dose of 20 mg/day of hydrocortisone the plasma levels of drug are around 8 μM [38], making unlikely an in vivo effect on MCT8, unless hydrocortisone can exert partial inhibition in some organs during long-term treatment or can accumulate in some tissue. Concentrations lower than those having an inhibiting effect in our in vitro system are also reached after intravenous administration of 100–300 mg/day used for anti-inflammatory purposes [39]. Prednisone and prednisolone were devoid of inhibitory potential on T3 uptake by MCT8 in the statistical modeling used in this study. In contrast, dexamethasone behaved as a more potent inhibitor. Indeed, it could significantly inhibit T3 transport into hMCT8-transfected COS-7 cells already at 10 μM concentration and showed an IC50 of 48.5 μM. These findings make more likely an in vivo effect of the drug on MCT8.
Dexamethasone is a synthetic glucocorticoid used as long-term treatment of adults affected by congenital adrenal hyperplasia (CAH). Furthermore, it can also be used throughout pregnancy in the management of fetuses with CAH or administered during early pregnancy if a fetal CAH is suspected. Finally, it is indicated for the management of women at risk of preterm birth, since it promotes the rapid maturation of underdeveloped organs in the fetus [26, 27, 40, 41]. However, the use of this drug as that of other synthetic glucocorticoids, especially if administered as multiple courses, has been associated with adverse effect on the developing brain [18,19,20, 39,40,41]. Recommended treatment courses include four doses of 6 mg dexamethasone administered intramuscularly every 12 h, reaching mean maximum plasma levels higher than 400 nmol/L [42]. A study performed on mice showed reduced plasticity and a lower number of proliferating cells in the hippocampus, impaired cognitive function, and reduced lifespan after a single dose of dexamethasone administered prenatally [43]. In humans, dose-dependent associations are found between repeated administration of dexamethasone prenatally and the incidence of periventricular leukomalacia and neurodevelopmental abnormalities [44], attention deficits in children of two years of age [45], and poorer cognitive performance at 6 years of age [46]. All these evidences, together with the potential teratogenicity and long-term effects of prenatal treatment with dexamethasone, prompted the authors of the 2018 Endocrine Society’s guidelines on CAH to do not recommend specific prenatal treatment protocols and to advise that clinicians continue to regard prenatal therapy with dexamethasone as experimental [47]. In contrast, evaluation of treatment with hydrocortisone of premature infants found no difference in cognitive function, incidence of cerebral palsy, motor function or occurrence of brain lesions on MRI [48]. These differences are usually explained by pharmacological differences between dexamethasone and hydrocortisone [18], but our study shows that other factors might contribute to these disparities such as the different effect of these drugs on MCT8-mediated T3 transport. The adverse cerebral effects of synthetic glucocorticoids are attributed to impaired neuronal glucose uptake, decreased excitability, atrophy of dentrites, altered development of myelin-producing oligodendrocytes, and perturbation of important structures involved in axonal transport evoked by genomic and not genomic action of these drugs [18, 19]. However, the findings herein reported suggest that some of the detrimental neurological effects of dexamethasone can also be due or enhanced by the reduced TH entry into brain caused by the inhibition of MCT8-mediated transport; indeed, the association between hypothyroidism and neurological and psychiatric impairment [49, 50] is well known. As the mode of inhibition in our cellular system was noncompetitive, dexamethasone likewise blocks the substrate channel of MCT8 through direct binding to the transporter, a property that it shares only partially with hydrocortisone, but not with the other glucocorticoids tested in the present study.
The antiarrhythmic agents amiodarone, its main metabolite DEA, and the derivative dronedarone were the other drugs tested in our heterologous expression system for interfering effects on MCT8. Only few previous studies in rat cell lines, performed before the identification of the different classes of TH transporters, have showed some inhibiting effects of amiodarone on TH transport into hepatocytes and pituitary cells [51, 52]. In COS-7 cells transiently transfected, we found that amiodarone caused a significant reduction of T3 uptake by MCT8 only at 50 and 100 μM with an inhibition of 44 and 68%, respectively, of baseline values. Its metabolite DEA produced a stronger effect, reducing the T3 uptake already at 10 μM. Serum levels of amiodarone in humans receiving long-term treatment vary from 1 to 6 μM [53], which are, therefore, lower than the inhibiting concentrations observed in the present study. However, amiodarone is concentrated in certain tissues over time, and it may conceivably accumulate at levels that would allow it to work as inhibitor of MCT8 transport. Indeed, autopsy studies have revealed that liver, lung, and heart preferentially accumulate high concentrations of the drug, containing between 2600 mg/kg and 200 mg/kg of amiodarone and desethylamiodarone, while brain and thyroid gland accumulate 60 mg/kg [53]. In light of the foregoing, amiodarone might produce variable in vivo effects on different tissues based on varying concentrations within tissue and the type of TH transmembrane transporters expressed. The mode of inhibition we found for both compounds was noncompetitive; therefore; it might be postulated that amiodarone and its metabolite bind to MCT8 and hamper T3 uptake by steric hindrance or conformational changes, but this hypothesis remains to be proven. Dronedarone exhibited the strongest effect inhibiting T3 uptake by MCT8 starting from 1 μM concentration and also in a noncompetitive manner. In vivo, relatively high doses of dronedarone (100 mg/kg/day) are required to reduce plasma concentrations of TSH, T3, and T4 significantly [28]. Although it has little effect on plasma thyroid hormones, our results suggest that it can alter TH status in some tissues by reducing transmembrane transport mediated by MCT8.
Similarly to dronedarone and dexamethasone, in our in vitro system the psychotropic agent buspirone acted as a potent inhibitor of MCT8, significantly reducing the uptake of T3 by MCT8 even at low concentrations. Therapeutic plasma levels of buspirone range between 1.6 and 4.8 μM, values which are in the same order of our inhibiting concentration in vitro. Buspirone is an anxiolytic medication that acts as a partial serotonin 1A receptor agonist. It is also used in major depression in augmentation with SSRIs or tricyclic antidepressants, showing, however, to be less effective than T3 in improving the response of clinical non responders [30, 31]. It is well known that thyroid hormones influence mood [29]. Since previous studies have suggested a possible inhibition of antidepressant DMI on T3 uptake in neurons [12] our data show that it should be safe to avoid the association of these two drugs for a possible additive effect on T3 transport in brain.
In contrast with buspirone and the above described drugs, the anticonvulsants carbamazepine and valproic acid did not show any inhibitory effect on MCT8-mediated T3 uptake at all concentrations used. We decided to test these drugs because TFTs abnormalities have been reported during their use [32]. Specifically, a reduction in serum T4 and less frequently in T3, associated with unchanged TSH levels, has been found in children using carbamazepine. Although the results are controversial, studies report alteration in TFTs also during treatment with valproic acid, being subclinal hypothyroidism the more frequent feature found [32]. Carbamazepine seems to increase the metabolism of the TH in the liver and the peripheral conversion of T4 to T3; furthermore, it competitively binds to thyroxin-binding globulin [54,55,56]. For valproic acid the mechanisms are only hypothesized and not clearly established [57]. Our study seems to exclude for both drugs an inhibitory effect on MCT8 function as the pathogenetic mechanism of the associated TFTs.
Last, we tested the effect of l-carnitine on T3 transport mediated by MCT8. In our in vitro system l-carnitine behaved as a weak inhibitor of T3 transport by MCT8. In fact, T3 uptake was reduced only at very high concentrations of l-carnitine (500 mM and 1 M), values not reached even during oral administration of pharmacological doses of l-carnitine (i.e. in the order of grams) [58, 59]. Plasma carnitine concentrations are approximately 0.05 mM, which are 20- to 100-times less than in tissues, being the highest tissue concentration around 100 mM [60]. Therefore, it can be hypothesized that l-carnitine could exert its inhibitory effect on transmembrane cell transporters other than MCT8 and, as previously shown, manly on a still unknown nuclear membrane TH transporter [35].
Interestingly, none of the substances able to reduce uptake by MCT8 affected efflux of T3. The current mechanism of membrane traversing for TH by MCT8 is that of the two banana-shaped 6-transmebrane helix bundle tilting around a central TH-interacting cavity, with alternating extra-and intracellular accessibility [10]. Starting from this model, the possible explanation for the lack of effect on efflux of the tested compounds may be the conformational change induced by the binding of these drugs to some sites of TH-interacting cavity, that while blocking extracellular TH entrance leads to an enlargement of the intracellular entrance. One such phenomenon has been already described in association with mutations of MCT8 gene [10].
Conclusion
In this study we show in vitro a novel effect of some commonly used drugs, which is the inhibition of T3 transport into cells mediated by MCT8. Specifically, hydrocortisone, amiodarone, and l-carnitine modestly inhibit T3 uptake, whereas dexamethasone, desethylamiodarone, dronedarone, and buspirone behave as potent inhibitors. Treatment with these substances may interfere with T3 delivery and action in the tissues where MCT8 represents the main mediator of transmembrane passage of TH. Perturbation of tissue TH concentrations may explain some of the side effects related to the use of these drugs.
References
Dumitrescu AM, Liao XH, Best TB, Brockmann K, Refetoff S (2004) A novel syndrome combining thyroid and neurological abnormalities is associated with mutations in a monocarboxylate transporter gene. Am J Hum Genet 74(1):168–175. https://doi.org/10.1086/380999
Friesema EC, Grueters A, Biebermann H, Krude H, von Moers A, Reeser M, Barrett TG, Mancilla EE, Svensson J, Kester MH (2004) Association between mutations in a thyroid hormone transporter and severe X-linked psychomotor retardation. Lancet 364:1435–1437. https://doi.org/10.1016/S0140-6736(04)17226-7
Dumitrescu AM, Refetoff S (2013) The syndromes of reduced sensitivity to thyroid hormone. Biochim Biophys Acta 1830(7):3987–4003. https://doi.org/10.1016/j.bbagen.2012.08.005
Nishimura M, Naito S (2008) Tissue-specific mRNA expression profiles of human solute carrier transporter superfamilies. Drug Metab Pharmacokinet 23(1):22–44. https://doi.org/10.2133/dmpk.23.22
Friesema EC, Visser TJ, Borgers AJ, Kalsbeek A, Swaab DF, Fliers E, Alkemade A (2012) Thyroid hormone transporters and deiodinases in the developing human hypothalamus. Eur J Endocrinol 167(3):379–386. https://doi.org/10.1530/EJE-12-0177
Roberts LM, Woodford K, Zhou M, Black DS, Haggerty JE, Tate EH, Grindstaff KK, Mengesha W, Raman C, Zerangue N (2008) Expression of the thyroid hormone transporters monocarboxylate transporter-8 (SLC16A2) and organic ion transporter-14 (SLCO1C1) at the blood-brain barrier. Endocrinology 149(12):6251–6261. https://doi.org/10.1210/en.2008-0378
Friesema EC, Ganguly S, Abdalla A, Manning Fox JE, Halestrap AP, Visser TJ (2003) Identification of monocarboxylate transporter 8 as a specific thyroid hormone transporter. J Biol Chem 278(41):40128–40135. https://doi.org/10.1074/jbc.m300909200
Friesema EC, Kuiper GG, Jansen J, Visser TJ, Kester MH (2006) Thyroid hormone transport by the human monocarboxylate transporter 8 and its rate-limiting role in intracellular metabolism. Mol Endocrinol 20(11):2761–2772. https://doi.org/10.1210/me.2005-0256
Friesema EC, Jansen J, Jachtenberg J, Visser WE, Kester M, Visser T (2008) Effective cellular uptake and efflux of thyroid hormone by human monocarboxylate transporter 10. Mol Endocrinol 22(6):1357–1369. https://doi.org/10.1210/me.2007-0112
Protz J, Braun D, Hinz KM, Bayer-Kusch D, Schweizer U, G. Krause G, (2017) Membrane-traversing mechanism of thyroid hormone transport by monocarboxylate transporter 8. Cell Mol Life Sci 74(12):2299–2318. https://doi.org/10.1007/s00018-017-2461-9
Groeneweg S, van Geest FS, Peeters RP, Heuer H, Visser WE (2020) Thyroid HORMONE TRANSPORTERS. Endocr Rev 41(2):146–201. https://doi.org/10.1210/endrev/bnz008
Roth S, Kinne A, Schweizer U (2010) The tricyclic antidepressant desipramine inhibits T3 import into primary neurons. Neurosci Lett 478(1):5–8. https://doi.org/10.1016/j.neulet.2010.04.055
Braun D, Kim TD, le Coutre P, Köhrle J, Hershman JM, Schweizer U (2012) Tyrosine kinase inhibitors noncompetitively inhibit MCT8-mediated iodothyronine transport. J Clin Endocrinol Metab 97(1):E100-105. https://doi.org/10.1210/jc.2011-1837
Braun D, Schweizer U (2014) Authentic bosutinib inhibits triiodothyronine transport by monocarboxylate transporter 8. Thyroid 24(5):926–927. https://doi.org/10.1089/thy.2013.0660
Johannes J, Jayarama-Naidu R, Meyer F, Wirth EK, Schweizer U, Schomburg L, Köhrle J, Renko K (2016) A flavonolignan derived from the milk thistle, is a potent inhibitor of the thyroid hormone transporter MCT8. Endocrinology 157:1694–1701. https://doi.org/10.1210/en.2015-1933
Shaji D (2021) Identification of inhibitors based on moleular docking: thyroid hormone transmembrane transporter MCT8 as a target. Curr Drug Discov Technol 18(1):105–112. https://doi.org/10.2174/1570163816666191125123142
Schweizer U, Braun D, Forrest D (2019) The ins and outs of steroid hormone transport across the plasma membrane: insight from an insect. Endocrinology 160(2):339–340. https://doi.org/10.1210/en.2018-01034
Damsted SK, Born AP, Paulson OB, Uldall P (2011) Exogenous glucocorticoids and adverse cerebral effects in children. Eur J Paediatr Neurol 15(6):465–477. https://doi.org/10.1016/j.ejpn.2011.05.002
Peffer ME, Zhang JY, Umfrey L, Rudine AC, Monaghan AP, DeFranco DB (2015) Minireview: the impact of antenatal therapeutic synthetic glucocorticoids on the developing fetal brain. Mol Endocrinol 29(5):658–666. https://doi.org/10.1210/me.2015-1042
Carson R, Monaghan-Nichols AP, DeFranco DB, Rudine AC (2016) Effects of antenatal glucocorticoids on the developing brain. Steroids 114:25–32. https://doi.org/10.1016/j.steroids.2016.05.012
Martino E, Bartalena L, Bogazzi F, Braverman LE (2001) The effects of amiodarone on the thyroid. Endoc Rev 22(2):240–254. https://doi.org/10.1210/edrv.22.2.0427
Kannan R, Ookhtens M, Chopra IJ, Singh BN (1984) Effects of chronic administration of amiodarone on kinetics of metabolism of iodothyronines. Endocrinology 115(5):1710–1716. https://doi.org/10.1210/endo-115-5-1710
Singh BN, Vaughan Williams EM (1970) The effect of amiodarone, a new anti-anginal drug, on cardiac muscle. Br J Pharmacol 39(4):657–667. https://doi.org/10.1111/j.1476-5381.1970.tb09891.x
Bogazzi F, Bartalena L, Brogioni S, Burelli A, Raggi F, Ultimieri F, Cosci C, Vitale M, Fenzi G, Martino E (2001) Desethylamiodarone antagonizes the effect of thyroid hormone at the molecular level. Eur J Endocrinol 145(1):59–64. https://doi.org/10.1530/eje.0.1450059
Stoykov L, van Beeren HC, Moorman AFM, Christoffels VM, Wiersinga WM, Bakker O (2007) Effect of amiodarone and dronedarone administration in rats on thyroid hormone-dependent gene expression in different cardiac components. Eur J Endocrinol 156(6):695–702. https://doi.org/10.1530/eje-07-0017
Hudig F, Bakker O, Wiersinga WM (1997) Tri-iodothyronine prevents the amiodarone-induced decrease in the expression of the liver low-density lipoprotein receptor gene. J Endocrinol 152(3):413–421. https://doi.org/10.1677/joe.0.1520413
van Beeren HC, Bakker O, Chatterjee VK, Wiersinga WM (1999) Effect of mutations in the beta1-thyroid hormone receptor on the inhibition of T3 binding by desethylamiodarone. FEBS Lett 450(1–2):35–38. https://doi.org/10.1016/s0014-5793(99)00453-6
van Beeren HC, Jong WMC, Kaptein E, Visser TJ, Bakker O, Wiersinga WM (2003) Dronerarone acts as a selective inhibitor of 3,5,3′-triiodothyronine binding to thyroid hormone receptor-alpha1: in vitro and in vivo evidence. Endocrinology 144(2):552–558. https://doi.org/10.1210/en.2002-220604
Hall RC (1983) Psychiatric effects of thyroid hormone disturbance. Psychosomatics 24(1):7–11, 15–18. https://doi.org/10.1016/s0033-3182(83)73255-x
Appelberg BG, Syvalahti EK, Koskinen TE, Mehtonen OP, Muhonen TT, Naukkarinen HH (2001) Patients with severe depression may benefit from buspirone augmentation of selective serotonin reuptake inhibitors: results from a placebo-controlled, randomized, double-blind, placebo wash-in study. J Clin Psychiatry 62(6):448–452. https://doi.org/10.4088/jcp.v62n0608
Onder E, Tural U (2003) Faster response in depressive patients treated with fluoxetine alone than in combination with buspirone. J Affect Disord 76(1–3):223–227. https://doi.org/10.1016/s0165-0327(02)00090-3
Cansu A (2010) Antiepileptic drugs and hormones in children. Epilepsy Res 89(1):89–95. https://doi.org/10.1016/j.eplepsyres.2009.09.008
Strack E, Woratz G, Rotzsch W (1959) Effects of carnitine in hyperfunction of the thyroid gland. Endokrinologie 38:228–225
Hellthaler G, Wenzel KW, Rotzsch W (1967) Aminotransferases influenced by thyroxine and carnitine. Acta Biol Med Ger 19:641–652
Benvenga S, Lakshmanan M, Trimarchi F (2000) Carnitine is a naturally occurring inhibitor of thyroid hormone nuclear uptake. Thyroid 10(12):1043–1050. https://doi.org/10.1089/thy.2000.10.1043
Kinne A, Kleinau G, Hoefig CS, Grüters A, Köhrle J, Krause G, Schweizer U (2010) Essential molecular determinants for thyroid hormone transport and first structural implications for monocarboxylate transporter 8. J Biol Chem 285(36):28054–28063. https://doi.org/10.1074/jbc.m110.129577
Agretti P, Dimida A, De Marco G, Ferrarini E, Rodrìguez Gonzàlez JC, Santini F, Vitti P, Pinchera A, Tonacchera M (2011) Study of potential inhibitors of thyroid iodide uptake by using CHO cells stably expressing the human sodium/iodide symporter (hNIS) protein. J Endocrinol Investig 34:170–174. https://doi.org/10.1007/BF03347061
Derendorf H, Möllmann H, Barth J, Möllmann C, Tunn S, Krieg M (1991) Pharmacokinetics and oral bioavailability of hydrocortisone. J Clin Pharmacol 31(5):473–476. https://doi.org/10.1002/j.1552-4604.1991.tb01906.x
Dandona P, Thusu K, Hafeez R, Abdel-Rahman E, Chaudhuri A (1998) Effect of hydrocortisone on oxygen free radical generation by mononuclear cells. Metabolism 47(7):788–791. https://doi.org/10.1016/s0026-0495(98)90113-5
Moisiadis VG, Matthews SG (2014) Glucocorticoids and fetal programming part 1: outcomes. Nat Rev Endocrinol 10(7):91–402. https://doi.org/10.1038/nrendo.2014.73
Moisiadis VG, Matthews SG (2014) Glucocorticoids and fetal programming part 2: mecchanism. Nat Rev Endocrinol 10(7):403–411. https://doi.org/10.1038/nrendo.2014.74
Elliott CL, Read GF, Wallace EM (1996) The pharmacokinetics of oral and intramuscular administration of dexamethasone in late pregnancy. Acta Obstet Gynecol Scand 75(3):213–216. https://doi.org/10.3109/00016349609047089
Noorlander CW, Visser GH, Ramakers GM, Nikkels PG, de Graan PN (2008) Prenatal corticosteroid exposure affects hippocampal plasticity and reduces lifespan. Dev Neurobiol 68(2):237–246. https://doi.org/10.1002/dneu.20583
Spinillo A, Viazzo F, Colleonia R, Chiara A, Cerbo RM, Fazzic E (2004) Two-year infant neurodevelopmental outcome after single or multiple antenatal courses of corticosteroids to prevent complications of prematurity. Am J Obstet Gynecol 191(1):217–224. https://doi.org/10.1016/j.ajog.2003.12.023
Crowther CA, Doyle LW, Haslam RR, Hiller JE, Harding JE, Robinson JS (2004) Outcomes at 2 years of age after repeat doses of antenatal corticosteroids. N Eng J Med 357(12):217–224. https://doi.org/10.1056/nejmoa071152
MacArthur BA, Howie RN, Dezoete JA, Elkins J (1982) School progress and cognitive development of 6-year-old children whose mothers were treated antenatally with betamethasone. Pediatric 70(1):99–105
Speiser PW, Arlt W, Auchus RJ, Laurence SB, Conway GB, Merke DB, Meyer-Bahlburg PL, Miller WL, Murad MH, Sharon E (2018) Oberfield congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 103(11):4043–4088. https://doi.org/10.1210/jc.2018-01865
Rademaker KJ, Uiterwaal CS, Groenendaal F, Venema MM, van Bel F, Beek FJ, van Haastert IJ, Grobbee DE, de Vries LS (2007) Neonatal hydrocortisone treatment: neurodevelopmental outcome and MRI at school age in preterm-born children. J Pediatr 150(4):351–357. https://doi.org/10.1016/j.jpeds.2006.10.051
Zoeller RT, Rovet J (2004) Timing of thyroid hormone action in the developing brain: clinical observations and experimental findings. J Neuroendocrinol 16(10):809–818. https://doi.org/10.1111/j.1365-2826.2004.01243.x
Williams GR (2008) Neurodevelopmental and neurophysiological actions of thyroid hormone. J Neuroendocrinol 20(6):784–794. https://doi.org/10.1111/j.1365-2826.2008.01733.x
de Jong M, Docter R, Van der Hoek H, Krenning E, Van der Heide D, Quero C, Plaisier P, Vos R, Hennemann G (1994) Different effects of amiodarone on transport of T4 and T3 into the perfused rat liver. Am J Physiol 266(1PT1):E44-49. https://doi.org/10.1152/ajpendo.1994.266.1.e44
Norman MF, Lavin TN (1989) Antagonism of thyroid hormone action by amiodarone in rat pituitary tumor cells. J Clin Investig 83(1):306–313. https://doi.org/10.1172/jci113874
Holt DW, Tucker GT, Jackson PR, Storey GC (1983) Amiodarone pharmacokinetics. Am Heart J 106(4 Pt 2):840–847. https://doi.org/10.1016/0002-8703(83)90006-6
Connell JM, Rapeport WG, Gordon S, Brodie MJ (1984) Changes in circulating thyroid hormones during short-term hepatic enzyme induction with carbamazepine. Eur J Clin Pharmacol 26(4):453–456. https://doi.org/10.1007/bf00542140
Liewendahl K, Majuri H, Helenius T (1978) Thyroid function tests in patients on long-term treatment with various anticonvulsant drugs. Clin Endocrinol (Oxf) 8(3):185–191. https://doi.org/10.1111/j.1365-2265.1978.tb01493.x
Rootwelt K, Ganes J, Johannessen SJ (1978) Effect of carbamazepine, phenytoin and phenobarbitone on serum levels of thyroid hormones and thyrotropin in humans. Scand J Clin Lab Investig 38(8):731–736. https://doi.org/10.3109/00365517809104880
Kim SH, Chung HR, Kim SH, Kim H, Chan Lim B, Chae JH, Kim KJ, Hwang YS, Hwang H (2012) Subclinical hypothyroidism during valproic acid therapy in children and adolescents with epilepsy. Neuropediatrics 43(3):135–139. https://doi.org/10.1055/s-0032-1313913
Bach AC, Schirardin H, Sihr MO, Storck D (1983) Free and total carnitine in human serum after oral ingestion of l-carnitine. Diabete Metab 9(2):121–124
Harper P, Elwin CE, Cederblad G (1988) Pharmacokinetics of intravenous and oral bolus doses of l-carnitine in healthy subjects. Eur J Clin Pharmacol 35(1):69–75. https://doi.org/10.1007/bf00555510
Bremer J (1997) The role of carnitine in cell metabolism. In: De Simone C, Famularo G (eds) Carnitine today. RG Landes Company, Austin, pp 1–37
Acknowledgements
We thank Dr. Alexandra M. Dumitrescu for kindly providing hMCT8 cloned in pcDNA3 expression vector.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
CDC designed, performed and interpreted the data and wrote the manuscript. GDM, EF, AD design of the work and interpretation of data. PA interpreted the data and revised the manuscript. PF analyzed the data. SB, PV, MT revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this article.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Di Cosmo, C., De Marco, G., Agretti, P. et al. Screening for drugs potentially interfering with MCT8-mediated T3 transport in vitro identifies dexamethasone and some commonly used drugs as inhibitors of MCT8 activity. J Endocrinol Invest 45, 803–814 (2022). https://doi.org/10.1007/s40618-021-01711-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01711-4