Abstract
Objective
Vitamin D deficiency is widespread and often reported in subjects treated for osteoporosis. Optimal vitamin D repletion was previously shown to maximize the efficacy of anti-resorptive agents. To date, no information exists about the role of vitamin D in the response to strontium ranelate (SrR) treatment. The aim of our study was to investigate the BMD response to SrR in accordance with change of vitamin D status.
Methods
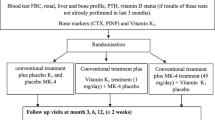
A retrospective analysis of 108 women receiving SrR for postmenopausal osteoporosis was carried out. Women were treated with SrR (2 g/day), with cholecalciferol (25,000 IU biweekly) and calcium carbonate as appropriate. Lumbar spine and femoral neck BMD, bone formation markers (BGP, ALP), resorption marker (OH-PRO) and serum 25(OH)D were measured at baseline after 18-months. All participants were divided into two groups according to the median variation of 25(OH)D over the observation period.
Results
SrR was associated with improvement of BMD at lumbar spine (p < 0.0001) and to a non significant variation at femoral neck (p = 0.2). Only subjects with Δ25(OH)D > 6.14 %, reported a significant BMD gain at femoral neck (p = 0.03). Change of BMD at femoral neck was positively associated with modification of ALP (r = 0.28, p = 0.01). This association was not maintained when considering only women with Δ25(OH)D < 6.14 % (r = 0.28, p = 0.09). At a multiple regression analysis, ALP change was the only predictor of femoral neck BMD modification (β 0.13; SE 0.05; p = 0.01).
Conclusion
Improvement of vitamin D status was associated with enhancement of BMD response to SrR in women with postmenopausal osteoporosis, in particular, at femoral neck.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D deficiency is a common condition among elderly subjects, particularly in Southern European countries [1]. Although there is no consensus on optimal serum levels of 25(OH)D, most experts consider a 25(OH)D level less than 20 ng/mL to be indicative of vitamin D deficiency. 25(OH)D levels are inversely associated with PTH levels until the former reach 30–40 ng/mL, then PTH begins to level off; thus, 25(OH)D levels of 21–29 ng/mL can be considered to indicate a relative insufficiency of vitamin D, and a level greater than 30 ng/mL can be indicative of sufficient vitamin D [2–6]. It was previously reported that more than 50 % of postmenopausal women taking medication for osteoporosis had 25(OH)D levels below 30 ng/mL [4]. Low 25(OH)D levels affect bone metabolism through osteoclastic bone resorption and bone loss induced by enhanced PTH secretion, but also negatively impact on muscle mass and function [4, 7]. Vitamin D deficiency has been associated with an increased risk of falls, because of impaired muscle function, this contributing, at least in part, to the development of osteoporotic fractures [1–7]. Maintenance of optimal calcium intake and vitamin D status are required for optimal therapeutic efficacy of bisphosphonates, the most commonly used drugs for the treatment of osteoporosis. An inverse association between vitamin D repletion and the changes in BMD at both the spine and the hip after treatment with anti-resorbers was reported [8, 9].
Strontium ranelate (SrR) is a current treatment option for postmenopausal and male osteoporosis [10–12]. It has been proposed that SrR acts by simultaneously promoting bone formation and inhibiting bone resorption, leading to a gain of BMD, an increase of bone strength and finally, a fracture risk reduction [10–13].
In randomized clinical trials designed to assess the efficacy of SrR in decreasing fracture risk, recruited postmenopausal women used calcium and vitamin D supplements as adjunctive therapy [10, 11]. Several guidelines recommend guaranteeing a good intake of calcium and vitamin D in subjects treated for osteoporosis. In a clinical setting of postmenopausal women with established osteoporosis, an inadequate clinical response to anti-resorptive agents was associated to poorer treatment compliance and a less frequent co-administration of calcium and vitamin D supplements [14]. To date, it is not known whether improving vitamin D status could enhance the efficacy of SrR in term of BMD, thus the aim of our study was to address this issue.
Methods
We carried out a retrospective analysis of 108 patients selected from women attending the Outpatients Clinic for Osteoporosis in the Department of Clinical and Experimental Medicine of the University Hospital of Messina. Study subjects were osteoporotic postmenopausal women with evidence of prevalent clinical or morphometric vertebral fractures that were treated with SrR. Women were excluded if they had steroid use or medical conditions associated with bone loss, including renal disease (creatinine clearance <30 mL/min), active malignancy, hyperparathyroidism, and malabsorption syndromes; women with an adherence to SrR treatment <80 % checked by count of sachets or women lost to follow-up were not considered in this analysis. Previous oral or intramuscular treatment with BPs was not an exclusion criterion, whether BPs had been suspended more than six months prior to the administration of SrR.
All subjects received treatment with SrR 2 g once a day at bedtime (2 h after food) and vitamin D (cholecalciferol 25,000 IU biweekly). Subjects with an estimated poor calcium intake were supplied with calcium carbonate (500–1000 mg, daily) to reach the recommended daily allowance of calcium.
BMD was assessed by a dual-energy X-ray absorptiometry (DXA) densitometer (Hologic 4500 QDR) at the lumbar spine (L1–L4) in AP projection and at the femoral neck. DXA densitometer was calibrated on a daily basis according to the manufacturer’s instruction and its coefficient of variation (CV) was 0.5 % with the standard phantom. BMD measurement was obtained before SrR treatment and then was repeated after 18 months. Bone formation markers, such as serum osteocalcin (BGP) and alkaline phosphatase (ALP), and urinary hydroxyproline (OH-PRO) as resorption marker, were assessed before and after SrR treatment in all the subjects considered. Serum 25(OH)D, calcium, phosphorus, creatinine were also measured.
25(OH)D and urine OH-PRO were determined by high-performance liquid chromatography (Bio-Rad Laboratories); BGP was measured by immunoenzymatic assay (Invitrogen Ltd, UK) with an intra-assay coefficient of variance (CV) of 3.1 % and inter-assay CV of 3.5 %. Calcium, phosphorus, ALP and creatinine were measured by routine procedures. All participants were considered together and then divided into two groups according to the median variation of serum 25(OH)D. The research was conducted in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. For this retrospective study, formal consent was not required.
Statistical analyses were performed using MedCalc software (version 10.2.0.0; MedCalc Software, Mariakerke, Belgium). The Kolmogorov–Smirnov test for normality was used to assess the distribution of the data. Values were expressed as mean ± SD or median (interquartile range). Comparisons between groups were performed by unpaired t test or Mann–Whitney test, and within-group comparisons were determined with a paired t test or Wilcoxon matched rank sum test for paired data as appropriate. The Spearman correlation coefficient rho was calculated to evaluate the correlation between variables, and multiple regression was performed to analyze the relationship between a dependent variable and one or more predictor variables. For all tests, a p value <0.05 was considered to indicate statistical significance. All reported p values were two-sided.
Results
At baseline, the study population (age 59.68 ± 8.65 years; time since menopause 8.62 ± 2.46 years; BMI 24.8 ± 3.8 kg/m2) showed sufficient serum levels of 25(OH)D (Table 1). Treatment with SrR was associated with an improvement of BMD at lumbar spine (p < 0.0001) and with minor non significant gain of BMD at femoral neck (p = 0.2) in comparison to baseline. After 18 months, modifications of bone turnover markers were observed, with a slight, not significant, reduction of OH-PRO (p = 0.22) and a significant increase of BGP (p < 0.0001), ALP (p = 0.008). At the same time, levels of 25(OH)D rose in comparison to baseline (p = 0.01). In accordance with the median percent modification of 25(OH)D over the observation period (6.14 %), the entire population was divided into two groups (with 25(OH)D variation > or < of 6.14 %) (Table 2). Age, time since menopause, BMI, smoking and alcohol habit, as well as number and severity of prevalent vertebral fractures were not significantly different between the two groups (data not shown). Subjects with the 25(OH)D variation greater than 6.14 % reported a significant increase of BMD at both lumbar spine (p = 0.01) and femoral neck (p = 0.03), whereas, subjects with the 25(OH)D variation lower than 6.14 % showed a significant increase of only lumbar spine (p = 0.01), but not femoral neck BMD (p = 0.30). Percent modification of BMD was related to variation of 25(OH)D levels at femoral neck site, and women with 25(OH)D variation greater than 6.14 % reported the highest femoral neck BMD gain in comparison to subjects with 25(OH)D variation lower than 6.14 % [5.2 % (0.2–8.3) vs. 1.5 % (−1.5 to 6), respectively] (Fig. 1). In both groups, subjects previously exposed to BPs (56 and 52 % among women with 25(OH)D variation greater than 6.14 % and lower than 6.14 %, respectively) exhibited a BMD gain not significantly different in comparison to subjects not exposed to BPs.
In the overall population, the variation of BMD at femoral neck was positively associated to modification of ALP (r = 0.28, p = 0.01). This association was maintained in the group of subjects with the variation of 25(OH)D > 6.14 % (r = 0.33, p = 0.04), but not in subjects with 25(OH)D < 6.14 % (r = 0.287, p = 0.09). At a multiple regression analysis, ALP variation over time was the only predictor of femoral neck modification even after correcting for age, BMI, and modification of BGP and OH-PRO levels (β 0.13; SE 0.05; p = 0.01).
Treatment with SrR associated with vitamin D and calcium was well-tolerated and no adverse events, including clinical fractures or cardiovascular disorders, were reported during the observation period.
Discussion
This study highlights for the first time the role of vitamin D status in the enhancement of efficacy of SrR treatment in a clinical setting. Our findings suggest that women improving their vitamin D status, as measured by 25(OH)D serum levels, show a more relevant gain of BMD both at lumbar spine and at femoral neck.
BMD is a surrogate marker of bone strength and a large percentage of the anti fracture efficacy observed with antiosteoporotic drugs can be explained by changes in BMD [15]. An analysis of data from the SOTI and TROPOS trials provided that increases in BMD obtained with SrR translated into reduced fracture risk, and each percentage point increase in femoral neck BMD was associated with a 3 % reduction in risk of new vertebral fracture [16, 17].
As known, vitamin D is able to reduce fracture risk possibly through a reduction in fall risk. This ability of vitamin D could be associated with improvement of muscle function, but also with positive effects on cognitive function that have been previously shown to be a risk factor for falling, at least in elderly women [18]. Fracture risk reduction obtained by vitamin D administration was estimated to yield cost savings through reduction of hip fracture alone in the first year [19].
Moreover, in a recent meta-analysis of 23 randomized controlled trials of vitamin D with calcium or vitamin D alone, Reid et al. [20] found a small but significant positive effect of the treatment on femoral neck BMD. The latter point is consistent with our data showing a more pronounced effect of SrR on femoral neck BMD in subjects that improved their vitamin D status. Because calcium and strontium have common chemical features and are absorbed by the same pathways, it could be speculated that improving vitamin D status could affect calcium, but also strontium intestinal absorption. Nevertheless, Vilaca T et al. [21] have recently found no difference at a 4-h oral strontium overload test, according to vitamin D status, and vitamin D replacement in the deficient subjects was not able to enhance strontium absorption.
The role of vitamin D in the medical management of postmenopausal osteoporosis is otherwise highlighted by inadequate response to BPs, which represent to date the most prescribed drugs for osteoporosis [22]; indeed, patients classified as inadequate responders to BPs treatment, by BMD loss or the development of fractures, presented significantly lower levels of 25(OH)D despite vitamin D supplementation, and maintenance of 25(OH)D serum levels higher than 30 ng/ml was claimed to obtain adequate response to BPs [23].
Our data confirm that improving 25(OH)D level with cholecalciferol administration is useful to optimize the effects of SrR on BMD. In accordance with these findings, it was observed that a combination of SrR and alfacalcidol improves bone quality to a greater extent than SrR alone, reducing PTH levels significantly in patients with established osteoporosis [24].
SrR treatment was well-tolerated in this study, and no adverse events were recorded; in particular, no patients reported any clinical fractures, or any type of cardiovascular diseases. In addition to the already known risk of venous thromboembolism, the European Medicines Agency has recently reported that SrR increases the risk of myocardial infarction in postmenopausal women [25]. A growing body of evidence suggests that vitamin D deficiency may adversely affect the cardiovascular system [26]; remarkably, in our study population, mean values of 25(OH)D were considered sufficient, and possibly have preserved the cardiovascular health of patients, although this research study was not aimed to look at cardiovascular safety.
Limitations of our research are the retrospective design, the lack of quantitative information on physical activity and the overall health status of patients, the inclusion of only patients who did return for a follow-up visit, and the use of OH-PRO that is not a specific bone resorption marker. Moreover, the sample size is small and the observation period is not long enough to account for fractures. However, our findings came from real life and this is the first time that modification of vitamin D status has been reported to affect the BMD response to SrR.
In conclusion, our results show that in postmenopausal women with severe osteoporosis, the magnitude of BMD gain with SrR may depend, at least in part, on the modification of vitamin D status.
References
Isaia G, Giorgino R, Rini GB, Bevilacqua M, Maugeri D, Adami S (2003) Prevalence of hypovitaminosis D in elderly women in Italy: clinical consequences and risk factors. Oteoporos Int 14:577–582
Holick MF (2006) Resurrection of vitamin D deficiency and rickets. J Clin Invest 116:2062–2072
Holick MF (2006) High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc 81:353–373
Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, Petruschke RA, Chen E, de Papp AE (2005) Prevalence of vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab 90:3215–3224
Romagnoli E, Carnevale V, Biondi P, Minisola S (2014) Vitamin D supplementation: when and how? J Endocrinol Invest 37(7):603–607
Reid IR (2014) Effects of vitamin D supplements on bone density. J Endocrinol Invest (Epub ahead of print)
Cipriani C, Romagnoli E, Carnevale V, Clerico R, Pepe J, Cilli M, Diacinti D, Savoriti C, Colangelo L, Minisola S (2013) Effect of a single oral dose of 600,000 IU of cholecalciferol on muscle strength: a study in young women. J Endocrinol Invest 36(11):1051–1054
Adami S, Giannini S, Bianchi G, Sinigaglia L, Di Munno O, Fiore CE, Minisola S, Rossini M (2009) Vitamin D status and response to treatment in post-menopausal osteoporosis. Osteoporos Int 20(2):239–244
Carmel AS, Shieh A, Bang H, Bockman RS (2012) The 25(OH)D level needed to maintain a favorable bisphosphonate response is 33 ng/mL. Osteoporos Int 23(10):2479–2487
Meunier PJ, Roux C, Seeman E, Ortolani S, Badurski J, Spector T, Cannata J, Balogh A, Lemmel EM, Pors-Nielsen S, Rizzoli R, Genant HK, Reginster JY (2004) The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med 350:459–468
Reginster JY, Seeman E, De Vernejoul MC, Adami S, Compston J, Phenekos C, Devogelaer JP, Curiel MD, Sawicki A, Goemaere S, Sorensen OH, Felsenberg D, Meunier PJ (2005) Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) study. J Clin Endocrinol Metab 90(5):2816–2822
Kaufman JM, Audran M, Bianchi G, Braga V, Diaz-Curiel M, Francis RM, Goemaere S, Josse R, Palacios S, Ringe JD, Felsenberg D, Boonen S (2013) Efficacy and safety of strontium ranelate in the treatment of osteoporosis in men. J Clin Endocrinol Metab 98(2):592–601
Marie PJ, Ammann P, Boivin G, Rey C (2001) Mechanisms of action and therapeutic potential of strontium in bone. Calcif Tissue Int 69:121–129
Adami S, Isaia G, Luisetto G, Minisola S, Sinigaglia L, Gentilella R, Agnusdei D, Iori N, Nuti R, ICARO Study Group (2006) Fracture incidence and characterization in patients on osteoporosis treatment: the ICARO study. J Bone Miner Res 21(10):1565–1570
Wasnich RD, Miller PD (2000) Antifracture efficacy of antiresorptive agents are related to changes in bone density. J Clin Endocrinol Metab 85(1):231–236
Bruyere O, Roux C, Badurski J, Isaia G, de Vernejoul MC, Cannata J, Ortolani S, Slosman D, Detilleux J, Reginster JY (2007) Relationship between change in femoral neck bone mineral density and hip fracture incidence during treatment with strontium ranelate. Curr Med Res Opin 23:3041–3045
Bruyere O, Roux C, Detilleux J, Slosman DO, Spector TD, Fardellone P, Brixen K, Devogelaer JP, Diaz-Curiel M, Albanese C, Kaufman JM, Pors-Nielsen S, Reginster JY (2007) Relationship between bone mineral density changes and fracture risk reduction in patients treated with strontium ranelate. J Clin Endocrinol Metab 92:3076–3081
Marcelli C, Chavoix C, Dargent-Molina P (2015) Beneficial effects of vitamin D on falls and fractures: is cognition rather than bone or muscle behind these benefits? Osteoporos Int 26(1):1–10
Poole CD, Smith JC, Davies JS (2014) The short-term impact of vitamin D-based hip fracture prevention in older adults in the United Kingdom. J Endocrinol Invest 37(9):811–817
Reid IR, Bolland MJ, Grey A (2014) Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Lancet 383:146–155
Vilaca T, Camargo MB, Rocha OF, Lazaretti-Castro M (2014) Vitamin D supplementation and strontium ranelate absorption in postmenopausal women with low bone mass. Eur J Endocrinol 170(4):469–475
Ishtiaq S, Fogelman I, Hampson G. (2014) Treatment of post-menopausal osteoporosis: beyond bisphosphonates. J Endocrinol Invest (Epub ahead of print)
Peris P, Martínez-Ferrer A, Monegal A, Martínez de Osaba MJ, Muxi A, Guañabens N (2012) 25-hydroxyvitamin D serum levels influence adequate response to bisphosphonate treatment in postmenopausal osteoporosis. Bone 51(1):54–55
Abboskhujaeva LS, Ismailov SI, Alikhanova NM (2014) Efficacy of strontium ranelate in combination with a d-hormone analog for the treatment of postmenopausal osteoporosis. Drugs R D 14(4):315–324
European Medicines Agency (2013) protelos-H-C-560-PSU-31: EPAR-assessment report-periodic safety update report
Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, Benjamin EJ, D’Agostino RB, Wolf M, Vasan RS (2008) Vitamin D deficiency and risk of cardiovascular disease. Circulation 117(4):503–511
Conflict of interest
Antonino Catalano, Nunziata Morabito, Antonina Di Stefano, Elisabetta Morini, Giorgio Basile, Bianca Faraci, Saverio Loddo, Riccardo Ientile and Antonino Lasco have no conflicts of interest.
Ethical standard
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
For this type of study, formal informed consent was not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Catalano, A., Morabito, N., Di Stefano, A. et al. Vitamin D and bone mineral density changes in postmenopausal women treated with strontium ranelate. J Endocrinol Invest 38, 859–863 (2015). https://doi.org/10.1007/s40618-015-0299-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-015-0299-2