Abstract
Purpose
Limited evidence exists on the impact of participation in community-based chronic disease self-management and prevention programs on health disparities. The purpose of this research was to determine the effects of participation in the Healthy Here Wellness Referral System on existing disparities in glycated hemoglobin (HbA1c), systolic blood pressure (BP), and diastolic BP among Hispanic/Latinx adults compared with non-Hispanic White adults.
Methods
We merged administrative clinical and referral data from 2018 through 2022 for adult patients in six focus ZIP codes in New Mexico resulting in a sample of 1331 patients and used regression models to examine predictors of intervention participation as well as propensity-adjusted impacts of participation on HbA1c and BP outcomes.
Results
Non-Hispanic White patients who were referred to community-based programming but did not participate saw statistically significant increases in HbA1c. Hispanic/Latinx patients saw statistically significant decreases in HbA1c with referral alone, with no added benefit from program participation. The impact of participation differed statistically significantly (t(683) = 3.55, p < .001) between these two groups for HbA1c levels, as well as for systolic (t(958) = 2.11, p = .04) and diastolic BP outcomes (t(958) = 2.96, p = .003).
Conclusions
Results of this study support the promise of using centralized referral systems to co-produce health improvement in community settings. Mixed findings highlight the need for further uptake of theory-informed measurement in evaluations seeking to understand heterogeneous program impacts by race and ethnicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attempts to address longstanding health inequities in the United States have led to a range of local, state, and federal responses. Among these, the Centers for Disease Control and Prevention’s Racial and Ethnic Approaches to Community Health (REACH) program aims to reduce health disparities and improve health equity for minoritized populations through the implementation of culturally appropriate, evidence-based interventions [1]. As a REACH initiative, Healthy Here engaged community partners with local knowledge in central New Mexico, co-developing the Healthy Here Wellness Referral System. At the core of the system is the Wellness Referral Center (WRC) that facilitates community-clinical linkages and connects referred patients to community-based physical activity and healthy eating programs [2]. To accomplish this, the WRC established and sustained connections with health clinics in three under-resourced communities in central New Mexico and identified community-based opportunities for chronic-disease prevention and management in and around those communities. This approach is consistent with evidence and recommendations for prevention and control of chronic diseases including diabetes and hypertension [3,4,5,6,7].
Key elements of the Healthy Here WRC map to constructs in the theories of Reasoned Action and Planned Behavior [8] which, together, posit that an individual’s intention to engage in a particular behavior is determined by their attitude toward the behavior, their perceived social norms about the behavior, and their perceived behavioral control [9]. Indeed, WRC activities, by design, reinforced both injunctive and descriptive social norms: provider referral to programs paired with post-clinic follow-up contact from WRC staff helped reinforce injunctive expectations that the behavior was considered desirable by referent others while collective community-based programs, such as cooking classes and walking groups, reinforced descriptive perceptions that the behavior was common among referent others. Additionally, by removing barriers (e.g., covering participation costs, offering programs in Spanish, providing child care) and increasing availability and access (e.g., recruiting local agencies to provide programming) to community-based prevention programs, the Healthy Here WRC sought to enhance individual agency, promoting perceived behavioral control and patient confidence in their ability to engage in prevention behaviors. The WRC linked patients to local programs that were free to participants, typically provided child care, and were available in both English and Spanish. The WRC also provided incentives to participants for participation and completion of programs, and incentives to programs for tracking participation. The Healthy Here WRC team expected that removing barriers and creating more access and opportunities to engage in community-based chronic disease prevention and self-management programs, while simultaneously increasing social support and perceived social norms about healthy behaviors, would increase patients’ intention to engage in community-based programs across groups and, ultimately, improve health outcomes and reduce disparities.
Study Setting
Study participants were drawn from residents of six ZIP codes centered around three core urban neighborhoods in Bernalillo County, NM. Bernalillo County is the most populous county in New Mexico, home to 672,508 residents in 2022, which constitutes about 32% of the state’s total population [10]. The county has a median household income of $59,640, and 15.6% of residents live below the federal poverty line. More than half (50.9%) of county residents identify as Hispanic or Latinx and just over one-third (37.1%) as non-Hispanic White. However, the population in Bernalillo County is unevenly distributed by race and ethnicity and socio-economic class, leading to contrasts in poverty and wealth and access to resources, all of which affect health outcomes and contribute to inequities [11]. For example, crude diabetes prevalence rate estimates for 2021 among adults ranged from 1.3 to 18.1% across Bernalillo county ZIP codes, while corresponding hypertension estimates ranged from 8.8 to 40% [12]. In the ZIP codes included in this study, Hispanic/Latinx residents are a majority (66%), Mexican American residents are a plurality (45%), 15% of residents were born outside the United States, and 23% of residents are non-Hispanic White [10]. Although the three focal communities engaged in this study have unique characteristics, disparate histories of colonization and residential segregation, and varying population density, non-Hispanic White vs. Hispanic/Latinx resource gaps are present in each community with median non-Hispanic White household income, on average, 30% higher than that of Hispanic/Latinx households. The communities in these ZIP codes have long struggled with structural under-investment impacting walkability as well as access to healthy foods, despite some areas retaining links to their agricultural roots.
Previous Results
In earlier work [13], using an intent to treat approach, we examined comparative impacts of WRC referral alone on patient health outcomes of body mass index (BMI), HbA1c, and systolic and diastolic blood pressure. While findings regarding BMI were unremarkable, not meriting follow-up analysis, mixed results using data from 2018 to 2021 included unexpected findings regarding HbA1c and BP outcomes:
-
1.
HbA1c. Relative to non-referred counterparts, referred Hispanic/Latinx patients, showed consistently beneficial impacts as Hba1c levels changed over time. In absolute terms, referred Hispanic/Latinx patients showed significant pre-/post-reductions in HbA1c levels and referral was observed to significantly and substantially reduce disparities in HbA1c levels between Hispanic/Latinx and non-Hispanic White patients. Unexpectedly, these benefits of referral were not observed for non-Hispanic White patients and, indeed, pre-/post-increases in mean HbA1c levels occurred in this group of patients.
-
2.
Systolic blood pressure (BP). Contrary to prior research [14, 15], referral was not associated with relatively beneficial impacts on systolic BP. In absolute terms, significant and substantial pre-/post-increases in systolic BP values occurred among both Hispanic/Latinx and non-Hispanic White patients.
-
3.
Diastolic BP. Unexpectedly, but consistent with systolic BP, diastolic BP values increased pre/post for both Hispanic/Latinx and non-Hispanic White patients and statistically significantly increased in the sample overall. Relative to non-referred patients, referred non-Hispanic White patients saw, unexpectedly, consistent increases in diastolic BP values over time, while Hispanic/Latinx patients showed, in contrast and as expected, consistent benefits.
While our previous analyses did examine and adjust for systematic differences between referred and non-referred patients, they did not examine predictors of nor seek to quantify the impact of extent of participation in referred activities. We leverage updated data from 2018 to 2022 to do so here.
Methods
Detailed information on study and intervention design, participant eligibility, data collection, data de-identification, data handling, and core measures used are available in our prior publications [2, 13]. Briefly, primary care clinics referred adult residents of our focus communities who showed above-normal-range HbA1c, BP, or BMI values to the Healthy Here WRC. In turn, the WRC acted as a central hub to match referred patients to incentivized health promotion programs provided by community-based organizations. Electronic health record data, including data from non-referred comparators, from one primary referring health system were then matched with WRC referral data and de-identified for analysis by the referring health system. As this analysis focuses on participation in referred activities, it does not include non-referred comparators.
Measures
As in our prior work, we relied on systematic pharmacist review of prescribed medications to code for both adverse and beneficial impacts on BP and HbA1c. In this follow-up analysis, demographic determinations continued to be limited by electronic health record availability: gender was limited to two categories, race to seven mutually exclusive categories, and ethnicity to Hispanic vs. non-Hispanic, precluding detailed examination of within-group heterogeneity by ethnicity. Also, as in our previous work, pre-/post-outcome comparisons were made between the last available measure preceding or coinciding with initial referral and the first available measure at least 180 days after initial referral.
Community-based organizations were incentivized to track and report participation data to the WRC. Patient participation for each referred activity was designated by the WRC as “full,” “partial,” or some other designation indicating participation had not yet occurred. In order of frequency, non-participant designations included “dropped,” “referred,” “declined,” “registered,” “event cancelled,” and “wait list.” Although the WRC was actively working to connect patients in the “referred,” “registered,” “event canceled,” and “wait list” categories to programs, they were categorized as non-participants for the purposes of this analysis. Since patients could be referred to multiple activities over multiple time points, a patient was designated as a “full participant” if they had completed any program within 180 days of initial referral. A patient was designated as a “partial participant” if they participated in a community-based program within 180 days of initial referral but did not complete any program within 180 days of initial referral. A patient was categorized as a “non-participant” if they did not fully or partially participate in any referred activity within 180 days of initial referral.
In practice, patient participation completion rates varied widely by referral type with some types of activities having systematically more wait listing, cancellations, and patients dropping out than others. In order to include adjustments in analysis for such variability, we calculated two systemic participation rates reflecting a priori probabilities of full and partial patient participation, given aggregate referral-system-wide participation rates in referred patient activity types, for inclusion at the patient level in our analysis. Specifically, for patient i referred to j activities each with system-wide full participation probability pfk and non-participation probability pnk, patient-level full participation probability(i) = \(100*(1-\prod_{k=1}^{j}\left(1-{pf}_{k}\right))\) and partial participation probability(i) = \(100*(\prod_{k=1}^{j}\left(1-{pf}_{k}\right)-\prod_{k=1}^{j}\left({pn}_{k}\right))\). For example, for a patient referred to two activities, the first of which was a type of activity having a system-wide full completion rate of 4% and a system-wide non-completion rate of 88% and the second of which had a system-wide full completion rate of 9% and a system-wide non-completion rate of 80%, the patient’s full participation probability based on overall completion rates would be 100*(1 − 0.96*0.91) = 12.64% and the patient’s partial participation probability would be 100*(0.96*0.91 − 0.88*0.80) = 16.96%. Arithmetically, for other factors held constant, both full and partial systemic participation rates are guaranteed non-decreasing as the number of referred activities increases. Statistically, both full and partial systemic participation rates are patient-level measures incorporating aggregated rates of documented program participation by activity type.
Data Analysis
Data analysis was conducted within a research center not delivering the intervention or collecting related data. Per data use agreements, analytic results involving fewer than 20 participants are not reported publicly. Descriptive statistics consistent with measurement type of clinical and demographic characteristics were compared across patient-level participation categories using one-way ANOVAs for continuous measures and chi-square tests of independence for categorical variables. Effect sizes for analyses of observed differences across categories were chosen to admit common conventional effect size threshold interpretations of 0.1 “small,” 0.3 “medium,” and 0.5 “large.”
Notably, since participants could be initially referred from clinics outside of the core health system partner that shared clinical data for analysis, baseline clinical measures were not available for all referred participants meeting eligibility criteria. In order to incorporate systemic participation rates, then, into at least one model for participation probability available for all participants, two sequential multinomial logistic regression models of participation were calculated, one including only core demographic, study quarter, and systemic participation rates, and a further model adding baseline clinical- and medication-related measures. Consistent with classic recommendations from the literature [16, 17], inverse probability weights were calculated based on these two models to allow for weighted balance across participation groups on baseline characteristics, reducing confounding and enhancing accuracy of estimates of comparative impacts of participation on outcomes.
Effect sizes for the extent of observed weighted and unweighted pre-/post-differences were calculated using Cohen’s dz with the conventional effect size thresholds of 0.2 “small,” 0.5 “medium,” and 0.8 “large,” and weighted and unweighted linear regression models were fit to calculate main, simple, and interaction effects of participation and race and ethnicity on patient-level pre-/post-outcome differences. Consistent with our approach, statistical significance involving comparative impacts of participation was only considered using weighted models. Post hoc Wald tests were used for joint tests of significance of regression model coefficients, and, per convention, α = 0.05 was the threshold for statistical significance. Stata 17 was used for all statistical analyses [18].
Results
A total of 1331 patients met study inclusion criteria of residing in communities of interest, showing elevated clinical values in at least one focal indicator between January 2018 and September 2022, and having been referred to the WRC between January 2019 and September 2022. These patients were referred to a recorded total of 4636 activities with “Healthier Eating Education” (1440 instances) and “Physical Activity Opportunity” (1266 instances) being the most common referral types, together comprising a majority (58%) of referrals. At the activity level, completion rates within 180 days of initial referral were variable, with healthier eating education referrals being partially completed in 10% of cases (n = 144) and fully completed in 8% of cases (n = 108) and physical activity opportunity referrals being partially completed in 6% of cases (n = 76) and fully completed in 4% of cases (n = 50). Overall, 299 referred activities (6%) were recorded as partially completed and 199 referred activities (4%) were recorded as fully completed within 180 days of initial referral.
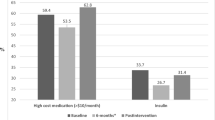
As shown in Table 1, at the patient level, about three-quarters of patients (1009/1331 = 76%) were non-participants with the remaining approximate quarter split roughly equally between partial participants (165/1331 = 12%) and full participants (157/1331 = 12%). Statistically significant predictors of participation shown in Tables 1 and 2 included age, systemic probability of full participation, and baseline HbA1c levels; younger patients, patients with higher baseline HbA1c, and patients having, a priori, lower systemic full participation probabilities had lower probabilities of full participation. Not shown in the table, participation rates also varied statistically significantly across the 15 study quarters from 2019 to 2022 (χ2(28) = 154.73, p < 0.001, V = 0.24), exceeding 40% in the second quarter of 2019 as well as the second and third quarters of 2020 and dropping below 5% by the fourth quarter of 2021. After weighting, differences across groups on all analyzed predictors of participation were statistically non-significant, and only non-Hispanic White and Hispanic/Latinx subgroups achieved subsample sizes exceeding 20 across all participation categories (Table 1).
Table 3 illustrates variability in pre-/post-changes in HbA1c and BP outcomes across participation and race and ethnicity categories. In this table, both weighted and unweighted estimates are presented, with weights used to statistically adjust for baseline differences across participation categories on predictors of documented program participation such as systemic participation probabilities. We unpack these results over the next two paragraphs, first focusing on HbA1c levels and then focusing on blood pressure outcomes, referencing corresponding statistics parenthetically in the text.
Pre-/post-changes in HbA1c levels varied statistically significantly across participation and race and ethnicity categories. Although HbA1c was not observed to change significantly in the overall sample in any participation category, aggregate means masked substantial heterogeneity in impacts of participation by race and ethnicity. Non-Hispanic White patients who did not participate in any referred activities saw statistically significant increases in HbA1c (M = 6.92, SD = 1.81 to M = 7.30, SD = 2.32, t(71) = 2.43, p = 0.02 (unweighted); M = 6.87, SD = 1.71 to M = 7.23, SD = 2.20, t(71) = 2.40, p = 0.02 (weighted)), while their Hispanic/Latinx non-participant counterparts saw statistically significant decreases in HbA1c (M = 7.40, SD = 2.33 to M = 7.10, SD = 2.07, t(379) = 3.34, p < 0.001 (unweighted); M = 7.27, SD = 2.19 to M = 7.03, SD = 1.97, t(379) = 3.11, p = 0.002 (weighted)). This observed difference in impact on HbA1c by race and ethnicity within documented non-participants was statistically significant in both unweighted (t(683) = 3.40, p < 0.001) and weighted analyses (t(683) = 3.55, p < 0.001), and, further, the interaction term between non-participation vs. partial participation and Hispanic/Latinx vs. non-Hispanic White race and ethnicity was also statistically significant in weighted analysis (t(683) = 2.18, p = 0.03). Essentially, levels of documented program participation were observed to impact Hispanic/Latinx patients and non-Hispanic White patients differently, with non-Hispanic White patients experiencing worsening HbA1c in the absence of program participation and Hispanic/Latinx patients having improved HbA1c overall, with no significant added benefit with documented program participation.
Heterogeneity in participation impacts was also noted for blood pressure outcomes. For systolic BP, non-participants saw significantly worsening pre-/post-values across and within race and ethnicity categories (e.g., overall sample: M = 127.84, SD = 16.28 to M = 130.41, SD = 17.09, t(966) = 4.66, p < 0.001 (unweighted)), and, again, a statistically significant contrast in the impact of non-participation vs. partial participation was observed by race and ethnicity (t(958) = 2.11, p = 0.04 for the interaction term) with a statistically significant difference between the impacts of non-participation v. partial participation only observed among non-Hispanic Whites (t(958) = 2.27, p = 0.03; Mdiff (SE) 4.87 (2.26) vs. − 4.84 (3.67)). For diastolic BP, non-Hispanic White partial participants saw, on average, statistically significant pre-/post-improvements in weighted analyses (M = 76.44, SD = 9.34 to M = 71.19, SD = 9.89, t(32) = 2.26, p = 0.03). Again, for diastolic BP, a statistically significant contrast in the impact of non-participation vs. partial participation was observed by race and ethnicity (t(958) = 2.96, p = 0.003 for the interaction term) with a statistically significant difference between the impacts of non-participation v. partial participation only observed among non-Hispanic Whites (t(958) = 2.74, p = 0.01; Mdiff (SE) 2.01 (1.31) vs. − 5.26 (2.33)). Further, within partial participants, non-Hispanic White patients saw significantly better impacts on diastolic BP than Hispanic/Latinx patients in both unweighted (t(958) = 2.23, p = 0.03; Mdiff (SE) − 3.12 (2.33) vs. 2.40 (1.33)) and weighted analyses (t(958) = 2.64, p = 0.01; Mdiff (SE) − 5.26 (2.33) vs. 2.03 (1.51)). As with HbA1c levels, levels of documented program participation were observed to impact Hispanic/Latinx and non-Hispanic White blood pressure outcomes differently; only non-Hispanic White patients showed any significant relative benefit from any documented program participation.
Discussion
These results further our understanding of the comparative impacts of patient engagement with a centralized community-clinical linkage program, highlighting the interacting roles of levels of participation and race and ethnicity in explaining mixed impacts of program referral. For non-Hispanic White patients, documented partial participation in referred program activities was observed to be a particularly salient predictor of benefit with statistically significant contrasts between non-participation and partial participation noted for blood pressure outcomes. Non-participants showed statistically significant increases in both HbA1c and systolic BP, whereas partial participants showed statistically significant decreases in diastolic BP. Documented participation, in contrast, was not observed to be an important predictor of changes in outcomes for Hispanic/Latinx patients. Indeed, for Hispanic/Latinx patients, statistically significant pre-/post-referral HbA1c impacts were noted even among non-participants.
While these results do expand discernment of conditional process pathways to community-clinical linkage intervention outcomes, the observed heterogeneity of participation impact by race and ethnicity was unanticipated. That WRC referral, even in the absence of documented participation, led to improved health outcomes for Hispanic/Latinx patients is consistent with theory regarding the importance of injunctive norms, often operationalized with Hispanic/Latinx populations by measuring perceived normative attitudes arising from family and friends [19, 20]. There is also some general, albeit somewhat dated, theory-based evidence that social norms are particularly important for prompting behavioral intention as a pathway to behavior change for patients at risk for diabetes [21] and less important for patients with hypertension [22]. However, such theory does not explain the worsening of outcomes in the absence of documented participation for non-Hispanic Whites referred to the WRC. This finding is particularly noteworthy in the face of robust and long-standing evidence [23, 24] that doctors are, overall, but with heterogenous nuance [25,26,27], more trusted as messengers of health information, and therefore more likely to enhance normative pressure, for non-Hispanic White patients than for Hispanic/Latinx patients.
However, more recent theory does provide some possible insights into the relative importance of intervention participation for non-Hispanic White patients. The behavior change wheel of the COM-B model for behavior change posits that the interlinked domains of capability, opportunity, and motivation shape behavior [28]. In COM-B, opportunity is contextual, situated outside the individual, and has both physical and social facets. It is consistent with COM-B that the WRC’s efforts to increase the physical facet of opportunity for healthy eating and physical activity led to positive impacts for non-Hispanic White patients. It is also possible that persistent gaps in the social facet of opportunity for Hispanic/Latinx patients, mirrored in abiding income inequality and reflective of structural racism and patterns of institutional exclusion, interacted to blunt the beneficial impacts of increasing opportunities for these individuals [11]. Although community health workers (CHWs) were partners in developing and implementing the centralized referral system, the increased opportunities provided by the system, despite efforts, may, in the end, have been less responsive to cultural and social needs among Latinx patients than those provided by alternate and more established models such as individualized referral systems that directly utilize CHWs or promotoras to connect patients with community-based programs [29]. We suggest future programs seeking to increase physical access to opportunities as a mechanism to improve health behavior engage in rapid cycle quality improvement strategies to monitor and address possible heterogenous impacts with marginalized groups, perhaps leveraging social conditions to level realized advantages.
Regarding contextual factors, our data analysis, while limited, does point to the importance of structural factors beyond the individual, such as systemic participation rates and exogenous time trends, in shaping, at the least, intervention participation probability. Although intervention participation probability was not observed to vary meaningfully between non-Hispanic White and Hispanic/Latinx patients, intervention participation probability did vary markedly over time, dropping to its lowest level in later 2021, post the occurrence of COVID-19 related challenges to both adequate staffing and focused prioritization of chronic conditions amidst acute distress we observed in previous work [2]. Moreover, while we observe that heterogeneity in impacts and levels of social challenges between groups may be one mechanism for explaining heterogeneity in our results, we lack direct measures of these impacts at the individual level for participants. Additionally, as always, race and ethnicity, the measures that were available to us, are poor and coarse markers of differential individual-level exposure to the impacts of structural racism [30].
Limitations and Future Research
As a planned evaluation of administrative data, this analysis has limitations. Over three-quarters of patients had not participated in any referred programs within 180 days of initial referral, limiting statistical power to detect differential impacts of full vs. partial participation and rendering infeasible efforts to further disaggregate our analysis of participant impacts (e.g., by referral type or program type or ZIP code). Relatedly, our limited measure of participation is not a direct measure of actual health behavior. Patients may have engaged in health-impacting behaviors beyond documented participation in referred programs. Indeed, results suggest that Hispanic/Latinx patients, in particular, may have engaged in positive health promoting behaviors, improving mean HbA1c, in lieu of documented formal program participation upon referral. While beyond the scope of this effort, greater understanding of health behaviors adopted upon program referral could be important for supporting generalizable and culturally inherent efforts to improve chronic disease outcomes, especially for diabetes, among Hispanic/Latinx patients.
Additionally, despite the WRC’s efforts to incentivize community-based programs to record and report participant attendance, there may also have been misclassification of participation due to inconsistent reporting. Further, detailed measures of systematically different clinical experiences and profiles of patients that may affect outcomes, such as cultural humility and competency of care providers [31], over- and under-treatment of chronic disease [32], and levels of insulin resistance, as a measure of diabetes history, were not available for this analysis. Our lack of measures on issues such as access to health information, possible COVID-related hesitancy to participate in in-person group activities, and patient-provider communication patterns at referral precluded adequate consideration of such issues as alternate explanations for observed results. Future research that includes a larger sample of program participants, investigates health behavior changes following referral but outside structured programming, incorporates measures of discrimination, and includes patient clinical profiles and experiences beyond chronic disease indicators and prescribed medications could further elucidate differential effects of referral to chronic disease prevention and self-management programs by race and ethnicity.
Conclusion
Participation in a centralized referral system that links patients with community-based chronic disease self-management and prevention programs has differential impacts on health outcomes for individuals with different racial and ethnic identities. Referred non-Hispanic White individuals experienced improved outcomes with documented participation in programming and worsened outcomes with no participation. In contrast, Hispanic/Latinx patients experienced significant improvement in HbA1c from referral, but did not experience any added benefit from participation. Results of this study support use of a centralized referral system and the promise of implementing culturally appropriate, evidence-based programming in community settings, while pointing to the need for more comprehensive measurement and evaluation to better understand heterogeneous impacts by race and ethnicity such as those observed in this study. Further, our theory-informed discussion of our mixed results contributes to an evidence base on the need for culturally responsive equitable interventions that extend beyond self-management foci, empowering patients while also directly linking to enhanced structural opportunities.
References
Centers for Disease Control and Prevention. Racial and ethnic approaches to community health. Centers for Disease Control and Prevention. Accessed August 10, 2023. https://www.cdc.gov/nccdphp/dnpao/state-local-programs/reach/index.htm.
Cruz TH, FitzGerald CA, Quintana V, et al. Healthy Here: a promising referral system model for community-clinical linkages to prevent chronic disease. Health Promot Pract. 2022;23(1):153S-163S. https://doi.org/10.1177/15248399221111192.
Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the Community Preventive Services Task Force. Ann Intern Med. 2015;163(6):437–51. https://doi.org/10.7326/M15-0452.
Community Preventive Services Task Force. Heart disease and stroke prevention: interventions engaging community health workers. Updated August 21, 2017. Accessed August 10, 2023. https://www.thecommunityguide.org/pages/tffrs-heart-disease-stroke-prevention-interventions-engaging-community-health-workers.html.
Lohr AM, Ingram M, Nunez AV, Reinschmidt KM, Carvajal SC. Community-clinical linkages with community health workers in the United States: a scoping review. Health Promot Pract. 2018;19(3):349–60. https://doi.org/10.1177/1524839918754868.
Centers for Disease Control and Prevention. Community-clinical linkages for the prevention and control of chronic diseases: a practitioner’s guide. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2016.
Community Preventive Services Task Force. Diabetes prevention: interventions engaging community health workers. Updated August 21, 2017. Accessed August 10, 2023. https://www.thecommunityguide.org/findings/diabetes-prevention-interventions-engaging-community-health-workers.html.
Ajzen I. The theory of planned behavior. Organ Behav Hum Dec. 1991;50(2):179–211. https://doi.org/10.1016/0749-5978(91)90020-T.
Montano DE, Kasprzyk D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior: Theory, research, and practice. 5th ed. San Francisco, CA: Jossey-Bass/Wiley; 2015. p. 95–124.
US Census Bureau. American community survey 5-year data (2017-2021). US Census Bureau. Accessed September 20, 2023. https://www.census.gov/data/developers/data-sets/acs-5year.html.
Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–63. https://doi.org/10.1016/S0140-6736(17)30569-X.
National Center for Chronic Disease Prevention and Health Promotion. PLACES: local data for better health. Centers for Disease Control and Prevention. Accessed September 20, 2023. https://www.cdc.gov/places.
Cruz TH, Boursaw B, Barqawi YK, et al. Community-clinical linkages: the effects of the Healthy Here Wellness Referral Center on chronic disease indicators among underserved populations in New Mexico. Health Promot Pract. 2022;23(1_suppl):164S-173S. https://doi.org/10.1177/15248399221111191.
Balcazar HG, de Heer H, Rosenthal L, et al. A promotores de salud intervention to reduce cardiovascular disease risk in a high-risk Hispanic border population, 2005–2008. Prev Chronic Dis. 2010;7(2):A28.
de Heer HD, Balcazar HG, Wise S, Redelfs AH, Rosenthal EL, Duarte MO. Improved cardiovascular risk among Hispanic border participants of the Mi Corazon Mi Comunidad promotores de salud model: the HEART II cohort intervention study 2009–2013. Front Public Health. 2015;3:149. https://doi.org/10.3389/fpubh.2015.00149.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–79. https://doi.org/10.1002/sim.6607.
Spreeuwenberg MD, Bartak A, Croon MA, et al. The multiple propensity score as control for bias in the comparison of more than two treatment arms: an introduction from a case study in mental health. Med Care. 2010;48(2):166–74. https://doi.org/10.1097/MLR.0b013e3181c1328f.
StataCorp. Stata Statistical Software, Release 17. College Station, TX: StataCorp LLC; 2021.
Abraído-Lanza AF, Shelton RC, Martins MC, Crookes DM. Social norms, acculturation, and physical activity among Latina women. J Immigr Minor Health. 2017;19:285–93.
Kam JA, Mendez Murillo R, Cornejo M, Mendoza N. The importance of norms and efficacy in predicting undocumented college students’ intentions to talk to an on-campus mental health professional. Health Commun. 2022;37(2):230–41.
Blue CL. Does the theory of planned behavior identify diabetes-related cognitions for intention to be physically active and eat a healthy diet? Public Health Nurs. 2007;24(2):141–50. https://doi.org/10.1111/j.1525-1446.2007.00618.x.
Pourmand G, Doshmangir L, Ahmadi A, et al. An application of the theory of planned behavior to self-care in patients with hypertension. BMC Public Health. 2020;20(1):1290. https://doi.org/10.1186/s12889-020-09385-y.
Fareed N, Swoboda CM, Jonnalagadda P, Walker DM, Huerta TR. Differences between races in health information seeking and trust over time: evidence from a cross-sectional, pooled analyses of HINTS data. Am J Health Promot. 2021;35(1):84–92. https://doi.org/10.1177/0890117120934609.
Wheldon CW, Carroll KT, Moser RP. Trust in health information sources among underserved and vulnerable populations in the US. J Health Care Poor Underserved. 2020;31(3):1471–87.
Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97(7):1283–9.
Escobedo LE, Cervantes L, Havranek E. Barriers in healthcare for Latinx patients with limited English proficiency—a narrative review. J Gen Intern Med. 2023;38(5):1264–71.
Smith GH, Hampton C, Tripp HL, Brandon WP. Acculturation, Hispanic ethnicity, and trust: verifying and explaining racial/ethnic differences in trust in health providers in North Carolina Medicaid. Politics Life Sci. 2023;42(1):120–45.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. https://doi.org/10.1186/1748-5908-6-42.
Kubicek K, Robles M, Baezconde-Garbanati L, Cordero-Barazaga M, Kipke MD. Promotoras (community health workers) improve heart health among Latinos in rural and urban settings. Implement Sci. 2015;10(1):A55. https://doi.org/10.1186/1748-5908-10-S1-A55.
Chae DH, Snipes SA, Chung KW, Martz CD, LaVeist TA. Vulnerability and resilience: use and misuse of these terms in the public health discourse. Am J Public Health. 2021;111(10):1736–40. https://doi.org/10.2105/ajph.2021.306413.
Dragomanovich HM, Shubrook JH. Improving cultural humility and competency in diabetes care for primary care providers. Clin Diabetes. 2021;39(2):220–4. https://doi.org/10.2337/cd20-0063.
McCoy RG, Lipska KJ, Van Houten HK, Shah ND. Development and evaluation of a patient-centered quality indicator for the appropriateness of type 2 diabetes management. BMJ Open Diabetes Res Care. 2020;8(2):e001878. https://doi.org/10.1136/bmjdrc-2020-001878.
Acknowledgements
We would like to thank the Healthy Here partners, especially Adelante Development Center, for their steadfast efforts to implement this health equity work. We also appreciate the leadership of Presbyterian Healthcare Services Community Health in implementing this project.
Funding
This publication was supported by Presbyterian Healthcare Services through a Cooperative Agreement Number U58 DP005868, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Author information
Authors and Affiliations
Contributions
CF, LC, and TC contributed to study conception and design. Data analysis was performed by BB and validated by ELC. CF, LT, and TC contributed to theoretical grounding and data interpretation. All authors contributed to manuscript preparation, revision, and final approval.
Corresponding author
Ethics declarations
Ethics Approval
The University of New Mexico Human Research Protections Office approved this study as exempt due to the exclusive use of de-identified administrative data (approval 16–146).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Boursaw, B., FitzGerald, C.A., Taylor, L.M. et al. Improving Health and Reducing Chronic Disease Disparities with Latinx Communities: Evaluating the Role of Documented Community-Based Intervention Participation. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-02078-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-02078-x