Abstract
Background
Obstetric care in the US is complicated by marked racial and ethnic disparities in maternal obstetric outcomes, including severe morbidity and mortality, which are not explained by underlying differences in patient characteristics. Understanding differences in care delivery related to clinical acuity across different racial groups may help elucidate the source of these disparities.
Objective
This study examined the association of maternal race with utilization of critical care interventions.
Study Design
This is a retrospective cohort study conducted as a secondary analysis of a large, multicenter observational study of women undergoing cesarean delivery. All women with a known delivery date were included. The primary outcome measure, a composite of critical care interventions (CCI) at delivery or postpartum that included mechanical ventilation, central and arterial line placement, and intensive care unit (ICU) admission were compared by racial/ethnic group—non-Hispanic white, non-Hispanic black, Hispanic, Asian, and Native American. We evaluated differences in utilization of critical care with a multivariable regression model accounting for selected characteristics present at admission for delivery, including maternal age, BMI, co-morbidities, parity, and plurality. Maternal mortality was also evaluated as a secondary outcome and the frequency of CCI by significant maternal co-morbidity, specifically heart disease, renal disease, and chronic hypertension was assessed to ascertain the level of care provided to women of different race/ethnicity with specific baseline co-morbidities.
Results
73,096 of 73,257 women in the parent trial met inclusion criteria, of whom 505 (0.7%) received a CCI and 3337 (4.6%) had a significant medical co-morbidity (1.2% heart disease, 0.8% renal disease, 2.5% chronic hypertension). The mortality rate was significantly higher among non-Hispanic black women, compared to non-Hispanic white and Hispanic women. In the adjusted model, there was no significant association between CCI and race/ethnicity.
Conclusion
This study suggests that differences in maternal morbidity by race may be accounted for by differential escalation to higher intensity care. Further investigation into processes for care intensification may continue to clarify sources of racial and ethnic disparities in maternal morbidity and potential for improvement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Severe maternal morbidity during pregnancy and postpartum affects approximately 50,000 women per year, a number which appears to be increasing despite the otherwise rapid advancement of medical technology [1]. The growing prevalence of maternal morbidity is likely multifactorial, related to the rising tide of maternal cardiometabolic disease, trends in maternal age and cesarean delivery, and assisted reproductive technologies [2, 3]. The utilization of critical care, including intensive care unit (ICU) admission, is becoming an increasingly important resource to care for patients who encounter severe morbidity during pregnancy.
Situated within the broader problem of maternal morbidity and mortality, there is a specific and very concerning phenomenon of racial and ethnic disparities in obstetrics, with non-Hispanic black and Hispanic women experiencing significantly more adverse outcomes [4, 5]. There is a growing body of research on the topic of racial disparities in obstetrics, which has identified this trend and elucidated race and ethnicity as independent predictors of adverse obstetric outcomes. Most of this literature focuses on population-level patterns as well as relationship to other sociodemographic determinants of health and specific clinical contexts in which these disparities are pronounced [6,7,8,9]. Prior research has also examined structural elements of racial and ethnic obstetric disparities, including types of hospitals and other hospital-level factors [10].
In an effort to target maternal outcome disparities, further investigation into racial and ethnic variations in the type of care interventions that obstetric patients receive is necessary. The purpose of this study, therefore, is to identify the association of maternal race and ethnicity with utilization of critical care interventions during delivery hospitalizations.
Materials and Methods
This is a retrospective cohort study designed as a secondary analysis of the Cesarean Registry, a 4-year observational cohort study of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units. Demographic information and medical histories of the patients as well as features of the current pregnancy were obtained from the medical record by trained research staff. Full details of the parent study have previously been reported [11,12,13],
The current analysis included all women in the parent registry with a documented delivery date; there were no other exclusion criteria. The exposure of interest was maternal race and ethnicity, defined in this study as non-Hispanic white, non-Hispanic black, Hispanic, Asian, Native American, and unknown. The analysis focuses on non-Hispanic white, non-Hispanic black, and Hispanic women as the other sub-groups were comparatively small. The primary outcome was defined as a composite of critical care interventions (CCI) including postpartum intensive care unit (ICU) admission, mechanical ventilation, central intravenous access, and arterial line placement. A patient with at least one of the components was considered to have the composite outcome. Maternal mortality was evaluated as a secondary outcome.
Baseline characteristics present at admission for delivery were compared between racial groups using Student t test, Mann–Whitney U test, and chi-square tests, as appropriate. A multivariable logistic regression model was employed to calculate the odds of CCI by racial/ethnic group after accounting for potentially confounding factors. Variables that were statistically significant in univariable analyses or otherwise suspected to be associated with the outcome were included in the regression model. Adjusted odds ratios (aORs) with 95% confidence intervals from the regression model are reported as measures of effect. This model ultimately accounted for maternal age, BMI, marital status, education, nulliparity, plurality, toxic exposures during pregnancy (tobacco, alcohol, illicit drug use), maternal co-morbidities—specifically hypertension, heart disease, renal disease, diabetes, thyroid disease, seizure disorders, asthma, and connective tissue disease—anemia, thrombocytopenia, hypertensive disorders of pregnancy (gestational hypertension, pre-eclampsia, pre-eclampsia with severe features, eclampsia, HELLP), and attempted vaginal delivery. As defined by the parent study, maternal heart disease included valvular heart disease, rheumatic heart disease, congenital heart disease, cardiomyopathy, myocardial infarction, angina, thyroid related heart disease, syphilitic related heart disease, kyphoscoliotic related heart disease, cor pulmonale, pericarditis, myocarditis, heart block, arrhythmias and super ventricular tachycardia; renal disease included non-infectious kidney disease, known glomerular kidney disease; and connective tissue disease included lupus, rheumatoid arthritis, scleroderma, Sjogren’s disease, or a mixed connective tissue disorder. A significant baseline co-morbidity in this study was defined as having heart disease, renal disease, or chronic hypertension.
All statistical tests were two-tailed and p < 0.05 was considered significant. The sample size was fixed from the original registry study. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC). This analysis was considered exempt by the Institutional Review Board at Columbia University Medical Center as these data are de-identified and publicly available.
Results
Of 73,257 women in the parent registry, 73,096 met inclusion criteria and were incorporated in the analysis. One hundred and sixty-one women were excluded due to lack of recorded delivery date (Fig. 1). There were 505 (0.7%) women in the study population who underwent a CCI, as defined above, and 3337 women (4.6%) had a significant medical co-morbidity (1.2% heart disease, 0.8% renal disease, 2.5% chronic hypertension). The population was comprised of 29,430 non-Hispanic white women (40.3%), 21,329 non-Hispanic black women (29.2%), 18,689 Hispanic women (25.6%), 1240 Asian women (1.7%), 140 Native American women (0.2%), and 2268 women with reported unknown race (3.1%). Significant differences in demographics and underlying co-morbidities were present by racial/ethnic group (Table 1).
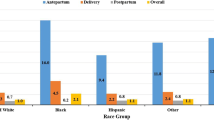
Non-Hispanic white and non-Hispanic black women received significantly more central lines than Hispanic women (0.2% for both vs. 0.07%, p = 0.01) and non-Hispanic black women had significantly more ICU admissions than non-Hispanic white and Hispanic women (0.9% vs. 0.7 and 0.5%, p < 0.01). There was a significantly higher mortality rate for non-Hispanic black women (0.08%) compared to non-Hispanic white (0.04%) and Hispanic (0.02%) women (p < 0.01). In an assessment of the frequency of critical care interventions by racial/ethnic group stratified into categories of significant maternal-co-morbidity (heart disease, renal disease, hypertension), non-Hispanic white women with heart disease were significantly more likely to undergo a CCI than non-Hispanic black and Hispanic women (0.1% vs. 0.08 and 0.05%, p = 0.02).
On unadjusted analysis, CCI was found to be significantly associated with black race (OR 1.27, 95% confidence interval [CI] 1.04–1.56, p = 0.02) (Table 2). However, on adjusted analysis with a multivariable logistic regression model to account for confounders, maternal CCI was not found to be significantly higher for non-Hispanic black (aOR 1.15, 95% CI 0.79–1.67, p = 0.46) or Hispanic women (aOR 0.78, 95% CI 0.50–1.24, p = 0.30) compared to non-Hispanic white women.
Discussion
In this cohort of obstetric patients, there was no difference in the frequency of critical care interventions by race and ethnicity after adjusting for baseline differences including co-morbidities. While non-Hispanic black women did have a higher incidence of CCI in unadjusted analysis, this did not persist after adjustment for potentially confounding variables. Similarly, the only significant difference in CCI frequency by co-morbidity sub-group existed for heart disease and favored increased CCI for non-Hispanic white patients compared to non-Hispanic black and Hispanic women. Mortality in this cohort, however, was significantly higher for non-Hispanic black women compared to non-Hispanic white and Hispanic women. These findings suggest that a possible root cause of the known outcome disparity among women with different racial backgrounds may relate to appropriate care escalation for specific groups of women, which ultimately can precipitate divergent outcomes.
Significant prior research has demonstrated that black race and Hispanic ethnicity are independently associated with severe maternal morbidity [4]. Given this knowledge, it would seem that the level of care afforded to black and Hispanic patients should be higher, to account for this increased morbidity and to combat it. However, this study, which utilizes a composite critical care intervention outcome variable, demonstrates no difference in higher level of care interventions across racial and ethnic groups after accounting for potential confounders. It is possible, therefore, that failure to escalate care in an appropriate or timely fashion could be a previously unidentified factor in the phenomenon of racial disparities in obstetrics. Implicit bias may be a mechanism in this problem [14, 15], and this research suggests that a lower intensity of care could be implicated in the manifestation of this bias. Innovative solutions are necessary to pave the way forward for better care for all women, such as implicit bias training and simulation for clinical staff, and electronic medical record-generated trigger tools to detect acuity that are inherently “race-blind.”
The findings of this study invite further investigation into the role of level of care in obstetric racial disparities. In the context of the general epidemic of maternal morbidity and mortality, there has been significant research and policy headway concentrated on understanding and improving maternal level of care and risk-appropriate care in pregnancy [16, 17]. This has been coupled with research dedicated to understanding critical illness in pregnancy and patterns of intensive care utilization by obstetric patients [18,19,20]. However, it is unknown whether there is practice trend toward inadequate critical care utilization for black and Hispanic women. This is an essential future direction for research in an attempt to reduce the burden of obstetric racial disparities and should involve further study of intensive care admission and other proxy measures of care escalation to assess for disproportionality between morbidity burden and hospital care utilization.
The strengths of this study include the richness of the parent study, which possesses granular clinical data that allows for the assessment of a composite critical care outcome based on research-quality, as opposed to administrative, data. However, the study is limited by the extent of the variables available for analysis in the original, its inclusion of primarily major academic medical centers, and the data collection time frame from 1999 to 2002, all of which may render the results less generalizable and less relevant to contemporary clinical practice. It is also limited by its inclusion only of patients who underwent cesarean delivery which may impact generalizability and introduce bias into the results. Prior research has already demonstrated differences in cesarean section rates by race [21]. Finally, the study is limited by the assumption that all components in the critical care composite represent true care escalations, which may vary based on individual hospital standards of practice.
Racial disparities in obstetric outcomes remain a pervasive problem in obstetrics and every effort must be taken to understand and address them. This study sheds light on the role that escalation of care may play in yielding these disparate outcomes. Given that there is a known morbidity and mortality differential across racial and ethnic groups, the parity observed in critical care interventions in this study suggests a possible failure to intervene on behalf of patients from minority backgrounds. This is ultimately a concern that must be targeted as part of our efforts to reduce maternal morbidity and mortality and racial disparities.
References
Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120(5):1029–36.
Berg CJMA, Qin C, et al. Overview of maternal morbidity during hospitalizations for labor and delivery in the United States 1993 – 1997 and 2001 – 2005. Obstetr Gynecol. 2009;113(5):1075–81.
Martin AS, Monsour M, Kissin DM, Jamieson DJ, Callaghan WM, Boulet SL. Trends in severe maternal morbidity after assisted reproductive technology in the United States, 2008-2012. Obstet Gynecol. 2016;127(1):59–66.
Creanga AA, Bateman BT, Kuklina EV, Callaghan WM. Racial and ethnic disparities in severe maternal morbidity: a multistate analysis, 2008-2010. Am J Obstet Gynecol. 2014;210(5):435 e431–8.
Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW, et al. Racial and ethnic disparities in maternal morbidity and obstetric care. Obstet Gynecol. 2015;125(6):1460–7.
Admon LK, Winkelman TNA, Zivin K, Terplan M, Mhyre JM, Dalton VK. Racial and ethnic disparities in the incidence of severe maternal morbidity in the United States, 2012-2015. Obstet Gynecol. 2018;132(5):1158–66.
Booker WA, Gyamfi-Bannerman C, Sheen JJ, Wright JD, Siddiq Z, D’Alton ME, et al. Maternal outcomes by race for women aged 40 years or older. Obstet Gynecol. 2018;132(2):404–13.
Gyamfi-Bannerman C, Srinivas SK, Wright JD, et al. Postpartum hemorrhage outcomes and race. Am J Obstet Gynecol. 2018;219(2):185 e181–10.
Shahul S, Tung A, Minhaj M, Nizamuddin J, Wenger J, Mahmood E, et al. Racial disparities in comorbidities, complications, and maternal and fetal outcomes in women with preeclampsia/eclampsia. Hypertens Pregnancy. 2015;34(4):506–15.
Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215(2):143–52.
Alexander JM, Leveno KJ, Rouse DJ, Landon MB, Gilbert S, Spong CY, et al. Comparison of maternal and infant outcomes from primary cesarean delivery during the second compared with first stage of labor. Obstet Gynecol. 2007;109(4):917–21.
Bailit JL, Landon MB, Lai Y, et al. Maternal-Fetal Medicine Units Network cesarean registry: impact of shift change on cesarean complications. Am J Obstet Gynecol. 2008;198(2):173 e171–5.
Landon MB, Leindecker S, Spong CY, Hauth JC, Bloom S, Varner MW, et al. The MFMU Cesarean Registry: factors affecting the success of trial of labor after previous cesarean delivery. Am J Obstet Gynecol. 2005;193(3 Pt 2):1016–23.
Howell EA, Brown H, Brumley J, Bryant AS, Caughey AB, Cornell AM, et al. Reduction of peripartum racial and ethnic disparities: a conceptual framework and maternal safety consensus bundle. J Obstet Gynecol Neonatal Nurs. 2018;47(3):275–89.
Jain JA, Temming LA, D'Alton ME, et al. SMFM Special Report: putting the "M" back in MFM: reducing racial and ethnic disparities in maternal morbidity and mortality: a call to action. Am J Obstet Gynecol. 2018;218(2):B9–B17.
Vladutiu CJ, Minnaert JJ, Sosa S, Menard MK. Levels of maternal care in the United States: an assessment of publicly available state guidelines. J Womens Health (Larchmt). 2019.
Levels of maternal care: obstetric care consensus no, 9. Obstet Gynecol. 2019;134(2):e41–e55.
Rossi RM, Hall E, Dufendach K, DeFranco EA. Predictive model of factors associated with maternal intensive care unit admission. Obstet Gynecol. 2019;134(2):216–24.
Wanderer JPLL, Mhyre JM, et al. Epidemiology of obstetric-related intensive care unit admissions in Maryland: 1999 – 2008. Crit Care Med. 2013;41(8):1844–52.
Easter SR, Bateman BT, Sweeney VH, et al. A comorbidity-based screening tool to predict severe maternal morbidity at the time of delivery. Am J Obstet Gynecol. 2019;221(3):271 e271–10.
Min CJ, Ehrenthal DB, Strobino DM. Investigating racial differences in risk factors for primary cesarean delivery. Am J Obstet Gynecol. 2015;212(6):814 e811–4.
Availability of Data and Material
Not applicable
Code Availability
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kern-Goldberger, A.R., Friedman, A., Moroz, L. et al. Racial Disparities in Maternal Critical Care: Are There Racial Differences in Level of Care?. J. Racial and Ethnic Health Disparities 9, 679–683 (2022). https://doi.org/10.1007/s40615-021-01000-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-021-01000-z