Abstract
Purpose of Review
Severe asthma can be difficult to manage. While not always indicated, bronchoscopy has a role in the diagnosis and management of asthma, particularly in ruling out other differential diagnoses. Additionally, the emergence of biologic therapies has changed the landscape for treating severe asthma, but bronchoscopic techniques such as bronchial thermoplasty (BT) may also play a role.
Recent Findings
More data has emerged regarding the longevity and efficacy of BT as well as in identifying ideal candidates. Other bronchoscopic techniques may also be useful in treating patients with severe asthma but more studies are needed.
Summary
This review focuses on the use of bronchoscopy to aid in diagnosis and treatment of asthma with a focus on bronchial thermoplasty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma affects more than 25 million Americans, representing almost 8% of our population [1]. It is typically characterized by chronic airway inflammation and expiratory airflow limitation, producing a constellation of symptoms including shortness of breath, cough, chest tightness, and wheezing.
The diagnosis of asthma can be challenging. It is imperative that other comorbid conditions and differential diagnoses are considered for an accurate diagnosis which in turn guides appropriate therapy. The mainstays of treatment focus on reducing airway inflammation and bronchospasm, often achieved with bronchodilators and inhaled corticosteroids. Asthma is variable in severity, with 17% considered difficult to treat and 3.7% classified as severe [2•]. More recently, the discovery and identification of different asthma phenotypes, mainly the distinction between type 2 airway inflammation and type 1, have shifted therapy for severe disease towards targeted biologic therapy [3].
Non-pharmacological asthma treatments are limited, although bronchial thermoplasty (BT) can be utilized as add-on therapy for those with refractory, severe asthma of either phenotype [2•, 4••]. BT uses radiofrequency energy targeted at reducing airway smooth muscle (ASM). Additionally, emerging data has shown that bronchoscopic targeted bronchial denervation can be used for treatment of chronic obstructive lung disease (COPD) [5] with thoughts that this may also be translated as a therapeutic option in the management of asthma. We review bronchoscopic techniques to aid in the diagnosis and treatment of asthma, especially in those with more refractory disease.
Diagnostic Utility of Bronchoscopy
The diagnosis of asthma requires a history of variable respiratory symptoms as well as documented expiratory airflow limitation and variability in lung function [2•]. Still, there are many other diagnoses that can be mistaken for asthma, especially for those with chronic cough. Bronchoscopy is not recommended as a routine part of the work up of asthma or cough. However, bronchoscopy can be useful in evaluating alternative diagnoses for select cases.
Flexible bronchoscopy can be particularly useful in identifying structural abnormalities of the airways. With the ability to evaluate the tracheobronchial tree, it can be used to rule out tracheobronchomalacia, tracheal and/or bronchial stenosis, endobronchial lesions, and airway foreign bodies, all of which can cause symptoms which mimic asthma such as wheezing, cough, and excess mucus. Flexible laryngoscopy may also be performed at the same time to evaluate the vocal cords and upper airway.
In combination with a bronchoalveolar lavage (BAL), other co-morbidities can be investigated such as GERD, infection, and chronic aspiration. A study in 2014 showed that lipid laden macrophages (LLM) were higher in severe asthmatics compared to those with mild or moderate asthma. Additionally, a higher LLM count was associated with higher incidence of GERD. While this correlation is not specific and LLM can be seen in many other respiratory conditions, it highlights the importance of ruling out other comorbid conditions, particularly in those with refractory disease [6].
Bronchoscopy and BAL has also been historically used to further classify those with a diagnosis of asthma. One study utilized bronchoscopy and BAL to distinguish different patterns in patients with severe or refractory asthma. The authors proposed five phenotypes based on BAL findings: GERD, subacute bacterial infection, those with tissue/BAL eosinophilia, combination, and non-specific. These groups were then given more targeted therapy based on their classification, and all groups except for the nonspecific phenotype demonstrated improved lung function and asthma control [7].
The advent of distinguishing type 1 from type 2 airway inflammation in those with severe asthma has transformed the diagnostic and treatment algorithm, and data obtained from bronchoscopy and/or BAL is not necessary in making this distinction. Serum eosinophil counts and IgE levels, as well as sputum eosinophil counts (not BAL), can be utilized to guide targeted therapy [2•, 3]. In those with uncontrolled, severe disease, consideration is made for add-on targeted biologic therapy earlier in the treatment algorithm for patients with type 2 inflammation, whereas the mainstay of treating those with type 1 inflammation focuses on ruling out alternative diagnoses and optimizing current management before considering biologics. Thus, bronchoscopy is not routinely recommended for all asthma patients, although those with type 1 inflammation or type 2 inflammation but refractory to biologics may benefit from earlier diagnostic testing with bronchoscopy to evaluate for alternative or co-morbid diagnoses.
Bronchial Thermoplasty
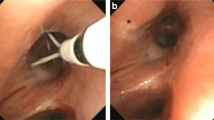
Increased ASM is thought to contribute to airway hyperreactivity and bronchoconstriction in asthma. BT is currently the only approved treatment focused on targeting ASM mass and is performed using the Alair™ Bronchial Thermoplasty System (Boston Scientific, Marlborough, MA). The flexible treatment catheter is introduced via flexible bronchoscopy and delivers temperature-controlled radiofrequency energy to the airway wall. BT has been shown to decrease ASM without changing airway structure or vasculature [8, 9]. It is typically performed under moderate sedation or general anesthesia and delivered over a series of three bronchoscopies. The sessions are typically 3 weeks apart target with each session targeting specific lobes of the lung in a sequential fashion: right lower lobe, left lower lobe, and finally bilateral upper lobes [10].
Three randomized controlled trials have investigated the efficacy and safety of bronchial thermoplasty. The Asthma Intervention Research (AIR) trial published in 2007 investigated 112 patients with moderate to severe asthma treated with combination inhaler therapy including a long-acting beta agonist (LABA) and inhaled corticosteroid (ICS) with a pre-bronchodilator FEV1 between 60 and 85% who were randomized to either BT or usual care. There was no sham bronchoscopy in the control arm raising the possibility of a significant placebo effect. There was an increase in early adverse events in the post-procedure period mostly due to a transient increase in asthma symptoms. However, the study ultimately demonstrated a significant improvement at 12 months in the rate of mild exacerbations between the treatment and control groups as well as improved Asthma Control Questionnaire (ACQ) and Asthma Quality of Life Questionnaire (AQLQ) [10].
The Research in Severe Asthma Trial (RISA) was also published in 2007, investigated 34 patients with severe persistent asthma randomized to either BT and medical management or medical management alone. This trial included patients also on combination LABA and ICS, but included those on up to 30 mg of oral corticosteroids (OCS) as well as those with an FEV1 greater or equal to 50% with an average of 62.9 and 66.4 in the BT and control groups, respectively. A transient increase in asthma-related symptoms were again seen in the initial treatment period, but the study demonstrated BT can be performed safely in patients with severe asthma with a lower baseline FEV1. Additionally, a sustained improvement in rescue bronchodilator use and ACQ scores were observed at 1 year. However, there was again no sham bronchoscopy performed in the control arm [11].
The Asthma Intervention Research 2 (AIR2) trial was published in 2010 and was the first randomized, double-blind study to evaluate the efficacy and safety of BT to include sham bronchoscopy to address concerns of a potential placebo effect. The study randomized 288 patients with a prebronchodilator FEV1 greater or equal to 60% who were stable on LABA and ICS therapy. OCS and other medications, including omalizumab, were also allowed. Sham bronchoscopies were performed at the same 3-week intervals as in the treatment arm with BT under the same conscious sedation for bronchoscopy. The Alair catheter was deployed, and a sham RF controller was utilized, which produced similar audio and visual signals when activated, indistinguishable from the active RF controllers. The primary outcome was the difference in AQLQ scores from baseline between the two groups at varying time points [12].
Both the BT and sham groups experienced an increase in respiratory adverse events during the early post-treatment period, with more events occurring in the BT group. The most common were worsening asthma symptoms and upper respiratory tract infections; 8.4% in the BT group were hospitalized during the treatment period compared with 2.0% in the sham group. However, rates of exacerbations, adverse events, hospitalizations, and ED visits were lower in the BT group at the 12-month follow-up which despite the transient higher rate in the early post-treatment period [12].
The observed increase in exacerbations during the treatment period is thought to be related to bronchoscopy and anesthesia as it was also observed in the sham bronchoscopy group [12]. This transient increased risk may be mitigated by administering a short course of OCS in the peri-procedural period. Long-term safety data was reported in a 5-year follow-up study on the AIR2 cohort which showed a lack of serious adverse events or significant structural changes on high-resolution CT (HRCT), as well as stability in FEV1 and/or FVC. Also notable was the rate of severe exacerbations and ED visits continued to be decreased after BT, suggesting a sustained benefit lasting at least 5 years [13].
In 2017, a phase 5 Post-FDA Approval Clinical Trial Evaluating Bronchial Thermoplasty in Severe Persistent Asthma (PAS2) trial was reported. PAS2 was a multicenter, open-label, single-arm study conducted to evaluate the short- and long-term efficacy and safety of bronchial thermoplasty in patients with severe, persistent asthma. The study enrolled patients with similar pre-bronchodilator FEV1 when compared to the AIR2 study. However, in contrast to AIR2, the PAS2 cohort had higher use of ICS, short acting beta agonist (SABA) puffs per day, and OCS. Importantly, exclusion criteria were less stringent and permitted comorbidities such as insulin-dependent diabetes, obstructive sleep apnea, interstitial lung disease, GERD, chronic sinus disease, and known coagulopathy, reflecting a more “real-world” cohort with more severe disease [14].
As with prior studies [10,11,12], an increase in asthma-related symptoms was observed during the early post-treatment period, although this was slightly increased when compared directly to the AIR2 study, possibly due to a cohort of patients with more severe disease. However, the number of exacerbations was decreased after the initial treatment period and was sustained at 3-year follow-up. A decrease in ED visits was observed, as was a trend toward reduction in hospitalizations at 3 years post-BT [14]. In 2022, a follow-up report of the PAS2 cohort was published after an extended follow-up period of 5 years and reported these benefits were sustained with an improvement in asthma control indicated by decreased exacerbation rates, hospitalizations, ED visits, and OCS use [15].
Furthermore, the international, multicenter BT10 + study published in 2021 was designed to address long-term safety concerns as well as the longevity of the observed treatment effect. Participants from the AIR, RISA, and AIR2 trials were enrolled and followed up over an extended period with a median of 12.1 years. Effectiveness was determined by comparing the proportion of participants with severe exacerbations during the first, fifth, and final years post-BT at the final BT10 + study visit which ranged from 10.8 to up to 15.6 years post-BT. The study found that the rate of exacerbations at the final BT10 + visit and the 12 months leading up to it were similar to rates at 1 year and 5 years post-BT, reflecting a durable benefit lasting at least 10 years [16•].
The long-term safety of bronchial thermoplasty in the BT10 + study included imaging looking for changes such as bronchiectasis or bronchial stenosis on high-resolution CT at the final BT10 + visit in AIR2 participants. Six patients (7%) were noted to have bronchiectasis after BT at the BT10 + time point, compared to 0% in the sham group. The bronchiectasis was noted to be mild and without an increase in symptoms. The authors proposed that along with a low number of sham patients enrolled, the bronchiectasis may reflect the natural history of asthma, as well as a possible improvement in HRCT over the previous decade. Moreover, they proposed the mild bronchiectasis may reflect airway dilation after BT, associated with reduced airway resistance and improved asthma symptoms [16•].
An additional criticism of these studies is the observed benefit in the control or sham groups compared to baseline. While decreased rates of mild and severe exacerbations, improved AQLQ were less than the improvement seen with BT. This effect may be explained by improved compliance and regular follow-up in a study setting. A small number of control or sham participants were enrolled, and additionally, 32% of those who did not initially receive BT, underwent BT after their original study and before the BT10 + visit [16•].
The Unraveling Targets of Therapy in Bronchial Thermoplasty in Severe Asthma (TASMA) trial published in 2019 investigated the effect of BT on ASM mass and also aimed to identify patient characteristics associated with BT response. The study demonstrated that the significant decrease in ASM after BT was sustained after a 6-month period after treatment. Interestingly, however, the study also found a positive correlation with BT response and baseline blood eosinophil counts and total IgE [17]. Another study in 2021 showed that younger patients with severe asthma may have a more robust response to BT, as well as those with higher peripheral eosinophil and IgE levels. These responders also had sustained lower eosinophil and IgE levels despite lower OCS use, suggesting that patients with type 2 inflammation may be stronger responders to BT than those with type 1 inflammation [18]. Determining which patients benefit the most from BT is anticipated to evolve as additional data emerge further refining patient selection criteria, particularly in patients on targeted biologics.
Those with poor baseline reserve and severe airflow limitation have previously been excluded from randomized controlled trials as there a short-term decrease in FEV1 immediately following BT [19]. However, given that BT targets ASM mass which is implicated in more severe bronchoconstriction [10], trials to date may have theoretically excluded those who could benefit the most. One study in 2020 looked at those with FEV1 < 50% and showed that there was no difference in the frequency of severe adverse events — defined as remaining in the hospital longer than the planned 24-h admission or being readmitted within 30 days of treatment. The study compared two groups, one with FEV1 < 50% and ≥ 50%, and showed that benefit, measured by SABA use, OCS use, and rate of exacerbations, were similar [20]. Nevertheless, special consideration should be given to patients who are unlikely to tolerate the sedation required for the 3 bronchoscopy sessions required for bronchial thermoplasty.(Tables 1 and 2).
Lastly, several studies have estimated the cost-effectiveness of BT. Among private and commercially insured patients with poorly controlled, severe persistent asthma, one study reported that BT was cost-effective when compared to medical management alone. This was measured as an improvement in quality of life through reduction of frequency of asthma exacerbations, while reducing the cost of each exacerbation. This benefit was magnified in those who had at least one exacerbation-related ER visit in the year prior to BT, and the authors proposed that BT would be even more cost-effective in those with more frequent exacerbations [21].
A contrasting study was performed in Singapore, where BT combined with standard therapy generated more QALYs over a 5-year period, but was not cost-effective in treating severe asthma. The authors attributed this finding to differing costs of healthcare including the procedure, ED visits, and hospitalizations between Singapore’s healthcare system to the USA [22].
Another study compared the cost of medical management, BT, and omalizumab therapy for those with moderate to severe allergic asthma. The investigators found that BT was a reasonable, cost-effective therapy compared to medical management and omalizumab. Additionally, omalizumab was not found to be cost-effective compared to medical management, despite having improved clinical outcomes [23]. With the introduction of additional biologic therapies since, additional research is warranted to evaluate associated cost-effectiveness.
Many factors may affect cost-effectiveness. For instance, if younger patients may benefit from BT [18], age at which a patient undergoes BT and the duration of treatment effect compared to the cost of biologics during the same period of time may have a significant impact on cost. Other factors, such as pharmaceutical support for biologic therapy may also have a substantial impact in select communities and patient populations. Access to BT may also be limited and institution dependent, requiring specialized equipment and providers able to perform the procedure. While BT has a place in the treatment algorithm for refractory and severe asthma, further studies to better define its role are warranted.
The current GINA guidelines recommend consideration for BT in patients with severe asthma with type 1 inflammation, or those with type 2 inflammation but fail biologic therapy [2•]. The available data supports that a subset of patients with asthma derive a significant benefit from BT. Subgroup analysis suggest that BT may be beneficial even for those on oral corticosteroids at baseline, as well as omalizumab. The PAS2 cohort had a higher use of OCS, and 15.8% of patients were on omalizumab compared to 1.1% in the AIR2 group, suggesting that these patients who are candidates for biologics may equally benefit from BT [14]. The body of BT literature including long-term follow-up data reporting a durable benefit up to 10 years post-treatment supports BT as a powerful treatment option. It is arguably underutilized and under recognized as an efficacious, cost-effective option which warrants ongoing support in guidelines as well as payor support which has been a rate limiting step in adoption.
Targeted Lung Denervation and the Future
Targeted lung denervation (TLD) is a novel bronchoscopic technique utilizing the specialized dNerva™ catheter (Nuvaira Inc., Minneapolis, MN). The catheter delivers radiofrequency ablation to a target tissue depth while also continuously circulating coolant minimizing heat and damage to the inner airway wall. As a result, bronchial branches of the parasympathetic nervous system are disrupted, thereby decreasing airway hyperresponsiveness and inflammation [5, 24].
While novel, several studies have been performed investigating the feasibility, safety, and optimal dosing. The first in-human study published in 2015 evaluated safety defined as freedom from documented and sustained worsening of COPD directly attributable to the procedure and was met in 95% of their cohort [5]. An additional study was performed investigating safety and dose range, demonstrating a safety profile that improved with dose adjustments [25]. A favorable safety profile was maintained in a 3-year follow-up study. In addition, decreased exacerbation rates, improved lung function (measured by FEV1 and FVC), and improvement in symptoms and quality of life, measured by the COPD Assessment Test (CAT) and COPD-specific St George’s Respiratory questionnaire (SGRQ-c), were observed at 3 years [26].
A randomized, sham-controlled, double-blind, prospective multicenter study was then conducted to evaluate safety of TLD in patients with moderate to severe COPD. The study trial demonstrated that TLD, performed in patients on maintenance inhaler therapy, is safe and also associated with fewer adverse respiratory events and hospitalizations over the 1-year follow-up period [27]. This effect was sustained in 2-year follow-up study [28], and a current study is enrolling patients to further investigate treatment and efficacy after TLD [29].
So far, only COPD patients have been investigated and it is yet to be seen if there is a potential benefit in those with asthma alone. While long-acting muscarinic antagonist (LAMA) therapy is only reserved for those with severe asthma or Step 5 of the GINA guideline algorithm for adults [2•], the relaxation of ASM by blocking nerve impulses suggests that TLD may play a role in those with severe asthma as well. A report of two patients with severe asthma treated with TLD showed that the procedure was feasible and safe. There were no adverse events up to 1 year of follow-up; both patients reported subjective improvement in cough with one patient citing significantly reduced rescue inhaler use [30]. More studies are warranted to determine if those with asthma might benefit from TLD.
Looking to the future, airway cryoablation may also play a role in managing those with severe asthma. A study has been performed comparing the effectiveness of BT and cryoballoon ablation (CBA) therapy on ASM in animal models. ASM was reduced in both groups, and thickness was significantly lower in the CBA group at 1 month than BT, suggesting a potential quicker effect [31]. Bronchoscopic rheoplasty, using non-electrical pulsed therapy to destroy airway goblet cells, is currently being studied in those with chronic bronchitis [32]. Goblet cell hyperplasia is also seen in asthma, and electroporation is another potential alternative bronchoscopic therapy worthy of further investigation.
Comment on Bronchoscopy in the Pediatric Asthma Population
While treatment options such as bronchial thermoplasty and bronchial denervation have not been investigated in the pediatric population, bronchoscopy is a key diagnostic tool in the workup of childhood asthma [2•]. Much like in the adult population, bronchoscopy can be used to rule out other etiologies of cough and wheezing, particularly structural abnormalities. Bronchoscopy in the pediatric population can be used to evaluate for tracheobronchomalacia, tracheal and/or bronchial stenosis, as well as extrinsic compression of the airways and other anatomic malformations, including those of the upper airway. Children are also particularly at risk for foreign body aspiration, which can cause symptoms of wheezing, cough, and mucus production. Timely bronchoscopy with either flexible or rigid bronchoscopes should be used to rule out and treat foreign body aspiration if suspected [33]. Similar to the adult diagnostic algorithm, bronchoscopy can be considered for those with refractory disease (2•, 34). Considerations must also be made regarding anesthesia and having trained bronchoscopists in dealing with this population.
Conclusion
The management of asthma can be challenging, particularly for patients with severe or refractory disease, and the role for bronchoscopy in diagnosis and treatment of these patients has evolved over time. While not always indicated, bronchoscopy can be useful, particularly for the investigation of other diagnostic and comorbid considerations. The advent of biologic therapies has changed the landscape for treating severe asthma. However, BT remains an efficacious, safe, durable, and cost-effective therapy and should be considered a therapeutic option. As more data emerges regarding redefining the patient population that may benefit the most, BT should be strongly considered as an adjunctive, if not essential, therapy in asthma.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Most Recent National Asthma Data | CDC. Published May 26, 2022. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm Accessed October 8 2022.
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2022. Available from: www.ginaasthma.org. https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf. Accessed October 8 2022. This article reviews the current Asthma guidelines.
Brusselle GG, Koppelman GH. Biologic therapies for severe asthma. Taichman DB, ed. N Engl J Med. 2022;386(2):157–171. https://doi.org/10.1056/NEJMra2032506
Hashmi MD, Khan A, Shafiq M. Bronchial thermoplasty: state of the art. Respirology. 2022;27(9):720–9. https://doi.org/10.1111/resp.14312. This is a comprehensive,up-to-date review of bronchial thermoplasty.
Slebos DJ, Klooster K, Koegelenberg CFN, et al. Targeted lung denervation for moderate to severe COPD: a pilot study. Thorax. 2015;70(5):411–9. https://doi.org/10.1136/thoraxjnl-2014-206146.
Gibeon D, Zhu J, Sogbesan A, et al. Lipid-laden bronchoalveolar macrophages in asthma and chronic cough. Respir Med. 2014;108(1):71–7. https://doi.org/10.1016/j.rmed.2013.10.005.
Good JT, Kolakowski CA, Groshong SD, Murphy JR, Martin RJ. Refractory asthma. Chest. 2012;141(3):599–606. https://doi.org/10.1378/chest.11-0741.
Ichikawa T, Panariti A, Audusseau S, et al. Effect of bronchial thermoplasty on structural changes and inflammatory mediators in the airways of subjects with severe asthma. Respir Med. 2019;150:165–72. https://doi.org/10.1016/j.rmed.2019.03.005.
Miller JD, Cox G, Vincic L, Lombard CM, Loomas BE, Danek CJ. A prospective feasibility study of bronchial thermoplasty in the human airway. Chest. 2005;127(6):1999–2006. https://doi.org/10.1378/chest.127.6.1999.
Cox G, Thomson NC, Rubin AS, et al. Asthma control during the year after bronchial thermoplasty. N Engl J Med. 2007;356(13):1327–37. https://doi.org/10.1056/NEJMoa064707.
Pavord ID, Cox G, Thomson NC, et al. Safety and efficacy of bronchial thermoplasty in symptomatic, severe asthma. Am J Respir Crit Care Med. 2007;176(12):1185–91. https://doi.org/10.1164/rccm.200704-571OC.
Castro M, Rubin AS, Laviolette M, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med. 2010;181(2):116–24. https://doi.org/10.1164/rccm.200903-0354OC.
Wechsler ME, Laviolette M, Rubin AS, et al. Bronchial thermoplasty: long-term safety and effectiveness in patients with severe persistent asthma. J Allergy Clin Immunol. 2013;132(6):1295-1302.e3. https://doi.org/10.1016/j.jaci.2013.08.009.
Chupp G, Laviolette M, Cohn L, et al. Long-term outcomes of bronchial thermoplasty in subjects with severe asthma: a comparison of 3-year follow-up results from two prospective multicentre studies. Eur Respir J. 2017;50(2):1700017. https://doi.org/10.1183/13993003.00017-2017.
Chupp G, Kline JN, Khatri SB, et al. Bronchial thermoplasty in patients with severe asthma at 5 years. Chest. 2022;161(3):614–28. https://doi.org/10.1016/j.chest.2021.10.044.
Chaudhuri R, Rubin A, Sumino K, et al. Safety and effectiveness of bronchial thermoplasty after 10 years in patients with persistent asthma (BT10+): a follow-up of three randomised controlled trials. Lancet Respir Med. 2021;9(5):457–66. https://doi.org/10.1016/S2213-2600(20)30408-2. This the first study to followup patients>5 years after bronchial thermoplasty.
Goorsenberg AWM, d’Hooghe JNS, Srikanthan K, et al. Bronchial thermoplasty induced airway smooth muscle reduction and clinical response in severe asthma The TASMA Randomized Trial. Am J Respir Crit Care Med. 2021;203(2):175–84. https://doi.org/10.1164/rccm.201911-2298OC.
Ladjemi MZ, Di Candia L, Heddebaut N, et al. Clinical and histopathologic predictors of therapeutic response to bronchial thermoplasty in severe refractory asthma. J Allergy Clin Immunol. 2021;148(5):1227-1235.e6. https://doi.org/10.1016/j.jaci.2020.12.642.
Langton D, Wang W, Thien F, Plummer V. The acute effects of bronchial thermoplasty on FEV1. Respir Med. 2018;137:147–51. https://doi.org/10.1016/j.rmed.2018.03.003.
Langton D, Ing A, Fielding D, et al. Safety and effectiveness of bronchial thermoplasty when FEV1 is less than 50%. Chest. 2020;157(3):509–15. https://doi.org/10.1016/j.chest.2019.08.2193.
Cangelosi MJ, Ortendahl JD, Meckley LM, et al. Cost–effectiveness of bronchial thermoplasty in commercially-insured patients with poorly controlled, severe, persistent asthma. Expert Rev Pharmacoecon Outcomes Res. 2015;15(2):357–64. https://doi.org/10.1586/14737167.2015.978292.
Nguyen HV, Bose S, Mital S, et al. Is bronchial thermoplasty cost-effective as treatment for problematic asthma patients? Singapore’s perspective on a global model: is bronchial thermoplasty cost-effective. Respirology. 2017;22(6):1102–9. https://doi.org/10.1111/resp.13027.
Zafari Z, Sadatsafavi M, Marra CA, Chen W, FitzGerald JM. Cost-effectiveness of bronchial thermoplasty, omalizumab, and standard therapy for moderate-to-severe allergic asthma. Feenstra TL, ed. PLOS ONE. 2016;11(1):e0146003. https://doi.org/10.1371/journal.pone.0146003
Perotin JM, Dewolf M, Launois C, Dormoy V, Deslee G. Bronchoscopic management of asthma. COPD and emphysema Eur Respir Rev. 2021;30(159):200029. https://doi.org/10.1183/16000617.0029-2020.
Valipour A, Shah PL, Pison C, et al. Safety and dose study of targeted lung denervation in moderate/severe COPD patients. Respiration. 2019;98(4):329–39. https://doi.org/10.1159/000500463.
Pison C, Shah PL, Slebos DJ, et al. Safety of denervation following targeted lung denervation therapy for COPD: AIRFLOW-1 3-year outcomes. Respir Res. 2021;22(1):62. https://doi.org/10.1186/s12931-021-01664-5.
Slebos DJ, Shah PL, Herth FJF, et al. Safety and adverse events after targeted lung denervation for symptomatic moderate to severe chronic obstructive pulmonary disease (AIRFLOW) A multicenter randomized controlled clinical trial. Am J Respir Crit Care Med. 2019;200(12):1477–86. https://doi.org/10.1164/rccm.201903-0624OC.
Valipour A, Shah PL, Herth FJ, et al. Two-year outcomes for the double-blind, randomized, sham-controlled study of targeted lung denervation in patients with moderate to severe COPD: AIRFLOW-2. Int J Chron Obstruct Pulmon Dis. 2020;15:2807–16. https://doi.org/10.2147/COPD.S267409.
on behalf of the AIRFLOW-3 Trial Study Group, Slebos DJ, Degano B, et al. Design for a multicenter, randomized, sham-controlled study to evaluate safety and efficacy after treatment with the Nuvaira® lung denervation system in subjects with chronic obstructive pulmonary disease AIRFLOW-3. BMC Pulm Med. 2020;20(1):41. https://doi.org/10.1186/s12890-020-1058-5.
Hartman JE, Srikanthan K, Caneja C, et al. Bronchoscopic targeted lung denervation in patients with severe asthma: preliminary findings. Respiration. 2022;101(2):184–9. https://doi.org/10.1159/000518515.
Li X, Xie SS, Li GS, Zeng J, Duan HX, Wang CH. Effects of bronchial thermoplasty and cryoablation on airway smooth muscle. Chin Med J (Engl). 2021;134(18):2166–74. https://doi.org/10.1097/CM9.0000000000001681.
Valipour A, Fernandez-Bussy S, Ing AJ, et al. Bronchial rheoplasty for treatment of chronic bronchitis Twelve-month results from a multicenter clinical trial. Am J Respir Crit Care Med. 2020;202(5):681–9. https://doi.org/10.1164/rccm.201908-1546OC.
Cramer N, Jabbour N, Tavarez MM, Taylor RS. Foreign body aspiration. In: StatPearls. StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK531480/ Accessed October 9, 2022.
Piccione J, Hysinger EB, Vicencio AG. Pediatric advanced diagnostic and interventional bronchoscopy. Semin Pediatr Surg. 2021;30(3):151065. https://doi.org/10.1016/j.sempedsurg.2021.151065.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Dermatology and Allergy.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ueoka, M., Oh, S. Role of Bronchoscopy in the Diagnosis and Treatment of Severe Asthma. Curr Treat Options Allergy 10, 106–119 (2023). https://doi.org/10.1007/s40521-023-00341-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40521-023-00341-w