Abstract
Background
Several technological advances and digital solutions have been proposed in the recent years to face the emerging need for tele-monitoring older adults with Chronic Obstructive Pulmonary Disease (COPD). However, several challenges have negatively influenced an evidence-based approach to improve Health-Related Quality of Life (HR-QoL) in these patients.
Aim
To assess the effects of tele-monitoring devices on HR-QoL in older adults with COPD.
Methods
On November 11, 2022, PubMed, Scopus, Web of Science, and Cochrane were systematically searched for randomized controlled trials (RCTs) consistent with the following PICO model: older people with COPD as participants, tele-monitoring devices as intervention, any comparator, and HR-QoL as the primary outcome. Functional outcomes, sanitary costs, safety, and feasibility were considered secondary outcomes. The quality assessment was performed in accordance with the Jadad scale.
Results
A total of 1845 records were identified and screened for eligibility. As a result, 5 RCTs assessing 584 patients (423 males and 161 females) were included in the systematic review. Tele-monitoring devices were ASTRI telecare system, WeChat social media, Pedometer, SweetAge monitoring system, and CHROMED monitoring platform. No significant improvements in terms of HR-QoL were reported in the included studies. However, positive effects were shown in terms of the number of respiratory events and hospitalization in patients telemonitored by SweetAge system and CHROMED platform.
Discussion
Although a little evidence supports the role of tele-monitoring devices in improving HR-QoL in older patients, positive effects were reported in COPD exacerbation consequences and functional outcomes.
Conclusion
Tele-monitoring solutions might be considered as sustainable strategies to implement HR-QoL in the long-term management of older patients with COPD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a disabling condition affecting approximately 14.2% of older adults [1], representing a significant cause of mobility and mortality [2,3,4,5,6,7,8,9,10]. The most recent report of the World Health Organization (WHO) estimated that over 65 million patients worldwide suffer from COPD, with crucial implications for physical, psychological, and social well-being [11,12,13]. Moreover, COPD represents a major economic burden for sanitary systems, with over 50 billion dollars spent in the United States and 2047 and 10,701 euros per patient spent in Europe every year [14]. In addition, the impact of respiratory symptoms on physical function and activities of daily living has been identified as a major contributory factor in the growing trend of disability underlined by the Global Burden of Disease Study of 2019 [15]. In this context, Health-related Quality of Life (HR-QoL) represents a critical issue due to the high levels of psychological distress that has been identified as highly prevalent in these subjects particularly in older adults [16, 17].
Rehabilitation should be considered a cost-effective therapy to improve HR-QoL in patients affected by COPD, with level II evidence supporting its effects in preventing COPD exacerbations and improving physical function in frail patients [18]. Despite these considerations, several barriers still affect rehabilitation in community settings, and pulmonary rehabilitation programs are still regrettably underestimated and underused [4, 19, 20].
Notably, several tele-monitoring, telemedicine, and tele-rehabilitation solutions have been proposed in the recent years to improve the clinical management and assistance at home of frail patients affected by respiratory disorders [21,22,23]. In this context, recent reports [4, 24] underlined that tele-rehabilitation might not be inferior to standard pulmonary rehabilitation in terms of functional outcomes and could be a useful tool for overcoming barriers to rehabilitation delivery in community-based settings. Moreover, telehealth solutions might reduce the resources and time that healthcare practitioners spend on the long-term management of COPD [25]. In this scenario, few systematic reviews assessed the effects of tele-monitoring patients with COPD [26,27,28,29]. However, to date, no previous systematic review focused on older adults. Nevertheless, different limitations might affect adherence to telehealth programs in older adults, including lack of access to technology or technology skills or patient impairment in hearing, vision, communication, or cognitive functions [30, 31].
Thus, implementing precise monitoring solutions might have a crucial role in the tailored management of frail patients with COPD, guiding clinicians in a more personalized approach to COPD-related disability.
Altogether, these findings suggested that the clinical integration of digital solutions should be considered a suitable option to optimize healthcare delivery and potentially reduce healthcare costs related to respiratory diseases. Nevertheless, to date, there is still a gap of knowledge about the available digital devices used for tele-monitoring older adults with COPD, and the role of digital innovation in the clinical management of these patients is still debated.
Therefore, the aim of this systematic review was to provide a broad overview about the currently available instrumental tools for tele-monitoring COPD patients, highlighting the potential effects of digital innovation to improve the HR-QoL of these patients.
Methods
Registration
This systematic review has been performed ethically in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [32]. The international prospective register of systematic reviews (PROSPERO) was preliminarily searched for similar review protocols in progress. No similar review was identified; thus, the systematic review was submitted to PROSPERO and accepted on November 26, 2022 (available at https://www.crd.york.ac.uk/prospero; registration number CRD42022340500).
Search strategy
Four databases [PubMed/Medline, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials (CENTRAL)] were systematically searched simultaneously by two different independent investigators (L.L. and A.d.S.) 2022. The search strategies for each database are shown in Table 1.
Selection criteria
In accordance with the PICO model, we considered eligible clinical trials satisfying the following criteria:
-
P) Participants: older adults with COPD;
-
I) Intervention: we considered all tele-monitoring devices to assess patients in community settings;
-
C) Comparator: any comparator.
-
O) Outcome: the primary outcome was HR-QoL assessed with any validated scale. The secondary outcomes were: (i) Pulmonary function; (ii) Physical function; (iii) Adherence and feasibility; (iv) Costs; v) Safety.
Only clinical trials published in peer-reviewed International Journal were included. The exclusion criteria were: (i) studies involving animals; (ii) participants with pregnancy, clinical instability, or palliation; (iii) Master or doctorate theses, letters to the editor, and conference proceedings; (iv) language other than English. No publication date restriction was applied.
After duplication removal, the records were screened by two investigators that independently reviewed titles and abstracts (A.T. and A.F.). The articles meeting the enrollment criteria proceeded to the full-text review screening phase. Any disagreements were discussed with a third reviewer (L.L.) to reach a consensus.
Data extraction and synthesis
Two independent reviewers (A.T. and A.F.) assessed all the records screened in full text for eligibility, and relevant data were extracted using Excel. Any disagreement was solved by discussion between the two reviewers or by consulting a third reviewer (L.L.).
Therefore, a qualitative method has been used in data synthesis. More in detail, the following data have been presented: (1) title; (2) authors; (3) publication year; (4) nationality; (5) participants (number, mean age and age range, gender); (6) interventions´ characteristics; (7) comparator; (8) main findings (which presented the study results in terms of primary and secondary outcomes).
The data have been synthesized by two authors (A.T. and A.F.) independently from full-text documents. Any disagreement between the two reviewers has been solved by collegial discussion among the authors. In case of disagreement, a third author (L.L.) has been asked to provide an additional opinion.
Text and tables have been used to provide a descriptive summary and explanation of study characteristics and findings.
Quality assessment and risk of bias
The quality of the studies included was assessed independently by two Authors (A.T. and A.F.), according to the Jadad scale [33]. Discordances were solved by discussion between the Authors or by asking a third reviewer (L.L.). The items assessed were the following (i) random sequence generation; (ii) appropriate randomization; (iii) blinding of participants or personnel; (iv) blinding of outcome assessors; (v) withdrawals and dropouts. A Jadad score between 3 and 5 points was considered high quality.
The Cochrane risk-of-bias tool for randomized trials (RoBv.2) [34] was implemented for risk-of-bias assessment. The following domains were assessed by RoBv.2: (i) randomization process; (ii) deviations from the intended interventions; (iii) missing outcome data; (iv) measurements of the outcome; (v) selection of the reported results. According to these items, bias was classified as low, high, or some concerns.
Results
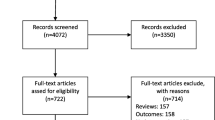
Through our search strategy, 1845 records were identified. Figure 1 shows the PRISMA 2020 flow diagram of the search process in detail. After duplication removal, 988 studies were assessed for eligibility and screened for title and abstract. Therefore, 878 records were excluded, and 110 full-text records were assessed for eligibility. One hundred and five records were excluded for inconsistency with the eligibility criteria. The studies assessed in full text and the reasons for exclusions are presented in detail in Supplementary Table 1. As a result, 5 studies were included in the present work [35,36,37,38,39].
Characteristics of the study included and study samples
The RCTs included were published between 2012 [35] and 2020 [36]. One study was conducted in Hong Kong [35], one was conducted in Japan [37], one was conducted in China [36], one was conducted in Italy [38], and one was an international collaboration [39]. Further details on the characteristics of the included studies are shown in Table 2.
In the present systematic review, a total of 584 subjects were assessed, 423 males and 161 females [35,36,37,38,39]. More in detail, 291 COPD patients were included in the intervention groups, while 293 COPD patients were included in the control groups. The subjects’ ages ranged from 70.92 ± 6.38 years [36] to 75 ± 9 years [37].
Intervention treatment assessed by tele-monitoring systems
In the present review, a high heterogeneity of digital devices was identified. More in detail, the devices and applications used to remotely monitor patients during therapeutic interventions were ASTRI telecare system (ATS) [35], WeChat social media [36], Pedometer [37], SweetAge monitoring system [38], and CHROMED monitoring platform [39]. Figure 2 shows digital tools description and a figure for each device in order to better summarize the devices and applications used to remotely monitor patients with COPD.
The therapeutic interventions assessed were different among the studies included. Specifically, 1 study [36] assessed Pulmonary Internet Explorer Rehabilitation (PeR), a therapeutic protocol based on evaluation, respiratory training, sports training, dietary counseling, and education on medication. Patients completed the home-based pulmonary rehabilitation program and data were recorded by a self-assessment report, and subsequently uploaded on WeChat.
In the study by Kawagoshi et al. [37], the authors assessed the effects of pulmonary rehabilitation sessions monitored by a pedometer, associated with monthly feedback. The pedometer was attached to the patient’s belt at the waist for a period of 12 h (from waking time until going to bed) each day for 1 year. In addition, a multidisciplinary home-based program was performed, including breathing retraining, sitting calisthenics, respiratory muscle stretching calisthenics, level walking for at least 15 min, inspiratory muscle exercises using an inspiratory muscle trainer intensity of 30–40% of the maximal inspiratory muscle force, and monthly 45 min education program. Patients practiced this program daily at home and were supervised by a respiratory therapist every 2 weeks.
On the other hand, three studies did not assess therapeutic rehabilitation intervention and tele-monitored patients at home [35, 38, 39]. The study by Pedone et al. [38] evaluated the role of the SweetAge monitoring system set up to perform 5 measurements of each parameter every three hours. Oxygen saturation was measured over 1 min. For the other parameters, five measurements of 1 min each were performed at a sampling rate of 60 Hz. The data received were analyzed every day by a physician skilled in the care of respiratory patients. The study by Chau et al. [35] assessed oxygen saturation, pulse rate, and respiration rate monitoring (three times a day from Monday to Friday) and transmitting the data to the online network platform. In the study by Walker et al. [39], the intervention group used the CHROMED monitoring platform for nine months at approximately the same time each day. Every two months, participants were contacted by phone and completed the questionnaires.
Control groups
Control groups included COPD patients that underwent usual care and conventional pulmonary rehabilitation. More in detail, control groups received usual care in 2 studies [35, 39], face-to-face pulmonary rehabilitation training in 1 study [36], and multidisciplinary home-based program in 1 study [37], including breathing retraining, sitting calisthenics, respiratory muscle stretching calisthenics, level walking for at least 15 min, inspiratory muscle exercises using an inspiratory muscle trainer intensity of 30–40% of the maximal inspiratory muscle force, and monthly 45-min education program. Just one study [38] did not report the intervention administered in the control group. Table 2 better characterizes the control groups for each study included and the treatments received.
Primary outcomes—health-related quality of life
Health-Related Quality of Life (HR-QoL) was assessed in 4 studies [35,36,37, 39]. More in detail, 2 studies [35, 37] assessed HR-QoL with the Chronic Respiratory Questionnaire (CRQ). In the study by Chau et al. [35], the authors did not report significant differences between groups in terms of CRQ subscales assessing dyspnea, fatigue, emotion, and mastery (p > 0.05).
On the other hand, the study by Kawagoshi et al. [37] showed significant improvement in CRQ in both intervention and control groups. In the study by Jiang et al. [36], HR-QoL was assessed with the chronic obstructive pulmonary disease assessment test (CAT). Nevertheless, the authors did not report significant differences between groups (p = 0.53). Lastly, the study by Walker et al. [39] assessed HR-QoL with the EuroQoL EQ-5D questionnaire (EQ-5D), chronic obstructive pulmonary disease assessment tool (CAT), and Patient Health Questionnaire (PHQ-9) scores. However, there were no significant between-group differences in the EQ-5D, CAT, or PHQ-9 scores (p > 0.05). Table 2 shows further details on outcomes assessed in each study included.
Secondary outcomes—pulmonary function
Two papers [35, 36] included in our study assessed Pulmonary Function. In particular, the study conducted by Chau et al. [35], assessed the pulmonary function in terms of % predicted Forced Expiratory Volume in one second (%FEV1) and FEV1/forced vital capacity (FVC) ratio. The authors reported no significant differences between-group in terms of %FEV1, FEV1/FVC ratio (all p > 0.05). In the study by Jiang [36], pulmonary function was evaluated with the modified Medical Research Council scale (mMRC) that provides a measurement method for perceived dyspnea. The authors reported no significant differences between groups (p > 0.05).
Secondary outcomes—physical function
Two papers [36, 37] assessed functional outcomes. In one study [36], physical function was assessed by the St. George Respiratory Questionnaire (SGRQ), showing no significant inter-group difference (p > 0.05). In addition, the authors assessed physical function with Exercise Self-Regulatory Efficacy Scale (Ex-SRES), without reporting significant differences between groups (p = 0.63).
In the study by Kawagoshi [37], daily walking time, physical performance assessed with the 6 Minutes Walking Test (6MWT), and quadriceps femoris muscle force (QF) were assessed. The authors reported an increase in the time spent walking in the intervention group (51.3 ± 63.7 min/day), with significant differences compared to the control group (12.3 ± 25.5 min/day) after the pulmonary rehabilitation. Moreover, changes in the time spent standing were significantly correlated with 6MWT (r = 0.401, p = 0.038). Lastly, the improvement rate of daily walking time after PR was significantly related to QF in all subjects.
Secondary outcomes—adherence and feasibility
In the study by Chau et al. [35], eight patients withdrew before the intervention: two patients withdrew due to worsening physical condition, two patients withdrew due to financial reasons, two patients refused to use the belt to measure their respiration rate in cold weather, one refused further participation as he commented that the device was difficult to carry around at work, and one patient found participation too demanding with regard to the frequency of tele-monitoring per day. Additionally, in the study by Jiang et al. [36], the intervention group showed a dropout of 6 patients, including 3 patients who felt that rehabilitation was of no use, 1 patient who got worse, and 2 who moved to other places. Concurrently, a dropout of 6 patients was reported in the control group, including 2 patients who moved to other places, 2 patients who got worse, and 2 patients who felt rehabilitation was of no use. Similarly, Kawagoshi et al. [37] showed that 12 patients dropped out of the rehabilitation program due to an acute exacerbation requiring long-term hospitalization (n = 2), death (n = 2), and a lack of motivation or personal reasons (n = 8). In the study by Pedone et al. [38], the main causes of drop-out were patients feeling uncomfortable with the wearable device or thinking that they disrupted the daily life rhythm. Walker et al. [39] showed that in the IG the main causes of drop-out were death (n = 3), patient worsening/hospitalization (n = 8), personal problems/decline to continue (n = 27), and technical issues/difficulties in using the equipment (n = 7), and in the CG were death (n = 4), patient worsening/hospitalization (n = 7), and personal problems/decline to continue (n = 25).
Secondary outcomes—costs
Just one study [39] assessed the sustainability and cost-effectiveness of tele-monitoring older people with COPD. The mean cost per patient in the intervention group was lower than in the control group for all the analyzed subgroups except for the subgroup with severe or very severe COPD. The largest differences in terms of costs were shown in patients with a previous hospitalization with COPD (€4147 vs. €6949, p = 0.008).
Secondary outcomes—safety
Only three papers [35, 38, 39] assessed the safety of tele-monitoring in older adults with COPD. In particular, the study by Chau et al. [35] assessed the number of emergency department visits and hospital readmissions during the intervention treatment. No significant differences in the number of emergency department visits and hospital readmissions between groups were found (p > 0.05). In the study by Pedone et al. [38], safety was assessed by the incidence rate of respiratory events and hospital admissions. The incidence rate of respiratory events was 28/100 person/years in the intervention group vs. 42/100 person/years in the control group (IRR: 0.67, 95% CI: 0.32–1.36). Similarly, the hospital admissions were 13/100 person/years and 20/100 person/years, respectively (IRR: 0.66, 95% CI: 0.21–1.86).
The study by Walker et al. [39] assessed hospitalization rate and time to the first hospitalization. The main finding is that telemedicine was associated with fewer repeat hospitalizations (− 54%, p = 0.017). Previously hospitalized patients showed the greatest reduction in hospitalization rate (− 53%, p = 0.017). The authors showed that tele-monitoring did not affect the time to first hospitalization (p > 0.05).
Quality assessment and risk of bias
According to the Jadad scale [33], all studies included (n = 5, 100%) [35,36,37,38,39] resulted in high-quality, with one study [36] reporting a score of 4, and four studies [35, 37,38,39] reporting a score of 3. It should be noted that due to the intrinsic nature of the intervention, it was impossible to blind both personnel and participants, which resulted in a score of 0 in the related item for all studies (n = 5, 100%) [35,36,37,38,39]. Table 3 shows in detail the score of each sub-item of the Jadad scale.
According to RoBv.2 [34], all studies (n = 5, 100%) [35,36,37,38,39] ensured a low risk of bias for the randomization process, measurement of the outcome, and selection of the reported result. The major concerns were about possible deviations from the intended interventions; this was mainly due to the lack of an appropriate analysis estimating the effect of assignment to intervention. In particular, 2 studies (40%) [35, 37] showed some concerns in the second domain because it was not clarified the intention-to-treat analysis; this evaluation leads to an overall presence of concerns regarding the risk of bias of the studies. Further information is shown in Fig. 3.
Discussion
Tele-monitoring systems have been recently proposed as suitable tools to effectively promote sustainable screening and optimize early identification of symptom worsening in COPD patients. These approaches might have crucial implications to implement early therapeutic interventions and improve the complex clinical management of these patients [26,27,28,29]. Despite these considerations, several barriers still affect their applicability in clinical settings, and their implementation in the management of older adults affected by respiratory conditions is still challenging [30, 31]. Therefore, the aim of this study was to assess the currently available tele-monitoring devices used in the clinical management of patients with COPD, characterizing their impact on HR-QoL.
The results of this systematic review highlighted a high heterogeneity in terms of the type of technology used, including five different technological tools [35,36,37,38,39]. More in detail, two studies [36, 37] assessed the effects of a comprehensive rehabilitation intervention at home tele-monitored with digital tools. These studies showed promising effects in terms of HR-QoL in older patients performing home-based rehabilitation. However, no significant advantages were shown in tele-monitored patients suggesting that the significant effects in terms of HR-QoL found in the intervention group might be related to the widely noted benefits of pulmonary rehabilitation programs rather than to the technological tools [40]. In accordance, the studies that did not investigate the impact of rehabilitation programs did not report significant differences between groups in terms of HR-QoL improvement [35, 38, 39]. Thus, the results of the present systematic review suggested that tele-monitoring devices were not effective in improving HR-QoL of older patients affected by COPD.
Similarly, positive results were reported on functional outcomes in both studies assessing tele-monitoring systems to assisted pulmonary rehabilitation programs [36, 37]. On the other hand, no significant differences were reported between standard pulmonary rehabilitation and tele-monitored ones in terms of functional outcomes.
In contrast, intriguing results were reported in terms of the number of respiratory events and hospitalization rate, with two studies suggesting positive effects of tele-monitoring systems on these crucial outcomes [38, 39]. Thus, these results are particularly important due to the higher rate of pulmonary complications in frail older patients that might need a comprehensive approach, including digital innovation, with positive implications in terms of both clinical outcomes and sanitary cost reduction [41,42,43,44,45]. In addition, it should be noted that positive effects on sanitary costs have been previously reported, underlining that the clinical implementation of a tele-monitoring system in routine clinical settings might be a suitable strategy to enhance the long-term health care of older patients affected by COPD. Moreover, our findings reported good feasibility data about specific tele-monitoring systems, suggesting that these tools might be effectively accepted by patients with COPD, even in older adults. In this scenario, specific strategies are needed to increase awareness among the different healthcare professions about the currently available digital solutions to improve patient engagement in a tailored technological approach in a community setting [4].
Despite these positive results, previous systematic reviews assessed the effects of tele-monitoring systems in COPD patients’ HR-QoL providing controversial conclusions. More in detail, in 2011, McLean et al. [28] evaluated the role of telehealth interventions in COPD patients. Interestingly, the authors reported that telehealth interventions might reduce the risk of emergency department attendance and hospitalization of these patients. However, the authors did not focus on HR-QoL, and no information about this outcome was provided. Differently, in 2016 the systematic review by Gregersen et al. [26] assessed the effects of telehealth intervention in terms of HR-QoL in patients with COPD. In this scenario, the authors reported that few studies were available to fully characterize the effects of telehealth intervention in HR-QoL. However, due to the boosting of telemedicine and tele-rehabilitation during the COVID-19 pandemic [46, 47], an update is necessary to further characterize the recent advance in telemedicine solutions optimizing health outcomes in patients with respiratory conditions. Additionally, to the best of our knowledge, no previous systematic review focused on older adults, despite the growing evidence emphasizing the need for tailored strategies for older people due to limitations in accessibility to technological innovations. In this scenario, two systematic reviews [27, 29] assessed the effects of tele-monitoring systems on patient’s adherence. The results of these studies underlined that the individual assessment of patients’ needs is mandatory to improve adherence and acceptance of tele-monitoring systems. In line with this evidence, our systematic review focused on older adults, a target population with specific needs and characterized by several barriers to technological advances [30, 31]. In particular, it has been reported that older adults might have low technology skills, and impairment in hearing, vision, communication, or cognitive functions, with detrimental consequences on tele-monitoring system implementation in a clinical setting [30, 31].
Despite these considerations, we are aware that the present review is not free from limitations. In particular, the small number of studies included might be considered the main limitation of this work. On the other hand, this result reflects the low number of studies focusing on older adults with COPD. Given the recent trend of personalized medicine, further evidence is needed to better characterize the benefits of digital innovation in older adults with COPD. Moreover, due to the large heterogeneity of technological devices assessed, a meta-analysis was not possible, in accordance with the Cochrane Handbook for Systematic Review of Intervention (Ver, 6.1, 2020) [48].
Conclusions
In recent years, growing attention has been paid to telehealth solutions and digital innovation in pulmonary disorders. However, to date, several questions are still open about the effects of tele-monitoring devices on frail older adults. Altogether, the results of the present systematic review showed promising effects of the SweetAge system and CHROMED platform, with potential implications for healthcare monitoring in the community setting for these subjects. On the other hand, the few studies included in this review reflect a large gap of knowledge in this field about the evidence focusing on technological advances in older adults. Therefore, it should be noted that further studies are needed to better characterize the optimal tele-monitoring devices to better address the critical issue of HR-QoL in older adults suffering from COPD.
Data availability
The dataset is available on request.
References
Halbert RJ, Natoli JL, Gano A (2006) Global burden of COPD: systematic review and meta-analysis. Eur Respir J 28:523–532
de Sire A, Lippi L, Aprile V et al (2022) Pharmacological, Nutritional, and Rehabilitative Interventions to Improve the Complex Management of Osteoporosis in Patients with Chronic Obstructive Pulmonary Disease: A Narrative Review. J Pers Med 12:1626
Ståhl E, Lindberg A, Jansson SA et al (2005) Health-related quality of life is related to COPD disease severity. Health Qual Life Outcomes 3:56
Lippi L, D'Abrosca F, Folli A et al (2022) Closing the Gap between Inpatient and Outpatient Settings: Integrating Pulmonary Rehabilitation and Technological Advances in the Comprehensive Management of Frail Patients. Int J Environ Res Public Health 19:9150
Costanzo L, Pedone C, Battistoni F (2017) Relationship between FEV(1) and arterial stiffness in elderly people with chronic obstructive pulmonary disease. Aging Clin Exp Res 29:157–164
Testa G, Cacciatore F, Bianco A (2017) Chronic obstructive pulmonary disease and long-term mortality in elderly subjects with chronic heart failure. Aging Clin Exp Res 29:1157–1164
Ozalevli S, Ilgin D, Narin S (2011) Association between disease-related factors and balance and falls among the elderly with COPD: a cross-sectional study. Aging Clin Exp Res 23:372–377
Apostolovic S, Jankovic-Tomasevic R, Salinger-Martinovic S (2011) Frequency and significance of unrecognized chronic obstructive pulmonary disease in elderly patients with stable heart failure. Aging Clin Exp Res 23:337–342
Antonelli Incalzi R (2004) Management of chronic obstructive pulmonary disease in the elderly. Aging Clin Exp Res 16:13–21
Antonelli Incalzi R, Pistelli R, Imperiale C (2004) Effects of chronic airway disease on health status of geriatric patients. Aging Clin Exp Res 16:26–33
Sritharan SS, Østergaard EB, Callesen J (2021) Barriers toward physical activity in COPD: a quantitative cross-sectional, questionnaire-based study. COPD 18:272–280
Scarlata S, Finamore P, Laudisio A (2021) Association between frailty index, lung function, and major clinical determinants in chronic obstructive pulmonary disease. Aging Clin Exp Res 33:2165–2173
Galizia G, Cacciatore F, Testa G (2011) Role of clinical frailty on long-term mortality of elderly subjects with and without chronic obstructive pulmonary disease. Aging Clin Exp Res 23:118–125
Mei F, Dalmartello M, Bonifazi M (2022) Chronic obstructive pulmonary disease (COPD) mortality trends worldwide: an update to 2019. Respirology. https://doi.org/10.1111/resp.14328
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1204–1222
Dziewierz A, Tokarek T, Kleczynski P (2018) Impact of chronic obstructive pulmonary disease and frailty on long-term outcomes and quality of life after transcatheter aortic valve implantation. Aging Clin Exp Res 30:1033–1040
Finamore P, Spruit MA, Schols J (2021) Clustering of patients with end-stage chronic diseases by symptoms: a new approach to identify health needs. Aging Clin Exp Res 33:407–417
Li N, Li P, Lu Y (2020) Effects of resistance training on exercise capacity in elderly patients with chronic obstructive pulmonary disease: a meta-analysis and systematic review. Aging Clin Exp Res 32:1911–1922
Golmohammadi K, Jacobs P, Sin DD (2004) Economic evaluation of a community-based pulmonary rehabilitation program for chronic obstructive pulmonary disease. Lung 182:187–196
Spitzer KA, Stefan MS, Priya A (2019) Participation in pulmonary rehabilitation after hospitalization for chronic obstructive pulmonary disease among medicare beneficiaries. Ann Am Thorac Soc 16:99–106
Md Fadzil NH, Shahar S, Rajikan R et al (2022) A scoping review for usage of telerehabilitation among older adults with mild cognitive impairment or cognitive frailty. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph19074000
Sebio-García R (2020) Pulmonary rehabilitation: time for an upgrade. J Clin Med. https://doi.org/10.3390/jcm9092742
Hao JF, Cui HM, Han JM (2014) Tele-ICU: the way forward in geriatric care? Aging Clin Exp Res 26:575–582
Stickland MK, Jourdain T, Wong EY (2011) Using telehealth technology to deliver pulmonary rehabilitation to patients with chronic obstructive pulmonary disease. Can Respir J 18:216–220
Russo JE, McCool RR, Davies L (2016) VA telemedicine: an analysis of cost and time savings. Telemed J E Health 22:209–215
Gregersen TL, Green A, Frausing E (2016) Do telemedical interventions improve quality of life in patients with COPD? A systematic review. Int J Chron Obstruct Pulmon Dis 11:809–822
Alghamdi SM, Janaudis-Ferreira T, Alhasani R (2019) Acceptance, adherence and dropout rates of individuals with COPD approached in telehealth interventions: a protocol for systematic review and meta-analysis. BMJ Open 9:e026794
McLean S, Nurmatov U, Liu JL (2011) Telehealthcare for chronic obstructive pulmonary disease. Cochrane Database of Syst Rev. https://doi.org/10.1002/14651858.CD007718.pub2
Cruz J, Brooks D, Marques A (2014) Home telemonitoring in COPD: a systematic review of methodologies and patients’ adherence. Int J Med Informatics 83:249–263
Kalicki AV, Moody KA, Franzosa E (2021) Barriers to telehealth access among homebound older adults. J Am Geriatr Soc 69:2404–2411
Kruse C, Fohn J, Wilson N (2020) Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: systematic review. JMIR Med Inform 8:e20359
Moher D, Liberati A, Tetzlaff J (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Jadad AR, Moore RA, Carroll D (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Sterne JAC, Savović J, Page MJ (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Chau JP, Lee DT, Yu DS (2012) A feasibility study to investigate the acceptability and potential effectiveness of a telecare service for older people with chronic obstructive pulmonary disease. Int J Med Inform 81:674–682
Jiang Y, Liu F, Guo J (2020) Evaluating an intervention program using wechat for patients with chronic obstructive pulmonary disease: randomized controlled trial. J Med Internet Res 22:e17089
Kawagoshi A, Kiyokawa N, Sugawara K (2015) Effects of low-intensity exercise and home-based pulmonary rehabilitation with pedometer feedback on physical activity in elderly patients with chronic obstructive pulmonary disease. Respir Med 109:364–371
Pedone C, Chiurco D, Scarlata S (2013) Efficacy of multiparametric telemonitoring on respiratory outcomes in elderly people with COPD: a randomized controlled trial. BMC Health Serv Res 13:82
Walker PP, Pompilio PP, Zanaboni P (2018) Telemonitoring in chronic obstructive pulmonary disease (CHROMED). A randomized clinical trial. Am J Respir Crit Care Med 198:620–628
Lacasse Y, Martin S, Lasserson T (2007) Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. A Cochrane systematic review. Eur medicophys 43:475–485
Yang J, Lin R, Xu Z, Zhang H (2019) Significance of pulmonary rehabilitation in improving quality of life for subjects with COPD. Respir Care 64:99–107
Spruit MA, Augustin IM, Vanfleteren LE (2015) Differential response to pulmonary rehabilitation in COPD: multidimensional profiling. Eur Respir J 46:1625–1635
Spruit MA, Pitta F, McAuley E (2015) Pulmonary rehabilitation and physical activity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 192:924–933
Gephine S, Saey D, Grosbois J-M (2022) Home-based pulmonary rehabilitation is effective in frail COPD patients with chronic respiratory failure. Chronic Obstr Pulm Dis 9:15–25
Attwell L, Vassallo M (2017) Response to pulmonary rehabilitation in older people with physical frailty, sarcopenia and chronic lung disease. Geriatrics 2:9
de Sire A, Andrenelli E, Negrini F (2020) Rehabilitation and COVID-19: the Cochrane Rehabilitation 2020 rapid living systematic review. Update as of August 31st, 2020 Eur J Phys Rehabil Med 56:839–845
de Sire A, Marotta N, Agostini F (2022) A telerehabilitation approach to chronic facial paralysis in the COVID-19 pandemic scenario: what role for electromyography assessment? J Pers Med. https://doi.org/10.3390/jpm12030497
Higgins JPT, Thomas J, Chandler J et al Eds (2021) Cochrane handbook for systematic reviews of interventions version 6.2 Wiley
Acknowledgements
None.
Funding
The study was not funded.
Author information
Authors and Affiliations
Contributions
Conceptualization: LL, AdS, and MI; Methodology: AdS, and MI; Database searching: LL, AdS, MI; Data screening: LL, AT, AF; Data extraction LL, AT, AF; Data synthesis and interpretation: LL, AT, AF; Writing—original draft preparation: LL, AT, AdS; Writing—review and editing: KM, MI; Visualization: AF, FDA, CC; Study supervision: AdS, MI. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflicts of interest.
Consent to participate
For this type of study, formal consent is not required.
Consent for publication
All the authors declare that they give their consent for publication.
Research involves human and animals rights participants
This review reports no participant data or original research findings that require ethics approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lippi, L., Turco, A., Folli, A. et al. Technological advances and digital solutions to improve quality of life in older adults with chronic obstructive pulmonary disease: a systematic review. Aging Clin Exp Res 35, 953–968 (2023). https://doi.org/10.1007/s40520-023-02381-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02381-3