Abstract
Objective
The objective of this study was to summarize and determine the effectiveness of resistance training on exercise capacity in patients with chronic obstructive pulmonary disease (COPD).
Methods
We searched PubMed, EMBASE, Cochrane Library, and two Chinese databases (China National Knowledge Infrastructure and Wanfang Data) to identify articles written in English or Chinese and published from January 2000 to January 2019. Randomized controlled trials were included if they evaluated the effects of resistance training on exercise capacity in COPD patients. We assessed the quality of the trials using the Physiotherapy Evidence Database Scale. Data from these studies were pooled to calculate weighted mean difference (WMD) or standardized mean difference (SMD) with 95% confidence intervals (CI).
Results
Eleven studies with a total of 405 participants met the inclusion criteria. Compared with the non-exercise control group, resistance training significantly improved 6-min walking distance (WMD, 54.52; 95% CI 25.47–83.56; I2 = 43%; P = 0.14), transfer numbers for the 6-min pegboard and ring test (WMD, 25.17; 95% CI 10.17–40.16; I2 = 0%; P = 0.55), and tolerance time for the unsupported upper-limb exercise test (SMD, 0.41; 95% CI 0.03–0.79; I2 = 0%; P = 0.83). There were no significant differences in constant work rate endurance test results or in peak oxygen uptake between the two groups.
Conclusions
Resistance training was an effective approach to improve functional exercise capacity, endurance exercise capacity, and peak exercise capacity in COPD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common disease that is characterized by persistent respiratory symptoms and airflow limitation [1]. According to a 2018 Lancet report, the prevalence of COPD has risen from 8.2% in 2008 to 13.7% among Chinese people aged ≥ 40 years [2]. Patients with COPD often complain of a decline in exercise capacity, which is associated with hospital admissions [3], leading to a substantial financial burden on individuals and families. Exercise capacity is the most significant predictor of mortality in COPD patients [4]. In addition, exercise capacity showed measurable and progressive deterioration with the decline of airflow limitation in COPD patients [5]. Therefore, COPD patients and clinical staff should place high emphasis on the evaluation and rehabilitation of exercise capacity.
Exercise training, as the cornerstone of pulmonary rehabilitation, is the optimal strategy for improving exercise capacity and health-related quality of life (QOL) in COPD patients [6]. Resistance training method, which uses specific resistance to induce muscle contractions, requires fewer minute ventilation and oxygen consumption, thereby causing less dyspnea [7]. Recently, research into training with elastic bands training has been conducted, extending the prospective applications of resistance training [8]. Studies have shown that resistance training significantly improves pulmonary function [9] and reverses muscle dysfunction in patients with COPD [10]. Liao et al. found that resistance training improved the percentage of predicted forced expiratory volume (FEV1), the dyspnea domain of the Chronic Respiratory Disease Questionnaire and skeletal muscle strength [11]. As dyspnea and muscle functions are the main factors influencing the exercise capacity of patients with COPD, it can be speculated that resistance training is an effective rehabilitation method for improving the exercise capacity in such patients.
However, previous meta-analyses have not demonstrated the effectiveness of resistance training on various types of exercise capacity in patients with COPD. Of these studies, that by Liao et al. found that resistance training could not induce significant improvements in 6-min walking distance (6MWD), maximum oxygen consumption (VO2max) or maximum exercise workload [11]. McKeough et al. found that upper limb resistance training did not significantly improve the results of the incremental arm crank test, unsupported upper limb exercise test (UULEX) or 6-min pegboard and ring test (6PBRT) [12]. Moreover, the abovementioned meta-analyses had many limitations, including small sample size and low methodological quality of included studies. Clinical trials have demonstrated the positive role of resistance training in improving the exercise capacity of COPD patients [13,14,15]. Considering the controversy of resistance training targeted at such improvement, an updated meta-analysis focused on the specific effects of resistance training on various types of exercise capacity should be conducted.
According to the differences between the relative contributions of subjective and objective factors to performance on different exercise tests [16, 17], exercise capacity can be divided into three types: functional, endurance, and peak. The 6-min walk test (6MWT) reflects the functional exercise capacity [18], the constant work rate endurance test (CWRET) and the 6PBRT reflect endurance exercise capacity [12, 19], and cardiopulmonary exercise test (CPET) and the UULEX reflect peak exercise capacity [12, 19]. Therefore, in this study, we aimed to analyze the results of these different exercise tests to explore the comprehensive effect of resistance training on the various types of exercise capacities of COPD patients.
Methods
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.
Literature search strategy
To identify randomized controlled trials (RCTs) of resistance training intervention for COPD patients, we searched PubMed, EMBASE, Cochrane Library, the China National Knowledge Infrastructure (CNKI), and Wanfang Data for the time period January 2000 to January 2019. All publications in English or Chinese were considered. The search strategy used three sets of keywords and synonyms: participants, interventions, and study design. The controlled vocabulary is shown in Table 1. In addition, we screened references to relevant systematic reviews and meta-analyses to find other potentially eligible studies.
Inclusion and exclusion criteria
Inclusion criteria were as follows: (a) participants with stable moderate-to-severe COPD; (b) ≥ 4 weeks’ resistance training intervention; (c) a comparable control group for other treatments, including health education and breathing training; (d) outcomes including 6MWT, CWRET, 6PBRT, UULEX, and CPET; and (e) RCTs.
Exclusion criteria were as follows: (a) patients with acute exacerbations of COPD, with the healthy population as the control group; (b) combined endurance and resistance training for intervention, with endurance training for the control group; (c) within-group comparison before and after intervention; (d) no extractable data; and (e) low methodological quality (PEDro score < 6 points).
Study quality assessment
Two reviewers independently assessed the methodological features of each identified study using the Physiotherapy Evidence Database (PEDro) scale. This scale, a useful instrument for assessing the methodological quality of rehabilitation trials [20], measures the following factors: random allocation; concealed allocation; baseline similarity; blinding of subjects, therapists, and assessors; measures of key outcomes for > 85% of subjects; intention-to-treat analysis; between-group statistical comparisons; and point measures. The assessment consists of 10 scored yes-or-no questions worth 1 point each; the higher the score, the higher the quality of the study.
Data extraction
Two reviewers independently checked the title and abstract of each article to exclude irrelevant studies. The remaining full-text articles were evaluated for whether they met the inclusion and exclusion criteria. If a disagreement arose, a third reviewer participated in the discussion until a consensus was achieved. Finally, descriptive characteristics of the included articles were extracted as follows: study population, intervention performed (e.g., modality, movements, intensity, duration), and outcome measures. If a trial was multiple-arm RCT, we extracted data of relevant intervention groups. In addition, we contacted authors for missing values.
Statistical assessment
We used Review Manager (RevMan software version 5.2; Cochrane, London, UK) for meta-analysis. Pooled effects were estimated by weighted mean difference (WMD) or standardized mean difference (SMD) and a 95% confidence interval (CI) to compare the resistance training group with the control group. WMD was chosen to report the pooled effect of the same measurement method and unit, while SMD was chosen for comparing data across different measurement methods or units. We calculated results using a fixed-effects or random-effects model. Heterogeneity among studies was quantified via I2 statistic. I2 values of < 25%, 25–50%, and > 50% were considered to represent small, moderate, and large amounts of heterogeneity, respectively. The fixed-effect model was used when heterogeneity was small or moderate, while the random-effects model was adopted for highly heterogeneous studies. The level of significance was set at P < 0.05.
Results
Study selection
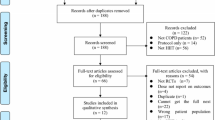
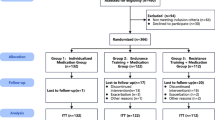
The initial search identified 4729 records from electronic databases, and 4 additional records were identified by manual searching. After screening for duplicate records, we included 3779 articles. Subsequent to title screening, 683 abstracts were screened and 641 were excluded. We identified 42 full-text articles as potentially relevant. Of which, we excluded 31 articles for having unextracted data, no relevant indicators, and/or PEDro score < 6 points. Ultimately, 11 articles met our inclusion criteria and were included in the systematic review and meta-analysis (Fig. 1).
Study characteristics
The characteristics of the included studies are summarized in Table 2. The final analysis included a total of 405 patients, 204 (50.3%) of whom received resistance training intervention. Their mean age was 58–70 years and their disease severity was moderate to severe. Nine studies included patients of both sexes and two studies included men only. Resistance training was performed on weight machine, free weights, and elastic bands. Four of the studies applied weight machine, another four studies applied free weights, and the other three studies applied elastic bands. Training movements were mainly concentrated on the upper and lower limbs. Four studies conducted both upper and lower limb training; four studies conducted upper limb training only; and the other three studies conducted lower limb training only. Exercise intensity ranged from 40% to 80% 1-repetition maximum (1RM), and duration (frequency) ranged from 6 to 12 weeks (3–5 times/week).In addition, for the control groups, four studies applied non-exercise interventions; three studies applied breathing exercises; two studies applied patient education; one study applied lower limb endurance and strength training; and one study applied limb flexibility and stretching exercises.
Quality assessment
The quality and domain scores for each study are presented individually in Table 3, with a mean value of 7. Four studies scored 6 points [21,22,23,24], four scored 7 points [25,26,27,28], two scored 8 points [29, 30], and one scored 9 points [31]. All RCTs reported random allocation, baseline similarity, group comparison, and point measures. Ten studies reported intention-to-treat analysis, nine reported measures of key outcomes for > 85% of subjects,and five reported concealed allocation. Eight studies reported assessor blinding, as well as common limitations related to subjects or therapist blinding. One study implemented blinding of subjects. None of the studies implemented blinding of therapists, due to the difficulty of such blinding in training studies.
Outcomes of resistance training
Functional exercise capacity assessment
Five studies assessed 6MWD [21, 23, 27, 28, 30] to measure the effects of resistance training on functional exercise capacity. Our meta-analysis results are presented as a forest plot in Fig. 2. They showed a significant improvement in 6MWD for patients in the resistance training group compared with the control group (WMD, 54.52; 95% CI 25.47–83.56; I2 = 43%; P = 0.14).
Endurance exercise capacity assessments
Three studies assessed endurance exercise capacity via 6PBRT [24, 30, 31]. Our meta-analysis results are presented as a forest plot in Fig. 3a. They showed a significant improvement in transfer number for patients in the resistance training group compared with the control group (WMD, 25.17; 95% CI 10.17–40.16; I2 = 0%; P = 0.55).
Three studies assessed endurance exercise capacity via CWRET [26, 29, 30]. Our meta-analysis results are presented as a forest plot in Fig. 3b. Comparisons between the resistance training group and the control group revealed no significant differences in exercise tolerance time (SMD, 0.43; 95% CI 0.00–0.86; I2 = 0%; P = 0.68).
Peak exercise capacity assessments
Three studies assessed peak exercise capacity via UULEX [29,30,31]. Our meta-analysis results are presented as a forest plot in Fig. 4a. They showed a significant improvement in exercise tolerance time for patients in the resistance training group compared with the control group (SMD, 0.41; 95% CI 0.03–0.79; I2 = 0%; P = 0.83).
Four studies assessed peak exercise capacity via CPET [22, 25, 26, 28]. Our meta-analysis results are presented as a forest plot in Fig. 4b. Comparisons between the resistance training group and the control group revealed no significant differences in peak oxygen uptake (SMD, 0.24; 95% CI − 0.16–0.63; I2 = 0%; P = 0.79).
Discussion
This study comprehensively explored the rehabilitative effect of resistance training on functional, endurance, and peak exercise capacities in patients with COPD. Pooled analysis revealed significant beneficial effects of such training on 6MWT, 6PBRT, and UULEX in COPD patients. These findings indicated that resistance training could be adopted to improve the functional, endurance, and maximum exercise capacity of people with COPD.
Effect of resistance training on functional exercise capacity
As an independent determinant of QOL in patients with COPD, the 6MWT showed a significant correlation with physical activity level, which is mainly used to reflect functional exercise capacity [18, 32]. Unlike the results of this study, Liao’s meta-analysis did not support that resistance training improved 6MWD in COPD patients. This inconsistency in results may be partially explained by increased sample size, and that patients who received endurance training were excluded from this study. Previous studies have shown a significant relationship between 6MWD and quadriceps strength in COPD patients [16] and found resistance training to be beneficial in improving such patients’ muscle strength and endurance [33]. Consistently, our meta-analysis showed that resistance training significantly improved 6MWD in COPD patients compared with the control group. Moreover, the increase of 54.52 m (95% CI 25.47–83.56) exceeded the minimum clinically important difference (MCID) of the 6MWD in chronic respiratory diseases of 33 m [19], which verified the contribution of resistance training to functional exercise capacity in patients with COPD. In addition, as emphysema and diffusing capacity of the lungs for carbon monoxide (DLCO) can predict the MCID of 6MWD reduction in patients with COPD [34], resistance training could be practicable for improving pulmonary ventilation and gas exchange dysfunction and for relieving dyspnea in these patients.
Effect of resistance training on endurance exercise capacity
The 6PBRT is often used to evaluate upper limb endurance exercise capacity in patients with COPD [12]. The test requires patients to transfer ten plastic rings from two shoulder-high pegs to two other pegs set 10 cm higher into the same board, and then transfer the rings back to the lower pegs [35]. Patients are required to repeatedly move as many rings as possible in 6 min [35]. Unlike the results of this study, McKeough’s meta-analysis did not support that resistance training improved 6PBRT scores in COPD patients. The inconsistent results may be partially explained by increased sample size and the fact that we excluded research [36] not meeting our test criteria. A previous study found a significantly positive relationship between the transfer number for the 6PBRT and physical activity that relies on the upper limbs, such as bathing, dressing, and preparing lunch [37]. Unsurprisingly, previous meta-analysis showed that unsupported upper limb exercise training increased 6PBRT transfer numbers [38]. The present meta-analysis included only studies that used resistance training as intervention for COPD patients and found consistent results. Therefore, it can be speculated that resistance training is conducive to maintaining these patients’ capacity for independence in daily life by effectively improving their upper limb endurance exercise capacity. During the test, thoracic muscles are passively stretched and the thoracic cavity expands which aggravate the diaphragmatic burden and cause severe excessive dynamic inflation [37]. In addition, resistance training for peripheral muscles has a therapeutic effect on respiratory muscles, reflected by improved forced vital capacity (FVC: 0.37) and maximum minute ventilation (3.77 L/min) [9]. Therefore, resistance training could improve upper limb endurance exercise capacity in COPD patients by alleviating excessive dynamic inflation.
As the disease progresses, the exercise tolerance time progressively decreases in COPD patients [39]. Longer exercise duration on the CWRET reflects muscles’ increased oxidative capacity and delayed metabolic acidosis [19]. A previous study has shown that increased exercise tolerance time is significantly associated with increased inspiratory capacity and decreased respiratory rate after endurance training [40]. In addition, non-invasive ventilation promotes a significant improvement in the exercise tolerance of COPD patients, accompanied by reduced electromyographic activity in respiratory muscles [41]. Our meta-analysis discovered a trend that resistance training increased the exercise time on the CWRET. However, the related mechanisms are still not clear and more studies are needed in the future.
Effect of resistance training on peak exercise capacity
The UULEX, one of the symptom-limited tests, requires subjects to repeatedly perform lifting tasks with their arms [42]. The exercise time can be used to reflect peak exercise capacity of COPD patients’ upper limbs [43]. Our meta-analysis showed that resistance training significantly increased exercise time in patients with COPD. In contrast, a previous meta-analysis showed that upper limb resistance training caused no improvement to UULEX exercise time in such patients [12]. These inconsistent results might be partially explained by differences in research interventions and measurement protocols and by increased sample size. Furthermore, we could not provide specific values for the increase in exercise time, and the SMD value was small. Therefore, more studies are needed to clarify the effects of resistance training on peak exercise capacity as evaluated by UULEX.
Peak VO2 can be used to measure peak exercise capacity, which is assessed via CPET. Our meta-analysis found that resistance training could not improve peak VO2 in patients with COPD, which was consistent with a previous study that also observed no significant increase in peak VO2 after resistance training for COPD patients [44]. However, another study showed that FEV1 is the most important predictor of peak VO2 in COPD patients after eliminating the influence of age and gender [16], and a meta-analysis found that resistance training significantly improved FEV1 in COPD patients [11]. Therefore, it can be speculated that peak VO2 improves after resistance training. However, a resistance training program targeted at improving peak VO2 in COPD patients should be further explored.
Recommended resistance training program for elderly COPD patients
Considering that there are no specific, well-defined prescriptions for resistance training targeted at improving the exercise capacity of COPD patients, we have summarized the RCTs included in this study to provide suggestions for applying resistance training in COPD rehabilitation. It can be applied with weight machines, free weights or elastic bands based on different training modes with different exercise intensities. Weight machines are mainly used for lower limb training, with exercise intensity at 50–80% 1RM. The advantages of weight machines are quantified intensity with progressive scheme, while their disadvantage is the requirement of professional exercise facilities. Free weights are mainly used for upper limb training, with exercise intensity generally at 50% 1RM, the load should increase when the targeted number of repetitions achieved. Such weights are simple to use and easy to obtain, and they tend to improve upper limb exercise capacity. Finally, elastic bands can be used for both upper and lower limb training, and the exercise intensity can be increased by changing the color of the band. Elastic bands are suitable for home-based training and beneficial to improving functional exercise capacity. However, the exercise intensity of elastic band training has not been quantified, and few studies have clarified a progressive scheme. In conclusion, the training mode should be selected according to the patient’s needs and existing resources. We specifically recommend a training program of three sets of 8–12 repetitions for each movement, 3 days/week, for at least 8 weeks.
Strengths and limitations
This study recruited high-quality RCTs (PEDro score ≥ 6 points) for meta-analysis to provide robust results. Such results were comprehensive, including not only function, endurance, and peak exercise capacity reflecting the overall state of COPD patients but also upper limb endurance and peak exercise capacity as they affected patients’ self-sufficiency. The results further clarified the role of resistance training in exercise capacity rehabilitation of COPD patients. The summary of the resistance training program could provide a reference for its application in improving the exercise capacity of COPD patients.
However, this study had some limitations. First, the interventional heterogeneity of training mode, movement, intensity, and duration might have affected the outcomes. Second, inconsistency in measurement protocols and results’ units, and unit conversion might have led to bias. Third, more than half of the included studies did not implement allocation concealment, and defects existed in blinding for therapists and patients. Fourth, there might have been a potential publication bias due to the small number of included studies. Finally, this study did not investigate the long-term effects of resistance training on exercise capacity in patients with COPD.
Conclusion
This meta-analysis confirmed that resistance training improved the functional exercise capacity of COPD patients. Our results showed that resistance training led to improvements in upper limb endurance and peak exercise capacity, compared with overall endurance and peak exercise capacity. However, larger, longer, multi-center RCTs are required to further determine the effectiveness of resistance training on exercise capacity in COPD patients.
References
Global Initiative for Chronic Obstructive Pulmonary Disease [homepage on the Internet] (2018) Global strategy for the Diagnosis, Management and Prevention of chronic obstructive pulmonary disease (2019 report). https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf. Accessed Apr 25 2018
Wang C, Xu J, Yang L et al (2018) Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet 391:1706–1717
Ramon MA, Gimeno-Santos E, Ferrer J et al (2014) Hospital admissions and exercise capacity decline in patients with COPD. Eur Respir J 43:1018–1027
Oga T, Nishimura K, Tsukino M et al (2003) Analysis of the factors related to mortality in chronic obstructive pulmonary disease: role of exercise capacity and health status. Am J Respir Crit Care Med 167:544–549
Oga T, Nishimura K, Tsukino M et al (2005) Exercise capacity deterioration in patients with COPD: longitudinal evaluation over 5 years. Chest 128:62–69
McCarthy B, Casey D, Devane D et al (2015) Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2:D3793
Spruit MA, Singh SJ, Garvey C et al (2013) An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 188:e13–e64
Wu W, Liu X, Li P et al (2018) Effect of Liuzijue exercise combined with elastic band resistance exercise on patients with COPD: a randomized controlled trial. Evid Based Complement Alternat Med 2018:2361962
Strasser B, Siebert U, Schobersberger W (2013) Effects of resistance training on respiratory function in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Sleep Breath 17:217–226
O’Shea SD, Taylor NF, Paratz JD (2009) Progressive resistance exercise improves muscle strength and may improve elements of performance of daily activities for people with COPD: a systematic review. Chest 136:1269–1283
Liao WH, Chen JW, Chen X et al (2015) Impact of resistance training in subjects with COPD: a systematic review and meta-analysis. Respir Care 60:1130–1145
McKeough ZJ, Velloso M, Lima VP et al (2016) Upper limb exercise training for COPD. Cochrane Database Syst Rev 11:011434
Kongsgaard M, Backer V, Jorgensen K et al (2004) Heavy resistance training increases muscle size, strength and physical function in elderly male COPD-patients–a pilot study. Respir Med 98:1000–1007
Santiworakul A, Jarungjitaree S, Jalayondeja W et al (2009) Effect of lower extremity exercise on muscle strength and physical capacity in COPD patients. J Med Assoc Thai 92:556–563
Wright PR, Heck H, Langenkamp H et al (2002) Influence of a resistance training on pulmonary function and performance measures of patients with COPD. Pneumologie 56:413–417
McNamara RJ, Houben-Wilke S, Franssen F et al (2018) Determinants of functional, peak and endurance exercise capacity in people with chronic obstructive pulmonary disease. Respir Med 138:81–87
Oga T, Nishimura K, Tsukino M et al (2002) Relationship between different indices of exercise capacity and clinical measures in patients with chronic obstructive pulmonary disease. Heart Lung 31:374–381
Singh SJ, Puhan MA, Andrianopoulos V et al (2014) An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J 44:1447–1478
Puente-Maestu L, Palange P, Casaburi R et al (2016) Use of exercise testing in the evaluation of interventional efficacy: an official ERS statement. Eur Respir J 47:429–460
Maher CG, Sherrington C, Herbert RD et al (2003) Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 83:713–721
Chen Y, Niu M, Zhang X et al (2018) Effects of home-based lower limb resistance training on muscle strength and functional status in stable chronic obstructive pulmonary disease patients. J Clin Nurs 27:e1022–e1037
Hoff J, Tjonna AE, Steinshamn S et al (2007) Maximal strength training of the legs in COPD: a therapy for mechanical inefficiency. Med Sci Sports Exerc 39:220–226
Silva C, Gomes NM, Saquetto MB et al (2018) Effects of upper limb resistance exercise on aerobic capacity, muscle strength, and quality of life in COPD patients: a randomized controlled trial. Clin Rehabil 32:1636–1644
Li YJ, Shi TY, Liu QG (2016) Effect of unsupported arm exercise on patients with chronic obstructive pulmonary disease. Zhongguo kang fu li lun yu shi jian 6:719–723 (in Chinese)
Calik-Kutukcu E, Arikan H, Saglam M et al (2017) Arm strength training improves activities of daily living and occupational performance in patients with COPD. Clin Respir J 11:820–832
Casaburi R, Bhasin S, Cosentino L et al (2004) Effects of testosterone and resistance training in men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 170:870–878
O’Shea SD, Taylor NF, Paratz JD (2007) A predominantly home-based progressive resistance exercise program increases knee extensor strength in the short-term in people with chronic obstructive pulmonary disease: a randomised controlled trial. Aust J Physiother 53:229–237
Zambom-Ferraresi F, Cebollero P, Gorostiaga EM et al (2015) Effects of combined resistance and endurance training versus resistance training alone on strength, exercise capacity, and quality of life in patients with COPD. J Cardiopulm Rehabil Prev 35:446–453
McKeough ZJ, Bye PT, Alison JA (2012) Arm exercise training in chronic obstructive pulmonary disease: a randomised controlled trial. Chron Respir Dis 9:153–162
Nyberg A, Lindstrom B, Rickenlund A et al (2015) Low-load/high-repetition elastic band resistance training in patients with COPD: a randomized, controlled, multicenter trial. Clin Respir J 9:278–288
Janaudis-Ferreira T, Hill K, Goldstein RS et al (2011) Resistance arm training in patients with COPD: a Randomized Controlled Trial. Chest 139:151–158
Durr S, Zogg S, Miedinger D et al (2014) Daily physical activity, functional capacity and quality of life in patients with COPD. COPD 11:689–696
De Brandt J, Spruit MA, Hansen D et al (2018) Changes in lower limb muscle function and muscle mass following exercise-based interventions in patients with chronic obstructive pulmonary disease: a review of the English-language literature. Chron Respir Dis 15:182–219
Diaz AA, Pinto-Plata V, Hernandez C et al (2015) Emphysema and DLCO predict a clinically important difference for 6MWD decline in COPD. Respir Med 109:882–889
Felisberto RM, de Barros CF, Nucci K et al (2018) Is the 6-minute pegboard and ring test valid to evaluate upper limb function in hospitalized patients with acute exacerbation of COPD? Int J Chron Obstruct Pulmon Dis 13:1663–1673
Ries AL, Ellis B, Hawkins RW (1988) Upper extremity exercise training in chronic obstructive pulmonary disease. Chest 93:688–692
Takeda K, Kawasaki Y, Yoshida K et al (2013) The 6-minute pegboard and ring test is correlated with upper extremity activity of daily living in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 8:347–351
Wang YN, Xu JL, Song HL et al (2017) The effects of unsupported arm exercise in patients with chronic obstructive pulmonary disease: a metaanalysis of randomized controlled trails. Zhonghua Hu Li Za Zhi 9:1077–1081 (in Chinese)
O’Donnell DE, Guenette JA, Maltais F et al (2012) Decline of resting inspiratory capacity in COPD: the impact on breathing pattern, dyspnea, and ventilatory capacity during exercise. Chest 141:753–762
Porszasz J, Emtner M, Goto S et al (2005) Exercise training decreases ventilatory requirements and exercise-induced hyperinflation at submaximal intensities in patients with COPD. Chest 128:2025–2034
Porszasz J, Cao R, Morishige R et al (2013) Physiologic effects of an ambulatory ventilation system in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 188:334–342
Janaudis-Ferreira T, Hill K, Goldstein RS et al (2013) Relationship and responsiveness of three upper-limb tests in patients with chronic obstructive pulmonary disease. Physiother Can 65:40–43
Janaudis-Ferreira T, Beauchamp MK, Goldstein RS et al (2012) How should we measure arm exercise capacity in patients with COPD? A systematic review. Chest 141:111–120
Spruit MA, Gosselink R, Troosters T et al (2002) Resistance versus endurance training in patients with COPD and peripheral muscle weakness. Eur Respir J 19:1072–1078
Funding
This systematic review was funded by national fitness project of General Administration of Sport of China (No. 2017B021), the “Qi Kang” young innovative talents project of School of Rehabilitation Medicine in Shanghai University of Traditional Chinese Medicine, the directed research grants from Science and Technology Commission of Shanghai Municipality (No. 18DZ1200600), and National Natural Science Foundation of China (No. 81902307).
Author information
Authors and Affiliations
Contributions
NL, PL: conception of the study and development of protocol. NL, YL, ZW participated in all stages of the study design, systematic literature view, statistical analyses and helped to draft the manuscript. JL, XL, WW contributed to the interpretation of data and revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This review does not contain any experiments involving human participants or animals performed by any authors.
Informed consent
For this review, informed consent forms were not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, N., Li, P., Lu, Y. et al. Effects of resistance training on exercise capacity in elderly patients with chronic obstructive pulmonary disease: a meta-analysis and systematic review. Aging Clin Exp Res 32, 1911–1922 (2020). https://doi.org/10.1007/s40520-019-01339-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01339-8