Abstract
Background
Vertebral fracture is often underdiagnosed. Patients with hip fracture may suffer from vertebral fracture without knowing it. The diagnosis of vertebral fracture is sometimes difficult because there is no consensus regarding the definition of osteoporotic vertebral fracture, and several indexes may be used to diagnose it and the concordance between several observers may not be optimal.
Objective
To study the concordance in the diagnosis of vertebral fracture done by three different doctors: an orthopedic surgeon, a radiologist, and a bone mineral metabolism expert.
Methods
A lateral thoracic-lumbar spine X-Ray was performed in 177 patients suffering from hip fracture to assess the presence or absence of vertebral fractures. Three different observers applied Genant’s criteria for it. Concordance between observers was measured using Cohen’s kappa coefficient.
Results
Patients suffering from hip fractures have undiagnosed vertebral fractures in a range that varies from 41.8 to 47.5 % depending on the observer. The concordance in the diagnosis of vertebral fractures is quite low, ranging a Cohen’s kappa coefficient from 0.43 to 0.55 and a percentage of concordance varying from 64 to 72 %. The best concordance was found between observers 1 and 3.
Discussion
Depending on the observer who made the diagnosis, the prevalence of previously undiagnosed vertebral fractures in patients with HF varied widely. We selected three different observers to assess the possible differences in the diagnosis of vertebral fractures among these patients and using the same method (Genant’s semi-quantitative assessment), surprisingly, there was little concordance among the three of them.
Conclusion
Patients with hip fracture have high prevalence of undiagnosed vertebral fractures. The diagnosis of these fractures varies widely depending on the observers and the Cohen’s kappa coefficient and percentage of concordance is rather low.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vertebral fracture (VF) is the osteoporotic fracture most frequent, although it prevalence varies widely depending on the population studied [1–3]. It is a potentially severe complication of osteoporosis because of acute and chronic back pain, impaired quality of life and increased mortality [4–7]. Vertebral body fractures result in pain and functional restrictions, and provoke a marked decrease in quality of life [5, 7, 8]. Therefore, early prevention of spinal fractures and accurate diagnosis and treatment are crucial. In clinical practice, osteoporotic VFs are usually identified by characteristic changes in vertebral shape on a lateral spine radiograph. For research consensus, VFs are defined by a reduction in anterior, middle, or posterior vertebral height, although the minimum required reduction (e.g., 15 or 20 % of vertebral height) varies among definition schemes [9]. Despite its common severity, and its value to predict further osteoporotic fracture, often VF is underdiagnosed [10].
Hip fracture (HF) is the most serious complication of osteoporosis. Patients suffering from HF have a high morbidity, mortality and a lower quality of life [7, 11–13]. There is a close relationship between previous VF and the incidence of new HF [14], but fewer studies have been performed about the prevalence of previously undiagnosed VF recognized at the moment of being admitted into a hospital due to a HF [15, 16].
We have performed this study in patients suffering from HF attended in an Orthopedic Ward on whom we have looked for previously undiagnosed VF, and the objective was to compare the concordance in the diagnosis of VF by three different observers: (1) an orthopedic surgeon, (2) a radiologist and (3) a bone mineral metabolism expert.
Materials and methods
The study was performed on 246 patients who were admitted into the Orthopedic Surgery Ward of the Hospital University Insular, Gran Canaria, Spain, suffering from a HF, from January 1, 2012 to December 31, 2012. We studied the prevalence of previously undiagnosed VF in these patients by performing an X-Ray study. 177 patients completed the study.
The patients were informed of the objectives of the study and their written consent was requested. For all subjects a questionnaire, previously validated and used in other similar clinical studies, was completed to gather clinical data on osteoporosis [17, 18]. A basic physical examination was also conducted. Lastly, a lateral thoracic-lumbar X-ray was carried out on the subjects.
All the X-rays were brought together and studied by three different observers: one was the Orthopedic Surgeon who attended most of the patients, another was a radiologist and the third was an expert on bone metabolic diseases. They were all instructed to use the Genant criteria for the diagnosis of VF [9]. According to this, the existence of vertebral deformity was stated when there was a reduction in the vertebral height higher than 20 %.
We excluded from the study those patients who where not living in the Canaries (mainly tourists), those who had a high-energy trauma and those suffering from cancer, with or without bone metastases (See flow chart, Fig. 1).
The data collected were entered into a database already set up in the statistical program SPSS (Statistical Package for the Social Sciences), for which we had the necessary legal licenses. For the analysis of the data, the Kolmogorov–Smirnoff test was applied to establish the goodness of fit to normality for the variables studied. For each group studied, the variables categorized were summarized in frequencies and percentages, and the numericals in averages and standard deviations.
Interobserver variation was measured by means of concordance, which was calculated in our study calculating the degree of agreement among several observers using the Kappa index, published by Cohen [19]. Cohen’s kappa coefficient is a statistical measure of inter-rater agreement or inter-annotator agreement [1] for qualitative (categorical) items. It is generally thought to be a more robust measure than simple percent agreement calculation, since κ takes into account the agreement occurring by chance. Applying this index, independent observers have a value = 0, while if the agreement is perfect, Kappa index reaches to 1.
Results
The flow chart of the study is shown in Fig. 1. From 246 patients who were admitted to the Orthopedic Ward because of a hip fracture, we excluded 69 because of different reasons. 177 patients completed the study, 108 women (61.1 %) and 69 men (38.9 %). Table 1 shows the characteristics of the population studied. The mean age of the whole patients was 78.6 ± 10.5 years old, 80.5 ± 8.8 years old for females and 75.5 ± 12.3 years old for males, p < 0.01. More than one third of the patients (34.1 %) had suffered from a previous fracture.
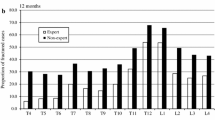
Table 2 shows the prevalence of vertebral fractures in the population studied depending on the observer. The differences vary from 41.8 %, observer 3 (Specialist in Bone Metabolic Diseases) to 47.5 %, observer 2 (Radiologist). Observer 1 (Orthopedic Surgeon) found a prevalence of 46.3 %, nearer to observer 2.
Table 3 shows the agreement found among these three different observers in the diagnosis of VF. The lowest concordance was found between observer 3 (Specialist in Bone Metabolic Diseases), compared to the other observers, 72.3 % in both cases, while the highest concordance was obtained between observer 1 (Orthopedic Surgeon) and observer 2 (Radiologist), 80.1 %.
Discussion
VF are the most frequent fragility fractures and its prevalence is thought to be 117 people per 100,000 in the general population [20], and the lifetime risk of spinal fracture in women over the age of 50 is about 15 % [21]. The data from the EVOS study have allowed a more precise assessment of radiographic vertebral fractures in a broad population.
Between the age of 75 and 89, the incidence of vertebral fractures is as high as 13.6 per 1000 inhabitants/year in men and 29.3 per 1000 people/year for women [1]. Recent studies indicate than the incidence of VF is even higher than previously described [2, 3, 7].
As a powerful predictor of future fracture risk, the identification of VF helps target individuals who will benefit from anti-fracture therapy, but this identification is problematic because: (a) “normal” radiological appearances in the spine vary greatly both among and within individuals; (b) “normal” vertebrae may exhibit misleading radiological appearances due to radiographic projection error; (c) “abnormal” appearances due to non-fracture deformities and normal variants are common, but it can be difficult to differentiate from true VF [22], and finally, (d) there is no consensus regarding the definition of osteoporotic VF [23].
Genant’s semi-quantitative assessment on standard radiographs may offer useful information about the severity and prognosis of osteoporosis and it is the standardized visual method for the diagnosis of vertebral fracture, commonly applied in research studies as a surrogate gold standard, based on its good reproducibility and ability to differentiate fractures from other deformities [23]. Underdiagnosis of vertebral fracture is a worldwide problem [10]. In a multicenter, multinational study, the authors assessed radiographic diagnoses of vertebral fracture in 2451 postmenopausal women with osteoporosis and comparison between local and central readings yielded a false-negative rate of 34 %.
Indeed, in patients suffering from HF, underdiagnosis of vertebral fracture is still a problem. Some studies performed to look for VF previously undiagnosed in different populations have shown high rates of VF, either in patients attended in primary care with chronic back pain [5], in outpatients attended at Internal Medicine [24], in patients with osteopenia [25] or in patients admitted in hospitals because of a HF [15].
In our study, depending on the observer who made the diagnosis, the prevalence of previously undiagnosed VF in patients with HF varied from 41.8 to 47.5 %. Irrespective of these differences, the figures are high enough to be a major cause of concern, since none of these patients had been diagnosed with VF or treated for this problem. Accordingly, we selected three different observers to assess the possible differences in the diagnosis of vertebral fractures among these patients. Actually, the same method was used, i.e., Genant’s semi-quantitative assessment [9]. Surprisingly, there was little concordance among the three of them. Cohen’s kappa coefficient varied from 0.432, the lowest, to 0.598, the highest, being the perfect concordance 1. Our results show that the diagnosis of VF may differ substantially depending on the observer who performs the study.
To avoid this variability, some other methods have been used; for example, DXA, when it is done for bone mineral density measurement, may also detect VF in asymptomatic patients [23]. Many other reports have stated that magnetic resonance imaging (MRI) has a high degree of accuracy for the definite diagnosis of incident spinal fracture, and it continues to be used as the most useful tool. However, due to limitations in access to the required equipment and considerations that must be given to the economics of medical treatments, it is not possible to use MRI with all patients [23, 26, 27].
Our results suggest that a gold standard for the diagnosis of VF is needed because, in some cases, one patient could be diagnosed with a vertebral fracture or not, depending on the physician who sees the X-Ray, and, certainly this situation should be avoided. The problem would be even bigger if instead of using a unique method for the diagnosis of vertebral fracture, Genant’s method, some other criteria were used [1, 28–32]. Then, the concordance would be even lower.
One limitation of the study is the lack of a gold standard to diagnose vertebral fracture, which would allow us to know which observer was nearer to the right diagnosis of vertebral fracture.
In conclusion, patients suffering from HF have a high prevalence of previously undiagnosed and untreated VF. There is a low concordance among three different observers; so further studies are required to look for a gold standard that allow to diagnose accurately VF.
References
O’Neill TW, Felsenberg D, Varlow J et al (1996) The prevalence of vertebral deformity in european men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11:1010–1018
Lambrinoudaki I, Flokatoula M, Armeni E et al (2015) Vertebral fracture prevalence among Greek healthy middle-aged postmenopausal women: association with demographics, anthropometric parameters, and bone mineral density. Spine J 15:86–94
Herrera A, Mateo J, Gil-Albarova J et al (2015) Prevalence of osteoporotic vertebral fracture in Spanish women over age 45. Maturitas 80:288–295
Jódar-Gimeno E (2010) Epidemiology of osteoporotic fractures. Mortality and morbidity. Rev Osteoporos Metab Miner 2:5–9
Nevitt MC, Ettinger B, Black DM et al (1998) The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128:793–800
Center JR, Nguyen TV, Schneider D et al (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Ratti C, Vulcano E, La Barbera G et al (2013) The incidence of fragility fractures in Italy. Aging Clin Exper Res 25(Suppl 1):S13–S14
Maggio D, Ruggiero C, Ercolani S et al (2010) A multi-dimensional questionnaire quantifying quality of life in elderly osteoporotic women: the Italian triple-Q osteoporosis study. Aging Clin Exper Res 22:330–339
Genant HK, Wu CY, van Kuijk C et al (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Delmas PD, van de Langerijt L, Watts NB et al (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 20:557–563
de Luise C, Brimacombe M, Pedersen L et al (2008) Comorbidity and mortality following hip fracture: a population-based cohort study. Aging Clin Exper Res 20:412–418
Maggi S, Siviero P, Gonnelli S et al (2011) The burden of previous fractures in hip fracture patients. The Break Study. Aging Clin Exper Res 23:183–186
Gonzalez-Rozas M, Perez-Castrillon JL, Gonzalez-Sagrado M et al (2012) Risk of mortality and predisposing factors after osteoporotic hip fracture: a 1-year follow-up study. Aging Clin Exper Res 24:181–187
Buckens CF, de Jong PA, Mali WP et al (2014) Prevalent vertebral fractures on chest CT: higher risk for future hip fracture. J Bone Miner Res 29:392–398
Sosa Henríquez M, Saavedra Santana P, y el grupo de trabajo en osteoporosis de la SEMI et al (2007) Prevalence of vertebral fractures in patients with hip fractures. Rev Clin Esp 207:464–468
Watt J, Cox L, Crilly RG (2015) Distribution of vertebral fractures varies among patients according to hip fracture type. Osteoporos Int 26:885–890. doi:10.1007/s00198-014-2887-y
Sosa M, Saavedra P, del Pino-Montes J et al (2005) Postmenopausal women with colles’ fracture have lower values of bone mineral density than controls as measured by quantitative ultrasound and densitometry. J Clin Densitom 8:430–435
Navarro Mdel C, Saavedra P, Gomez-de-Tejada MJ et al (2012) Discriminative ability of heel quantitative ultrasound in postmenopausal women with prevalent vertebral fractures: application of optimal threshold cutoff values using classification and regression tree models. Calcif Tissue Int 91:114–120
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Measur 20:37–46
Cooper C, Atkinson EJ, O’Fallon WM et al (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7:221–227
Dennison E, Cooper C (2000) Epidemiology of osteoporotic fractures. Hor Res 54(Suppl 1):58–63
Ferrar L, Jiang G, Adams J et al (2005) Identification of vertebral fractures: an update. Osteoporos Int 16:717–728
Grados F, Fechtenbaum J, Flipon E et al (2009) Radiographic methods for evaluating osteoporotic vertebral fractures. Joint Bone Spine 76:241–247
Sosa Henríquez M, Díaz Curiel M, Work Group in Osteoporosis of SEMI (GTO-SEMI) (2010) Prevalence of vertebral fractures in patients attending Internal Medicine outpatient clinics. Rev Osteoporos Metab Miner 2:9–13
Arboleya L, Diaz-Curiel M, Del Rio L et al (2010) Prevalence of vertebral fracture in postmenopausal women with lumbar osteopenia using MorphoXpress (R) (OSTEOXPRESS Study). Aging Clin Exper Res 22:419–426
Kishimoto H (2011) Calcium Pros and Cons-Which method is useful for diagnosis of vertebral body fracture; radiograph or MRI? Vertebral radiograph is the useful method for diagnosis and monitoring of vertebral body fractures. Clin Calcium 21:127–130
Nakano T (2011) Calcium Pros and Cons-Which method is useful for diagnosis of vertebral body fracture; radiograph or MRI? X-ray examination is not enough for diagnosis of fresh vertebral body fractures. Clin Calcium 21:131–135
McCloskey EV, Spector TD, Eyres KS et al (1993) The assessment of vertebral deformity: a method for use in population studies and clinical trials. Osteoporos Int 3:138–147
Minne HW, Leidig G, Wuster C et al (1988) A newly developed spine deformity index (SDI) to quantitate vertebral crush fractures in patients with osteoporosis. Bone Miner 3:335–349
Kleerekoper M, Nelson DA (1992) Vertebral fracture or vertebral deformity. Calcif Tissue Int 50:5–6
Davies KM, Recker RR, Heaney RP (1993) Revisable criteria for vertebral deformity. Osteoporos Int 3:265–270
Melton LJ 3rd (1997) Epidemiology of spinal osteoporosis. Spine 22:2S–11S
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Human and Animal Rights
The study was carried out with approval of the Committee on Medical Trials of the Hospital University Insular of Gran Canaria and was conducted according to standards derived from the Declaration of Helsinki.
Informed consent
A written inform consent was obtained from every patient.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sosa, M., Saavedra, P., Gómez-de-Tejada, MJ. et al. High prevalence of undiagnosed vertebral fractures in patients suffering from hip fracture at their hospital admission: weak concordance among observers. Aging Clin Exp Res 27, 835–839 (2015). https://doi.org/10.1007/s40520-015-0365-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0365-9