Abstract
The application of well-documented treatment concepts and improvements in digital technologies have changed modern prosthodontics, specifically for the design and manufacturing of fixed implant-supported prosthesis in edentulous patients to restore their quality of life. However, important factors such as inter-arch occlusal relationships, the need for a buccal flange, and the ability to perform a proper oral hygiene make the fixed restoration not the best treatment option for some edentulous patients, especially for the elderly. The treatment of old population with implant-supported prosthesis has become increasingly common, since life expectancy has been generally growing over time. This clinical report describes in a systematic sequence the diagnosis, treatment planning, and surgical-prosthetic management of an elderly systemically compromised patient who receives both maxillary and mandibular implant-supported rehabilitation following an innovative digital working method using novel CAD CAM millable materials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prosthetic rehabilitation of the severely compromised dentition possesses a true challenge for both the prosthodontist and his team. However, a clear understanding of the etiology, proper diagnosis, and meticulous design of a comprehensive treatment plan suited to the needs of each patient’s profile and the integration of evidence-based clinical and laboratory techniques along with an artistic philosophy can lead to positive results. The treatment of elderly patients with implant-supported prosthesis has become increasingly common, since life expectancy has generally growing over time [1]. Nevertheless, treating old population with dental implants requires a complete understanding about physiology of aging and its consequences such as physical and cognitive function, general health, their motivation, compliance, and their skills to adapt, manipulate, and clean different types of dental prosthesis [2].
The improvements in digital technology have allowed the introduction of new clinical protocols in order to improve the efficiency, safety, and predictability in the fabrication of dental restorations. Nowadays, a wide range of millable materials with excellent optical and mechanical properties are available, specially for the fabrication of implant-supported rehabilitations.
The following case report describes the sequence of a complete rehabilitation of an elderly female patient presenting with terminal dentition, a condition referred to subjects who are at the transition stage between natural dentition and edentulism [3], with implant-supported overdentures using novel millable CADCAM materials, following a specific digital/analogue method. According to the manufacturer (Zirkonzahn GmbH, Gais, Italy), this digital workflow, including innovative devices and software, is based on the synchronization and transmission of the digital and physical working basis in order to allow the prosthodontist and dental technician to combine virtual and analogue steps to benefit from the advantages of both work methods, resulting in high-quality masterpieces in terms of esthetics and accuracy.
Case Presentation
Phase I: Diagnosis and Treatment Planning
A 70-year-old woman with medical history of epilepsy controlled with medication presented with failing dentition. Her chief complaint concerned the unnatural and compromised esthetic appearance of her smile and difficulty with chewing all types of food and function.
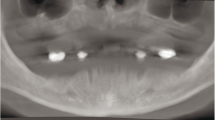
Clinical and radiographic analysis revealed terminal dentition due to stage IV periodontitis [4] (Figs. 1, 2, 3, 4, and 5). Based on the initial intraoral and extraoral clinical assessment, digital analysis, the patient’s functional/esthetic requirements, and financial aspects, a definitive interdisciplinary treatment planning was selected. Consequently, the proposed treatment plan was the extraction of all remaining teeth and the rehabilitation of both the maxillae and mandible with prostheses that the patient could remove and were easily to maintain. Therefore, implant-supported fixed/detachable overdentures were selected as final restorations.
Phase II: Pre-prosthetic Conditioning
This treatment stage consisted in a first surgical phase where extraction of all remaining teeth and fabrication of transitional complete dentures with soft relining material were performed (Figs. 6, 7, and 8).
In a 12-week healing period where bone remodeling occurs after teeth extraction, the patient’s habits were changed, and the virtual implant planning was started in order to continue the surgical and prosthetic treatment. The transitional dentures with the proposed esthetic and functional parameters were duplicated into clear radiographic guides with gutta-percha points that were placed in the potential implant sites. A radiography and cone beam computed tomography (CBCT) were performed and analyzed in order to corroborate the areas of interest with the bone availability and the prosthetic principles (Figs. 9 and 10). It was decided to perform a less invasive approach through the placement of four implants in the maxilla according to the All-on-four concept [5] avoiding sinus augmentation procedures and four inter-foraminal implants for the mandible placed in axially position.
Implant Placement
After local anesthesia, a crestal incision in the maxilla was performed slightly palatal to preserve the attached gingiva, and a full thickness flap was raised with the purpose of reducing the alveolar ridge to create an adequate platform assuring the vertical space required for the final prostheses. Following the osteotomy, four implants (RC BLT SLActive, Straumann® Basel, Switzerland) were placed (Figs. 11, 12, 13, and 14) and left with closure screws, and the primary wound closure was performed with a modified continuous sling suture using a non-resorbable PTFE monofilament suture material (Cytoplast, Osteogenics Biomedical, Lubbock, TX). The patient left with transitional complete dentures with soft relining material (Ufi Gel SC, Voco, Cuxhaven, Germany).
After 4 weeks, the second surgery consisting in the placement of 4 implants (Straumann BL SLActive, Straumann®) in the mandible located in inter-foraminal position was performed (Figs. 15, 16, 17, 18, 19, and 20).
The implants were left with closure screws for a two-phase submucosal healing, and a conventional loading protocol was selected in both the maxilla and mandible according to the ITI Consensus Statement on loading protocols for implant-supported overdentures in edentulous jaws [6] (Fig. 21).
After 12 weeks of healing, a second surgery was performed to uncover the implants and placing transmucosal abutments for the maxilla (SRA abutment, Straumann®) and conventional healing abutments in the mandible preserving the existing attached gingiva.
Prosthetic Phase
Virtual Planning and Data Acquisition
Four weeks after placement of transmucosal abutments, the prosthetic phase was initiated. The first step was to accurately transfer the implant 3D position from the patient to the laboratory. For this purpose, the authors considered a double-impression protocol as the most accurate technique. In this technique, scanbodies were connected and hand tightened to the implants (Scanbodies, Straumann) followed by the placement of resin CT scan markers (CT Markers, PDC Healthcare, Valencia, California) placed well distributed in the hard palate in order to serve as a common landmarks for accurate registration with an intraoral scanner (IOS). The first full arch digital impression with an intraoral scanner (Trios 3, 3 Shape, Copenhagen, Denmark) was gradually captured by scanning the soft tissues and the polymer scanbodies, viewing on the touchscreen during the scanning no part were missing. After the acquisition of digital impression, the digital volumes were exported as STL files and imported into the Zirkonzahn software (Figs. 22 and 23). Then, a rigid impression splint was designed in the software (Figs. 24 and 25) and wet milled (M1 Wet Milling Unit, Zirkonzahn) in slightly sintered cobalt-chrome blank material (Sintermetall, Zirkonzahn) (Figs. 26, 27, and 28) with the purpose of connecting each open tray impression coping with this metal splint using non-shrinking photopolymerizable gel (Triad gel, Dentsply, York, PA), and finally, a second analogue impression procedure with open tray technique using polyvinyl siloxane and customized impression tray was performed.
The master working models with artificial gum derived from the final impressions were obtained (Figs. 29, 30) using IV gypsum (Elite Rock, Zhermack, Badia Polesine, Italy). Afterwards, the next mandatory step after obtaining the working models in cases of multiple implants was to check the passivity and accuracy of the previous impressions through the fabrication of a stone verification jig as described in Figs. 31, 32, 33, 34, 35, 36, 37 and connection to the implants intraorally in the maxilla and mandible.
As stone does not flex, it will break if there is any discrepancy in the previous impression.
The Plane System
In order to register the patient’s reference planes and facial physiognomy, an innovative approach was used, the Plane System (Zirkonzahn). This system is composed of a tool for the detection of the patients physical planes (Plane Finder, Zirkonzahn), the PS1 physical and virtual articulator, and finally, an specific mounting plate to position the models in the physical articulator (Plane Positioner, Zirkonzahn). After confirming the accuracy of the working models with the stone verification jigs, the following step was the fabrication of wax rims (Figs. 38 and 39) and 3D digitization of the patient’s face, providing all the necessary information for planning the final restoration in a 3D environment using the 3D face scanner (Face Hunter, Zirkonzahn). The exact transfer of patient data into the software (Zirkonzahn software) represented the foundation for manufacturing individualized full-arch dental prosthesis, allowing the clinician to acquire the natural head position of the patient as well as the facial data in three dimensions (Figs. 40, 41, 42, and 43) and then were integrated into the virtual articulator (PS1 Articulator, Zirkonzahn) (Figs. 44, 45, and 46). The virtual articulator positioned the upper jaw according to the patient’s information recorded with the Plane Finder (Fig. 47).
With the objective of accurately transferring the maxillary model onto the physical articulator (PS1 Articulator, Zirkonzahn), a resin blank pattern (Jaw Positioner, Zirkonzahn) which represents the record of the maxillary wax rim (Fig. 48) was milled and placed into the articulator on top of the Plane Positioner (Figs. 49, 50, and 51). After fixing the maxillary model on the articulator, a maxillomandibular record was taken to the patient using a lower wax rim reproducing the VDO and final occlusion. At this point, the upper and lower models were correctly fixed on the physical articulator (Figs. 52 and 53) allowing the prosthodontist and dental technician to corroborate and perform any hand-made adjustment of the virtually planned and fabricated final restoration.
Fabrication of Final Prosthesis
Maxilla
The esthetic designed wax up was performed according to the incisal edge position previously determined in reference to the patient’s face (Figs. 54 and 55), and then STL files were created, providing the information for framework design for the maxillary overdenture. A CADCAM milled titanium friction bar with two additional stud type attachments (Equator, Rehin 8, Bolonia, Italy) was designed, milled in the M1 Wet Heavy Metal milling unit and refined (Figs. 56, 57, 58, 59, 60, and 61). A secondary structure (friction element) was milled in polyether ether ketone material (Tecno Med, Zirkonzahn) in a minimum thickness of 0.65 mm (Fig. 62 and 63) and then the final structure of the prosthesis consisting in an overdenture CADCAM base material milled out in ceramic reinforced PEEK (Tecno Med Mineral, Zirkonzahn), a biocompatible, high fracture resistance and stable material, with individual anatomic reduction to receive customized monolithic zirconia denture teeth (Figs. 64, 65, and 66). The final design of the customized denture teeth was in accordance with the digital wax up and milled in full monolithic pre-colored zirconia (Prettau 2 Dispersive, Zirkonzahn), allowing high translucency, excellent flexural strength, and natural color gradient (Figs. 67 and 68). After color infiltration and sinterization, the monolithic zirconia crowns were polished and cleaned for 10 min in an ultrasonic bath with detergent solution (Figs. 69, 70, 71, 72, and 73). The final characterization was completed using 3D extrinsic stains and fluorescent glaze (ICE Zirkon 3D stains, Zirkonzahn) (Figs. 74 and 75). Subsequently, the custom-designed denture teeth were bonded to the denture base using a 10-MDP based silane coupling agent (Clearfil Ceramic Primer Plus, Kuraray America, NY) and resin-based dual-cured adhesive cement (Panavia V5, Kuraray America).
The PEEK denture base material was sandblasted with 50 microns alumina particles, cleaned with compressed air, followed by the application of a laboratory dental adhesive (Visio.link, Bredent, Senden, Germany), and adhesive cementation of the zirconia crowns was performed (Fig. 76 and 77). Lastly, indirect pink veneering composite was used to reproduce the gingiva anatomy with a lifelike appearance (Gingiva-Composite, Zirkonzahn) (Figs. 78, 79, 80, and 81).
Mandible
The fabrication of the final prosthesis for the mandibular arch consisting in an implant-supported overdenture is described in Figs. 82, 83, 84, 85, 86, 87, 88, 89 and composed as follows: four monolithic zirconia telescopic crowns (ICE Zirkon Translucent, Zirkonzahn) on titanium bases (Variobase, Straumann), four PEEK friction copings (Tecno Med, Zirkonzahn), and lastly, predosed high impact resin was selected as overdenture base material with prefabricated acrylic denture teeth customized with layering composite.
The occlusion was verified and adjusted on the physical articulator (Fig. 90) to achieve a mutually protected occlusion. Final intraoral, extraoral, and radiographic views are shown in Figs. 91, 92, 93, 94, 95, and 96.
Conclusion
Periodontal disease was the main cause of the patient’s terminal dentition. However, before the implant therapy, the patient was submitted under strict plaque control and non-surgical periodontal treatment. Key to the success of this treatment was the clear understanding of the disease etiology, diagnosis, and the meticulously designed treatment planning according to the patient profile in conjunction with an artistic philosophy and digital approach.
References
Müller F, Barter S (2016) Implant therapy in the geriatric patient Vol 9 (in English). Berlin, Germany. Quintessence.
Mericske Stern RE, Taylor TD, Belser U. Management of the edentulous patient. Clin Oral Impl Res. 2000;11:108–25.
Salvi GE, Brown CE, Fujihashi K, Kiyono H, Smith FW, Beck JD, Offenbacher S. Inflammatory mediatorns of the terminal dentition in adult and early onset periodontitis. J Periodontal Res. 1998;33:212–25.
Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, Mealey BL, Papapanou PN, Sanz M, Tonetti MS. A new classification scheme for periodontal and peri-implant diseases and conditions - introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(Suppl 20):S1–8.
Maló P, Rangert B, Nobre M. All on four immediate function concept with Branemark system implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5:2–9.
Schimmel M, Srinivasan M, Herrmann F, Muller F. Loading protocols for implant-supported overdentures in the edentulous jaw: a systematic review and meta-analysis. In J Oral Maxillofac Implants. 2014;29:271–86.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Modern Production Laboratory Advances in Dental Technology
Rights and permissions
About this article
Cite this article
Sánchez, S.A., Balcazar, E. & Sánchez, E. Esthetic Rehabilitation in a Fully Edentulous Patient with Implant-Supported Overdentures Using Novel Digital Techniques and CAD/CAM Materials. Curr Oral Health Rep 8, 132–158 (2021). https://doi.org/10.1007/s40496-021-00300-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-021-00300-x