Abstract
Introduction
There is a dearth of evidence to document treatment of FMS-like tyrosine kinase 3 (FLT3)-mutated acute myeloid leukemia (AML) in real-world settings before the introduction of FLT3 inhibitors. A retrospective cohort study was conducted to understand treatment practices prior to the availability of FLT3 inhibitors in patients with FLT3-mutated AML from two registries in France.
Methods
Patient data from January 1, 2009 to December 31, 2017 were collected from the Hauts-de-France and Midi-Pyrénées registries. Patients aged ≥ 18 years at diagnosis with FLT3-mutated AML were included. Demographic and disease characteristics of patients with FLT3-mutated AML and relapsed or refractory (R/R) FLT3-mutated AML were documented. Treatment regimens, overall survival (OS), and event-free survival were assessed in patients with R/R FLT3-mutated AML who did not participate in clinical trials.
Results
Overall, 819 and 1244 adult patients with AML from the Midi-Pyrénées and Hauts-de-France cohorts, respectively, underwent FLT3 mutation testing; 172 (21.0%) and 263 (21.1%) patients, respectively, had a FLT3 mutation. Primary R/R status was identified in 41.3% (n = 71/172) of the Midi-Pyrénées and 34.6% (n = 91/263) of the Hauts-de-France cohorts. Before R/R AML diagnosis, 82.0% and 97.5% of patients in the Midi-Pyrénées and Hauts-de-France cohorts, respectively, achieved complete remission (CR) or CR with incomplete hematologic recovery (CRi) following induction chemotherapy; after diagnosis of R/R AML, CR/CRi rates with salvage therapy were 33.3% and 28.1%, respectively. Median OS (interquartile range) in patients receiving salvage therapy (n = 49, n = 78) was 5.2 (2.3–11.1) and 6.1 (2.5–35.2) months, in the Midi-Pyrénées and Hauts-de-France cohorts, respectively. Across both cohorts, patients with R/R FLT3-mutated AML had low rates of CR/CRi with salvage therapy and a median OS of approximately 6 months.
Conclusion
Before FLT3 inhibitor availability, real-world treatment patterns and outcomes in French patients with R/R FLT3-mutated AML were consistent with clinical trial data, highlighting a poor prognosis and unmet need for effective treatment.
Plain Language Summary
Acute myeloid leukemia is a cancer affecting the blood and bone marrow. The presence of specific mutations in the FMS-like tyrosine kinase 3 (FLT3) gene in patients with acute myeloid leukemia can negatively impact response to standard chemotherapy. Patients with these mutations may not respond to chemotherapy or have a shortened duration of response causing a return of the disease, which in turn substantially decreases their life span. In the era prior to the availability of drugs specifically designed to counteract the negative effects of FLT3 mutations, evidence related to patient characteristics and treatment effects in individuals with acute myeloid leukemia harboring FLT3 mutations was mainly derived from clinical studies, with little evidence based on real-world experience. To better understand real-world patient characteristics and treatment effects in patients with acute myeloid leukemia and FLT3 mutations, we analyzed patients from two French registries, Midi-Pyrénées and Hauts-de-France, with a focus on patients who did not respond to or whose disease returned after initial chemotherapy. Patient data from between January 2009 and December 2017 included patients with FLT3-mutated acute myeloid leukemia from Midi-Pyrénées and Hauts-de-France who did not respond to or had recurrent disease after responding to initial chemotherapy, had low response to salvage chemotherapy, and a survival duration of 6 months or less. Our real-world observations in patients with relapsed or refractory FLT3-mutated acute myeloid leukemia from these two registries were consistent with results reported in clinical trials. Our results highlight the bleak forecast for these patients in the absence of effective drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The presence of FMS-like tyrosine kinase 3 (FLT3) mutations in patients with acute myeloid leukemia (AML) confers a poor prognosis in the absence of targeted FLT3 inhibitor therapy; however, there is a paucity of real-world evidence on patients with FLT3-mutated AML. |
A real-world French registry-based analysis was conducted to evaluate patient characteristics, treatment patterns, and outcomes in real-world clinical settings. |
What was learned from this study? |
Patients with relapsed or refractory (R/R) FLT3-mutated AML in this real-world French registry-based analysis demonstrated demographic, disease, and treatment characteristics consistent with those established for AML. |
Consistent with findings reported in the literature, development of R/R disease was associated with worsening remission rates and overall survival. |
These findings highlight the poor prognosis associated with R/R FLT3-mutated AML prior to the availability of FLT3 inhibitor therapy. |
Introduction
Acute myeloid leukemia (AML) is a rare malignant hematologic disease characterized by excess myeloblasts in bone marrow and blood [1]. In France, AML accounts for 10% of all hematological malignancies with an overall incidence of 3428 per year [2] and an age-adjusted incidence of 2.3/100,000 person-years (PY) in women and 3.1/100,000 PY in men [2]. The main risk factors for AML are advanced age, history of hematologic disease, genetic mutations, radiation exposure, viruses, chemical hazards, and chemotherapy treatments [3].
FMS-like tyrosine kinase 3 (FLT3) is a cytokine receptor kinase expressed in early hematopoietic stem and progenitor cells [4]. The FLT3 receptor pathway plays an important role in cell proliferation, survival and differentiation. Mutations in the FLT3 gene are one of the most common mutations in patients with AML. Approximately 30% of patients with AML harbor an activating FLT3 mutation [5], which may lead to uncontrolled cell proliferation by constitutive activation of the FLT3 gene [6, 7]. Such mutations consist of internal tandem duplication (ITD) mutations that occur in approximately 25% of patients and tyrosine kinase domain (TKD) point mutations that occur in around 5–10% of patients [5]. A high FLT3-ITD allelic ratio is associated with early relapse and short disease-free and overall survival (OS) after standard chemotherapy [8, 9]. The impact of FLT3-TKD mutations on AML prognosis is less clear; however, evidence suggests that in the absence of NPM1 mutations, FLT3-TKD mutations may have a negative impact on OS and event-free survival (EFS) [10].
Initial assessments of patients with AML determine whether the patient is eligible for intensive induction chemotherapy, which carries a risk of treatment-related mortality [11]. Elderly patients have a poor prognosis with standard chemotherapy, with 70% of patients aged ≥ 65 years not surviving beyond 1 year after AML diagnosis [12]. Prior to the availability of targeted therapies, patients with AML who were resistant to, or had relapsed after achieving initial remission with, standard induction chemotherapy had extremely limited treatment options; salvage chemotherapy regimens were largely ineffective in this population [13]. As such, in 2017 the European LeukemiaNet (ELN) deemed that no specific salvage regimen could be considered standard of care for relapsed or refractory (R/R) AML [14].
Midostaurin was the first FLT3 inhibitor approved for the treatment of FLT3-mutated AML on the basis of findings from the phase 3 RATIFY trial, which demonstrated that midostaurin combined with chemotherapy improved survival in newly diagnosed patients with FLT3-mutated AML [15, 16]. Although first-generation FLT3 inhibitors such as midostaurin were largely nonspecific, subsequently developed second-generation inhibitors (i.e., quizartinib and gilteritinib) had greater FLT3 receptor specificity, were more potent inhibitors of the FLT3 receptor, and demonstrated efficacy and safety in patients with R/R AML [17, 18]. Preclinical studies demonstrated that quizartinib effectively inhibited FLT3 receptor activity in FLT3-ITD-positive tumor xenograft models and primary AML cells [19]. In patients with FLT3-ITD-positive R/R AML, quizartinib improved OS compared with salvage chemotherapy [17]. Gilteritinib inhibits FLT3 receptor activity in cell lines harboring FLT3-ITD or FLT3-TKD mutations [20]. The phase 3 ADMIRAL study compared gilteritinib with salvage chemotherapy in patients with R/R FLT3-mutated AML. Median OS was significantly longer in patients treated with gilteritinib than in those treated with standard salvage chemotherapy (9.3 vs 5.6 months; hazard ratio for death, 0.64; 95% confidence interval, 0.49–0.83; p < 0.001) [18].
Most data related to patients with FLT3-mutated R/R AML are derived from clinical trials and few studies are designed to evaluate the AML treatment landscape in real-world settings. There is a paucity of information related to real-world outcomes prior to the availability of FLT3-targeted therapies for patients with FLT3-mutated R/R AML. The aim of the present study was to review data from two French registries to assess characteristics, treatment patterns, and outcomes of real-world patients with AML before the availability of FLT3 inhibitors.
Methods
Statement of Ethics
This study was conducted in adherence to the study protocol and the ethical principles of the Declaration of Helsinki, Commission Nationale de l’Informatique et des Libertés (CNIL) reference methodology MR-004, and any applicable regulations. Because this was a registry-based retrospective study, approval from an ethics review board was not required. Patient consent for the general use of data from the Midi-Pyrénées and Hauts-de-France registries was approved by the CNIL, and permission was obtained from the registry owners to use the information from the data repository for the purpose of this study.
Study Design and Patients
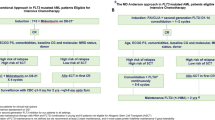
This retrospective cohort study was conducted using data collected from two French AML registries, Hauts-de-France and Midi-Pyrénées, from January 1, 2009 to December 31, 2017. Out of all AML registries in France, the Hauts-de-France and Midi-Pyrénées registries were specifically selected because they provided the best quality and most complete data sets, which (following a structured feasibility assessment) were in line with our objectives.
Patients included in the study met the following criteria: date of diagnosis of AML recorded in the database within the study period; at least 18 years of age on the date of AML diagnosis; and documented FLT3 mutation testing during the study period. Patients were excluded if they had a French-American-British code M3 (acute promyelocytic leukemia). The index date was defined as the date a patient acquired primary R/R status.
Objectives
The objectives of this study were to describe (1) the proportion of patients with AML who harbored a FLT3 mutation at any time and the proportion of patients with FLT3-mutated AML who became R/R at any time; (2) the demographic, clinical, and treatment characteristics of patients with R/R FLT3-mutated AML at the time of diagnosis and at the time when primary R/R status (index date) was achieved; (3) treatment regimens from index date until end of follow-up (e.g., treatment sequence, response to treatment, and rate of hematopoietic stem cell transplantation [HSCT]) in patients with R/R FLT3-mutated AML not participating in clinical trials; (4) OS in patients with R/R FLT3-mutated AML (stratified by participation in a clinical trial or treatment with HSCT) from the index date; and (5) EFS in patients with R/R FLT3-mutated AML (Midi-Pyrénées cohort only; stratified by participation in a clinical trial) from the index date.
Data Sources and Variables
The Midi-Pyrénées registry was launched in the year 2000. Comorbidity data in this registry were collected only in patients aged 60 years or older, and data on healthcare resource utilization (HRU) were not systematically collected. The Hauts-de-France registry was launched in 2008 in Lille and nine additional hospitals in the Hauts-de-France region were incorporated in 2009. This registry does not include data on HRU, and data related to comorbidities and elderly patients ineligible for induction chemotherapy are limited.
The following variables were extracted from the two registries to meet the objectives of the study: patient age, FLT3 mutation status, primary R/R status, and index date (objective 1); patient demographics, characteristics of AML disease, clinical characteristics, and treatment characteristics (objective 2); participation in a clinical trial, salvage therapy, treatment response, HSCT and time to HSCT, date of death, and OS (objective 3); date of death and OS from index date until the end of the follow-up (objective 4); date of event and EFS from the index date until the date of documented relapse, treatment failure, or death from any cause (objective 5).
Response Definitions
Treatment response was defined as the achievement of complete remission or complete remission with incomplete hematologic recovery (CR/CRi). First relapse was defined as hematologic relapse after achieving CR/CRi with first-line treatment. In the Midi-Pyrénées registry, primary refractory AML was defined as an absence of CR after one cycle of intensive induction therapy, excluding death from aplasia or an undetermined cause. In the Hauts-de-France registry, primary refractory AML was defined as an absence of CR after one cycle of induction chemotherapy and one cycle of first-line salvage chemotherapy, excluding death from aplasia or an undetermined cause.
OS was defined as the time from the index date to the date of death or censored event (loss to follow-up or end of study period). EFS was defined as the time from the index date to the date of documented relapse, treatment failure, or death due to any cause during the study period. Patients who were lost to follow-up were censored at the date of loss of follow-up or the end of the study period, whichever came first.
Data Analysis
As a result of the variation in patient profiles between the two registries, data were analyzed separately for the Midi-Pyrénées and Hauts-de-France cohorts. Demographic characteristics, treatment regimens, and response rates were reported as frequency and percentage. Median OS and EFS and associated interquartile ranges (IQR) were estimated using the Kaplan–Meier method. For patients with R/R FLT3-mutated AML, OS was stratified according to whether patients had participated in clinical trials and by HSCT status. Statistical analyses were descriptive, and no hypothesis testing was performed.
Results
Proportion of Patients with AML and FLT3 Mutations
Overall, 819 of the 2282 patients (35.9%) diagnosed with AML from the Midi-Pyrénées registry and 1244 of the 1953 patients (63.7%) diagnosed with AML from the Hauts-de-France registry were eligible for inclusion in the study (Table 1). In the Midi-Pyrénées and Hauts-de-France cohorts, 172 (21.0%) and 263 (21.1%) of the eligible patients, respectively, had a documented FLT3 mutation (Table 1). A total of 71 patients in the Midi-Pyrénées cohort and 91 in the Hauts-de-France cohort had documented R/R AML; 61 (85.9%) and 81 (89.0%) of these patients, respectively, acquired R/R status with an index date on or before December 31, 2017.
Demographic and Clinical Characteristics of Patients with FLT3-Mutated R/R AML
Midi-Pyrénées Cohort
The median age at AML diagnosis was 61.0 years; the median age at the index date was 61.7 years. Most patients were female (54.1%) with de novo AML (82.0%) and intermediate 1 cytogenetic risk status (78.7%) (ELN 2010 criteria) (Table 2). Proportions of patients with an Eastern Cooperative Oncology Group (ECOG) performance status < 2 were similar at the time of diagnosis (62.3%) and at the index date (59.0%). Comorbidity data were available for 32 (52.5%) patients aged 60 years or older at the time of diagnosis. The most common comorbidities were high blood pressure (37.5%), history of cardiovascular disease (34.4%), diabetes (12.5%), and history of cancer (12.5%); almost two-thirds (65.6%) of these patients had a Charlson Comorbidity Index score of 0.
Hauts-de-France Cohort
The median age was 55.7 years at the time of AML diagnosis and 56.9 years at the index date (Table 2). Most patients were female (56.8%) with de novo AML (92.6%). Data related to ECOG performance status at the date of diagnosis were missing for most patients (70.4%).
Treatments Before Acquiring R/R Status and Outcomes
Midi-Pyrénées Cohort
Of the 61 patients with FLT3-mutated R/R AML, most received intensive induction chemotherapy with idarubicin–cytarabine combination regimens: 20 patients (32.8%) received an idarubicin–cytarabine combination regimen and 24 (39.3%) received an idarubicin–cytarabine–lomustine combination regimen. A daunorubicin–cytarabine combination regimen was administered in 13 (21.3%) patients (Table 2). In addition to intensive chemotherapy, 40 (65.6%) patients received hydroxyurea and 24 (39.3%) received dexamethasone before the index date.
Achievement of CR/CRi with induction chemotherapy before the index date was reported in 50 (82.0%) patients; 11 (18.0%) of these patients also received allogeneic HSCT before the index date. One patient (1.6%) received autologous HSCT before the index date but did not achieve CR/CRi.
Hauts-de-France Cohort
Among the 71 patients with R/R FLT3-mutated AML, the most common induction chemotherapy regimens were idarubicin–cytarabine–lomustine (n = 45, 55.6%) and daunorubicin–cytarabine (n = 29, 35.8%) (Table 2). Idarubicin–cytarabine (n = 7, 8.6%) and other types of induction chemotherapy were administered in the setting of clinical trials for 45 (55.6%) patients (Table 2); 28 (62.2%) of these 45 patients received daunorubicin–cytarabine combination regimens either in the comparator or in the interventional arm. In addition to intensive chemotherapy, hydroxyurea was administered in 20 (24.7%) patients before the index date.
Most patients (n = 79, 97.5%) achieved CR/CRi before the index date, including 76 (93.8%) patients who achieved CR. Of the 79 patients who achieved CR/CRi after intensive induction chemotherapy, 13 (16.0%) also received allogeneic HSCT before the index date. Most patients (n = 66, 81.5%) received consolidation therapy, most frequently with high-dose cytarabine (n = 34/66, 51.5%).
Eight patients received salvage therapy as first-line therapy; seven of these patients received high-dose cytarabine (high-dose cytarabine plus amsacrine, n = 5; high-dose cytarabine plus anthracycline, n = 1; high-dose cytarabine, n = 1).
Treatments After the Index Date and Outcomes
Midi-Pyrénées Cohort
Of the 42 patients with R/R FLT3-mutated AML who did not participate in a clinical trial, 31 (73.8%) received salvage therapy after the index date (Table 3). Salvage treatments were highly variable with six patients receiving high-dose cytarabine, two patients receiving anthracycline plus cytarabine, and the remaining 21 patients receiving a range of other therapies. Data related to allogeneic HSCT after acquiring primary R/R status were missing for most patients (78.6%) (Table 3). Eight patients received allogeneic HSCT after reaching primary R/R status and the median time to allogeneic HSCT in these patients was 4.0 months after the index date. Information on autologous HSCT treatment after the index date was missing for all patients.
Fourteen of the 42 patients (33.3%) achieved CR/CRi after salvage therapy (Table 3). Five of these 14 patients achieved CR, salvage therapy failed in 10 (23.8%) patients, and data were missing for 18 (42.9%) patients.
Hauts-de-France Cohort
Of the 32 patients with R/R FLT3-mutated AML who did not participate in a clinical trial, 31 (96.9%) received post-index therapy, which included palliative care (n = 9), amsacrine plus cytarabine (n = 8), demethylating agents (n = 6), high-dose cytarabine (n = 2), intensive chemotherapy plus gemtuzumab ozogamicin (n = 2), fludarabine plus high-dose cytarabine plus novantrone (n = 1), and others (n = 3). Nine (28.1%) patients received allogeneic HSCT after the index date, and the median time to allogeneic HSCT in these patients was 3.5 months after the index date. Nine (28.1%) patients achieved CR/CRi after salvage treatment and treatment failure was reported in 22 (68.8%) patients (Table 3).
OS After the Index Date
Midi-Pyrénées Cohort
Of the 49 patients with R/R FLT3-mutated AML who were analyzed for OS, 38 (77.6%) died after the index date. The median survival time was 5.2 (IQR 2.3–11.1) months (Fig. 1). Twenty-five (80.6%) of the 31 patients who did not participate in a clinical trial and 13 (72.2%) of the 18 patients who participated in a trial had died; median OS was 4.9 (IQR 1.5–9.4) months and 6.4 (IQR 2.6–17.3) months, respectively.
Ten (90.9%) of the 11 patients who received HSCT and 28 (73.7%) of the 38 patients who did not receive HSCT had died; median OS was 7.6 (IQR 2.7–12.9) months and 4.9 (IQR 1.6–9.9) months, respectively.
Hauts-de-France Cohort
Of the 78 patients with R/R FLT3-mutated AML who were analyzed for OS, 54 (69.2%) patients died after the index date; median OS was 6.1 (IQR 2.5–35.2) months (Fig. 2). Twenty-four (75.0%) of 32 patients who did not participate in a clinical trial and 40 (87.0%) of 46 patients who participated in a trial had died; median OS was 3.8 (IQR 2.1–21.9) months and 7.5 (IQR 3.6–NA) months, respectively.
Twenty-four (36.9%) of 65 patients who did not receive HSCT and 10 (76.9%) of 13 patients who received HSCT had died; median OS was 7.0 (IQR 2.4–35.2) months and 6.1 (IQR 3.6–18.5) months, respectively.
EFS After Index Date
Analysis of EFS was limited to the Midi-Pyrénées cohort. Of the 49 patients with R/R FLT3-mutated AML who were analyzed for EFS, 40 (81.6%) experienced an event after the index date; median EFS was 2.3 (IQR 1.5–7.0) months (Fig. 3). Overall, 18 of the 49 patients had participated in a clinical trial and 31 had not; respective numbers of patients who experienced an event were 26 (83.9%) and 14 (77.8%), respectively, and corresponding median EFS was 2.7 (IQR 1.0–6.8) months and 2.0 (IQR 1.6–12.9) months, respectively.
Discussion
Across both the Midi-Pyrénées and Hauts-de-France cohorts, approximately 21% of adult patients diagnosed with AML harbored a FLT3 mutation. These percentages were slightly lower than those reported in the literature (approx. 30%) for patients with newly diagnosed AML [5]. The percentages of patients with FLT3 mutations may have been underestimated in our study because not all patients with AML were systematically tested for FLT3 mutations, despite ELN recommendations to do so. For example, patients who were allocated to receive supportive or palliative care were usually not tested for FLT3 mutations [5].
The percentages of FLT3-mutated patients who acquired R/R status were 41.3% in the Midi-Pyrénées cohort and 34.6% in the Hauts-de-France cohort. Other studies reported higher rates of R/R AML ranging from approximately 40% to 60% [8, 21]. The lower incidence of R/R AML reported in the current study may be partly explained by the more stringent definition of refractory disease in the Hauts-de-France cohort, where patients with refractory AML were defined as those who failed both induction chemotherapy and first-line salvage chemotherapy.
Median ages at diagnosis of patients with FLT3-mutated R/R AML in the Midi-Pyrénées and Hauts-de-France cohorts (61.0 and 55.7 years, respectively) were lower than the median age reported in the literature which is generally over 65 years [21]. Elderly patients with AML are less likely to receive induction chemotherapy because of the increased risk of toxicity and a poorer overall prognosis [21]. Since most patients in both cohorts received induction chemotherapy, they may be younger and healthier than the overall AML population. Notably, the rates of CR/CRi after induction chemotherapy (82.0% and 97.5%) in both registry cohorts were high, reflecting outcomes typically observed in younger adult patients [22].
In the Hauts-de-France cohort, induction chemotherapy with the daunorubicin–cytarabine combination regimen was commonly prescribed (35.8%), which was expected because it remains the standard of care for induction therapy [14]. Of the 45 patients in the Hauts-de-France cohort who received induction chemotherapy in clinical trials, 28 received daunorubicin–cytarabine combination regimens. In the Midi-Pyrénées cohort, daunorubicin–cytarabine (21.3%), idarubicin–cytarabine (32.8%), and idarubicin–cytarabine–lomustine (39.3%) combinations were commonly prescribed. Induction chemotherapy regimens were largely consistent with ELN recommendations [14].
As noted in the ELN guidelines, no specific salvage therapy has emerged as standard treatment for R/R AML [14]. In the Midi-Pyrénées cohort, 33.3% of patients achieved CR/CRi after salvage therapy (CR, 11.9%; CRi, 21.4%). In the Hauts-de-France cohort, 28.1% of patients achieved CR/CRi. Overall, observed remission rates were similar to those reported in adult patients with R/R AML who received salvage therapy (20–30%) [14].
For patients who received salvage therapy, the median OS from the index date was 5.2 months (IQR 2.3–11.1) in the Midi-Pyrénées cohort and 6.1 months (IQR 2.5–35.2) in the Hauts-de-France cohort. Data from the literature reported a comparable OS after relapse (6–8 months) for patients receiving conventional salvage chemotherapy after acquiring R/R status [12, 21]. For patients who received post-index treatment, the median EFS from the index date was 2.3 months (IQR 1.5–7.0).
The study has the typical limitations of a retrospective study with possible unknown selection biases. Clinical practices of hospitals covered by these registries may differ from those outside. Contributing hospitals may be often located in large cities and affiliated with universities, and may more frequently administer experimental treatments. In addition, the small sample size limits extrapolation of the results to the larger French AML population. As such, any differences in survival outcomes between stratified subgroups (participated or did not participate in a clinical trial; received or did not receive HSCT) should be interpreted with caution because of the small size of the strata sample. Not all variables of interest were directly recorded in the registries, and some were derived from available data (e.g., refractory date and date of treatment failure). Although derived variables may have induced biases because they were based on certain assumptions, they provided access to data otherwise unavailable. Information related to comorbidities was limited; it was not recorded in the Hauts-de-France cohort or recorded only for patients aged over 60 years in the Midi-Pyrénées cohort. Factors such as ethnicity, smoking, and chemical exposure can impact AML disease profile and treatment response [3]; however, these data were not systematically recorded in either registry. Despite these limitations, findings from this analysis provide valuable insight into real-world treatment practices in patients with R/R FLT3-mutated AML prior to the availability of FLT3-targeted therapies. We observed poor response and survival outcomes with existing salvage chemotherapy regimens in this historical population, which concurs with evidence reported in clinical trials during the same period.
Conclusion
In the era prior to the availability of FLT3-targeted therapy, real-world results in patients with AML and R/R FLT3-mutated AML from two French registries reflect pre-established demographic and disease characteristics and treatment reflected the recommended standard of care for induction chemotherapy. After patients acquired R/R status, remission rates worsened and OS was reduced to less than 6 months, which was consistent with previously reported findings. This study provides an insightful first look at real-world treatment practices and outcomes in a FLT3-mutated AML population and underlines the dismal prognosis of patients with R/R FLT3-mutated AML in the absence of FLT3-targeted therapy.
References
Short NJ, Rytting ME, Cortes JE. Acute myeloid leukaemia. Lancet. 2018;392(10147):593–606.
Le Guyader-Peyrou S, Defossez G, Dantony E et al. National estimates of cancer incidence and mortality in metropolitan France between 1990 and 2018. Volume 2 - malignant haemopathies. Study from cancer registers of the Francim network. Saint-Maurice (Fra): Public Health France, 2019. 169 p. https://www.registre-cancers-44-85.fr/recherche-epidemiologique/nos-dernieres-publications/. Accessed 19 July 2023.
Döhner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015;373(12):1136–52.
Small D, Levenstein M, Kim E, et al. STK-1, the human homolog of Flk-2/Flt-3, is selectively expressed in CD34+ human bone marrow cells and is involved in the proliferation of early progenitor/stem cells. Proc Natl Acad Sci U S A. 1994;91(2):459–63.
Daver N, Schlenk RF, Russell NH, Levis MJ. Targeting FLT3 mutations in AML: review of current knowledge and evidence. Leukemia. 2019;33(2):299–312.
Yanada M, Matsuo K, Suzuki T, Kiyoi H, Naoe T. Prognostic significance of FLT3 internal tandem duplication and tyrosine kinase domain mutations for acute myeloid leukemia: a meta-analysis. Leukemia. 2005;19(8):1345–9.
Frohling S, Scholl C, Levine RL, et al. Identification of driver and passenger mutations of FLT3 by high-throughput DNA sequence analysis and functional assessment of candidate alleles. Cancer Cell. 2007;12(6):501–13.
Kottaridis PD, Gale RE, Frew ME, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98(6):1752–9.
Thiede C, Steudel C, Mohr B, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99(12):4326–35.
Bacher U, Haferlach C, Kern W, Haferlach T, Schnittger S. Prognostic relevance of FLT3-TKD mutations in AML: the combination matters–an analysis of 3082 patients. Blood. 2008;111(5):2527–37.
Cheson BD, Bennett JM, Kopecky KJ, et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol. 2003;21(24):4642–9.
Megias-Vericat JE, Martinez-Cuadron D, Sanz MA, Montesinos P. Salvage regimens using conventional chemotherapy agents for relapsed/refractory adult AML patients: a systematic literature review. Ann Hematol. 2018;97(7):1115–53.
Roboz GJ, Rosenblat T, Arellano M, et al. International randomized phase III study of elacytarabine versus investigator choice in patients with relapsed/refractory acute myeloid leukemia. J Clin Oncol. 2014;32(18):1919–26.
Döhner H, Estey E, Grimwade D, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47.
Levis M. Midostaurin approved for FLT3-mutated AML. Blood. 2017;129(26):3403–6.
Stone RM, Mandrekar SJ, Sanford BL, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med. 2017;377(5):454–64.
Cortes JE, Khaled S, Martinelli G, et al. Quizartinib versus salvage chemotherapy in relapsed or refractory FLT3-ITD acute myeloid leukaemia (QuANTUM-R): a multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2019;20(7):984–97.
Perl AE, Martinelli G, Cortes JE, et al. Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med. 2019;381(18):1728–40.
Zarrinkar PP, Gunawardane RN, Cramer MD, et al. AC220 is a uniquely potent and selective inhibitor of FLT3 for the treatment of acute myeloid leukemia (AML). Blood. 2009;114(14):2984–92.
Mori M, Kaneko N, Ueno Y, et al. Gilteritinib, a FLT3/AXL inhibitor, shows antileukemic activity in mouse models of FLT3 mutated acute myeloid leukemia. Invest New Drugs. 2017;35(5):556–65.
Ferrara F, Lessi F, Vitagliano O, Birkenghi E, Rossi G. Current therapeutic results and treatment options for older patients with relapsed acute myeloid leukemia. Cancers (Basel). 2019;11(2):224.
Short NJ, Kantarjian H, Ravandi F, Daver N. Emerging treatment paradigms with FLT3 inhibitors in acute myeloid leukemia. Ther Adv Hematol. 2019;10:2040620719827310.
Acknowledgements
Funding
This study and general project management support from OPEN Health, and the journal’s Rapid Service Fee, were funded by Astellas Pharma, Inc.
Medical Writing, Editorial, and Other Assistance
Medical writing/editorial support was provided by Francis Beauvais (Francis Beauvais – Rédaction Médicale et Scientifique, 91 Grande Rue, 92310 Sèvres, France) and funded by Astellas Pharma, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Andy Garnham, Franck Bruon, Mounika Parimi, Rosalind Polya, and Marie-Hélène Dramard-Goasdoue were responsible for substantial contribution to study design. Franck Bruon, Céline Berthon, Delphine Lebon, Mounika Parimi, and Rosalind Polya were responsible for acquisition of study data. Andy Garnham, Céline Berthon, Delphine Lebon, Mounika Parimi, Rosalind Polya, Kahina M. Makhloufi and Marie-Hélène Dramard-Goasdoue were responsible for analysis and interpretation of study data. Andy Garnham, Céline Berthon, Delphine Lebon, Mounika Parimi, Rosalind Polya, Kahina M. Makhloufi and Marie-Hélène Dramard-Goasdoue were responsible for drafting the work or revising critically for important intellectual content. All authors gave final approval of the version to be published.
Prior Presentation
Some data from this study were previously presented at the 40th Congress of the French Society of Hematology (Société Francaise d’Hematologie), Paris, France, September 9–11, 2020. P175 (07–42)—Analyse rétrospective de la démographie, des caractéristiques cliniques et des schémas thérapeutiques des patients atteints de LAM R/R FLT3 muté dans deux observatoires français.
Disclosures
Andy Garnham, Franck Bruon, and Kahina M. Makhloufi are employees of Astellas Pharma. Marie-Hélène Dramard-Goasdoue was a former employee of Astellas, but they have since retired. Mounika Parimi and Rosalind Polya were employees of IQVIA during the data analysis of the study, which received funding from Astellas for the conduct of this study. Céline Berthon and Delphine Lebon have no conflicts to disclose.
Compliance with Ethics Guidelines
This study was conducted in adherence to the study protocol and the ethical principles of the Declaration of Helsinki, Commission Nationale de l’Informatique et des Libertés (CNIL) reference methodology MR-004, and any applicable regulations. Because this was a registry-based retrospective study, approval from an ethics review board was not required. Patient consent for the general use of data from the Midi-Pyrénées and Hauts-de-France registries was approved by the CNIL, and permission was obtained from the registry owners to use the information from the data repository for the purpose of this study.
Data Availability
Researchers may request access to anonymized participant level data, trial level data and protocols from Astellas sponsored clinical trials at www.clinicalstudydatarequest.com. For the Astellas criteria on data sharing see: https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Astellas.aspx.
Author information
Authors and Affiliations
Corresponding author
Additional information
Andy Garnham and Marie-Hélène Dramard-Goasdoue: affiliation at the time of the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Garnham, A., Bruon, F., Berthon, C. et al. French Retrospective Database Analysis of Patient Characteristics and Treatment Patterns in Patients with R/R FLT3-Mutated AML: A Registry-Based Cohort Study. Oncol Ther 11, 375–389 (2023). https://doi.org/10.1007/s40487-023-00239-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-023-00239-2