Abstract
Gastroschisis is the most common congenital defect of the abdominal wall, typically located to the right of the umbilical cord, through which the intestinal loops and viscera exit without being covered by the amniotic membrane. Despite the known risk factors for gastroschisis, there is no consensus on the cause of this malformation. Prenatal ultrasound is useful for diagnosis, prognostic prediction (ultrasonographic markers) and appropriate monitoring of fetal vitality. Survival rate of children with gastroschisis is more than 95% in developed countries; however, complex gastroschisis requires multiple neonatal interventions and is associated with adverse perinatal outcomes. In this article, we conducted a narrative review including embryology, pathogenesis, risk factors, and ultrasonographic markers for adverse neonatal outcomes in fetuses with gastroschisis. Prenatal risk stratification of gastroschisis helps to better counsel parents, predict complications, and prepare the multidisciplinary team to intervene appropriately and improve postnatal outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastroschisis is the most common congenital defect of the abdominal wall. This defect is typically small and is located in 95% of cases to the right of the umbilical cord, through which the intestinal loops and viscera exit. Unlike omphalocele, the exposed loops are not protected from the amniotic fluid by the peritoneal membrane, so blood flow to the intestinal loops is more likely to be interrupted [1] (Fig. 1). According to data from the US Centers for Disease Control and Prevention (CDC), the prevalence of gastroschisis has increased by about 30% in the prevalence of gastroschisis from 3.6 per 10,000 births (between 1995 and 2005) to 4.9 per 10,000 births (between 2006 and 2012), but the reason for this trend is unclear [2, 3].
Classically, early maternal age (< 20 years), maternal infections (sexually transmitted diseases and urinary tract infections) and smoking are well documented risk factors for gastroschisis [4, 5]. Early diagnosis of gastroschisis during prenatal care can be made by ultrasound as early as the 12th week of pregnancy, when there is complete closure of the physiologic herniation of the intestine. However, in most cases this malformation is not diagnosed until the second trimester of pregnancy [6].
Fetal growth restriction is quite common in fetuses with gastroschisis (24–67% of cases). It is believed that this is due to the loss of substances through the externalized loops, mainly proteins, leading to nutritional depletion of the fetus. This is supported by the finding of high concentrations of proteins in the amniotic fluid of fetuses with gastroschisis. Placental insufficiency does not appear to be the cause of this growth restriction [7].
Fetal death is more common in fetuses with gastroschisis (4.5%) compared to normal pregnancies (0.6%) [8], with a progressive increase in risk in cases where expectant management was chosen beyond 37 weeks of gestation [9]. A recent meta-analysis showed that 38 weeks is the optimal timing for delivery of fetuses with gastroschisis, fetal growth restriction, and normal umbilical artery Doppler for minimizing overall perinatal mortality and resulting in the highest total quality-adjusted life-years [10]. In the past, it was believed that cesarean section was the best delivery option for fetuses with gastroschisis because it reduced the risk of trauma to the intestinal loops and avoided contact with the vaginal flora. However, several studies have shown that there is no benefit in neonatal outcomes of elective cesarean section compared to vaginal delivery [6, 11].
Neonates with gastroschisis are associated with several complications such as sepsis, necrotizing enterocolitis, short bowel syndrome, bowel obstruction, and volvulus [12]. Complex gastroschisis requires multiple neonatal surgeries and is associated with higher rates of adverse perinatal outcomes than simple gastroschisis [13].
The purpose of this article is to review the embryology, pathogenesis, risk factors, prognosis, and ultrasonographic markers for adverse neonatal outcomes in fetuses with gastroschisis.
Embriology
During the third week of embryonic development, the gastrulation process takes place, in which the bilaminar embryonic disc is converted into a trilaminar disc with the three germ layers (ectoderm, mesoderm and endoderm). This disc lies between two cavities, the amniotic cavity located dorsally, and the umbilical vesicle located ventrally [14, 15].
At the beginning of the fourth week, the trilaminar embryonic disc grows and folds around its ventral part. Cranial, caudal, and lateral folds occur simultaneously. This results in a relative constriction of the embryo in the umbilical vesicle, causing the cephalic and caudal folds to appear in the embryo. In this way, the dorsal part of the umbilical vesicle is incorporated into the embryo as the anterior (cranial) intestine and the posterior (caudal) intestine. This process is also responsible for the cranial displacement of the caudal connecting trunk, bringing it closer to the ventral surface of the embryo [14].
During lateral folding, the primordium of the abdominal wall bends relative to the median plane, incorporating a portion of the endodermal layer as the midgut. This leads to a narrowing of the communication between the midgut and the umbilical vesicle, forming the omphaloenteric duct. At this point, the umbilical cord is observed, formed by the allantois, the connecting pedicle and the omphaloenteric duct, and lined by the amnion [14].
Around the sixth week, the rapid growth of the intestine and other organs, especially the liver, forces the intestine to migrate out of the abdominal cavity, through the umbilical ring, and into the umbilical cord. The intestine rotates 90º counterclockwise around the superior mesenteric artery. This process is the physiologic herniation of the fetus, which is completed by the 11th week with the retraction of the midgut and its return to the abdominal cavity [16].
Pathogenesis
Despite the known risk factors for gastroschisis, there is no consensus on the cause of this malformation. Several theories have been proposed to explain the development of this pathology:
-
(1)
Embryologic failure in mesenchymal differentiation after teratogenic exposure around the fourth week of embryonic development, which would impair abdominal growth, resulting in an opening through which herniation would occur. The possible teratogenic agent was not explained [17]. Feldkamp et al. [18] suggested that gastroschisis is the result of a failure in the fusion of the lateral folds, leading to an abnormal closure of the thoracic and abdominal cavities.
-
(2)
An amniotic rupture at the base of the umbilical cord would weaken the abdominal wall, allowing the loops to herniate [19]. Although this theory did not explain the cause of such a rupture, it was taken up in 1996 by Kluth and Lambrecht [20] who argued that gastroschisis could be the result of the rupture of a small omphalocele. In 2014, Bargy and Beaudoin [21] proposed that the origin of this malformation was due to the rupture of the amnion surrounding the eviscerated loops during physiological herniation. This theory was justified by the observation of vacuolar changes in the cells of the embryos studied, caused by exposure to teratogenic agents.
-
(3)
Possible vascular alterations such as abnormal involution of the right umbilical artery and interruption of the left omphalomesenteric artery could lead to abdominal wall weakness and infarction with necrosis of the umbilical cord base, resulting in intestinal herniation [22, 23]. Both hypotheses were ruled out because they were not compatible with the real embryonic vascular anatomy. However, Lubinsky [24] proposed a vascular/thrombotic theory, postulating that normal involution of the right umbilical vein leaves a space in the umbilical ring that would be susceptible to thrombotic events when estrogen levels are high. This thrombosis would impair cell growth and allow abdominal organs to herniate.
Epidemiology and risk factors
Gastroschisis is a defect of the anterior abdominal wall with herniation of abdominal organs, mainly intestinal loops, without their being covered by the amniotic membrane. There is a worldwide trend of increasing incidence. In the United States, it is estimated to occur in 4–5 children per 10,000 births [25]. In Brazil, a recent study reported an incidence of 2.47 cases per 10,000 births between 2007 and 2020, an increase of 23% in the last two years compared to the first [26].
It is now believed that gastroschisis is the result of an interaction between molecular mechanisms and genetic predisposition during the first 10 weeks of embryonic development. Low maternal age seems to be the main risk factor. An American study estimated that between 2005 and 2013, 74% of gastroschisis cases were diagnosed in women under 25 years of age [27, 28]. However, high BMI seems to be a protective factor [29].
Skarsgard et al. [30] analyzed Canadian databases from 2006–2012 to establish a profile of risk factors for the occurrence of gastroschisis. The authors compared 692 pregnancies with gastroschisis with 4708 normal pregnancies (control group). It was observed that young mothers, smoking, history of pregestational/gestational diabetes and use of antidepressants had a significant association with gastroschisis. Liu et al. [31] evaluated the epidemiologic characteristics of gastroschisis in the Canadian population between 2006 and 2017 by analyzing the Canadian Health Information Institute database. The authors concluded that patients with depressive disorders and the use of cigarettes, alcohol, cocaine, cannabinoids, and opiates were associated with an increased risk of gastroschisis.
To support their hypothesis that gastroschisis is caused by accumulated exposure to potential stressors that induce an oxidative/inflammatory response, Werler et al. [32] performed a case–control study using database analysis. Exposure to 16 agents was assessed: maternal health problems, fever, intensive care unit, bronchodilators, cigarettes, alcohol, illicit drug use, opioids, anti-herpetic medications, oral contraceptives, aspirin, venlafaxine, paroxetine, ibuprofen, parity less than 12 months, and moving. It has been observed that the more stressors a woman is exposed to, the greater her risk of gastroschisis, indicating a dose–response effect. In a recent systematic review, Baldacci et al. [33] conducted a survey of epidemiologic studies published between 1990 and 2018, analyzing risk estimates between lifestyle and sociodemographic factors and gastroschisis. The authors found that smoking, illicit drug use, and alcohol consumption during pregnancy were associated with an increased risk of gastroschisis.
To assess possible risk factors, Weber et al. [34] conducted a retrospective case–control study in the state of California, United States, comparing 286 cases of gastroschisis with 1263 normal pregnancies. The cases analyzed were divided into two groups according to maternal age at delivery: < 20 and ≥ 20 years. In the < 20 years group, the highest odds of having a child with gastroschisis were observed in cases with frequent consumption of chocolate and moderate consumption of sweets, low iron intake, use of paracetamol in the first two months of pregnancy, and a history of urinary tract infection in the first month of pregnancy. In the ≥ 20 years group, Hispanic origin and illicit substance abuse one month before pregnancy were considered important variables.
Diagnosis
The diagnosis of gastroschisis is usually made during the second trimester of pregnancy using ultrasound. The ultrasound examination of the abdominal wall consists of an axial view of the fetal abdomen at the level of the umbilical cord insertion, which may be supplemented by a sagittal view. The color Doppler study helps to demonstrate the normal insertion of the umbilical cord with a right-sided inguinal hernia. The ultrasound findings of gastroschisis are: a reduced fetal abdomen, an anterior abdominal closure defect to the right of the umbilical cord insertion, and varying degrees of exteriorization of the abdominal contents (intestines, stomach, liver, and bladder), which are in contact with the amniotic fluid because they are not covered by the amniotic membrane [35] (Fig. 2).
Prenatal diagnosis of gastroschisis is fundamental because it allows us to advise the parents, to predict the prognosis and to adequately control the fetal vitality, as well as to plan the delivery in a tertiary hospital with a specialized team and postnatal surgical correction.
Prognosis
Complicated pregnancies with gastroschisis are associated with unfavorable outcomes, including fetal growth restriction, amniotic fluid volume alterations, fetal death, prematurity, and low birth weight, as well as the need for prolonged postpartum hospitalization [36].
Fetuses with gastroschisis often have growth restriction in 24–67% of cases [37, 38] and low birth weight in approximately 60% [39]. The mechanism responsible for these conditions is controversial, but is thought to be due to loss of protein by exudation through the walls of the herniated intestinal loops in contact with the amniotic fluid, leading to fetal nutritional depletion and subsequent growth impairment [37, 40]. Dixon et al. [41] concluded that intestinal atresia appears to protect against growth restriction. The healthy intestine, with its intact vascular supply and large surface area, would show greater protein loss than atresic loops.
Horton et al. [7] studied the parameters for calculating weight using the Hadlock formula (biparietal diameter—BPD, head circumference—HC, abdominal circumference—AC and femur length—FL) and showed that fetuses with gastroschisis had impaired intrauterine growth, mainly due to the small AC measurement. This pattern was observed in the middle of the second trimester and did not progress throughout the pregnancy. Thus, placental insufficiency does not seem to be the cause, since there is no worsening of fetal growth. On the other hand, it is believed that the fetal growth restriction index may be overestimated because most formulas for calculating fetal weight use the AC measurement, which is reduced in fetuses with gastroschisis due to herniation of abdominal contents.
Fetal death is common in pregnancies with gastroschisis, with a prevalence of 4.5 deaths per 100 pregnancies, with most cases occurring in the third trimester [8]. The cause is still under debate, but it appears to be related to compression of the umbilical cord by the herniated abdominal contents [42]. The risk begins to increase at around 35 weeks, particularly from 37 weeks, and peaks at 39 weeks. Therefore, the risk of mortality can be minimized by delivering around 37 weeks [9]. Gastroschisis also has a higher neonatal mortality rate (1.75%) compared to normal pregnancies (0.47%) [43].
The survival rate of children with gastroschisis is good, reaching over 95% in developed countries [44]. This is thought to be due to a number of factors, including prenatal diagnosis, delivery in a tertiary hospital with a pediatric surgical service, advances in neonatal intensive care, and continuous improvement in surgical techniques [45]. However, neonates may face several postnatal complications, such as prolonged hospital stay and parenteral nutrition, sepsis, necrotizing enterocolitis, short bowel syndrome, and prolonged mechanical ventilation [46].
After birth, initial management of gastroschisis includes intravenous fluids, respiratory support, and bowel protection. Surgical correction on the first day of life is one of the main goals of treatment, with reduction of herniated contents and abdominal closure to avoid abdominal compartment syndrome [47]. This technique protects the bowel loops from mechanical trauma and eliminates the risk of additional injury, possibly caused by compression of the mesenteric artery [48] (Fig. 3).
If primary closure is not possible, other techniques can be used, such as silo placement with gradual closure of the abdominal wall and closure without suture. In this type of closure, the umbilical cord is placed over the defect after the viscera have been reduced and there is circumferential contraction of the fascia and formation of granulation tissue with subsequent local epithelialization [49] (Fig. 4). An American study compared the results of surgical techniques and concluded that children who underwent primary closure had a shorter hospital stay and a lower risk of surgical site infection. However, they required more days of mechanical ventilation and were more likely to require nutritional support after hospital discharge [50].
In 2001, to categorize the risk of gastroschisis patients and predict adverse outcomes, Molik et al. [51] created two categories based on the presence or absence of intestinal loop anomalies at birth: simple and complex. After analyzing 103 newborns with gastroschisis, they observed that children who had intestinal atresia, volvulus, perforation, or necrosis at birth (complex cases) had higher morbidity and mortality compared to simple cases who did not have such intestinal complications. The complex cases required longer periods of mechanical ventilation, had longer paralytic ileus, and took longer to tolerate total enteral nutrition (Fig. 5).
A Canadian cohort correlated postnatal outcomes with the macroscopic appearance of the intestinal loops at birth using a lesion score (GPS—gastroschisis prognostic score) that included the following variables: matting, necrosis, atresia, and perforation. The presence of each variable was assigned a score ranging from 0 to 4. Patients with a GPS greater ≥ 4 had a mortality rate of 16% [52]. Complex gastroschisis occurs in about 17% of cases and is associated with a higher risk of complications compared to simple gastroschisis. In addition to those mentioned above, we can include short intestine syndrome, sepsis, and necrotizing enterocolitis [53]. Risk stratification helps to better counsel parents, predict complications, and prepare the medical/multidisciplinary team to intervene appropriately.
Prognostic ultrasonographic markers
The rate of prenatal diagnosis of gastroschisis is about 90% in the second trimester of pregnancy in developed countries [54, 55]. Although early diagnosis in the first trimester is possible, it should be remembered that during fetal embryological development, physiological herniation of the small intestine occurs, which ends around 10–12 weeks with the return of the loops to the abdominal cavity [1]. Early detection does not alter management during prenatal care or improve neonatal outcomes, but it does favor early counseling of parents [56].
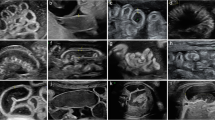
Gastroschisis postnatal outcomes are known to be influenced by the presence or absence of intestinal complications. With this in mind, some studies have been conducted in recent years to identify prenatal factors that may be predictive of adverse neonatal outcomes in order to promote better prenatal counseling and planning for delivery and postnatal care. A meta-analysis by D'Antonio et al. [57] analyzed 26 studies that included 2,023 fetuses with prenatal diagnosis of gastroschisis and compared the ultrasonographic parameters (intra-abdominal intestinal dilatation—IID, extra-abdominal intestinal dilatation—EID, gastric dilatation, intestinal wall thickness, polyhydramnios, and small-for-gestational-age fetus) (Fig. 6) and adverse neonatal outcomes (intestinal atresia, intrauterine death, neonatal death, prolonged hospital stay, duration of parenteral nutrition, and time of total enteral nutrition). Among the variables analyzed, an association was found between increased IID and polyhydramnios and intestinal atresia.
In a retrospective study by Frybova et al. [58], ultrasound data at 30 weeks of 64 fetuses diagnosed with gastroschisis were analyzed and compared with postnatal outcomes. It was observed that fetuses with increased IID (> 10 mm) and wall thickening of the extra-abdominal intestinal loop (≥ 3 mm) (Fig. 7) had longer periods of parenteral nutrition and hospitalization. Intestinal dilatation was also found in 83% of neonates with intestinal atresia. The presence of oligohydramnios (amniotic fluid index—AFI < 8 cm) was associated with increased duration of enteral nutrition. Martillotti et al. [59] showed that increased IID is a strong predictive ultrasound marker of complex gastroschisis with high accuracy when corrected for gestational age. They established IID thresholds for the following gestational age ranges 12 mm (25–30 weeks), 19 mm (30–35 weeks), and 24 mm (35–40 weeks).
Regarding EID, Robertson et al. [60] showed that this parameter was the only one that was statistically significant as a marker for complex gastroschisis. A value greater than 10 mm was used to diagnose EID, which was present in 79% of complex gastroschisis cases (p = 0.037). In a retrospective cohort, Andrade et al. [61] evaluated different ultrasound parameters and their correlation with complex gastroschisis. They found that increased EID (≥ 8, ≥ 9, ≥ 10, and ≥ 11 mm at 25, 26, 27, and 28 weeks, respectively) was a good predictor of complex gastroschisis and was associated with higher mortality and longer hospital stay. To obtain at these results, we used the ratio of observed EID/expected EID for each gestational age. An association was also found between gestational age and IID and polyhydramnios (AFI > 24 cm).
The study by Mazzoni et al. [62], despite its small casuistry (21 cases), found statistical significance between IID ≥ 10 mm occurring before 30 weeks with the need for intestinal resection, increased time on total parenteral nutrition and prolonged hospitalization stay. All cases of intestinal resection occurred in complex gastroschisis cases because the intestinal loops were atresic, volvulus or necrotic. The gestational diagnosis of growth restriction proved to be a risk factor for surgery to correct the abdominal defect at different stages. Some other ultrasound findings have been studied [gastric dilatation (Fig. 8), gastric herniation and size of the abdominal wall defect], but there is disagreement in the literature as to their significance in relation to complex gastroschisis or neonatal morbidity and mortality. Table 1 summarizes the manly studies in the literature that have evaluated prognostic ultrasonographic markers in fetuses with gastroschisis.
A recent study by Simon et al. [63] reviewed ultrasounds documenting fetal intestinal measurements in 116 pregnancies complicated by gastroschisis. They found statistical significance between utero intestinal characteristics and 11 outcomes, but with minimal meaningful clinical differences in outcomes. The IID was associated with a decrease in gestational age at delivery of 0.5 weeks and an increase in birth weight of 6.93 g.
Conclusion
Gastroschisis is the most common congenital defect of the abdominal wall and its prevalence is increasing due to the influence of numerous risk factors. Prenatal diagnosis can be made by ultrasonography, which is also the method used to monitor fetal vitality and help guide the prognosis and postnatal management. Fetal death can occur in gastroschisis, especially at the end of the third trimester. Complex gastroschisis or gastroschisis associated with fetal growth restriction, changes in amniotic fluid volume, prematurity, and low birth weight often result in unfavorable postnatal outcomes. In summary, the best postnatal outcomes for gastroschisis can be achieved with appropriate planning and follow-up by a multidisciplinary team.
References
Prefumo F, Izzi C (2014) Fetal abdominal wall defects. Best Pract Res Clin Obstet Gynaecol 28(3):391–402
Kirby RS (2017) The prevalence of selected major birth defects in the United States. Semin Perinatol 41(6):338–344
Jones AM, Isenburg J, Salemi JL, Arnold KE, Mai CT, Aggarwal D et al (2016) Increasing prevalence of gastroschisis—14 states, 1995–2012. MMWR Morb Mortal Wkly Rep 65(2):23–26
Baer RJ, Chambers CD, Jones KL, Shew SB, MacKenzie TC, Shaw GM et al (2015) Maternal factors associated with the occurrence of gastroschisis. Am J Med Genet A 167(7):1534–1541
Given JE, Wiesel A, Rissmann A, Lynch C, Neville AJ, Pierini A et al (2017) Gastroschisis in Europe—a case-malformed-control study of medication and maternal illness during pregnancy as risk factors. Paediatr Perinatal Epidemiol 31(6):549–559
Oakes MC, Porto M, Chung JH (2018) Advances in prenatal and perinatal diagnosis and management of gastroschisis. Semin Pediatr Surg 27(5):289–299
Horton AL, Powell MS, Wolfe HM (2010) Intrauterine growth patterns in fetal gastroschisis. Am J Perinatol 27(3):211–217
South AP, Stutey KM, Meinzen-Derr J (2013) Metaanalysis of the prevalence of intrauterine fetal death in gastroschisis. Am J Obstet Gynecol 209(2):114.e1-114.e13
Sparks TN, Shaffer BL, Page J, Caughey AB (2017) Gastroschisis: mortality risks with each additional week of expectant management. Am J Obstet Gynecol 216(1):66.e1-66.e7
Packer CH, Pilliod RA, Caughey AB, Sparks TN (2023) Optimal timing of delivery for growth restricted fetuses with gastroschisis: a decision analysis. Prenat Diagn 43(12):1506–1513
Kirollos DW, Abdel-Latif ME (2018) Mode of delivery and outcomes of infants with gastroschisis: a meta-analysis of observational studies. Arch Dis Child Fetal Neonatal Ed 103(4):F355–F363
Ferreira RG, Mendonça CR, Gonçalves Ramos LL, de Abreu Tacon FS, Naves do Amaral W, Ruano R (2022) Gastroschisis: a systematic review of diagnosis, prognosis and treatment. J Matern Fetal Neonatal Med 35(25):6199–6212
Joyeux L, Belfort MA, De Coppi P, Basurto D, Valenzuela I, King A et al (2021) Complex gastroschisis: a new indication for fetal surgery? Ultrasound Obstet Gynecol 58(6):804–812
Moore KL, Persaud TVN, Torchia MG (2018) The developing human: clinically oriented embryology, 11th edn. Elsevier, Philadelphia, PA
Beaudoin S (2018) Insights into the etiology and embryology of gastroschisis. Semin Pediatr Surg 27(5):283–288
Schoenwolf GC, Bleyl SB, Brauer PR (2014) Larsen’s human embryology, FWP, 5th edn. Elsevier, Philadelphia, PA
Duhamel B (1963) Embryology of exomphalos and allied malformations. Arch Dis Child 38(198):142–147
Feldkamp ML, Carey JC, Sadler TW (2007) Development of gastroschisis: review of hypotheses, a novel hypothesis, and implications for research. Am J Med Genet 143A(7):639–652
Shaw A (1975) The myth of gastroschisis. J Pediatr Surg 10(2):235–244
Kluth D, Lambrecht W (1996) The pathogenesis of omphalocele and gastroschisis an unsolved problem. Pediatr Surg Int 11(2–3):62–66
Bargy F, Beaudoin S (2014) Comprehensive developmental mechanisms in gastroschisis. Fetal Diagn Ther 36(3):223–230
de Vries PA (1980) The pathogenesis of gastroschisis and omphalocele. J Pediatr Surg 15(3):245–251
Hoyme HE, Higginhottom MC, Jones KL (1981) The vascular pathogenesis of gastroschisis: intrauterine interruption of the omphalomesenteric artery. J Pediatr 98(2):228–231
Lubinsky M (2014) A vascular and thrombotic model of gastroschisis. Am J Med Genet A 164(4):915–917
Burjonrappa S, Snyder AN (2021) Regional variation in gastroschisis: a nationwide database review of demographics and outcomes. Pediatr Surg Int 37(7):911–917
Regadas CT, Escosteguy CC, Fonseca SC, Pinheiro RS, Coeli CM (2023) Trends in prevalence of gastroschisis in Brazil from 2007 to 2020: a national population-based cross-sectional study. Birth Defects Res 115(6):633–646
Salinas-Torres VM, Gallardo-Blanco HL, Salinas-Torres RA, Cerda-Flores RM, Lugo-Trampe JJ, Villarreal-Martínez DZ et al (2019) Bioinformatic analysis of gene variants from gastroschisis recurrence identifies multiple novel pathogenetic pathways: implication for the closure of the ventral body wall. Int J Mol Sci 20(9):2295
Friedman AM, Ananth CV, Siddiq Z, D’Alton ME, Wright JD (2016) Gastroschisis: epidemiology and mode of delivery, 2005–2013. Am J Obstet Gynecol 215(3):348.e1-348.e9
Raitio A, Tauriainen A, Leinonen MK, Syvänen J, Kemppainen T, Löyttyniemi E et al (2020) Maternal risk factors for gastroschisis: a population-based case–control study. Birth Defects Res 112(13):989–995
Skarsgard ED, Meaney C, Bassil K, Brindle M, Arbour L, Moineddin R (2015) Maternal risk factors for gastroschisis in Canada. Birth Defects Res A Clin Mol Teratol 103(2):111–118
Liu S, Evans J, Boutin A, Luo W, Gheorghe M, Auger N et al (2021) Time trends, geographic variation and risk factors for gastroschisis in Canada: a population-based cohort study 2006–2017. Paediatr Perinat Epidemiol 35(6):664–673
Werler MM, Guéry E, Waller DK, Parker SE (2018) Gastroschisis and cumulative stressor exposures. Epidemiology 29(5):721–728
Baldacci S, Santoro M, Coi A, Mezzasalma L, Bianchi F, Pierini A (2020) Lifestyle and sociodemographic risk factors for gastroschisis: a systematic review and meta-analysis. Arch Dis Child 105(8):756–764
Weber KA, Yang W, Carmichael SL, Padula AM, Shaw GM (2019) A machine learning approach to investigate potential risk factors for gastroschisis in California. Birth Defects Res 111(4):212–221
Raia-Barjat T, Stadler A, Varlet MN, Fanget C, Noblot E, Prieur F et al (2016) Accuracy of antenatal ultrasound signs in predicting the risk for bowel atresia in patients with gastroschisis. Eur J Obstet Gynecol Reprod Biol 203:116–120
Tauriainen A, Sankilampi U, Raitio A, Tauriainen T, Helenius I, Vanamo K et al (2021) The association of perinatal and clinical factors with outcomes in infants with gastroschisis—a retrospective multicenter study in Finland. Eur J Pediatr 180(6):1875–1883
Crawford RA, Ryan G, Wright VM, Rodeck CH (1992) The importance of serial biophysical assessment of fetal wellbeing in gastroschisis. Br J Obstet Gynaecol 99(11):899–902
Fries MH, Filly RA, Callen PW, Goldstein RB, Goldberg JD, Golbus MS (1993) Growth retardation in prenatally diagnosed cases of gastroschisis. J Ultrasound Med 12(10):583–588
Miranda ME, Emil S, de Mattos PR, Piçarro C, Cruzeiro PCF, Campos BA et al (2019) A 25-year study of gastroschisis outcomes in a middle-income country. J Pediatr Surg 54(7):1481–1486
Payne NR, Simonton SC, Olsen S, Arnesen MA, Pfleghaar KM (2011) Growth restriction in gastroschisis: quantification of its severity and exploration of a placental cause. BMC Pediatr 11:90
Dixon J, Penman D, Soothill P (2000) The influence of bowel atresia in gastroschisis on fetal growth, cardiotocograph abnormalities and amniotic fluid staining. BJOG 107(4):472–475
Kalache KD, Bierlich A, Hammer H, Bollmann R (2002) Is unexplained third trimester intrauterine death of fetuses with gastroschisis caused by umbilical cord compression due to acute extra-abdominal bowel dilatation? Prenat Diagn 22(8):715–717
Broth R, Shlossman P, Kaufmann M, Berghella V (2001) Increased incidence of stillbirth in fetuses with gastroschisis. Am J Obstet Gynecol 185(6):S246
Bradnock TJ, Marven S, Owen A, Johnson P, Kurinczuk JJ, Spark P et al (2011) Gastroschisis: one year outcomes from national cohort study. BMJ 343:d6749
Wright NJ, Sekabira J, Ade-Ajayi N (2018) Care of infants with gastroschisis in low-resource settings. Semin Pediatr Surg 27(5):321–326
Nicholas SS, Stamilio DM, Dicke JM, Gray DL, Macones GA, Odibo AO (2009) Predicting adverse neonatal outcomes in fetuses with abdominal wall defects using prenatal risk factors. Am J Obstet Gynecol 201(4):383.e1-383.e6
Haddock C, Skarsgard ED (2018) Understanding gastroschisis and its clinical management: where are we? Expert Rev Gastroenterol Hepatol 12(4):405–415
Ryckman J, Aspirot A, Laberge JM, Shaw K (2009) Intestinal venous congestion as a complication of elective silo placement for gastroschisis. Semin Pediatr Surg 18(2):109–112
Skarsgard ED (2016) Management of gastroschisis. Curr Opin Pediatr 28(3):363–369
Gurien LA, Dassinger MS, Burford JM, Saylors ME, Smith SD (2017) Does timing of gastroschisis repair matter? A comparison using the ACS NSQIP pediatric database. J Pediatr Surg 52(11):1751–1754
Molik KA, Gingalewski CA, West KW, Rescorla FJ, Scherer LR, Engum SA et al (2001) Gastroschisis: a plea for risk categorization. J Pediatr Surg 36(1):51–55
Cowan KN, Puligandla PS, Laberge JM, Skarsgard ED, Bouchard S, Yanchar N et al (2012) The gastroschisis prognostic score: reliable outcome prediction in gastroschisis. J Pediatr Surg 47(6):1111–1117
Bergholz R, Boettcher M, Reinshagen K, Wenke K (2014) Complex gastroschisis is a different entity to simple gastroschisis affecting morbidity and mortality—a systematic review and meta-analysis. J Pediatr Surg 49(10):1527–1532
Faugstad TM, Brantberg A, Blaas HGK, Vogt C (2014) Prenatal examination and postmortem findings in fetuses with gastroschisis and omphalocele. Prenat Diagn 34(6):570–576
Garne E, Loane M, Dolk H, De Vigan C, Scarano G, Tucker D et al (2005) Prenatal diagnosis of severe structural congenital malformations in Europe. Ultrasound Obstet Gynecol 25(1):6–11
Cerekja A, Piazze J, Cozzi D (2012) Early prenatal sonographic diagnosis of gastroschisis. J Clin Ultrasound 40(8):526–528
D’Antonio F, Virgone C, Rizzo G, Khalil A, Baud D, Cohen-Overbeek TE et al (2015) Prenatal risk factors and outcomes in gastroschisis: a meta-analysis. Pediatrics 136(1):e159–e169
Frybova B, Vlk R, Kokesova A, Rygl M (2015) Isolated prenatal ultrasound findings predict the postnatal course in gastroschisis. Pediatr Surg Int 31(4):381–387
Martillotti G, Boucoiran I, Damphousse A, Grignon A, Dubé E, Moussa A et al (2016) Predicting perinatal outcome from prenatal ultrasound characteristics in pregnancies complicated by gastroschisis. Fetal Diagn Ther 39(4):279–286
Robertson JA, Kimble RM, Stockton K, Sekar R (2017) Antenatal ultrasound features in fetuses with gastroschisis and its prediction in neonatal outcome. Aust N Z J Obstet Gynaecol 57(1):52–56
Andrade WS, Brizot ML, Rodrigues AS, Tannuri AC, Krebs VL, Nishie EN et al (2018) Sonographic markers in the prediction of fetal complex gastroschisis. Fetal Diagn Ther 43(1):45–52
Mazzoni G, Alberti D, Torri F, Motta M, Platto C, Franceschetti L et al (2022) Prediction of complex gastroschisis: the evolution of therapeutic techniques and their relation with fetal sonographic features. J Neonatal Perinatal Med 15(1):137–145
Simon R, Shay R, Bergam B, Katz R, Delaney S (2023) Gastroschisis ultrasound bowel characteristics demonstrate minimal impact on perinatal outcomes. J Neonatal Perinatal Med 16(4):639–647
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Ethical approval
No necessary.
Consent to participate
No necessary.
Consent to publish
Patients gave their consent to publish the images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muniz, T.D., Rolo, L.C. & Araujo Júnior, E. Gastroschisis: embriology, pathogenesis, risk factors, prognosis, and ultrasonographic markers for adverse neonatal outcomes. J Ultrasound 27, 241–250 (2024). https://doi.org/10.1007/s40477-024-00887-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-024-00887-8