Abstract
Background
A biloma refers to an abnormal, well-defined accumulation of bile outside the biliary tree within the abdomen, which can be either intra- or extra-hepatic in nature. It can result from traumatic or iatrogenic causes, leading to a disruption in the biliary system. Without prompt diagnosis and appropriate management, it can result in significant morbidity and mortality. While magnetic resonance cholangiopancreatography (MRCP) is the typical diagnostic method, there are instances where it may not provide conclusive results.
Case presentation
We present the case of a 72-year-old woman who underwent an hepatic resection of the seventh segment after recurrence of hepatocellular carcinoma (HCC). During the ultrasound (US) follow-up, she developed a peri-hepatic collection which proved to be a biloma continuously refurnished by the biliary tree. Neither the MRCP nor the percutaneous transhepatic cholangiography (PTC) were able to clearly detect the exact site of the bile leak. While awaiting the Endoscopic Retrograde Cholangio-Pancreatography (ERCP), a Contrast-Enhanced Ultrasound (CEUS) was conducted administering the contrast agent directly through the percutaneous drainage catheter placed in the biloma. This revealed the presence of contrast flow from the collection to a peripheral right bile duct, confirming the intra-hepatic leak communication.
Conclusions
This case demonstrates that Contrast-Enhanced Ultrasound (CEUS) presents a straightforward, secure, and precise approach to detect biliary leakage responsible for the formation of a biloma. Additionally, the adoption of CEUS offers the dual benefit of minimizing radiation exposure for the patient and obviating the requirement for anesthesia. In summary, CEUS emerges as a compelling alternative to conventional diagnostic methods for effectively managing a biloma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A biloma is currently considered as any abnormal, well-circumscribed, intra-abdominal bile collection external to the biliary tree, which can either be intra- or extra-hepatic. This entity needs to be differentiated by intraperitoneal free bile, which is referred to as ‘choleperitoneum’ or ‘bile ascites’ leading to a different surgical approach [1].
Bilomas represent a rare yet potentially severe complication of biliary tree disruption secondary to iatrogenic surgical damage, such as cholecystectomy, endoscopic retrograde cholangiopancreatography (ERCP), radiofrequency ablation, transcatheter arterial chemoembolization, liver transplantation, liver resection and biopsy, or can be induced by trauma-related biliary tract damage [1].
The interventional radiologist plays a key role in providing a prompt diagnosis and consequently appropriate treatment, since bilomas may lead to significant morbidity and mortality when not adequately treated [2].
Ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), magnetic resonance cholangiopancreatography (MRCP), hepatobiliary cholescintigraphy and ERCP are the main radiological techniques in use to diagnose and evaluate the least invasive treatment [2, 3].
However, in our case, these modalities were not successful, so, awaiting the ERCP, we attempted to demonstrate the presence of the source supplying the biloma through contrast-enhanced ultrasound (CEUS), which may represent a less invasive and more affordable diagnostic technique compared to traditional ones.
Case presentation
A 72-year-old woman with a history of orthotopic liver transplantation for hepatocellular carcinoma underwent surgery at our center to remove the seventh hepatic segment after recurrence of disease.
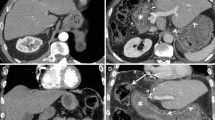
The postoperative course was hampered by the formation of a postero-lateral collection, which was confirmed by CT and US (Figs. 1, 2).
A percutaneous CT-guided drainage of the collection was therefore carried out, allowing the leakage of corpuscular exudate along with greenish-yellow biliary material.
However, the drainage of the collection was not resolutive, ince the biloma revealed to by supplied by the biliary tree.
The patient therefore underwent an upper abdomen MRI with hepatospecific contrast medium to identify the precise bile leakage site, though the exam did not prove to be conclusive.
Consequently, a PTC was performed injecting the contrast medium directly through the drainage tube, which revealed a potential initial transit of contrast medium in a branch of the biliary system beneath the collection, nevertheless it was unable to identify the exact site of the bile leak (Fig. 3).
While awaiting the ERCP and the placement of a naso-biliary tube (NBT), it was made the decision to perform CEUS: the micro-bubble contrast agent was administered directly by the percutaneous drainage catheter placed in the biloma, which successfully identified the flow of the contrast agent from the biloma to a peripheral right bile duct confirming the intrahepatic leak communication (Video).
Discussion
A biloma is an encapsulated collection of bile external to the biliary tract, which can either be intra or extra-hepatic. Its development can result from several causes, including spontaneous events, traumas and post-instrumental maneuvers.
Abdominal US represents the first-level diagnostic radiological investigation in the diagnosis of biloma [1, 3]. Generally, the visualization of an anechoic fluid collection with low-level internal echoes, well-defined borders, and a lack of vascularization on Doppler ultrasonography are all leading to the presence of a biloma.
Since CT sensitivity is superior to that of US, it typically represents the second-level diagnostic modality. Furthermore, CT has a higher spatial resolution and greater identification of the fluid collection morphology and site [3]. In CT scans biloma appears as a well-circumscribed collection with clear hypodense borders, showing values of density below 20 Hounsfield units and no contrast-enhancement [4, 5].
However, these radiological features are not highly specific for biloma as they are also found in all those formations showing similar densities; as a result, the differential diagnosis includes an extensive variety of entities, such as lymphocele, abscess, hematoma, liver cyst, cystic seroma, or peritoneal cystic metastases. [3, 6].
In this case, MRI represents a further useful diagnostic technique in order to identify the root cause of the collection along with locating the potential site of the leakage. On MRI images, bilomas typically produce a high-signal homogeneous intensity on T2-weighted images, while showing heterogeneous low signal intensity on T1-weighted imaging. Normally, they do not show contrast-enhancement, however in cases of reactive inflammation, there is a possibility that the medium permeates into the biloma, subsequently displaying a rim-enhancement or enhancing septation [1].
MRCP represents the “gold standard” for a complete morphological evaluation of the biliary tree, since it is non- invasive, ionizing radiation free and guarantees a great spatial resolution providing excellent anatomical information [3].
Important details regarding biliary anatomy can be acquired through the aid of hepatocyte-selective contrast agent with biliary excretion, which enables precise identification of biliary fistulas and bilomas: the latter appear on hepatobiliary delayed phase imaging as gradual fill-in and, if the sequence of the exam is particularly thin, it may be further useful in identifying the exact location of the biliary duct injury [7, 8].
In our case, the MRCP was performed with Primovist® contrast (disodium gadoxetate; Bayer, Australia) through repeated sequences over a period of thirty-five minutes and at one and a half hour after the initial administration. However, the MRCP failed to demonstrate the fistulous path.
In some cases, the resolution of a biloma can be accomplished by placing a percutaneous drainage into the collection. However, in our case the collection was continuously re-filled with bile and tended to regenerate despite the presence of the drainage.
PTC and ERCP, as third level studies, can identify the presence of a continuous bile leak, providing the exact anatomical diagnosis as well as allowing the treatment of the condition. However, both studies are invasive and associated with a non-negligible risk of complications. In our case, it was therefore carried out the decision to perform a PTC, injecting the contrast medium directly in the drainage tube, which resulted unsuccessful since it allowed only a partial visualization of the leak.
Meanwhile, awaiting the ERCP and the placement of a NBT, the interventional radiologist attempted a rapid and non-invasive mean to visualize the fistula through CEUS, injecting contrast directly through the percutaneous trans-hepatic biliary drainage catheter already located in the biloma. The injection consisted of one phial of sulphur hexafluoride namely SonoVue® (Bracco, Milan, Italy) diluted in 20 mL of saline solution, even though the biloma was already partially filled by the previous fistulography procedure. With the aid of CEUS, we were instantly able to visualize the micro-bubble contrast flowing from the biloma through a peripheral right bile duct which successively opacified the common bile duct. Finally, the cholangiography performed injecting the contrast through the NBT also confirmed the location of the biliary leakage previously diagnosed by CEUS (Fig. 4, Table 1).
However, it should be acknowledged that CEUS has some US-related intrinsic limitations, such as the patient’s BMI, the presence of free intraperitoneal air and the inability of the patient to maintain breath-hold. This technique also requires proper training and experience on the part of the technician, added to the fact it is often hindered by machine characteristics: some have device-specific software, which may alter image quality and potentially invalidate its reproducibility. Finally, US does not provide a panoramic view since it offers limited abdomen window visualization and, in the specific case of abdominal fluid collection, it is unable to characterize the nature of the collection alone.
Conclusion
This case proved that CEUS may be considered in clinical practice to identify the precise biliary leakage supplying a biloma since it appears to be a simple, safe and accurate diagnostic technique. Furthermore, this method is rapid, reproducible, and minimally invasive as it avoids the need for anesthesiology and ensures minor radiation exposure, with consequently less risk of renal injury compared to traditional techniques. In conclusion, this approach to biliary tract injuries appears to be a promising option and further studies with a larger number of patients are necessary to evaluate and fully standardize the application of CEUS in clinical practice.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MRCP:
-
Magnetic resonance cholangiopancreatography
- HCC:
-
Hepatocellular carcinoma
- US:
-
Ultrasound
- ERCP:
-
Endoscopic Retrograde Cholangio-Pancreatography
- CEUS:
-
Contrast-Enhanced Ultrasound
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- NBT:
-
Naso-biliary tube
- PTC:
-
Percutaneous transhepatic cholangiography
References
Balfour J, Ewing A (2023) Hepatic Biloma. 2023 Jun 26. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing
Copelan A, Bahoura L, Tardy F, Kirsch M, Sokhandon F, Kapoor B (2015) Etiology, diagnosis, and management of bilomas: a current update. Tech Vasc Interv Radiol 18(4):236–243. https://doi.org/10.1053/j.tvir.2015.07.007. (Epub 2015 Jul 15)
De'Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de'Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D (2021) 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg 16(1):30. https://doi.org/10.1186/s13017-021-00369-w
Vazquez JL, Thorsen MK, Dodds WJ, Quiroz FA, Martinez ML, Lawson TL, Stewart ET, Foley WD (1985) Evaluation and treatment of intraabdominal bilomas. AJR Am J Roentgenol 144(5):933–938. https://doi.org/10.2214/ajr.144.5.933
Akin K, Ozturk A, Guvenc Z, Isiklar I, Haberal M (2006) Localized fluid collections after liver transplantation. Transplant Proc 38(2):627–630. https://doi.org/10.1016/j.transproceed.2006.02.006
Walker AT, Shapiro AW, Brooks DC, Braver JM, Tumeh SS (1992) Bile duct disruption and biloma after laparoscopic cholecystectomy: imaging evaluation. AJR Am J Roentgenol 158(4):785–789. https://doi.org/10.2214/ajr.158.4.1532111
Chaudhary A, Negi SS, Puri SK, Narang P (2002) Comparison of magnetic resonance cholangiography and percutaneous transhepatic cholangiography in the evaluation of bile duct strictures after cholecystectomy. Br J Surg 89(4):433–436
Di Serafino M, Iacobellis E, Ronza R, Martino A, Grimaldi D, Rinaldo C, Caruso M, Dell’Aversano Orabona G, Barbuto L, Verde F, Sabatino V, Schillirò ML, Brillantino A, Romano L (2023) Hepatobiliary-specific magnetic resonance contrast agents: role in biliary trauma. Gland Surg. https://doi.org/10.21037/gs-23-29
Thompson CM, Saad NE, Quazi RR, Darcy MD, Picus DD, Menias CO (2013) Management of iatrogenic bile duct injuries: role of the interventional radiologist. Radiographics 33(1):117–134. https://doi.org/10.1148/rg.331125044
Funding
The authors did not receive any funding.
Author information
Authors and Affiliations
Contributions
RL observed the case and performed the ultrasound examinations. VM collected the data, performed the literature review, drafted the manuscript, created the figures and edited the videos. AP and LG contributed significantly to the drafting and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests.
Ethics approval and consent to participate
The institutional review board approved this case report, its publication and the corresponding written informed consent was obtained from the patient.
Consent for publication
Informed consent was obtained from the patient for publication of this report and/or any accompanying images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 14771 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marinato, V., Phillips, A., Giuliano, L. et al. The role of CEUS in the management of biloma. J Ultrasound 27, 745–749 (2024). https://doi.org/10.1007/s40477-023-00849-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-023-00849-6