Abstract
Purpose
Skeletal muscle ultrasound is a valuable tool for assessing muscle wasting in ICU. Previous studies on skeletal muscle ultrasound in ICU have been performed on lower limb muscles. The current study is formulated to assess the feasibility and reliability of anterior temporalis (AT) muscle ultrasound for measuring muscle wasting in ICU.
Methods
In this prospective cohort study in 48 critically ill patients with sepsis, muscle layer thicknesses (MLTs) and mean grayscale (GS) values of anterior temporalis muscles and quadriceps femoris (Q) were measured at baseline and serially till 7 days. Correlation was made between baseline and change in MLT and GS values of AT and Q muscle and these parameters were compared between ICU survivors and non survivors.
Results
Baseline anterior temporalis MLTs or their longitudinal changes over 7 days did not correlate significantly with the corresponding parameters of quadriceps femoris muscles. The baseline GS values of two muscle groups correlated weakly at baseline, but the change in GS over 7 days showed no correlation. The baseline MLTs of both muscle groups and their longitudinal change over 7 days did not correlate with ICU length of stay. The change in MLT of AT over 7 days was significantly greater in ICU non-survivors compared to survivors.
Conclusion
Measurement of ultrasonographic muscle layer thickness and grayscale parameters of anterior temporalis muscle did not show good correlation with that of quadriceps muscle.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Skeletal muscle ultrasound is emerging as a valuable tool for assessing muscle wasting in critically ill patients. Ultrasound measurements correlate well with the findings of computerized tomography (CT) and magnetic resonance imaging (MRI) based muscle mass estimation [1, 2], with the additional advantages of point-of-care availability, low cost and absence of radiation exposure. Ultrasound derived Quadriceps muscle layer thickness (QMLT) has been found to accurately assess muscle mass in intensive care units (ICU). It also correlates with muscle strength and length of stay in ICU [3,4,5,6]. In addition to muscle cross-sectional area (CSA) and muscle layer thickness (MLT), some studies have found increase in echogenicity of limb muscles in critically ill patients to correlate with the development of muscle necrosis [7, 8].
The accuracy of sonographic assessment of lower limb musculature may be affected by peripheral edema and obesity [9]. While sunken temples have been described as part of Hippocratic facies found in cachectic patients and often found in critically ill patients with muscle wasting, ultrasonographic observation of temporalis muscle wasting in ICU has not been studied to the best of our knowledge. This muscle may be relatively spared from edema due to its anterior location and the insonation of the muscle may be easier with no requirement of disrobement or exposure of lower limbs.
This study is formulated to test the feasibility of sonographic assessment of temporalis muscle thickness and echogenicity. We hypothesize that the baseline MLT and echogenicity of anterior temporalis muscle and their percentage change over 7 days correlate with the antero-posterior MLT and echogenicity of quadriceps femoris muscle (i.e., the combined thickness of rectus femoris and vastus intermedius muscle layers).
The primary objective of our study is to assess the correlation between the percentage longitudinal change of anterior temporalis MLT over 7 days with the corresponding changes in quadriceps femoris muscle. We also assessed the relation between the baseline thickness of both muscle groups, the baseline grayscale values (echogenicity) and their change in both muscle groups. The relation of ultrasound parameters with ICU length of stay and mortality was also assessed.
Methods
Study design and settings
This single centre, prospective observational cohort study was undertaken in the ICU of Department of Anaesthesiology, Pain Medicine and Critical Care, All India Institute of Medical Sciences, New Delhi. The ethical clearance was obtained from the institutional ethics committee. Pre-trial registration of protocol was done with Clinical Trial Registry-India vide registration number CTRI/2018/09/015827.
Study population
Forty-eight critically ill adult (age more than 18 years) patients admitted to ICU with diagnosis of sepsis as per Sepsis-3 definition [10] and expected to have ICU stay of at least seven days were included in our study. Informed consent was obtained from the patients or their legally authorized representatives. Exclusion criteria were failure to obtain informed consent, paraparesis, quadriparesis, primary systemic neuromuscular disease and deep venous thrombosis.
Data collection
The following baseline variables were recorded: medical diagnosis, age, sex, body mass index, Acute Physiology and Chronic Health Evaluation (APACHE) II score, and Sequential Organ Function Assessment (SOFA) scores. Serial muscle ultrasonography was done on day 1, 3, 5 and 7. MLTs and mean grayscale values (GS) of anterior temporalis and quadriceps femoris (rectus femoris and vastus intermedius) muscles were recorded. The length of stay in ICU (ICU-LOS) and ICU outcome (death or discharge) for each patient were recorded.
Procedure for muscle ultrasonography
Ultrasound measurements of MLT and GS were done using 6–12 MHz linear array probe (FUJIFILM SonoSite Edge®, Bothell, WA), with the patients in supine position and the legs relaxed lying flat in extension and not clenching teeth or biting the endotracheal tube.
Quadriceps muscle ultrasound of each side was done at two positions: (i) the midpoint between the antero-superior iliac spine (ASIS) and the upper pole of the patella and (ii) the junction between the lower third and upper two-thirds between the ASIS and the upper pole of the patella [5, 11]. The mean values of readings from 4 points (two from each side) were recorded as a reading of anteroposterior MLT of Quadriceps femoris muscle. The average of three such readings were recorded as Quadriceps muscle layer thickness (QMLT) in millimeters (Fig. 1).
For the anterior temporalis muscle, the probe was placed in front of the anterior hair line just above the zygomatic arch on each side [12]. The thickness of the muscle layer was measured at three points- the point A corresponding to the deepest point of temporal fossa, the subsequent points B and C being 1 cm apart. The maximum thickness at point A and the mean values of the thickness at three points were recorded in millimeters. The maximum and mean thickness were measured thrice on both sides (i.e., 6 measures) and averaged and recorded as ATMLTmax (average of MLTs at point A) and ATMLTmean (average of MLTs measured at points A, B and C) (Fig. 1).
Muscle echogenicity was measured post image acquisition as mean grayscale value on a scale from 0 (black) to 255 (white) by gray-scale histogram analysis using the software ImageJ (National Institute of Health, USA; https://imagej.nih.gov). The region of interest (ROI) for histogram analysis was obtained by tracing the margins of anterior temporalis muscle and rectus femoris muscle. Vastus intermedius muscle area was not included in ROI due to the possibility of inadequate insonation of deeper muscle layers in patients with subcutaneous edema or thick musculature. The average of three readings from both sides were recorded as GSAT and GSQ, for anterior temporalis and quadriceps femoris muscle groups respectively (Fig. 2).
To eliminate inaccuracy due to variable gain settings, the measurements were done using default gain level and factory preset resolution. All ultrasonography were done by the same observer (AB), and subsequently saved images were checked by a radiologist (MJ). None of them participated in data collection.
Sample size calculation and data analysis
Assuming coefficient of correlation (r) ≥ 0.4, 47 critically ill adults were planned to be included in our study. Based on a planned interim analysis after 20 patients, sample size was modified to 48 patients. Nominal and ordinal data were represented as frequency (percentage). Parametric and non-parametric data were summarized as mean ± standard deviation and median (interquartile range) respectively. Normality of continuous data was tested by visual inspection of histograms, skewness, kurtosis and their critical values, and using Shapiro–Wilk test.
Pearson’s correlation was used to assess the correlation between values of two parametric variables, Spearman rho was used if one of the variables was non-parametric, and Kendall’s tau was used if both the variables were non-parametric. Paired t-test and Wilcoxon signed rank test were used for comparison of distribution of paired parametric and non-parametric data respectively. Student t-test and Mann Whitney U-test were done to compare distribution of values for independent parametric and non-parametric variables.
A two tailed p-value lower than 0.05 was considered significant for rejecting all null hypotheses. R Project with R Studio and Microsoft Excel were used for data compilation, statistical analysis and graphical representations.
Result
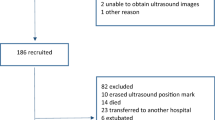
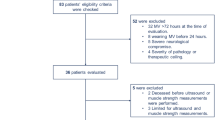
In this prospective observational trial, 48 patients were recruited. Demographic parameters, diagnosis and disease severity scores are displayed in Table 1. Baseline MLTs of 48 patients and their change over 7 days were included for analysis. After exclusion of a sub-optimal image of 1 patient for gray-scale analysis, the grayscale scores of 47 patients and their change over 7 days were included for analysis.
The maximum and mean anterior temporalis muscle layer thickness decreased by a median of 9.9% (IQR − 4.9 to 18.1%) and 7.1% (IQR − 1.8 to 17.1%) respectively over 7 days. The QMLT decreased by a median of 11.4% (IQR − 10.9 to 27.9%) over 7 days. The changes in measurements of quadriceps MLT, maximum and mean MLT of anterior temporalis over 7 days, henceforth mentioned as ΔQMLT, ΔATMLTmax and ΔATMLTmean, are statistically significant (Table 2).
The median increase in echogenicity of anterior temporalis muscle (ΔGSAT) is 5.2% (IQR − 7.4 to 17.1%), but the increase is not statistically significant, Wilcoxon signed rank test, W = 454, z = − 1.37, p = 0.246. The echogenicity of quadriceps femoris muscle increased by a median of 7.6% (IQR − 6.6 to 27.9%), and the increase is statistically significant, Wilcoxon signed rank test, W = 337, z = − 2.57, p = 0.016.
The baseline maximum or mean MLTs of aneterior temporalis muscle and their change over 7 days did not correlate significantly with those of Quadriceps femoris muscle (Table 3). A weak but statistically significant correlation was seen between the baseline mean grayscale of anterior temporalis and quadriceps femoris, rho(45) = 0.32, p = 0.026. However, there was no significant correlation between their percentage change over 7 days, rτ = 0.15, p = 0.133.
Thirty-three patients in the study population survived till discharge. The baseline characteristics of the ICU-survivors and non-survivors were comparable (Table 4). The median decrease in ATMLTmax was significantly greater in ICU non-survivors, compared to survivors (Mann Whitney U = 151.5, p = 0.034) (Fig. 3). No significant differences were found in other muscle parameters between ICU survivors and non-survivors (Table 5). None of the MLT and echogenicity parameters of both muscle groups correlated with the length of stay in ICU (Table 6).
The measurements of ATMLTmax is moderately reliable [ICC(2,1) = 0.663, 95% CI 0.594–0.726 p < 0.001]. The ATMLTmean and QMLT measurements have excellent reliability [ICC(2,1) = 0.893, 95% CI 0.865, 0.916, p < 0.001; ICC(2,1) = 0.992, 95% CI 0.990, 0.994, p < 0.001 respectively]. The echogenicity scores have excellent intra-rater agreement for anterior temporalis [ICC(2,1) = 0.925, 95% CI 0.905, 0.942, p < 0.001] and quadriceps femoris muscles ICC(2,1) = 0.964, 95% CI 0.953, 0.973, p < 0.001].
Discussion
This single center, prospective observational “proof of concept” study was designed to assess the feasibility of ultrasonographic assessment of anterior temporalis muscle for assessing muscle wasting in ICU. The findings of our present study suggest a significant decrease in thicknesses of anterior temporalis and quadriceps femoris in the first week of critical illness. There is, however, no correlation between the MLT of anterior temporalis and quadriceps muscle groups at baseline or the changes in their MLTs over 7 days. The echogenicity of both muscle groups correlates weakly at baseline, with no correlation seen in change in mean grayscale scores over 7 days. ICU non-survivors have significantly higher loss of maximum thickness of anterior temporalis muscle over 7 days compared to survivors.
Muscle weakness in ICU has been found to be an independent predictor of mortality [13, 14], prolonged mechanical ventilation [15, 16] and increased length of stay in ICU [17]. Lower limb muscle mass has been found to correlate with strength in healthy individuals and critically ill patients [18, 19]. Most of the studies on ultrasonographic assessment of muscle wasting involve quadriceps femoris muscle. This is the first study to assess the feasibility of using a facial muscle for assessing muscle wasting in critically ill patients. Previous studies using ultrasonographic assessment of temporalis muscle layer thicknesses were done in outpatients with brain metastasis and oral submuscosal fibrosis [12, 20]. The baseline maximum and mean thicknesses of anterior temporalis muscle in our study were approximately 7 mm and 5 mm, which were similar to the findings of previous studies. Serial measurements of anterior temporalis muscle layer thickness showed approximately 7–10% decrease over 7 days of ICU stay, depending on the method of measurement (i.e., ATMLTmax and ATMLTmean). Although statistically significant, the actual magnitude of such small changes in the thickness of a muscle whose average baseline thickness is 5–7 mm is minimal. This is a major limitation of using the serial assessment of anterior muscle layer thickness for monitoring muscle wasting.
Our study found no correlation in baseline MLT as well as the percentage changes of MLT over 7 days between the two muscle groups. These findings suggest that serial anterior temporalis muscle ultrasonography may not be ideally used in place of limb ultrasonography for assessment of muscle wasting in ICU.
Our study found no significant correlation between ICU length of stay and baseline thicknesses of either muscle groups. On the contrary, Gruther and colleagues had observed good correlation of baseline and change in quadriceps muscle mass with ICU length of stay [5]. However, the cohort of patients was different (polytrauma, cardiovascular diseases, post-transplantation etc.) and the follow up period was 28 days.
We observed significantly more decrease in ATMLT over 7 days in ICU non-survivors compared to those who survived till ICU discharge. No difference was seen in other muscle ultrasound parameters between ICU survivors and non-survivors. This is an important finding that may be explored as a hypothesis for testing in future studies.
Muscle echogenicity is higher in critically ill compared to healthy controls [8, 21]. Change in muscle echogenicity was greater in patients who developed muscle necrosis than in those who did not [22]. The present study found non-significant increase in mean echogenicity of anterior temporalis muscle over 7 days. The mean echogenicity of quadriceps femoris increased by 7.6% over 7 days. The increase in echogenicity was similar to the findings of Parry and colleagues [7]. The baseline echogenicity of the two muscle groups correlated weakly with each other. No significant correlation was seen between the changes in echogenicity of the two muscle groups over 7 days. No significant correlation of baseline echogenicity and percent change in echogenicity of both the muscle groups with ICU-length of stay were observed. The relation of muscle echogenicity with ICU outcomes such as mortality or length of stay has not been studied previously.
Sarwal and colleagues found excellent inter-observer reliability of grayscale analysis of muscle ultrasonography images for measuring muscle echogenicity of quadriceps muscles [23]. We have also observed good intra-rater agreement between mean echogenicity measurements for both the muscle groups.
Our findings are subject to several limitations. First, the enrolled patients had varying durations of hospital stay before ICU admission, which may influence the results of the study. Second, the fluid balance, nutritional risk assessment and biochemical parameters of nutrition are important factors that may influence muscle layer thickness and echogenicity. These factors were not included in data collection. Third, steroid usage, mechanical ventilation days, handgrip strength were not assessed. MRC scoring was feasible in only 18 of 48 patients at baseline, and in 23 patients at day 7 of ICU stay. Among the patients whose muscle strength could be assessed at day 7, only 1 patient had MRC score less than 48. This may limit the generalization of our result to other patient cohorts with significantly higher incidence of ICU acquired weakness.
In conclusion, measurement of ultrasonographic muscle layer thickness and grayscale parameters of anterior temporalis muscle do not show good correlation with that of quadriceps muscle. The magnitude of changes in thicknesses of a fan-shaped muscle like anterior temporalis muscle is very small and therefore, may not be accurately measurable in serial scans. Therefore, serial ultrasound of anterior temporalis muscle may not be clinically useful in monitoring muscle wasting in critically ill patients with sepsis.
References
Reeves ND, Maganaris CN, Narici MV (2004) Ultrasonographic assessment of human skeletal muscle size. Eur J Appl Physiol 91(1):116–118
Paris MT, Mourtzakis M, Day A, Leung R, Watharkar S, Kozar R et al (2017) Validation of bedside ultrasound of muscle layer thickness of the quadriceps in the critically Ill patient (VALIDUM study). JPEN J Parenter Enteral Nutr 41(2):171–180
Chi-Fishman G, Hicks JE, Cintas HM, Sonies BC, Gerber LH (2004) Ultrasound imaging distinguishes between normal and weak muscle. Arch Phys Med Rehabil 85(6):980–986
Freilich RJ, Kirsner RL, Byrne E (1995) Isometric strength and thickness relationships in human quadriceps muscle. Neuromuscul Disord NMD 5(5):415–422
Gruther W, Benesch T, Zorn C, Paternostro-Sluga T, Quittan M, Fialka-Moser V et al (2008) Muscle wasting in intensive care patients: ultrasound observation of the M. quadriceps femoris muscle layer. J Rehabil Med 40(3):185–189
Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P et al (2013) Acute skeletal muscle wasting in critical illness. JAMA 310(15):1591–1600
Parry SM, El-Ansary D, Cartwright MS, Sarwal A, Berney S, Koopman R et al (2015) Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J Crit Care 30(5):1151.e9–14
Grimm A, Teschner U, Porzelius C, Ludewig K, Zielske J, Witte OW et al (2013) Muscle ultrasound for early assessment of critical illness neuromyopathy in severe sepsis. Crit Care Lond Engl 17(5):R227
Formenti P, Umbrello M, Coppola S, Froio S, Chiumello D (2019) Clinical review: peripheral muscular ultrasound in the ICU. Ann Intensive Care 9(1):57
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810
Tillquist M, Kutsogiannis DJ, Wischmeyer PE, Kummerlen C, Leung R, Stollery D et al (2014) Bedside ultrasound is a practical and reliable measurement tool for assessing quadriceps muscle layer thickness. JPEN J Parenter Enteral Nutr 38(7):886–890
Kant P, Bhowate RR, Sharda N (2014) Assessment of cross-sectional thickness and activity of masseter, anterior temporalis and orbicularis oris muscles in oral submucous fibrosis patients and healthy controls: an ultrasonography and electromyography study. Dento Maxillo Facial Radiol 43(3):20130016
Sharshar T, Bastuji-Garin S, Stevens RD, Durand M-C, Malissin I, Rodriguez P et al (2009) Presence and severity of intensive care unit-acquired paresis at time of awakening are associated with increased intensive care unit and hospital mortality. Crit Care Med 37(12):3047–3053
Ali NA, O’Brien JM, Hoffmann SP, Phillips G, Garland A, Finley JCW et al (2008) Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med 178(3):261–268
De Jonghe B, Bastuji-Garin S, Durand M-C, Malissin I, Rodrigues P, Cerf C et al (2007) Respiratory weakness is associated with limb weakness and delayed weaning in critical illness. Crit Care Med 35(9):2007–2015
De Jonghe B, Bastuji-Garin S, Sharshar T, Outin H, Brochard L (2004) Does ICU-acquired paresis lengthen weaning from mechanical ventilation? Intensive Care Med 30(6):1117–1121
Hermans G, Van Mechelen H, Clerckx B, Vanhullebusch T, Mesotten D, Wilmer A et al (2014) Acute outcomes and 1-year mortality of intensive care unit-acquired weakness. A cohort study and propensity-matched analysis. Am J Respir Crit Care Med 190(4):410–420
Abe T, Loenneke JP, Thiebaud RS (2015) Morphological and functional relationships with ultrasound measured muscle thickness of the lower extremity: a brief review. Ultrasound Leeds Engl 23(3):166–173
Borges RC, Soriano FG (2019) Association between muscle wasting and muscle strength in patients who developed severe sepsis and septic shock. Shock Augusta Ga 51(3):312–320
Furtner J, Berghoff AS, Schöpf V, Reumann R, Pascher B, Woitek R et al (2018) Temporal muscle thickness is an independent prognostic marker in melanoma patients with newly diagnosed brain metastases. J Neurooncol 140(1):173–178
Cartwright MS, Kwayisi G, Griffin LP, Sarwal A, Walker FO, Harris JM et al (2013) Quantitative neuromuscular ultrasound in the intensive care unit. Muscle Nerve 47(2):255–259
Puthucheary ZA, Phadke R, Rawal J, McPhail MJW, Sidhu PS, Rowlerson A et al (2015) Qualitative ultrasound in acute critical illness muscle wasting. Crit Care Med 43(8):1603–1611
Sarwal A, Parry SM, Berry MJ, Hsu F-C, Lewis MT, Justus NW et al (2015) Interobserver reliability of quantitative muscle sonographic analysis in the critically Ill population. J Ultrasound Med Off J Am Inst Ultrasound Med 34(7):1191–1200
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Anirban Bhattacharjee (AB), Rahul Kumar Anand (RKA), Rajeshwari Subramaniam (RS), Dalim Kumar Baidya (DKB), Vimi Rewari (VR), and Manisha Jana (MJ). Data collection was done by AB, RA and MJ. Data analysis was done by AB, DKB, Bikash Ranjan Ray (BKR) and Puneet Khanna (PK). The first draft of the manuscript was written by AB, RA and DKB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest to declare in relation to the present study.
Funding
No funding received.
Ethical clearance
Ethical clearance was obtained from the institute ethics board, and the trial was pre-registered with the national clinical trial registry.
Trial registration number: CTRI/2018/09/015827 [Registered on: 25/09/2018].
Informed consent
Informed consent was obtained from all patients or their legal guardians.
Consent to publish
The authors affirm that participants provided consent for publication of the images in Figures 1 and 2.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anand, R.K., Bhattacharjee, A., Baidya, D.K. et al. Feasibility of anterior temporalis muscle ultrasound for assessing muscle wasting in ICU: a prospective cohort study. J Ultrasound 26, 653–661 (2023). https://doi.org/10.1007/s40477-022-00703-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-022-00703-1