Abstract
Purpose
To assess the diagnostic accuracy and inter-observer variability of ultrasound (US) in recognizing signs of intra or extra-capsular rupture of silicone breast implants by using the magnetic resonance imaging (MRI) findings as the reference standard.
Methods
150 patients for a total of 300 implants underwent breast US and subsequently MR examination searching for signs of intra or extra-capsular rupture. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy were calculated for breast US having MRI findings as the reference standard. Cohen’s kappa statistics was used in order to assess inter-observer agreement for US.
Results
170/300 (57 %) implant ruptures were detected at US (intra-capsular n = 110, extra-capsular n = 60). By comparing US findings with MR results, overall sensitivity, specificity, accuracy, PPV, and NPV of 79, 63, 70, 65, and 77 %, respectively, were found for breast US. In case of intra-capsular rupture, sensitivity, specificity, accuracy, PPV, and NPV of 63, 63, 63, 45, and 77 %, respectively, were obtained; 100 % values were found for extra-capsular rupture US diagnosis.
Conclusion
US can be used as the first examination in patients with breast implants. US intra-capsular rupture detection requires further evaluation by MRI; in case of extra-capsular rupture US diagnosis, surgical implant removal could be proposed without further investigations.
Riassunto
Scopo
valutare l’accuratezza diagnostica e la variabilità inter-osservatore dell’ecografia nel riconoscimento dei segni di rottura intra od extra-capsulare di protesi mammarie in silicone avendo i segni RM con standard di riferimento.
Metodi
150 pazienti per un totale di 300 impianti sono stati sottoposti ad ecografia mammaria e successivamente ad esame RM ricercando segni di rottura intra od extracapsulare. Sono stati calcolati i valori di sensibilità, specificità, valori predittivi positivo (VPP) e negativo (VPN) ed accuratezza diagnostica avendo i segni RM come standard di riferimento. L’accordo inter-osservatore è stato calcolato mediante test statistico kappa di Cohen.
Risultati
170/300 (57 %) rotture di impianti sono state identificate all’esame ecografico (intra-capsulari, n = 110; extra-capsulari n = 60). Sono stati ottenuti valori di sensibilità, specificità, accuratezza, VPP e VPN rispettivamente pari a 79, 63, 70, 65 and 77 %, per l’ecografia mammaria. In caso di rottura intracapsulare, sono stati ottenuti valori di sensibilità, specificità, accuratezza, VPP e VPN rispettivamente pari a 63, 63, 63, 45 and 77 %; in caso di rottura extracapsulare, sono stati riscontrati valori pari a 100 % per l’ecografia mammaria.
Conclusioni
l’ecografia mammaria può essere utilizzata come metodica di primo livello nei pazienti con protesi mammarie. In caso di diagnosi ecografica di rottura intra-capsulare, è indicato approfondimento diagnostico con esame RM; in caso di rottura extra-capsulare rilevata all’esame ecografico, è proponibile la sostituzione chirurgica dell’impianto senza ulteriori indagini diagnostiche.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Esthetic breast augmentation and breast reconstruction after mastectomy have increased requests for implant surgery [1–3]. Post-operative complications of breast implantation are mainly represented by capsular contracture and implant rupture. Implant rupture that can occur from 10 to 15 years from implantation, is rarely associated with a traumatic event and represents the most common cause of prosthesis removal [4–8]. It can be intra-capsular or extra-capsular. In case of intra-capsular rupture, implant shell is breached without macroscopic silicone leakage beyond the intact fibrous capsule. In case of extra-capsular rupture, both the implant shell and the fibrous capsule are breached, with macroscopic silicone leakage into the surrounding tissues or lymph nodes [6–14].
Implant rupture is often asymptomatic and clinical examination fails to detect it in more than 50 % of cases [1]. For these reasons, the diagnosis of implant rupture is based on imaging techniques such as mammography, ultrasound (US), and magnetic resonance imaging (MRI).
With regard to mammography and US, the former has a variable sensitivity ranging between 25 and 30 % and 68 % being unable to recognize intra-capsular rupture because of the high opacity of silicone, while the latter has a reported sensitivity and specificity, respectively, of 50–77 and 55–84 % in detecting implant rupture because it allows to recognize intra- and extra-capsular rupture signs [1–4].
MRI represents the gold standard for the assessment of implant status and the latest step before the surgery in cases of rupture [15–17]. It has a reported sensitivity and specificity of 72–94 and 85–100 %, respectively, for the diagnosis of silicone implant rupture and its accuracy is due to the high spatial and soft-tissue resolution and the ability to set the signal from water, fat or silicone. The most reliable MR sign of intra-capsular rupture is represented by the “linguine sign” which consists of curvilinear hypo-intense lines within the hyper-intense silicone filled implant due to the collapse of the implant shell in silicone gel. Other signs of intra-capsular rupture are the “teardrop sign,” “keyhole” sign, and “sub-capsular line” sign. In case of extra-capsular implant rupture, MR sequences detect the presence of silicone particles in peri-prosthetic tissues and in lymph nodes [15–17].
The aim of this study is to assess the diagnostic accuracy and inter-observer variability of US in recognizing signs of intra- or extra-capsular rupture of silicone breast implants by using the MRI findings as the reference standard.
Materials and methods
Patient population
This prospective, single-center study was carried out between January 2013 and February 2014 and included 150 patients [age range 37–69 years; mean age ± standard deviation (SD), 47.3 ± 9.2 years], for a total of 300 implants, with suspected implant rupture basing on clinical assessment (n = 54) or with ≥10 years aged implant (n = 96).
The patients underwent breast US and subsequently MR examination performed within 15 days.
All patients with positive MRI were referred for surgical implant removal. All patients with negative MRI were referred for a 6-month follow-up MR examination which confirmed implant integrity.
The study followed the principles of Helsinki declaration and was approved by the local ethics committee. Written informed consent was obtained in all cases.
US examination
US examinations were performed by using a 13 MHz probe (MicroMaxx Ultrasound System, Sonosite, Bothell, WA, US) with a radial technique.
MRI protocol
Magnetic resonance images were acquired with a 1.5-T MR imaging device (Philips, Achieva 1.5) equipped with a 4-channel-phased array coil (SENSE-body coil).
Breast MRIs were performed regardless of menstrual cycle phase, without injection of contrast medium.
As already performed in other series [16], the following sequences were obtained:
-
Axial turbo spin echo (TSE) T2-weighted images: matrix 512 × 512; FOV 350–470; scan % 75; slice number 50; thickness 3 mm; TR short (mean value 4864 ms); TE 120;
-
Axial silicone-only images: matrix 512 × 512; scan % 80; TE 70 ms; TR short (mean value 9372 ms); TI 165 ms; slice number 40–50; thickness 3 mm;
-
Axial silicone suppression images: matrix 512 × 512; thickness 3 mm; slice number 35; FOV 350–400; RFOV 60; scan % 80; TE 2.4 ms; TR 4.9 ms; and
-
Sagittal short tau inversion recovery (STIR) images: matrix 512 × 512; slice number 40; thickness 3 mm, FOV 350–400; RFV 60; TR 7500 ms, TE 70 ms; TI 160 ms.
Image analysis
Two blinded radiologists with more than 5 years’ experience in the field breast imaging performed breast US evaluating implant morphology, contour, lumen, peri-implant tissues and axillae, and searching for signs of intra or extra-capsular implant rupture as already reported in the literature [1]:
-
“stepladder sign”;
-
inhomogeneous echo-texture of implant lumen;
-
discontinuity of implant capsule; and
-
“snowstorm sign” in breast glands or in axillary lymph nodes.
MR images were evaluated searching for the presence of clear signs of intra or extra-capsular implant rupture, as already reported in the literature [1]:
-
linguine sign;
-
“teardrop” sign;
-
“keyhole” sign; and
-
the presence of siliconomas and free silicone particles.
Statistical analysis
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy were calculated for breast US having MRI findings as the reference standard. Cohen’s kappa statistics was used in order to assess inter-observer agreement for US: poor concordance (κ = 0.01); low concordance (κ = 0.01–0.20); moderate concordance (κ = 0.21–0.40); good concordance (κ = 0.41–0.60); substantial concordance (κ = 0.61–0.80); and almost perfect concordance (κ = 0.81–1.00).
All calculations were performed using NCSS2007® statistical software.
Results
All the examined 300 breast implants were represented by single lumen silicone implants.
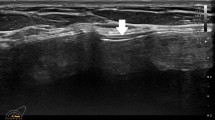
At US examination, 170 out of 300 (57 %) implant ruptures were detected, intra-capsular in 110 cases (65 %), and extra-capsular in 60 (35 %). In particular, intra-capsular rupture signs were represented by the stepladder sign in 92 cases (84 %) (Fig. 1) and inhomogeneous echo-texture of implant lumen in 18 (16 %). Among the 60 cases of extra-capsular rupture, the snowstorm sign was identified in all cases (Fig. 2a, b), and the detection of a discontinuity of the implant capsule was associated in 15 cases (25 %).
130 out of 300 (43 %) breast implants showed no rupture sign at US examination and were considered as intact prostheses.
At MRI examination, 140 (47 %) implants resulted to be damaged; in particular, in 80 out 140 (57 %) intra-capsular rupture signs were detected, while in the remaining 60 (43 %) extra-capsular rupture was diagnosed.
160 out of 300 (53 %) implants resulted to be intact at MRI.
By comparing US findings with MR results, overall sensitivity, specificity, accuracy, PPV, and NPV of 79, 63, 70, 65 and 77 %, respectively, were found for breast US.
In particular, US diagnosis of extra-capsular rupture was confirmed by MRI in all cases with 100 % values of sensitivity, specificity, accuracy, PPV, and NPV for breast US.
On the contrary, in case of intra-capsular rupture, 110 true positives, 60 false positives, 100 true negatives, and 30 false negatives occurred in our series by considering US examination. Therefore, the previous values referring to sensitivity, specificity, accuracy, PPV, and NPV decreased to 63, 63, 63, 45, and 77 %, respectively.
Almost perfect agreement between the two radiologists was found for US with a k value of 0.87 in our series.
Discussion
Breast US represents a valid tool and a first level technique for evaluating implant integrity. In fact, it results non-invasive, cheap, easily available, and well accepted by patients. It is usually performed by using a linear array transducer centered at 7.5 e 13 MHz with the patient in the supine and oblique position in order to examine respectively, medial and lateral quadrants of the breast [1, 15].
US implant examination includes the evaluation of implant morphology, shell and lumen, peri-prosthetic tissues, and axillae. The most reliable sign of implant integrity is represented by an anechoic lumen with a hyper-echoic linear shell. However, the normal infoldings of the implant membrane into the silicone gel, known as radial folds, often produce echogenic lines that extend perpendicularly from the periphery to the implant lumen [1, 14, 15].
Signs of intra-capsular rupture are represented by the “stepladder sign,” which consists of horizontal echogenic straight or curvilinear lines traversing the implant lumen, and by the inhomogeneous echo-texture of implant lumen probably due to influx of body fluids that mix with silicone. However, low-level echoes within the implant lumen may also be seen in intact silicone implants and should be interpreted with caution [1, 15, 18]. In our series, the “stepladder sign,” which is reported to be the most reliable US sign of intra-capsular rupture in the medical literature, occurred in 84 % of cases diagnosed as intra-capsular rupture; however, it provided correct information about the implant state in 54 % of cases. With regard to the “stepladder sign,” a sensitivity and specificity of 63 and 74 %, respectively, were found in our experience.
On the other side, accordingly to previous data reported in the literature, in our series, the inhomogeneous echo-texture of implant lumen does not represent a reliable sign of implant rupture; in fact, it was found in 16 % of cases suspected of having intra-capsular rupture at US examination and not confirmed by MRI in all cases.
US signs of extra-capsular rupture are represented by the “snowstorm sign” and by the discontinuity of implant capsule. The “snowstorm sign” is reported to be statistically significant for extra-capsular rupture and as the most sensitive and specific sign at US. It consists of hyper-echoic nodules with a well-defined anterior margin and dirty incoherent posterior shadowing which may be located within the breast tissue or the axillary lymph nodes. The nodules consist of silicone granulomas, composed of free silicone particles and surrounding fibrous tissue reaction, lying outside the fibrous capsule [1, 15, 18]. In our series, US allowed to diagnose extra-capsular rupture in all cases by recognizing the “snowstorm sign” in all cases and implant capsule discontinuity in 25 %.
The main limitations of US assessment of breast implant are the reverberation artifacts in the anterior part of the implant and the marked attenuation of the US beam by silicone which does not allow to evaluate the posterior wall of the prosthesis [1, 18].
In our series, US showed overall sensitivity, specificity, and accuracy values of 79, 63, and 70 %, respectively, in recognizing implant rupture signs. In particular, in case of extra-capsular rupture, a 100 % diagnostic accuracy was obtained for US diagnosis. On the contrary, in case of intra-capsular rupture, the previous values referring to sensitivity, specificity, accuracy, PPV, and NPV decreased to 63, 63, 63, 45, and 77 %, respectively, for US examination. In fact, thirty false negative cases at US included 18 implants with intra-capsular rupture signs mainly localized along the posterior implant wall and by 12 implants with minimal detachment of the implant shell from the fibrous capsule. Sixty false positive cases at US were represented by implants with complex radial folds mimicking intra-capsular rupture in 42 cases and by inhomogeneous content in 18, not confirmed by the subsequent MRI control.
Our data resulted to be consistent with Di Benedetto et al. who reported a sensitivity and specificity, respectively, of 77 and 69 % for US diagnosis of implant rupture. In fact, they concluded that US is a very specific method in detecting extra-capsular rupture, which is less frequent but represents an absolute indication for surgical removal. However, they proposed MRI not only in those cases where US yields suspicious or inconclusive results, but also in case of detection of intra-capsular rupture at mammography and US because of their low specificity [15].
In our experience, US detected extra-capsular rupture in all cases, while in case of suspected intra-capsular rupture, a sensitivity and specificity of 63 % were found. Therefore, in case of extra-capsular rupture US diagnosis, MRI could be avoided and surgical implant removal could be directly performed, while in case of US intra-capsular rupture signs, MRI should be performed in all cases in order to confirm diagnosis.
Finally, the almost perfect agreement between the two radiologists was found in our series confirming the reliability of the US examination in this field.
However, our study has some limitations, mainly represented by the relatively small size of the examined sample; the occurrence of only single lumen silicone gel implants; the lack of a true gold standard because of the use of a 6-month follow-up MR as a negative confirmation. Besides, the presence of symptomatic patients in our sample could represent a selection bias because the sensitivity and specificity on a symptomatic sample have been shown to be higher in comparison with studies using an asymptomatic sample.
Therefore, further studies are needed in order to evaluate the diagnostic accuracy of US in detecting rupture signs on different kinds of implants, such as double lumen or saline-filled implants.
In conclusion, US can be used as the first examination in the follow-up of patients with breast implants. The US detection of intra-capsular rupture requires further evaluation by means of MRI which represents the most sensitive technique in this field. In case of extra-capsular rupture US diagnosis, surgical implant removal could be proposed without further investigations.
References
Juanpere S, Perez E, Huc O et al (2011) Imaging of breast implants-a pictorial review. Insights Imaging 2:653–670
Frank S, Mahdi R, Sherko K (2010) Imaging in patients with breast implants-results of the First International Breast (Implant) Conference 2009. Insights Imaging 1:93–97
Colombo G, Ruvolo V, Stifanese R et al (2011) Prosthetic breast implant rupture: imaging-pictorial essay. Aesthetic Plast Surg 35:891–900
Yang N, Muradali D (2011) The augmented breast: a pictorial review of the abnormal and unusual. Am J Roentgenol 196:W451–W460
Hölmich LR, Fryzek JP, Kjøller K et al (2005) The diagnosis of silicone breast-implant rupture clinical findings compared with findings at magnetic resonance imaging. Ann Plast Surg 54:583–589
Hölmich LR, Hölmich LR, Friis S et al (2003) Incidence of silicone breast implant rupture. Arch Surg 138:801–806
Hölmich LR, Vejborg IM, Conrad C et al (2005) The diagnosis of breast implant rupture: MRI findings compared with findings at explantation. Eur J Radiol 53:213–225
Hölmich LR, Vejborg IM, Conrad C et al (2004) Untreated silicone breast implant rupture. Plast Reconstr Surg 114:204–214
Herborn CU, Marincek B, Erfmann D et al (2002) Breast augmentation and reconstructive surgery: MR imaging of implant rupture and malignancy. Eur Radiol 12:2198–2206
Tark KC, Jeong HS, Roh TS et al (2005) Analysis of 30 breast implant rupture cases. Aesthetic Plast Surg 29:460–469
Gorczyca DP, Gorczyca SM, Gorczyca KL (2007) The diagnosis of silicone breast implant rupture. Plast Reconstr Surg 120(suppl1):49S–61S
Glynn C, Litherland J (2008) Imaging breast augmentation and reconstruction. Br J Radiol 81:587–595
Berg WA, Berg WA, Nguyen TK et al (2002) MR imaging of extracapsular silicone from breast implants: diagnostic pitfalls. Am J Roentgenol 178:465–472
Handel N (2007) The effect of silicone implants on the diagnosis, prognosis, and treatment of breast cancer. Plast Reconstr Surg 120(suppl1):81S–93S
Di Benedetto G, Cecchini S, Grassetti L et al (2008) Comparative study of breast implant rupture using mammography, sonography, and magnetic resonance imaging: correlation with surgical findings. Breast J 14:532–537
Moschetta M, Telegrafo M, Capuano G et al (2013) Intra-prosthetic breast MR virtual navigation: a preliminary study for a new evaluation of silicone breast implants. Magn Reson Imaging 31(8):1292–1297
Maijers MC, Niessen FB (2012) Prevalence of rupture in poly implant prothèse silicone breast implants, recalled from the European market in 2010. Plast Reconstr Surg 129(6):1372–1378
Bassetti E, Pediconi F, Luciani ML et al (2011) Breast prosthesis: management of patients after plastic surgery. J Ultrasound 14(3):113–121
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. All patients provided written informed consent to enrollment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Telegrafo, M., Moschetta, M. Role of US in evaluating breast implant integrity. J Ultrasound 18, 329–333 (2015). https://doi.org/10.1007/s40477-015-0170-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-015-0170-5