Abstract
Purpose of Review
Autism is a lifelong neurodevelopmental condition characterised by differences in social interaction and communication across multiple contexts, as well as restricted, repetitive patterns of behaviour or interests. As all adults age, they face an appreciable decline in health and functioning. For autistic adults, the challenges are twofold: they may face autism-specific effects of ageing as well as other non-specific, age-related effects experienced by the general population. This report summarises the available literature regarding older autistic adults over the age of 50, from 2010 to mid-2019.
Recent Findings
Emerging evidence suggests that older autistic adults experience complex physical and mental health comorbidities. Studies that have included older adults report challenges such as underemployment, a lack of appropriate healthcare, and concerns for caring relationships as the adult ages. However, these studies have tended to be skewed towards younger and middle-aged adults.
Summary
Overall, there is a notable lack of studies that focus on older autistic adults and on ageing-relevant topics, with a particular absence of the autistic voice in the research. Resultantly, there remains a gap in our knowledge regarding the specific circumstances and needs of autistic adults in older age. In moving forward, it will be important to fill this gap with inclusive research to guide the most relevant and effective work that improves outcomes for this population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD or autism) is a neurodevelopmental condition characterised in the fifth revision of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5) by persistent deficits in social communication and social interaction across multiple contexts, as well as restricted, repetitive patterns of behaviour, interests or activities that are not better explained by intellectual disability or global developmental delay [1]. Those on the spectrum vary widely in their levels of functioning and intellectual ability with high reported rates of comorbid intellectual disability [2]. Whilst estimates have varied slightly, the most widely accepted prevalence of ASD in Western countries is approximately 1% in individuals of all ages [3, 4], with a notable increase from figures published around and before the 1990s. Studies have reliably documented a greater prevalence of ASD in males than in females, with a ratio of 3:1–4:1 cited most frequently in literature [5], though there has been an increasing suggestion of under-diagnosis in females for reasons such as ‘camouflaging’ or ‘masking’ symptoms [6]. Overall, studies concur with the lifelong nature of autism. Studies following children on the autism spectrum into adolescence and beyond find both improvement and stability in the core social and behavioural phenotype of autism, with most studies reporting either improvement or stability over time [7,8,9,10]. Despite this, there is a notable lack of robust research and supports available for autistic individuals beyond early adulthood [11•] .
As all adults age, they face an appreciable decline in health and functioning [12•]. Autistic adults may face specific challenges arising from ageing with autism, as well as other non-specific, age-related effects experienced by all adults. However, the majority of research and research expenditure has focused on early years, such as the genetic underpinnings of autism and early intervention [13••]. A 2016 systematic review found only twelve published articles exclusively examining older adults on the autism spectrum [14]. The oldest article was published in 2013, indicating the recency of interest. This is most likely due to the relative ‘newness’ of autism, which was first described by an Austrian paediatric psychiatrist Leo Kanner in 1943 [15] and first recognised in the third edition of the DSM as ‘infantile autism’ in 1980 [16]. Thus, the first cohorts of children diagnosed with ASD are now beginning to enter older adulthood.
This report summarises the available literature regarding older autistic adults from 2010 to mid-2019. The World Health Organization defines an ‘older person’ as one who has passed their median life expectancy at birth. For those on the spectrum, median life expectancy has been reported to be 50 for those with comorbid intellectual disability (ID) and 58 for those without ID [17]. This finding was reported in a 2015 Swedish study, which is the largest and only available population-based study reporting age of death for autistic individuals across the lifespan (n = 27,122) compared with the general population (n = 2,672,185). At present there are no comparable studies for other countries. This report therefore focuses on autistic adults aged 50 years or older.
The present report focuses on two ‘groups’ of literature regarding older autistic adults. The first group of studies describes the autistic adult and their life, such as their lifestyle, health, employment outcomes and experiences. A second group speaks to the emerging needs in research for adults on the spectrum, such as development and validation of measurement tools, health and care toolkits and other commentary. Studies that attempt to understand the neurological and biological differences that may characterise adults on the spectrum, such as differences in brain volume or differences in perception, are not a focus of this report. After a summary of the findings, we offer some thought around the existing body of literature for this population, as well as some key issues and challenges to be considered in moving forward.
We acknowledge ongoing discourse around appropriate terminology when referring to those with a diagnosis of autism (e.g. ‘autistic adult’ versus ‘adult with autism’). Debate on this topic is likely to persist, with preferences differing both between and within groups [18]. Mindful of these debates, we use the terms ‘autistic’ and ‘on the spectrum’ interchangeably throughout the present report.
What We Know
Autism Symptoms in Later Life
Autism is generally accepted to be a lifelong condition. Most studies that investigate the relationship between autism symptoms and age have followed children through to adolescence and early adulthood [7]. These findings generally report stability in symptoms, with some evidence of a modest decrease in symptoms as individuals get older. Very few studies of this kind have included older adults.
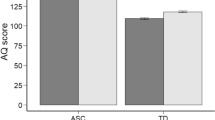
One longitudinal study of a clinical sample of 60 autistic adults (age range 29–64 at follow-up) reported a marginally significant decrease in overall autism quotient (AQ) scores over a mean follow-up of 37.5 years (SD = 9), with a significant decrease in restricted and repetitive behaviours [19]. On the other hand, a cross-sectional investigation (n = 562) of AQ scores for autistic adults aged 18 and over reported no difference in total or subscale scores across age groups (18–30, 30–40, 40–50 and 60+) [8]. One other cross-sectional survey by Hwang and colleagues [9] reports a significant negative association between age and repetitive behaviours for their sample according to the Adult Repetitive Behaviours Questionnaire-2 (n = 176; Mage = 41.7, range 25–78). Overall, these studies suggest similar findings to that of younger age groups; that autistic individuals retain their self-reported autism traits into older adulthood, with some decrease observed particularly in restricted and repetitive behaviours.
Autism is recognised and diagnosed based on observed behaviour, and it is difficult to conclude whether declines in symptoms such as repetitive behaviours necessarily indicate a decrease in autism or autistic tendencies, or a decline in the expression of these. Studies involving younger autistic individuals report that these behaviours may be masked by the individual to be more socially acceptable or be suppressed as a result of targeted therapies earlier in life [20,21,22]. For example, in one study exploring experiences of autism acceptance in a sample of 111 adults (age range 18–72, mean age = 36.4 years), participants reported ‘masking’ or ‘camouflaging’ their autism in order to appear neurotypical [18]. Another qualitative study interviewed 92 autistic adults (age range 18–79) regarding the nature of their camouflaging, which was described by participants as a combination of ‘masking’ and compensation. Reasons for camouflaging were ‘fitting in’ and ‘connecting with others’, whilst consequences were ‘exhaustion’, ‘challenging stereotypes’ and ‘threats to self-perception [22].
Autistic Identity and Late Diagnosis
Increasing public awareness of autism, more understanding of the presentation of autism in females [23] and identification of autism in cases with less pronounced autism traits [24] are potentially related to the increasing numbers of adults being diagnosed with autism. References have been made to a ‘lost generation’ [25] of autistic adults who have likely never been identified or diagnosed due to the lack of understanding of the condition during their childhood. A lack of specialist diagnostic services to manage the amount of individuals needing an adulthood diagnosis has led to the UK National Institute for Health and Care Excellence (NICE) guidelines suggesting the AQ measure be used to screen potential cases, though research highlights a large false-negative rate in adopting this approach [26]. Literature is emerging that documents the experiences of those adults who receive a late diagnosis, though it is primarily qualitative in nature and does not separate the experience specifically to those diagnosed in late adulthood. In general, based on interview (n = 13 to 25) or survey research (n = 74 to 128), there appears to be a positive impact and relief from receiving a diagnosis of autism in adulthood [27,28,29,30,31], with adults gaining a new understanding and re-interpretation of their life experiences. However, some have negative responses mostly related to a lack of support services and regret at not being diagnosed earlier.
A positive acceptance and identification with autism diagnosis is important, as it may impact on mental health [20, 32]. Bachmann et al. [33] found the internalised stigma of autistic adults without intellectual disability to be higher in their 35+ year old group, though overall less than the internalised stigma of adults with psychiatric disorders. Autism advocacy and the neurodiversity movement [34] may assist in more autistic adults building a positive self-identity.
Physical Health
Studies documenting the physical health and functioning of older adults on the spectrum have consistently reported high numbers of medical morbidities and poorer health outcomes compared with those from the general population. However, only a few have included focused investigations of older adults, and their comparative health relative to the general population. One recent investigation explore the self-reported general health status of a sample of 6649 autistic adults (18 years or older), which included 1405 adults over the age of 55 identified via 2011 Census data from Scotland [35]. This study found a self-rating of ‘bad’ or ‘very bad’ in response to the question: ‘How is your health in general’ (as opposed to ‘very good’, ‘good’ or ‘fair’) in a higher proportion of autistic adults aged 55 and over (24.6–29.5%), compared with those from the general population of the same age (10.5–13.7%). The study further reported that the influence of being autistic on self-reported poor health was greater than the influence of older age.
Another investigation of Medicaid claims for a sample of 154 adults on the spectrum aged between 40 and 88 reported a high prevalence of immune conditions (70.2%) and sleep disorders (85.3%) in their sample [36]. Contrastingly, one study of health conditions and functional status for 255 adults (18+) who completed Rochester Health Status Survey version IV reported significantly elevated rates of neurologic conditions, but no difference in gastrointestinal disorders between autistic and non-autistic adults aged 40 or over [37]. Finally, a widely cited examination of a population of 1507 health-insured adults from the USA, including 143 (9.5%) who were aged 50 or older, reported significantly higher rates of common chronic health conditions in those on the spectrum, such as hypertension, dyslipidaemia and diabetes [38]. Whilst a comparison of rates for these conditions between older non-autistic and autistic adults is not specifically available, the higher rates, even in early adulthood, will have ongoing implications as these adults age.
There is a lack of robust research examining the rates and progression of health conditions that are commonly related to older age in adults on the spectrum, with existing studies highly limited by small sample sizes. One study comparing the presence of medical comorbidities in younger (age < 50, n = 34) versus older (age 50+, n = 40) adults on the spectrum found no significant differences in the proportion of their sample who had conditions commonly associated with older age, including hypertension, hypothyroidism, urinary incontinence, liver disease, renal disease and cardiovascular disease [39]. In general, studies report comparable rates of osteoporosis, cancer, lung disease and circulatory conditions between those on the spectrum and those from the general population [38]. Another study reported Parkinsonism to be present in 20% of a sample of 37 adults on the spectrum over 39 years [40].
Overall, these studies report that autistic adults aged 40 years or older tend to experience higher rates of many, but not all common health conditions compared with those from the general population. Moreover, studies that specifically examine conditions that are related to older age, such as urinary incontinence, tend to report comparable rates in both autistic and non-autistic populations. Larger, representative studies of older autistic adults and their physical health are still needed. Given this, existing studies indicate that further understanding of physical health and management of comorbidities is a priority for autistic adults from middle age onwards.
Cognition
A considerable proportion of studies have focused on neurobiology and cognitive functioning in autistic adults. These studies have tended to focus on cognition and perception. Very few studies have specifically examined declines in cognitive functioning with no studies identified to document rates of dementia in older autistic adults. The existing handful of studies suggests that, when compared with non-autistic adults, older autistic adults perform poorly on some cognitive tasks and better on other tasks, with cognitive decline occurring differently for different cognitive processes.
One cross-sectional study, including 57 autistic adults (50–79 years old) and 56 non-autistic controls of the same age, reported more cognitive impairment in the autistic adults. However, autistic adults had higher visual memory and immediate recall than non-autistic adults [41]. Another study involving a small sample of middle-aged males (n = 16, age range = 40–64) with ‘high-functioning’ autism spectrum disorder also reported poorer executive functioning but similar verbal memory and visual search to a sample of age-matched controls (n = 17) [42]. In a third cross-sectional study, which did not focus on older autistic adults (n = 29 age range 30–67 years), age was a significant predictor of poorer performance on cognitive tasks, and autistic adults performed more poorly compared with a sample of age-matched non-autistic controls [43]. However, this study also found that the effect of age on specific cognitive processes differed for autistic adults. For example, older age had a disproportionate effect on cognitive flexibility, whilst learning was not significantly affected by age. Free recall and processing speed declined with age in a manner similar to that observed in non-autistic adults.
These findings suggest that age may affect different areas of cognitive functioning in autistic adults differently. Further study involving older adults specifically are needed to understand the specific strengths and difficulties that autistic adults may experience in cognition, compared with those from the general population.
Mental Health and Psychological Well-being
A limited number of studies of mental health and psychological well-being have included older autistic adults, and fewer have focused on older age groups specifically. Most studies involve age ranges that are skewed towards younger adults, with only small proportion of older adults in their sample [44,45,46]. Given this, findings are mostly consistent in reporting higher lifetime rates of psychiatric comorbidities for autistic adults of all ages compared with that of adults from the general population [38, 44, 45, 47,48,49]. In these studies, elevated lifetime rates of major depressive disorder, anxiety, social phobia and obsessive-compulsive disorder are reported. Also reported is a significantly higher proportion of autistic adults in Australia (n = 188, age range 25–80) versus non-autistic adults (n = 115, age range = 25–70) who take at least one psychotropic medication (adjusted OR = 4.54, 95% CI 2.26–9.10) even after adjusting for any psychiatric or neurologic diagnosis.
A few studies do include a focus on middle-aged to older autistic adults. One study specifically examining Medicaid claims for 143 middle-aged and older autistic adults (age range 40–88) reported a 72% prevalence of psychiatric disorders with no statistical difference in these rates between those with and without comorbid ID [36]. Another study of psychiatric comorbidities and medication use in 601 older autistic recipients of disability services aged 55 or older reported over 60% to have had contact with psychiatric care in 2012, the most common diagnoses being affective disorders, anxiety and psychotic disorders [50•]. One study specifically investigated self-reported anxiety and depression in autistic adults ranging from adolescence to older adulthood (n = 255; mean age = 33.52 years) from Australia reporting high rates of clinically significant anxiety (38.4%) and depression (38%) in their sample [51]. A 2019 meta-analysis exploring specifically anxiety and depression in adults on the spectrum identified 35 published studies [52]. Whilst eleven of these studies specifically report their sample age range to include adults over 50, the studies tend to be skewed towards younger adults, with mean age of samples within the mid-twenties to mid-thirties. None of the studies had a focus exclusively on middle-aged or older adults. This review reported a pooled prevalence of 37% and 42% for lifetime depression and anxiety, respectively.
Studies that have focused on the presentation of psychiatric comorbidities in autistic adults across different age groups have differing results regarding the prevalence of these conditions throughout the lifespan. A German study (n = 50) found that autistic adults 40 years old or older had more psychiatric comorbidities compared with those under 40 [46], whilst another Australian study (n = 255) found no significant differences in rates of anxiety and depression between adolescents (15–21 years old), younger (22–39 years old) and middle-aged adults (40–64 years old), and those over 65 years old [51]. Yet another study involving 172 Dutch adults on the spectrum (range 19–79 years) and 172 controls found that whilst elevated lifetime rates of psychiatric conditions were evident in autistic adults versus controls of all ages, older autistic adults (55 years or older) were significantly less likely to meet diagnostic criteria for a psychiatric condition compared with younger ones [47]. A notable decline in the prevalence of social phobia is reported in this study.
Of particular note is the appreciable number of studies that consider issues relating to suicidality and self-harm in autistic adults of all ages. Whilst large robust studies of older adults on this issue remain lacking, a handful of studies have reported heightened risk of self-injury and suicidal ideation for autistic adults versus non-autistic adults in samples that do include older adults [53,54,55]. One clinical cohort study of 374 adults diagnosed with Asperger’s syndrome reported suicidal ideation in 7 of its 9 (78%) adults over 55 years of age, and 29 of its 41 (71%) adults between 45 and 54 years of age [53]. This rate is notably higher than studies from the general population. One study suggests depression and suicidal ideation are similar in younger and older age groups [53], which differs from the findings discussed above in which other psychiatric conditions appear to decline in older adulthood. This suggests that suicidal ideation in older autistic adults may not necessarily co-occur with depression, which is commonly associated with suicidality. However, it is difficult to draw conclusions given the lack of existing research. Specific investigations exploring correlates, causal factors and especially qualitative investigations of self-harm and suicidality in older autistic adults will be needed to further clarify this. A clearer understanding of the specific trajectory of depression in autistic adults as they get older will also be useful in understanding self-harm and suicidality in older autistic adults.
Employment
No studies focused specifically on the employment experiences and needs of autistic adults over the age of 50. Generally, whilst autistic adults often meet the education requirements for employment and express a willingness to work, they are disadvantaged and face obstacles in the labour market. Underemployment is a pervasive issue in adults with autism, with unemployment rates in studies consistently reported to be around 30–40% [56•, 57, 58].
Common obstacles identified to being employed and maintaining employment include difficulty with job interviews, uncertainty about which jobs to apply for and transportation [56•, 59]. Research specific to older adults emphasises the need for ongoing supervision and support in places of employment, possibly to assist in navigating these employment-related difficulties. A study of 74 autistic adults, majority of whom were older than 50 years, found that nearly two-thirds of participants required staff supervision to allow them to remain at their current work [60].
Social Support and Connectedness
Studies indicate that autistic adults often have satisfying social relationships, though this has not been explored specifically with regards older autistic adults. Generally, autistic adults’ perceptions of their social support can be quite varied and are shaped by their personal experiences [61•]. In a study of female autistic adults with low support needs, 80% described themselves as ‘very satisfied’ or ‘fairly satisfied’ with their social lives [62]. Social media may have a role in this, as autistic adults who use social networking sites were found more likely to have close friends [63], though there is no data on the prevalence of social media use in older adults specifically.
Establishing social relationships often comes with unique challenges for autistic adults. Autistic individuals highlight that the desire to increase their connections with others often drives them to camouflage or ‘mask’ their autistic traits, which many find compromise their sense of authenticity [22, 64, 65]. In a comparison study, autistic adults were more likely than non-autistic participants to report being teased, emotionally bullied and sexually victimised, indicating that they may be more vulnerable to social exclusion than non-autistic individuals [65, 66]. Despite their general satisfaction with their social relationships, loneliness is a common experience amongst autistic adults, and this has been attributed to social communication difficulties and dissatisfaction with support [61•]. The unique challenges that older autistic adults face in maintaining social connectedness and social satisfaction have yet to be explored.
Transport Use
No studies regarding transport use were found to include or focus on older autistic adults, who may face added difficulties in driving and making use of public transportation given the increase in physical limitations that occur with ageing. These may be compounded by the sensory sensitivities and difficulties in motor skill execution they experience.
Healthcare
No study has been identified that specifically addresses older autistic adults’ access to healthcare resources, and no existing studies have included participants over the age of 64. This indicates that the experiences of elderly autistic adults, who may have a greater number of comorbidities and subsequent care needs, are not adequately represented.
Generally, autistic adults make use of a wide variety of healthcare services, including the emergency department, primary care, allied health, and various primary care services [67]. One study examining Nationwide Emergency Department data from the USA reported autistic adults (age range 22–64) to make 2.3 times more visits to the emergency department than non-autistic adults [68]. Unfortunately, they also face more barriers to healthcare, particularly regarding communicating with health practitioners [69•, 70•, 71]. Other barriers include providers’ lack of knowledge on autism, the accessibility of healthcare facilities and the stigma surrounding autism [69•]. Further studies are necessary to determine whether these observations are representative of the experiences of older autistic adults and whether their patterns of healthcare use differ from younger autistic adults.
Carers
Some, albeit not all, older adults on the autism spectrum will require differing levels of formal and informal care as they age, particularly as they may have an increased need for physical and mental health assistance. Informal carers are likely to be spouses or siblings of similar age but may also be children of the autistic adult. A recent systematic review regarding carers of autistic adults found that, whilst several studies have included carers of autistic adults aged > 50 in their sample, none were specifically focused on the carers of older autistic adults [72••]. The mean age of the autistic adult in these studies ranged from 25 to 39 years old, so they are not likely to reflect the unique concerns of proving care to an older autistic population.
However, universal themes for those who support autistic adults were explored. These included the quality of the caring relationship and adaptive skills of the adult being cared for. In particular, anxieties about the future of their autistic care recipient are reported in many of the qualitative interview studies, with siblings and parents of autistic adults expressing concerns regarding where their care recipient would reside, whether appropriate formal supports would be available to them and the autistic adult’s quality of life [73,74,75,76,77].
Studies focused specifically on carers of older autistic adults are lacking but are necessary to understand the concerns and experiences specific to caring for ageing autistic individuals. Differences between carer groups, such as between the spouses and children of autistic adults, also require further study, as different relationship dynamics may lead to different concerns arising in their role as carers.
Moving Forward in Research with Older Autistic Adults
In recent years, a general lack of research examining adults on the spectrum has caught the attention of researchers, families and national organisations, with a notable increase in the amount of literature dedicated to this population. A number of editorials have called for attention to ageing research specifically [78,79,80,81] and the lack of inclusion of autistic perspectives in research [82]. Special issues dedicated to adulthood have emerged in prominent autism journals, as have dedicated research programmes and interest groups within national and international organisations, such as the Australian Cooperative Research Centre for Living with Autism (Autism CRC) and the International Society for Autism Research (INSAR) [83]. Most recent has been the establishment of a journal dedicated to adulthood, Autism in Adulthood.
At present, considerable further research efforts are needed to create a robust understanding of the circumstances, experiences and needs of older autistic adults. Whilst some studies have included adults over the age of 50, the vast majority of studies do not focus on older adults. That is, whilst their inclusion criteria include adults of all ages (18+), the mean age was predominantly in the late twenties and early thirties, with only a few of the sample being over 50 years of age, and rarely with results presented stratified by age group. On occasion, older autistic adults are even excluded from analyses due to small numbers. Rarely is there a focus on ageing-specific topics or on the experiences of older autistic adults and studies that purposively sample older adults are scarce. A lack of robust knowledge may serve as a precursor to a lack of appropriate and adequate services for this population as they age [84]. Therefore, it is timely and important to attend to this paucity of information.
The present review has shed light on a number of areas where knowledge is particularly urgent and/or lacking. These include areas of health and functioning that are commonly researched in older non-autistic adults, such as aged care, dementia, healthcare use, cognitive decline, retirement and social connectedness. Other areas that may specifically affect well-being and quality of life for older autistic adults include their public transport use and associated sensory challenges, ageing as an autistic parent, experiences of receiving care and rights to autistic-friendly environments. Given the complex physical and mental health comorbidities present in this population, it will also be important to understand the service and health needs of this population, and the specific challenges that are present during the older autistic adult’s dealings with healthcare systems and professionals.
Several challenges will be present in furthering research with this population. As discussed, these may include appropriate diagnosis of older adults. This must be preceded by a better understanding of the presentation of autism in adulthood, as well as careful consideration of the barriers to receiving a diagnosis, which may outweigh the perceived benefits for adults in old age. Also, identification of such adults for research, especially in the case that they do not have a formal diagnosis, may be particularly challenging. Relatedly, it may therefore be preferable to include, rather than exclude in research, those older adults who self-identify as autistic and to use appropriate screening or assessment tools to ensure validity of the results.
In autism research generally, there has been a movement towards inclusive research, which values and represents the ‘autistic voice’. This involves having autistic adults closely involved in research processes, as advisors, co-producers, co-authors or presenters of the research [85•]. Some groups such as Academic Autism Spectrum Partnership in Research and Education (AASPIRE) [85•] have published practical guidelines regarding this. Older autistic adults will have rich lived experience and will be an important voice to be heard in determining priorities for future research for this population. The autistic voice will be particularly relevant for topics which entail sensitivities that require the guidance of those with lived experience, such as choices regarding residential care, suicidal ideation and healthcare.
Conclusion
Research on older autistic adults and on ageing-relevant topics is lacking, including in areas where research is already readily available regarding older non-autistic adults (e.g. cognitive functioning and social connectedness). There is also a clear absence of the autistic voice in this research. Resultantly, little is known regarding the specific circumstances and needs of autistic adults in older age. To improve outcomes for this population, inclusive research is needed to guide the establishment of effective interventions that are based on input from autistic adults.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. Neurodevelopmental disorders. 5th ed. Diagnostic and Statistical Manual of Mental Disorders. 2013.
Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107–14. https://doi.org/10.1016/j.ridd.2009.06.003.
Brugha TS, Spiers N, Bankart J, Cooper S-A, McManus S, Scott FJ, et al. Epidemiology of autism in adults across age groups and ability levels. Br J Psychiatry. 2016;209(6):498–503. https://doi.org/10.1192/bjp.bp.115.174649.
Elsabbagh M, Divan G, Koh Y-J, Kim YS, Kauchali S, Marcín C, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. 2012;5(3):160–79. https://doi.org/10.1002/aur.239.
Halladay AK, Bishop S, Constantino JN, Daniels AM, Koenig K, Palmer K, et al. Sex and gender differences in autism spectrum disorder: summarizing evidence gaps and identifying emerging areas of priority. Mol Autism. 2015;6(1):36. https://doi.org/10.1186/s13229-015-0019-y.
Baldwin S, Costley D. The experiences and needs of female adults with high-functioning autism spectrum disorder. Autism. 2016;20(4):483–95. https://doi.org/10.1177/1362361315590805.
Howlin P, Magiati I. Autism spectrum disorder: outcomes in adulthood. Curr Opin Psychiatry. 2017;30(2):69–76.
Siebes R, Muntjewerff JW, Staal W. Differences of symptom distribution across adult age in high functioning individuals on the autism spectrum using subscales of the Autism Spectrum Quotient. J Autism Dev Disord. 2018;48(11):3939–44. https://doi.org/10.1007/s10803-018-3657-z.
Hwang YI, Arnold S, Srasuebkul P, Trollor J. Understanding anxiety in adults on the autism spectrum: an investigation of its relationship with intolerance of uncertainty, sensory sensitivities and repetitive behaviours. Autism. 2019. https://doi.org/10.1177/1362361319868907.
Richler J, Huerta M, Bishop SL, Lord C. Developmental trajectories of restricted and repetitive behaviors and interests in children with autism spectrum disorders. Dev Psychopathol. 2010;22(1):55–69. https://doi.org/10.1017/S0954579409990265.
• Robison JE. Autism prevalence and outcomes in older adults. Autism Res. 2019;12(3):370–4. https://doi.org/10.1002/aur.2080Thoughtful commentary regarding the need for and challenges in research with older autistic adults.
• Diehr PH, Thielke SM, Newman AB, Hirsch C, Tracy R. Decline in health for older adults: five-year change in 13 key measures of standardized health. J Gerontol A Biol Sci Med Sci. 2013;68(9):1059–67. https://doi.org/10.1093/gerona/glt038One of very few studies that observe change in time for older adults using key standardized health measures.
•• Pellicano E, Dinsmore A, Charman T. What should autism research focus upon? Community views and priorities from the United Kingdom. Autism. 2014;18(7):756–70. https://doi.org/10.1177/1362361314529627An insightful breakdown of autism research funding and the views of the autistic community regarding priorities for research.
Patra S. Autism spectrum disorder in the elderly: a review of healthcare issues and challenges. J Geriatr Care Res. 2016;3:3–6.
Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217–50.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3 ed. Washington: 1980.
Hirvikoski T, Blomqvist M. High self-perceived stress and poor coping in intellectually able adults with autism spectrum disorder. Autism. 2015;19(6):752–7. https://doi.org/10.1177/1362361314543530.
Kenny L, Hattersley C, Molins B, Buckley C, Povey C, Pellicano E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism. 2016;20(4):442–62. https://doi.org/10.1177/1362361315588200.
Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. J Am Acad Child Adolesc Psychiatry. 2013;52(6):572–81 e1. https://doi.org/10.1016/j.jaac.2013.02.017.
Cage E, Di Monaco J, Newell V. Experiences of autism acceptance and mental health in autistic adults. J Autism Dev Disord. 2018;48(2):473–84. https://doi.org/10.1007/s10803-017-3342-7.
Dean M, Harwood R, Kasari C. The art of camouflage: gender differences in the social behaviors of girls and boys with autism spectrum disorder. Autism. 2017;21(6):678–89. https://doi.org/10.1177/1362361316671845.
Hull L, Petrides K, Allison C, Smith P, Baron-Cohen S, Lai M-C, et al. “Putting on my best normal”: Social camouflaging in adults with autism spectrum conditions. J Autism Dev Disord. 2017;47(8):2519–34. https://doi.org/10.1007/s10803-017-3166-5.
Jensen CMJ, Steinhausen H-C, Lauritsen MB. Time trends over 16 years in incidence-rates of autism spectrum disorders across the lifespan based on nationwide Danish register data. J Autism Dev Disord. 2014;44(8):1808–18. https://doi.org/10.1007/s10803-014-2053-6.
Whitehouse AJO, Cooper MN, Bebbington K, Alvares G, Lin A, Wray J, et al. Evidence of a reduction over time in the behavioral severity of autistic disorder diagnoses. Autism Res. 2017;10(1):179–87. https://doi.org/10.1002/aur.1740.
Lai M-C, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013–27.
Ashwood KL, Gillan N, Horder J, Hayward H, Woodhouse E, McEwen FS, et al. Predicting the diagnosis of autism in adults using the Autism-Spectrum Quotient (AQ) questionnaire. Psychol Med. 2016;46(12):2595–604. https://doi.org/10.1017/S0033291716001082.
Lewis LF. Realizing a diagnosis of autism spectrum disorder as an adult. Int J Ment Health Nurs. 2016;25(4):346–54. https://doi.org/10.1111/inm.12200.
Hickey A, Crabtree J, Stott J. ‘Suddenly the first fifty years of my life made sense’: Experiences of older people with autism. Autism. 2017;22(3):357–67. https://doi.org/10.1177/1362361316680914.
Jones L, Goddard L, Hill EL, Henry LA, Crane L. Experiences of receiving a diagnosis of autism spectrum disorder: a survey of adults in the United Kingdom. J Autism Dev Disord. 2014;44(12):3033–44. https://doi.org/10.1007/s10803-014-2161-3.
Powell T, Acker L. Adults’ experience of an Asperger syndrome diagnosis: analysis of its emotional meaning and effect on participants’ lives. Focus Autism Other Dev Disabl. 2015;31(1):72–80. https://doi.org/10.1177/1088357615588516.
Tan CD. “I’m a normal autistic person, not an abnormal neurotypical”: autism spectrum disorder diagnosis as biographical illumination. Soc Sci Med. 2018;197:161–7. https://doi.org/10.1016/j.socscimed.2017.12.008.
Cooper K, Smith LGE, Russell A. Social identity, self-esteem, and mental health in autism. Eur J Soc Psychol. 2017;47(7):844–54. https://doi.org/10.1002/ejsp.2297.
Bachmann CJ, Hofer J, Kamp-Becker I, Kupper C, Poustka L, Roepke S, et al. Internalised stigma in adults with autism: a German multi-center survey. Psychiatry Res. 2019;276:94–9. https://doi.org/10.1016/j.psychres.2019.04.023.
Kapp SK, Gillespie-Lynch K, Sherman LE, Hutman T. Deficit, difference, or both? Autism and neurodiversity. Dev Psychol. 2013;49(1):59–71. https://doi.org/10.1037/a0028353.
Rydzewska E, Hughes-McCormack LA, Gillberg C, Henderson A, MacIntyre C, Rintoul J, et al. General health of adults with autism spectrum disorders - a whole country population cross-sectional study. Res Autism Spectr Disord. 2019;60:59–66. https://doi.org/10.1016/j.rasd.2019.01.004.
Bishop-Fitzpatrick L, Rubenstein E. The physical and mental health of middle aged and older adults on the autism spectrum and the impact of intellectual disability. Res Autism Spectr Disord. 2019;63:34–41. https://doi.org/10.1016/j.rasd.2019.01.001.
Fortuna RJ, Robinson L, Smith TH, Meccarello J, Bullen B, Nobis K, et al. Health conditions and functional status in adults with autism: a cross-sectional evaluation. J Gen Intern Med. 2016;31(1):77–84. https://doi.org/10.1007/s11606-015-3509-x.
Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, et al. The health status of adults on the autism spectrum. Autism. 2015;19(7):814–23. https://doi.org/10.1177/1362361315577517.
Wise EA, Smith MD, Rabins PV. Aging and autism spectrum disorder: a naturalistic, longitudinal study of the comorbidities and behavioral and neuropsychiatric symptoms in adults with ASD. J Autism Dev Disord. 2017;47(6):1708–15. https://doi.org/10.1007/s10803-017-3095-3.
Starkstein S, Gellar S, Parlier M, Payne L, Piven J. High rates of parkinsonism in adults with autism. J Neurodev Disord. 2015;7(1):29.
Lever AG, Geurts HM. Age-related differences in cognition across the adult lifespan in autism spectrum disorder. Autism Res. 2016;9(6):666–76. https://doi.org/10.1002/aur.1545.
Braden BB, Smith CJ, Thompson A, Glaspy TK, Wood E, Vatsa D, et al. Executive function and functional and structural brain differences in middle-age adults with autism spectrum disorder. Autism Res. 2017;10(12):1945–59. https://doi.org/10.1002/aur.1842.
Powell PS, Klinger LG, Klinger MR. Patterns of age-related cognitive differences in adults with autism spectrum disorder. J Autism Dev Disord. 2017;47(10):3204–19. https://doi.org/10.1007/s10803-017-3238-6.
Buck TR, Viskochil J, Farley M, Coon H, McMahon WM, Morgan J, et al. Psychiatric comorbidity and medication use in adults with autism spectrum disorder. J Autism Dev Disord. 2014;44(12):3063–71. https://doi.org/10.1007/s10803-014-2170-2.
Joshi G, Wozniak J, Petty C, Martelon MK, Fried R, Bolfek A, et al. Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: a comparative study. J Autism Dev Disord. 2013;43(6):1314–25. https://doi.org/10.1007/s10803-012-1679-5.
Roy M, Prox-Vagedes V, Ohlmeier MD, Dillo W. Beyond childhood: psychiatric comorbidities and social background of adults with Asperger syndrome. Psychiatr. 2015;27(1):50–9.
Lever AG, Geurts HM. Psychiatric co-occurring symptoms and disorders in young, middle-aged, and older adults with autism spectrum disorder. J Autism Dev Disord. 2016;46(6):1916–30. https://doi.org/10.1007/s10803-016-2722-8.
Arnold SRC, Foley K, Hwang YI, Richdale A, Uljarevic M, Lawson L, et al. The Australian Longitudinal Study of Adults with Autism (ALSAA). BMJ Open. In press. https://doi.org/10.1136/bmjopen-2019-030798.
Cvejic RC, Arnold SRC, Foley KR, Trollor JN. Neuropsychiatric profile and psychotropic medication use in adults with autism spectrum disorder: results from the Australian Longitudinal Study of Adults with Autism. BJPsych Open. 2018;4(6):461–6. https://doi.org/10.1192/bjo.2018.64.
• Nylander L, Axmon A, Bjorne P, Ahlstrom G, Gillberg C. Older adults with autism spectrum disorders in Sweden: a register study of diagnoses, psychiatric care utilization and psychotropic medication of 601 individuals. J Autism Dev Disord. 2018;48(9):3076–85. https://doi.org/10.1007/s10803-018-3567-0A rare focus on the psychiatric circumstances of older adults on the spectrum.
Uljarevic M, Hedley D, Rose-Foley K, Magiati I, Cai RY, Dissanayake C, et al. Anxiety and depression from adolescence to old age in autism spectrum disorder. J Autism Dev Disord. 2019. https://doi.org/10.1007/s10803-019-04084-z.
Hollocks MJ, Lerh JW, Magiati I, Meiser-Stedman R, Brugha TS. Anxiety and depression in adults with autism spectrum disorder: a systematic review and meta-analysis. Psychol Med. 2019;49(4):559–72. https://doi.org/10.1017/S0033291718002283.
Cassidy S, Bradley P, Robinson J, Allison C, McHugh M, Baron-Cohen S. Suicidal ideation and suicide plans or attempts in adults with Asperger’s syndrome attending a specialist diagnostic clinic: a clinical cohort study. Lancet Psychiatry. 2014;1(2):142–7. https://doi.org/10.1016/s2215-0366(14)70248-2.
Hedley D, Uljarevic M, Wilmot M, Richdale A, Dissanayake C. Brief report: social support, depression and suicidal ideation in adults with autism spectrum disorder. J Autism Dev Disord. 2017;47(11):3669–77. https://doi.org/10.1007/s10803-017-3274-2.
Maddox BB, Trubanova A, White SW. Untended wounds: non-suicidal self-injury in adults with autism spectrum disorder. Autism. 2017;21(4):412–22. https://doi.org/10.1177/1362361316644731.
• Coleman DM, Adams JB. Survey of vocational experiences of adults with autism spectrum disorders, and recommendations on improving their employment. J Vocat Rehabil. 2018;49(1):67–78. https://doi.org/10.3233/JVR-180955This study outlines obstacles autistic individuals face in seeking and maintaining employment.
Frank F, Jablotschkin M, Arthen T, Riedel A, Fangmeier T, Holzel LP, et al. Education and employment status of adults with autism spectrum disorders in Germany-a cross-sectional-survey. BMC Psychiatry. 2018;18(1):75.
Ohl A, Sheff MG, Small S, Nguyen J, Paskor K, Zanjirian A. Predictors of employment status among adults with autism spectrum disorder. Work. 2017;56(2):345–55. https://doi.org/10.3233/WOR-172492.
Baldwin S, Costley D, Warren A. Employment activities and experiences of adults with high-functioning autism and Asperger’s disorder. J Autism Dev Disord. 2014;44(10):2440–9. https://doi.org/10.1007/s10803-014-2112-z.
Wise EA, Smith MD, Rabins PV. Correlates of daily functioning in older adults with autism spectrum disorder. Aging Ment Health. 2019;29:1–9. https://doi.org/10.1080/13607863.2019.1647138.
• Ee D, Hwang YIJ, Reppermund S, Srasuebkul P, Trollor JN, Foley K-R, et al. Loneliness in adults on the autism spectrum. Autism Adulthood. 2019;1(3):182–93. https://doi.org/10.1089/aut.2018.0038A unique study focusing on loneliness in autistic adults.
Alvarez-Fernandez S, Brown HR, Zhao Y, Raithel JA, Bishop SL, Kern SB, et al. Perceived social support in adults with autism spectrum disorder and attention-deficit/hyperactivity disorder. Autism Res. 2017;10(5):866–77. https://doi.org/10.1002/aur.1735.
Mazurek MO. Social media use among adults with autism spectrum disorders. Comput Hum Behav. 2013;29(4):1709–14. https://doi.org/10.1016/j.chb.2013.02.004.
Elmose M. Understanding loneliness and social relationships in autism: The reflections of autistic adults. Nord Psychol. 2019:No Pagination Specified. https://doi.org/10.1080/19012276.2019.1625068.
Milton D, Sims T. How is a sense of well-being and belonging constructed in the accounts of autistic adults? Disabil Soc. 2016;31(4):520–34. https://doi.org/10.1080/09687599.2016.1186529.
Weiss JA, Fardella MA. Victimization and perpetration experiences of adults with autism. Front Psychiatry. 2018;9:203. (MAY) (no pagination)(203). https://doi.org/10.3389/fpsyt.2018.00203.
Vogan V, Lake JK, Tint A, Weiss JA, Lunsky Y. Tracking health care service use and the experiences of adults with autism spectrum disorder without intellectual disability: a longitudinal study of service rates, barriers and satisfaction. Disabil Health J. 2017;10(2):264–70. https://doi.org/10.1016/j.dhjo.2016.11.002.
Vohra R, Madhavan S, Sambamoorthi U. Emergency department use among adults with autism spectrum disorders (ASD). J Autism Dev Disord. 2016;46(4):1441–54. https://doi.org/10.1007/s10803-015-2692-2.
• Nicolaidis C, Raymaker DM, Ashkenazy E, McDonald KE, Dern S, Baggs AE, et al. “Respect the way I need to communicate with you”: healthcare experiences of adults on the autism spectrum. Autism. 2015;19(7):824–31. https://doi.org/10.1177/1362361315576221A qualitative study that identifies the patient, provider, and system-level obstacles autistic adults face in seeking healthcare.
• Nicolaidis C, Raymaker D, McDonald K, Dern S, Boisclair W, Ashkenazy E, et al. Comparison of healthcare experiences in autistic and non-autistic adults: a cross-sectional online survey facilitated by an academic-community partnership. J Gen Intern Med. 2013;28(6):761–9. https://doi.org/10.1007/s11606-012-2262-7A helpful study that highlights the gaps in healthcare access and satisfaction between autistic and non-autistic adults.
Nicolaidis C, Raymaker D. Healthcare experiences of autistic adults. J Gen Intern Med. 2013;28(7):871. https://doi.org/10.1007/s11606-013-2427-z.
•• Sonido MT, Hwang YI, Trollor JN, Arnold SRC. The mental well-being of informal carers of adults on the autism spectrum: a systematic review. Rev J Autism Dev Disord. 2019. https://doi.org/10.1007/s40489-019-00177-8A comprehensive review of current research regarding experiences of carers of autistic adults.
Herrema R, Garland D, Osborne M, Freeston M, Honey E, Rodgers J. Mental wellbeing of family members of autistic adults. J Autism Dev Disord. 2017;47(11):3589–99. https://doi.org/10.1007/s10803-017-3269-z.
Herrema R, Garland D, Osborne M, Freeston M, Honey E, Rodgers J. Brief report: what happens when I can no longer support my autistic relative? Worries about the future for family members of autistic adults. J Autism Dev Disord. 2017;47(11):3659–68. https://doi.org/10.1007/s10803-017-3254-6.
Moss P, Eirinaki V, Savage S, Howlin P. Growing older with autism - the experiences of adult siblings of individuals with autism. Res Autism Spectr Disord. 2019;63:42–51. https://doi.org/10.1016/j.rasd.2018.10.005.
Tozer R, Atkin K. ‘Recognized, valued and supported’? The experiences of adult siblings of people with autism plus learning disability. J Appl Res Intellect Disabil. 2015;28(4):341–51. https://doi.org/10.1111/jar.12145.
Tozer R, Atkin K, Wenham A. Continuity, commitment and context: adult siblings of people with autism plus learning disability. Health Soc Care Community. 2013;21(5):480–8. https://doi.org/10.1111/hsc.12034.
Wright SD, Wright CA, D’Astous V, Wadsworth AM. Autism aging. Gerontol Geriatr Educ. 2019;40(3):322–38. https://doi.org/10.1080/02701960.2016.1247073.
Bennett M. “What is life like in the twilight years?” A letter about the scant amount of literature on the elderly with autism spectrum disorders. J Autism Dev Disord. 2016;46(5):1883–4. https://doi.org/10.1007/s10803-016-2710-z.
Perkins EA, Berkman KA. Into the unknown: aging with autism spectrum disorders. Am J Intellect Dev Disabil. 2012;117(6):478–96. https://doi.org/10.1352/1944-7558-117.6.478.
Piven J, Rabins P. Autism spectrum disorders in older adults: toward defining a research agenda. J Am Geriatr Soc. 2011;59(11):2151–5. https://doi.org/10.1111/j.1532-5415.2011.03632.x.
Nicolaidis C. Autism in adulthood: the new home for our emerging field. Autism Adulthood. 2018;1(1):1–3. https://doi.org/10.1089/aut.2018.28999.cjn.
Roestorf A, Bowler DM, Deserno MK, Howlin P, Klinger L, McConachie H, et al. “Older Adults with ASD: the consequences of aging.” Insights from a series of special interest group meetings held at the International Society for Autism Research 2016–2017. Res Autism Spectr Disord. 2019;63:3–12. https://doi.org/10.1016/j.rasd.2018.08.007.
Michael C. Why we need research about autism and ageing. Autism. 2016;20(5):515–6. https://doi.org/10.1177/1362361316647224.
• Nicolaidis C, Raymaker D, Kapp SK, Baggs A, Ashkenazy E, McDonald K, et al. The AASPIRE practice-based guidelines for the inclusion of autistic adults in research as co-researchers and study participants. Autism. 2019. https://doi.org/10.1177/1362361319830523An article outlining guidelines for the inclusion of autistic adults in research.
Funding
This work was supported by the Cooperative Research Centre for Living with Autism (Autism CRC), established and supported under the Australian Government’s Cooperative Research Centres Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Samuel Arnold reports grants from Autism CRC during the conduct of the study. Julianne Higgins reports grants from Autism CRC during the conduct of the study. Marisse Sonido and Ye In Hwang declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Autism Spectrum
Rights and permissions
About this article
Cite this article
Sonido, M., Arnold, S., Higgins, J. et al. Autism in Later Life: What Is Known and What Is Needed?. Curr Dev Disord Rep 7, 69–77 (2020). https://doi.org/10.1007/s40474-020-00192-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40474-020-00192-z