Abstract
Purpose of the Review
There is a heightened risk of suicide in Autism Spectrum Disorder (ASD). An up-to-date systematic review was conducted for studies examining suicide in ASD that were published in the past 5 years.
Recent Findings
Four previous systematic reviews were identified. The most recent review included studies published between 1995 and 2014. Combining data cross studies, prevalence of suicide attempts in ASD was estimated to be 7 to 47%, and suicidal ideation was 72%.
Summary
The current review included 13 studies. Compared to previous reviews, we identified a shift to the use of larger cohorts, including one population-based study. Prevalence rates for suicidal ideation were 11 to 66% and suicidal attempts were 1 to 35%. One study reported that 0.31% of premature deaths in ASD were due to suicide, significantly higher than general population controls. Further theoretical and empirical work is needed to identify causal mechanisms underlying suicidal risk in people with ASD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism Spectrum Disorder (ASD) is a lifelong condition with an estimated prevalence rate of 1 in 68 [1]. In addition to core difficulties in social communication and restricted and repetitive behaviors [2], people with ASD, across the lifespan, experience extremely high rates of comorbid psychopathology and other medical conditions, the most common being anxiety and depression [3,4,5,6,7,8] and sleep disorders [9, 10]. Given that in the general population history of depression is strongly associated with suicide [11, 12], the high rate of depression in ASD is particularly concerning as this factor alone is likely to place individuals with ASD at heightened risk [13]. Indeed, it has increasingly become apparent that suicidal ideation and behavior, including deaths, are overrepresented in people with ASD when compared to the general population [14, 15•]. Strikingly, a Swedish mortality study showed a sevenfold increased risk of premature death by suicide in people with ASD compared to the general population [16••].
Although reported prevalence of suicidal ideation and behavior varies widely across studies [15•], it is clear that the impact is alarming due to the increased risk in ASD compared to the general population. Given that (a) an understanding and appreciation of suicidal behavior in ASD and (b) the identification of underpinning mechanisms and risk factors are essential in identifying and providing appropriate supports to individuals at risk [14], we aim to summarize previous reviews on suicidal behavior in ASD and then report our own updated systematic review on the topic in order to provide a state of the art summary with regards to suicidal behavior in ASD. We also discuss a roadmap for future research.
Where the specific suicidal behaviors are not able to be ascertained from the original texts, the term “suicidal behavior” will be used forthwith as an overarching term that may describe suicidal ideation, suicidal attempts, and completed suicide, although where possible the specific term will be adopted [17].Footnote 1 In the general population, suicide accounts for 1.4% of deaths worldwide, is ranked as the 17th leading cause of death across all ages, and the second leading cause of death among 15–29-year-olds [18]. In a study involving 12,000 adults from the general community across eight sites and five European (EU) countries, Casey et al. [19] reported an overall rate for 2-week suicidal ideation of 7.6%. However, it is important to note that the rate varied across sites from 1.1 to 19.8% and was less for serious suicidal ideation (“I would like to kill myself”, “I would kill myself if I had the chance”; 0.4–1.8%). Factors which should be considered when assessing suicide risk in the general population include age and other demographic information, presence of psychiatric or other medical comorbidity, substance abuse and dependency, feelings of helplessness and hopelessness, poor sleep quality, family history of suicidal behavior, recent stressors and life events, and availability of social supports [17, 19].
It is currently not clear to what extent the risk factors derived from the general population are generalizable to people with ASD. Many of the factors affecting non-ASD populations (e.g., substance abuse, mental and physical health issues) are prevalent in ASD and seem to increase risk in this population [20, 21•]. However, other factors may function differently in ASD and non-ASD populations, possibly due to the influence of symptoms associated with the condition. For example, a recent study from our group [13] suggests that social support, in the form of appraisal and belonging, did not offer the same protection against risk for suicidal ideation and thoughts of self-harm in people with ASD as has been reported in studies with non-ASD populations. Core ASD symptoms may also increase risk. For example, reduced social capability may place the individual with ASD at risk of peer victimization, loneliness, and social isolation [13, 21•]. Other factors, such as a disproportionate number of males compared to females [21•], or indirect factors including, for example, high rates of under- and un-employment [22], may further increase risk [23]. Of concern, it has been suggested that individuals with ASD may be more likely to succeed in their first suicide attempt, may use more lethal means, and may be less connected to support services than other at risk groups [21•, 24].
Previous Systematic Reviews
We identified four systematic reviews concerning suicide in ASD published between 2013 and 2017 [15•, 21•, 23, 25]. Hannon and Taylor [23] reviewed studies examining suicidal behavior in adolescents and young adults with ASD with the aim of identifying prevalence and risk factors. Four studies published between 2005 and 2010 met their inclusion criteria. Key findings of the review were that rates of suicidal behavior were similar in young people with ASD and the typical population (7–8.5% based on one study), with overlapping risk factors between groups including comorbid mental health problems, abuse, and bullying. Hannon and Taylor further suggested that ASD symptoms may be risk factors, for example, more severe social and communication deficits may lead to interpersonal problems and social isolation. However, individuals with less severe symptom presentation may be at heightened risk due to better emotional insight and more contact with others. Indeed, Shtayermman [26] reported that individuals with less severe symptomology showed increased levels of suicidal ideation [23].
Segers and Rawana [21•] included 11 studies (published 1999–2013; three studies were also described in [23]) and three case reports in their review which targeted prevalence, clinical profiles, and risk and protective factors. Prevalence of suicidal behavior was reported to be 10.9–50% across studies. Four of the reviewed studies that examined the presence of ASD (which included retrospective diagnoses) in hospitalized cases suggested that individuals with ASD may comprise from 7.3 to 15% of suicidal inpatient populations. Suicidal risk factors in ASD identified across reviewed studies included peer victimization, behavioral problems, being Black or Hispanic, being male, and lower socioeconomic (SES) status and education level. Only one study [27] considered protective factors and, in addition to demographic variables (e.g., female, White, Asian, high SES), reported absence of impulsiveness, behavioral problems, or mood dysregulation to be associated with lower risk of suicidal behavior. However, absence of a certain factor or trait is not clearly a protective factor. Rather, a protective factor is better described as the presence of a particular trait or factor that reduces the risk of an unwanted or negative outcome occurring, despite negative circumstances.
Richa et al. [25] reviewed 11 studies published between 1999 and 2013 and identified a further 14 case studies and articles concerning suicide and ASD. The authors identified a need for large scale population studies to determine the extent of suicidal behavior in ASD and suggested research was needed to determine the extent to which suicidal behavior is associated with ASD symptoms and the extent to which it is associated with comorbid psychiatric disorders. They noted that suicidal ideation was one of the most common symptoms leading to a diagnosis of depression in people with ASD.
The most recent systematic review on suicide in ASD included 12 papers, published between 1995 and 2014 [15•]; four studies had not been included in previous reviews. Arguably the most significant of these is a study from the UK by Cassidy et al. [28••] wherein adults recently diagnosed with Asperger’s syndrome showed a significantly elevated risk of suicidal ideation or attempts compared to the general population and also several clinical groups (e.g., psychotic illness). This study also identified higher levels of both depression and ASD traits in individuals who reported planning or attempting suicide. Nonetheless, the study was reliant on only two self-report items (“have you ever felt suicidal”, “have you ever planned or attempted suicide”) to identify suicidal ideation and behavior, and the sample was non-representative of the broader ASD population given that all participants were diagnosed with Asperger’s syndrome in adulthood.
When combining samples across the reviewed studies (2651 cases), Zahid and Upthegrove [15•] reported the average prevalence for lifetime suicide attempts was 24.6% and the average rate of suicidal ideation was 32%––although rates varied considerably across studies most likely due to different samples and study methodologies. The most significant risk factors for suicidal behavior were a history of self-harm and depression. Being male was also identified as a factor increasing risk of suicidal behavior, although not all studies found significant effects for gender.
It is worth noting that conclusions that can be drawn from previous reviews are necessarily hampered by a number of methodological limitations of included studies, most notably small sample size, reliance on cross-sectional data, limited inclusion of comparison or control groups, lack of independent verification of ASD diagnosis or psychiatric comorbidities, limited use of gold standard diagnostic methods, poor sample characterization including limited information on level of adaptive or cognitive functioning (e.g., IQ), and often limited information on how suicidal behavior was operationalized. Overall, few of the reviewed studies administered standardized measures or assessments of suicidal behavior. Importantly, no measures of suicidal behavior have been validated for use in ASD populations.
Current Review
Given the most recent systematic review on suicidal behavior in ASD was completed in November 2014 [15•], we aimed to provide an updated systematic review by targeting studies published in the last 5 years. Selected studies were coded in terms of sample characteristics, diagnostic assessment, presence of comorbidities, how suicidal behavior was assessed, and prevalence rates for ideation and attempts. We paid particular attention to correlates of suicidal behavior, both in terms of risk and protective factors. Importantly, we aimed to identify gaps in current knowledge and highlight directions for future studies on suicidal behavior in ASD.
Method
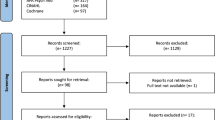
A systematic literature review following PRISMA guidelines [29] was conducted on August 11, 2017. PubMed, PsycINFO, and Web of Science databases were reviewed for studies examining suicidal behavior in people with ASD using the following search terms: (autis* [OR] asper* [OR] pervasive developmental disorder) [AND] suicid*. Search terms were derived from previous reviews. The initial search was limited to English language articles published from January 2012. No participant age restrictions were applied. Reference sections were reviewed to identify any missing studies. Exclusion criteria included qualitative or single case studies and non-empirical review (identified systematic reviews are summarized in the Introduction), correspondence, or commentary papers. Figure 1 provides the search results at each stage of the review process. Of 64 identified papers, 20 were excluded due to not meeting the inclusion criteria and 13 were included in the review. All included studies had been published between 2013 and 2017. These were analyzed for geographic location, participant characteristics (e.g., age, diagnostic information, use of control groups), ASD diagnostic method, comorbidity, method for assessing suicidal behavior and reporter (i.e., self, other), prevalence of suicidal ideation and attempts, and correlates or predictors of suicidal behavior.
Results
A summary of the included studies, including extracted data, is provided in Table 1. The present review identified six studies (superscript a) not included in previous systematic reviews [13, 16••, 30, 31, 32•, 36].
Sample Characteristics
A total of 30,663 (69.8% male) individuals with ASD were included in the reviewed studies. Five studies originated in the USA, three in Japan, and one each from Australia, Canada, Sweden, Turkey, and the UK. Four studies included sample sizes above 300 (range = 329–1507) [27, 28••, 30, 33] and one population study included mortality data for 27,122 individuals with ASD [16••]. Excluding the population-based mortality study, approximately 39% of participants were children or adolescents (1–18 years) and 61% were older adolescents or adults (17–65+ years). Six studies reported data regarding level of cognitive or intellectual functioning; however, they varied as to whether an IQ score of 80 or 70 was used as a cutoff to categorize individuals into lower or higher levels of intellectual functioning. Based on study criteria, approximately 86% of participants were reported to have higher IQ scores and 14% had lower IQ scores.
Control Groups
Eight studies (61%) included control groups or comparison data (refer to Table 1). Control groups were drawn from the general or other clinical populations. Two studies included gender and age matched control groups [16••, 30].
Quality of ASD Diagnostic Assessment
The quality of diagnostic assessments varied considerably between studies and included medical record review, clinical judgement, DSM-IV, DSM-5, ICD-9, or ICD-10 diagnostic criteria (n = 9 studies), self-report, and use of instruments including the full, translated, or abbreviated versions of the Autism Spectrum Quotient (AQ) [38,39,40], the Social Communication Questionnaire (SCQ) [41], and the Checklist for Autism Spectrum Disorder (CASD) [42]. Only two studies [32•, 35] reported using the “gold standard” Autism Diagnostic Observation Schedule (ADOS, ADOS-2) [43, 44] or Autism Diagnostic Interview-Revised (ADI-R) [45], to confirm diagnostic status. Three studies from Japan assessed participants for ASD retrospectively following admission to hospital for suicide attempts or who presented at an outpatient clinic for treatment [24, 36, 37].
Assessment of Suicidal Behavior
Suicide assessment included the use of self-report, including single item measures on existing scales, medical record review, including one study that examined cause of death in a national registry [16••], and clinical assessment. The only suicide-specific instrument that was used was Eskin’s Suicide Screening Questionnaire, which provides five yes/no questions about suicidal ideation and behavior [31].
Comorbidities
Across studies participants presented with multiple comorbidities, described in detail in Table 1. Depression or mood disorders and anxiety were common, with one study also reporting that 65% of participants had comorbid diagnoses of Attention Deficit Hyperactivity Disorder (ADHD) [31]. Studies varied in terms of how comorbidities were assessed and included self-report [13, 28••, 34, 36], medical record review based on diagnostic codes (e.g., ICD-9, ICD-10) [16••, 30], and clinical interview or assessment (may include clinical interview form, DSM-IV or DSM-5 criteria) [24, 31, 32•, 33, 35, 37].
Prevalence of Suicide Ideation and Attempts
Prevalence of suicide ideation ranged from 11 to 66% and suicidal attempts from 1 to 35%. Hirvikoski et al. [16••] reported a mortality rate for premature death by suicide in people with ASD of 0.31%, which compared to 0.04% in gender and age matched general population controls; odds ratio [OR] = 7.55 [6.04, 9.44], p = not reported. Compared to controls, risk of premature death by suicide was significantly increased for individuals with ASD who did not have a co-occurring intellectual disability (OR = 9.40 [7.43, 11.90], p < .001).
Correlates and Predictors
A range of correlates or predictors of suicidal thoughts or behavior were identified including bulimia, anxiety or mood disorders, female gender, presence of psychotic symptoms, family history of suicide, IQ (lower risk in those with intellectual disability), comorbid ADHD (negatively associated with parent report of suicidal ideation), behavior problems, Black or Hispanic, sleep disturbances, Post-Traumatic Stress Disorder (PTSD), and history of suicidal behavior. Only two studies identified a relationship between ASD traits assessed with the AQ and suicidal behavior (suicidal ideation and attempts) [28••, 34].
Discussion
The aim of this systematic review was to summarize recent studies (published in the last 5 years) concerning suicidal behavior in ASD and to provide directions for future research. This review identified six studies not included in previous reviews, one of which [16••] addressed an important gap in the literature concerning the need for large, population-derived studies to determine the true extent of suicide risk in the ASD population [23]. There is increasingly strong evidence that suicide is a critical issue facing people with ASD—recent studies report increased suicidal thoughts, behavior [28••], and premature death by suicide [16••] compared to both general and clinical populations.
Overall, prevalence rate for suicidal ideation was as high as 66%, and attempts were reported in up to 35% of study participants. The mortality rate reported by Hirvikoski et al. [16••] was 0.31% which indicated a higher risk of premature death by suicide compared to matched controls (0.04%). There is emerging evidence to suggest that suicide risk is increased in females and individuals without co-occurring intellectual disability [16••], although gender effects, if examined, were not always found to be significant [28••]. To date, studies have yet to unravel the underlying causal mechanisms leading to heightened risk of death by suicide in the ASD population.
Over half of reviewed studies included data from control groups, although only two studies matched controls on age and gender. Cassidy et al. [28••] provided data on the prevalence of suicidal ideation in adults from the general population, adults with medical or psychotic illnesses, and adults with ADHD and cocaine or opioid dependence, gleaned from a database search for studies using similar self-report questions on suicidal ideation. In this study, adults with Asperger’s syndrome reported a higher prevalence of lifetime suicidal ideation than all groups except those with ADHD and drug dependency. In terms of suicide prevalence, Hirvikoski et al. [16••] provide the most striking comparison data on premature mortality due to suicide in individuals diagnosed with ASD, each matched with up to 100 controls from the general population. Previous studies have been limited by small sample size or limited research involving young people with ASD [15•, 21•, 23, 25]. Therefore, increasing the use of larger samples and population-based studies covering a large age span and reasonable female representation (30% across studies) is an encouraging trend showing maturation of the field. Nonetheless, all studies used cross-sectional designs. As has been highlighted elsewhere [15•], large longitudinal studies are required to begin to unravel causal mechanisms regarding suicidal behavior in ASD.
Only two papers [32•, 35] used either the ADOS or ADI-R [43, 44] to confirm diagnosis and, although an improvement on previous reviews [15•], diagnostic methodology continues to present a significant limitation in terms of study quality. We found the AQ [38], which provides a standardized assessment of ASD traits and is available in different languages, continues to be used to assess ASD symptoms; however, as has been highlighted elsewhere [15•], the instrument is not a substitute for a diagnostic assessment. Diagnosis should be confirmed by an experienced examiner, include a review of developmental history, and incorporate the use of a standardized, valid, and reliable assessment instrument [46]. Similarly, the assessment of suicidal behavior varied in terms of quality. Not all studies assessed suicidal thoughts or behavior directly. Thus, in these studies, it was not possible to determine whether participants had explicit thoughts about suicide or a desire or plan of suicide. For example, Horowitz et al. [32•] used parent or caregiver report of their child talking about “death or suicide”; however, talk of death or suicide does not necessary imply that the child had a desire or thoughts of suiciding themselves. As the authors’ themselves acknowledge, talk of death may even represent a restricted interest in some individuals with ASD [32•]. Hedley et al. [13] used the Patient Health Questionnaire-9 (PHQ-9) [47] to assess suicidal ideation. Although the PHQ-9 includes a single item that assesses whether the respondent had “thoughts about being better off dead or of hurting yourself”, the question does not explicitly ask about suicidal ideation. It will be important for future studies to include standardized instruments that have been designed to assess suicidal ideation or behavior. Importantly, to the authors’ knowledge, there are no tools or instruments designed specifically to assess suicidal ideation or behavior in people with ASD. We therefore strongly recommend that future studies of suicide in ASD additionally incorporate a clinical interview by researchers or clinicians who have training and expertise in assessing suicidal behavior in this population.
It has been suggested that individuals with ASD and higher levels of cognitive functioning may be more affected by suicidal risk factors [23]. Indeed, Hirvikoski et al. [16••] found reduced risk of premature death by suicide in individuals who had been diagnosed with intellectual disability in addition to ASD. It has further been proposed that ASD symptom severity may be negatively associated with level of suicidal ideation [23]; however, support for this proposition initially came from a very small sample of adolescents and young adults (n = 5) who had been diagnosed with Asperger’s syndrome [26]. In contrast, Paquette-Smith et al. [34] found that individuals who attempted suicide returned higher AQ scores than those who did not have a history of suicide attempts, suggestive of a positive association between AQ symptom severity and suicide attempts. Cassidy et al. [28••] also found that individuals who reported suicide plans or attempts had higher AQ scores than those who did not; however, AQ scores did not differ significantly between those who did or did not report suicidal ideation. One other study also failed to find a significant relationship between AQ scores and either depression or suicidal ideation using the PHQ-9 [13]. Higher AQ scores may reflect greater cognitive insight into one’s condition [13]. It is therefore necessary when assessing symptom severity with the AQ to consider any potential interaction with IQ. Nonetheless, there seems to be some evidence of a positive association between ASD symptomatology, determined by self-report responses on the AQ, and history of suicide attempts but less support for an association between severity on the AQ and suicidal ideation. It will be important for future research to ascertain the contribution of ASD severity and level of cognitive functioning to risk for suicidal ideation and, importantly, attempts and completed suicide.
All of the reviewed studies provided information on comorbid conditions, with many using clinical assessments to determine presence of co-occurring psychopathology. However, methodology varied significantly between studies, with few reporting use of standardized assessment instruments to assess for comorbidities that may be associated with suicidal behavior such as depression, anxiety, and sleep disorders. Moreover, several studies relied on self-report to determine presence of comorbidities. One limitation of the reviewed studies, particularly those utilizing self-report or record review, was that it is not possible to determine temporal alignment as presence or absence of comorbid symptoms may not have been assessed at the same time as suicidal ideation or behavior. A second limitation, which applies to much of the research involving the assessment of psychopathology in ASD, is the lack of standardized assessment measures that have been validated in this population, particularly for anxiety and depression [7, 48•]. This is problematic as there can be significant overlap between ASD symptoms and other psychiatric conditions. For example, social avoidance and withdrawal may be a symptom of anxiety, or it could also be associated with social communication impairment that is central to ASD [7]. Similarly, symptoms of depression may manifest differently in people with ASD and may therefore be overlooked or dismissed or, on the other hand, symptoms of ASD may be misinterpreted as symptoms of depression [7]. Recent studies have failed to provide support for commonly used anxiety measures when applied to children and adolescents with ASD [49,50,51,52]. On a more promising note, one recent study provided initial support for the validity of the Hospital Anxiety and Depression Scale (HADS) [53] in older adolescents and young adults with ASD [7]. Nevertheless, we highly recommend both the inclusion of standardized assessment instruments for symptoms known to be associated with suicidal behavior (e.g., depression, anxiety, sleep disorders) and the use of clinical assessment, to determine the presence of comorbid psychopathology in future research concerning suicide in ASD.
Future Directions
One study from Japan found that people with ASD who had attempted suicide were less likely to be connected to services than those without ASD [24]. There has been little research with regards to what supports might effectively reduce suicide risk in the ASD population. A report of the US Surgeon General recommends that treatment and support for individuals at high risk of suicide should include identification and treatment of mental health and medical conditions, including treatments that specifically address suicide risk (i.e., that do not only treat underlying conditions), to work with high-risk patients to develop an action plan for crises, administration of evidence-based therapy (e.g., cognitive behavior therapy), improving patient-provider communication, providing multiple points of access to appropriate treatment, provision of integrated and continuous care across systems and settings, empowering families and significant others, peer support, and follow-up, and employment of recovery-oriented services supported by social relationships and networks and that involves the individual, family, and community [54]. We suggest that a similar strategic plan needs to be developed that specifically aims to reduce suicide risk and death in the ASD population. This should include the development of appropriate ASD support services and protocols. For example, health professionals can be trained to identify and manage suicidal ideation and behavior in individuals with ASD. Raised awareness in the ASD community and among families will also be important. This could include awareness around recognizing symptoms in oneself, family members, work colleagues, and peers. Clear pathways to service providers with necessary skills in working with clients with ASD will be integral to an integrated and appropriate support strategy.
Conclusions
Despite recent progress in describing the extent of suicidal risk in people with ASD, for example through inclusion of large samples and use of control groups and potential risk and protective factors, more theoretical work is needed to identify the causal mechanisms that increase suicidal risk in this population. In our own work, we have been examining the associations between loneliness, social support, ASD traits, and depression and suicidal ideation. One paper was included in the current review [13]; however, we did not include two additional studies as they were still under review when we conducted the initial search [55, 56]. Our intention is to begin to develop a theoretical framework for understanding increased suicidal risk in ASD that includes ASD specific risk factors, such as those associated with reduced social communication abilities. Furthermore, it will be important for future research to unravel the unique contributions of ASD symptom severity and co-occurring psychopathology and conditions (e.g., depression, anxiety, sleep disorders, intellectual disability).
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Christensen DL, Baio J, Braun KV, Bilder D, Charles J, Constantino JN, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. Centers Dis Control Prev MMWR Surveill Summ. 2016;65(SS-3):1–23.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
Bellini S. The development of social anxiety in adolescents with autism spectrum disorders. Focus Autism Other Dev Dis. 2006;21(3):138–45. https://doi.org/10.1177/10883576060210030201.
Evans DW, Canavera K, Kleinpeter FL, Maccubbin E, Taga K. The fears, phobias and anxieties of children with autism spectrum disorders and Down syndrome: comparisons with developmentally and chronologically age matched children. Child Psychiatry Hum Dev. 2005;36(1):3–26. https://doi.org/10.1007/s10578-004-3619-x.
Hofvander B, Delorme R, Chaste P, Nydén A, Wentz E, Ståhlberg O, et al. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry. 2009;9:1–9.
Lever AG, Geurts HM. Psychiatric co-occurring symptoms and disorders in young, middle-aged, and older adults with autism spectrum disorder. J Autism Dev Disord. 2016;46(6):1916–30. https://doi.org/10.1007/s10803-016-2722-8.
Uljarevic M, Richdale AL, McConachie H, Hedley D, Cai RY, Merrick H, et al. The Hospital Anxiety and Depression scale: factor structure and psychometric properties in older adolescents and young adults with autism spectrum disorder. Autism Res. 2017; https://doi.org/10.1002/aur.1872.
van Steensel FJ, Bogels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clin Child Fam Psychol Rev. 2011;14(3):302–17. https://doi.org/10.1007/s10567-011-0097-0.
Humphreys JS, Gringras P, Blair PS, Scott N, Henderson J, Fleming PJ, et al. Sleep patterns in children with autistic spectrum disorders: a prospective cohort study. Arch Dis Child. 2014;99(2):114–8. https://doi.org/10.1136/archdischild-2013-304083.
Richdale AL, Schreck KA. Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies. Sleep Med Rev. 2009;13(6):403–11. https://doi.org/10.1016/j.smrv.2009.02.003.
Barraclough B, Bunch J, Nelson B, Sainsbury P. A undred cases of suicide: clinical aspects. Br J Psychiatry. 1974;125(4):355–73. https://doi.org/10.1192/bjp.125.4.355.
Pagliaro LA. Adolescent depression and suicide: a review and analysis of the current literature. Can J Sch Psychol. 1996;11(2):191–201. https://doi.org/10.1177/082957359601100223.
Hedley D, Uljarević M, Wilmot M, Richdale A, Dissanayake C. Social support, depression and suicidal ideation in adults with autism spectrum disorder. J Autism Dev Disord. 2017;47(11):3669–77. https://doi.org/10.1007/s10803-017-3274-2.
Lai JKY, Rhee E, Nicholas D. Suicidality in autism spectrum disorder: a commentary. Adv Neurodev Disord. 2017;1(3):190–5. https://doi.org/10.1007/s41252-017-0018-4.
• Zahid S, Upthegrove R. Suicidality in autistic spectrum disorders: a systematic review. Crisis. 2017;38:237–46. Recent systematic review of suicide in ASD, includes prevalence of suicidal attempts and ideation and identifies significant risk factors.
•• Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, Bölte S. Premature mortality in autism spectrum disorder. Br J Psychiatry. 2016;208:232–8. Examined all-case and cause-specific mortality in ASD and matched controls from Swedish population-based register. Compared to controls, increased risk of premature death in ASD highest for diseases of the nervous system (OR = 7.49) and suicide (OR = 7.55).
Meyer RE, Salzman C, Youngstrom EA, Clayton PJ, Goodwin FK, Mann JJ, et al. Suicidality and risk of suicide—definition, drug safety concerns, and a necessary target for drug development: a consensus statement. J Clin Psychiatry. 2010;71(08):e1–e21. https://doi.org/10.4088/JCP.10cs06070blu.
World Health Organization. World Health Statistics 2017: monitoring health for the SDGs, sustainable developmental goals. Geneva: World Health Organization; 2017.
Casey P, Dunn G, Kelly BD, Lehtinen V, Dalgard OS, Dowrick C, et al. The prevalence of suicidal ideation in the general population: results from the Outcome of Depression International Network (ODIN) study. Soc Psychiatry Psychiatr Epidemiol. 2008;43(4):299–304. https://doi.org/10.1007/s00127-008-0313-5.
Raja M, Azzoni A, Frustaci A. Autism spectrum disorders and suicidality. Clin Pract Epidemiol Ment Health. 2011;7(1):97–105. https://doi.org/10.2174/1745017901107010097.
• Segers M, Rawana J. What do we know about suicidality in autism spectrum disorders? A systematic review. Autism Res. 2014;7:507–21. High quality systematic review of suicide in ASD.
Hedley D, Uljarević M, Cameron L, Halder S, Richdale A, Dissanayake C. Employment programmes and interventions targeting adults with autism spectrum disorder: a systematic review of the literature. Autism. 2017;21(8):929–41. https://doi.org/10.1177/1362361316661855.
Hannon G, Taylor EP. Suicidal behaviour in adolescents and young adults with ASD: findings from a systematic review. Clin Psychol Rev. 2013;33(8):1197–204. https://doi.org/10.1016/j.cpr.2013.10.003.
Kato K, Mikami K, Akama F, Yamada K, Maehara M, Kimoto K, et al. Clinical features of suicide attempts in adults with autism spectrum disorders. Gen Hosp Psychiatry. 2013;35(1):50–3. https://doi.org/10.1016/j.genhosppsych.2012.09.006.
Richa S, Fahed M, Khoury E, Mishara B. Suicide in autism spectrum disorders. Arch Suicide Res. 2014;18(4):327–39. https://doi.org/10.1080/13811118.2013.824834.
Shtayermman O. Peer victimization in adolescents and young adults diagnosed with Asperger's Syndrome: a link to depressive symptomatology, anxiety symptomatology and suicidal ideation. Issues Compr Pediatr Nurs. 2007;30(3):87–107. https://doi.org/10.1080/01460860701525089.
Mayes SD, Gorman AA, Hillwig-Garcia J, Syed E. Suicide ideation and attempts in children with autism. Res Autism Spectr Disord. 2013;7(1):109–19. https://doi.org/10.1016/j.rasd.2012.07.009.
•• Cassidy S, Bradley P, Robinson J, Allison C, McHugh M, Baron-Cohen S. Suicidal ideation and suicide plans or attempts in adults with Asperger's syndrome attending a specialist diagnostic clinic: a clinical cohort study. Lancet Psychiatry. 2014;1:142–7. Reported lifetime suicidal ideation (66%) and suicide plans or attempts (31%) in large sample of adults from the UK recently diagnosed with Asperger’s syndrome. Identified depression as important risk factor for suicidal behavior.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700. https://doi.org/10.1136/bmj.b2700.
Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, et al. The health status of adults on the autism spectrum. Autism. 2015;19(7):814–23. https://doi.org/10.1177/1362361315577517.
Demirkaya SK, Tutkunkardas MD, Mukaddes NM. Assessment of suicidality in children and adolescents with diagnosis of high functioning autism spectrum disorder in a Turkish clinical sample. Neuropsychiatr Dis Treat. 2016;12:2921–6. https://doi.org/10.2147/NDT.S118304.
• Horowitz LM, Thurm A, Farmer C, Mazefsky C, Lanzillo E, Bridge JA, et al. Talking about death or suicide: prevalence and clinical correlates in youth with autism spectrum disorder in the psychiatric inpatient setting. J Autism Dev Disord. 2017; https://doi.org/10.1007/s10803-017-3180-7. One of the few studies to report suicidal ideation (parent reported presence of talk about death or suicide) in youth with ASD with non-verbal IQ > 55. Identifed need for developmentally and ASD appropriate suicide risk screening instruments.
Mayes SD, Calhoun SL, Baweja R, Mahr F. Suicide ideation and attempts in children with psychiatric disorders and typical development. Crisis. 2015;36(1):55–60. https://doi.org/10.1027/0227-5910/a000284.
Paquette-Smith M, Weiss J, Lunsky Y. History of suicide attempts in adults with Asperger syndrome. Crisis. 2017;34:34–43.
Storch EA, Sulkowski ML, Nadeau J, Lewin AB, Arnold EB, Mutch P, et al. The phenomenology and clinical correlates of suicidal thoughts and behaviors in youth with autism spectrum disorders. J Autism Dev Disord. 2013;43(10):2450–9. https://doi.org/10.1007/s10803-013-1795-x.
Takara K, Kondo T. Autism spectrum disorder among first-visit depressed adult patients: diagnostic clues from backgrounds and past history. Gen Hosp Psychiatry. 2014;36(6):737–42. https://doi.org/10.1016/j.genhosppsych.2014.08.004.
Takara K, Kondo T. Comorbid atypical autistic traits as a potential risk factor for suicide attempts among adult depressed patients: a case-control study. Ann Gen Psychiatry. 2014;13(1):33. https://doi.org/10.1186/s12991-014-0033-z.
Baron-Cohen S, Wheelwright S, Skinner R, Martin J, Clubley E. The autism-spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. 2001;31(1):5–17. https://doi.org/10.1023/A:1005653411471.
Hoekstra RA, Vinkhuyzen AA, Wheelwright S, Bartels M, Boomsma DI, Baron-Cohen S, et al. The construction and validation of an abridged version of the autism-spectrum quotient (AQ-Short). J Autism Dev Disord. 2011;41(5):589–96. https://doi.org/10.1007/s10803-010-1073-0.
Kurita H, Koyama T, Osada H. Autism spectrum quotient Japanese version and its short forms for screening normally intelligent persons with pervasive developmental disorders. Psychiatry Clin Neurosci. 2005;59(4):490–6. https://doi.org/10.1111/j.1440-1819.2005.01403.x.
Rutter M, Bailey A, Lord C. The social communication questionnaire. Los Angeles: Western Psychol Serv; 2003.
Mayes SD. Checklist for autism spectrum disorder. Wood Dale: Stoelting; 2012.
Lord C, Rutter M, DiLavore PC, Risi S. Autism diagnostic observation schedule. Los Angeles: Western Psychological Services; 1999.
Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, Bishop SL. Autism diagnostic observation schedule, second edition (ADOS-2) manual (part I): modules. Torrance: Western Psychological Services; 2012. p. 1–4.
Rutter M, Le Couteur A, Lord C. Autism diagnostic interview-revised. Torrance: Western Psychological Services; 2003.
Langmann A, Becker J, Poustka L, Becker K, Kamp-Becker I. Diagnostic utility of the autism diagnostic observation schedule in a clinical sample of adolescents and adults. Res Autism Spectr Disord. 2013;7:109–19.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
• Wigham S, Barton S, Parr JR, Rodgers J. A systematic review of the rates of depression in children and adults with high-functioning Autism Spectrum Disorder. J Ment Health Res Intellect Disabil. 2017;10:1–21. Recent good quality systematic review of depression rates in ASD.
Glod M, Creswell C, Waite P, Jamieson R, McConachie H, South MD, et al. Comparisons of the factor structure and measurement invariance of the Spence Children's Anxiety Scale–Parent version in children with Autism Spectrum Disorder and typically developing anxious children. J Autism Dev Disord. 2017;47(12):3834–46. https://doi.org/10.1007/s10803-017-3118-0.
Jitlina K, Zumbo B, Mirenda P, Ford L, Bennett T, Georgiades S, et al. Psychometric properties of the Spence Children's Anxiety Scale: parent report in children with autism spectrum disorder. J Autism Dev Disord. 2017;47(12):3847–56. https://doi.org/10.1007/s10803-017-3110-8.
Magiati I, Lerh JW, Hollocks MJ, Uljarevic M, Rodgers J, McConachie H, et al. The measurement properties of the Spence Children's Anxiety Scale–Parent version in a large international pooled sample of young people with autism spectrum disorder. Autism Res. 2017;10(10):1629–52. https://doi.org/10.1002/aur.1809.
White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin Psychol Rev. 2009;29(3):216–29. https://doi.org/10.1016/j.cpr.2009.01.003.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Office of the Surgeon General and the National Action Alliance for Suicide Prevention. National strategy for suicide prevention: goals and objectives for action: a report of the U.S. Surgeon General and of the National Action Alliance for Suicide Prevention. Strategic Direction 3: Treatment and Support Services. Washington, DC: US Department of Health & Human Services; 2012.
Hedley D, Uljarević M, Wilmot M, Richdale A, Dissanayake C. Understanding depression and thoughts of self-harm in autism: a potential mechanism involving loneliness. Res Autism Spectr Disord. 2018;46:1-7. https://doi.org/10.1016/j.rasd.2017.11.003.
Hedley D, Uljarević M, Foley K-R, Richdale A, Trollor J. Risk and protective factors underlying suicidal ideation in Autism Spectrum Disorder. Manuscript submitted for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Darren Hedley reports grants from DXC Technology, Australian Government Department of Human Services, and Australian Government Department of Defense.
Mirko Uljarević reports a grant from Autism CRC.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Autism Spectrum
Rights and permissions
About this article
Cite this article
Hedley, D., Uljarević, M. Systematic Review of Suicide in Autism Spectrum Disorder: Current Trends and Implications. Curr Dev Disord Rep 5, 65–76 (2018). https://doi.org/10.1007/s40474-018-0133-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40474-018-0133-6