Abstract
Purpose of Review
This review aims to discuss historical aspects, mechanism of action, safety and efficacy, response predictors, and Magnetic Seizure Therapy (MST) protocol for treating depression. We also discuss the possibility of MST for personalized depression treatment and future directions.
Recent Findings
MST likely has a similar mechanism to the current gold standard neuromodulation treatment of Electroconvulsive Therapy (ECT) but differs in inducing seizures with a more controlled focus and pattern of cortical spread through the application of time-varying magnetic stimulation. The response and remission rates in depression with MST are comparable to ECT, but the cognitive adverse effects are likely to be more favorable with MST.
Summary
Depression is a common mental illness with significant burden globally, and about one-third of patients do not respond to treatment with multiple anti-depressant medications. Neuromodulation is one of the important treatment strategies for the management of depression, and among them MST is emerging as a promising treatment modality for depression. However, further evidence is needed to establish MST as a routine intervention in the clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression is a common mental disorder and has emerged as a major public health concern. The number of incident cases of depression worldwide have increased from 172 million in 1990 to 258 million in 2017 as per the Global Burden of Disease (GBD) study data suggesting an increase of about 50% [1]. It is seen that around 30% patients with depression do not respond to the conventional medical treatment options [2]. This group of patients need other modalities of treatment like Electroconvulsive Therapy (ECT) which is highly effective and is still widely considered as the gold-standard neuromodulation technique for depression treatment [3]. Neuromodulation is an evolving field of study with wide spectrum of implantable and noninvasive technology-based approaches for the treatment of neuropsychiatric disorders being developed and tested at different stages in pre-clinical and clinical trials with both animal and human participants respectively. Its central premise is to offer an interface with the nervous system (neurons and neurocircuits) through electrical, electromagnetic, chemical, or optogenetic methodologies with an aim of long-term activation, modification, inhibition, and/or regulation of neural activity [4].
Magnetic seizure therapy (MST) is a type of neuromodulation treatment which uses alternating magnetic fields across the scalp and the calvarium to induce an electric current in the cerebral cortex. The therapy works by inducing a seizure with relatively controlled focus and restricted pattern of spread through cerebral cortex as compared to the ECT-induced seizure [5]. In this review we aim to describe the historical aspects, possible mechanism of action, available evidence on its safety and efficacy from randomized controlled trials, and potential areas future research for establishing the role of MST in depression management.
Historical Aspects
ECT has undergone numerous revisions since its introduction, significantly improving its safety profile by the use of general anesthesia and muscle relaxant, introduction of right unilateral and bifrontal electrode placement, refinements in electrical stimulus parameters, enhanced control of electrical dosage for induction of seizure. Even with these improvements there are multiple problems like the limited control over distribution of electric current inside the cranial vault, shunting of current to other adjoining areas, cognitive adverse effects like amnesia, executive dysfunction, and disorientation, negative effect on neurocognitive functions of the patient [6].Considering this there is a need for exploring newer alternative techniques of neuromodulation for treatment of patients with depression. One such promising option that emerged in recent times is MST. The first MST-induced seizure reported in nonhuman primate was in the year 1998 [7]. The first human to receive MST was a 20-year-old inpatient with a medication-resistant major depression in 2000 in Bern, Switzerland [8]. There was a 50% drop in depression scores after four MST treatments. After this, the approval for conducting a feasibility trial of MST in the United State was obtained from the FDA and local institutional ethics review board [9]. It was seen that MST performed better as compared to ECT in terms of subjective side effects and recovery of orientation, measures of attention, retrograde amnesia, and category fluency [9].
Mechanisms of Action of MST in Depression
The exact mechanism(s) underlying the antidepressant effects of MST are still not fully understood and are likely to be similar to those proposed for the ECT. The induction of seizures is widely considered to play a vital role in producing treatment-related antidepressant effects in MST as well. However, there is a qualitative difference in the seizure produced by treatment with MST as compared to ECT. MST-induced seizure unlike ECT, mostly involves only the cerebral cortex and does not usually involve other deeper brain structures including the hippocampus [10, 11]. Similarly, MST-induced seizure results in a lesser degree of autonomic changes and is associated with a lower rise in serum prolactin levels as compared to that observed following an ECT-induced seizure [12, 13].
The emerging evidence from neuroimaging studies also suggests that the therapeutic effects of MST are possibly due to changes produced by MST in regional cerebral blood flow, neurotransmitter levels, and functional neural connectivity patterns [14,15,16]. Functional neuroimaging imaging-based studies have revealed changes in regional brain activity and connectivity patterns following MST, with alterations observed in areas implicated in emotion regulation, reward processing, and cognitive control. MST has been shown to enhance connectivity within the default mode network and favorably modulate activity in the anterior cingulate cortex and dorsolateral prefrontal cortex, and other regions thought to play a critical role in mood regulation and executive functioning. These neuroplastic changes may underlie the sustained antidepressant effects of MST and offer potential biomarkers for treatment response.
MST Protocol for Treatment of Depression
The MST protocol usually involves the application of a time-varying magnetic field from a magnetic stimulation coil placed over patients’ scalp which in turn produces an electrical current in the underlying brain or neurons. Magnetic stimulation in MST is applied at a higher frequency and intensity compared to the conventional transcranial magnetic stimulation treatment often called repetitive transcranial magnetic stimulation (rTMS). However, the strength of stimulation in MST is still lesser than in ECT. The most commonly used stimulation parameters for MST in the published RCTs (see Table 1) involved delivering magnetic stimulation at 100 Hz stimulation frequency at the maximum stimulation output of the machine as the strength of magnetic stimulation. However, there are variations in MST protocols across different RCTs in terms of the target site (vertex, bilaterally at F5-F6 as per the International 10–20 EEG system, etc.) and duration (2 weeks, 3 weeks, etc.) of MST treatment. Further, the ideal number of MST sessions or the gap between two consecutive MST sessions is also not yet established. Interestingly, one small open-label study tested the safety and efficacy of an accelerated MST protocol comprising one treatment session per day for six consecutive days in 15 patients with depression [17]. A rapid improvement in depressive symptoms with no significant cognitive side effects or other adverse events was reported by the authors. However, only a few human studies with relatively small sample sizes have been conducted to date for MST, with significant variations in the MST protocols even among them. Thus, there is a need to conduct adequately powered RCTs to determine the optimal stimulation parameters for the use of MST among patients with depression.
General anesthesia requirements for delivering MST are similar to that for ECT. There are no preferred pre-anesthetic medications, anesthetic agents, or muscle relaxants for MST compared to ECT. One notable exception would be the possible omission of the mandatory tongue bite block use [23]. This is because unlike ECT in which the masseter muscles get directly stimulated by the electric current applied through electrodes, the electric current gets directly produced inside brain tissue through electromagnetic induction by application of a time-varying magnetic field in MST. However, most human studies have still used a bite block as a precautionary measure. A repeated clicking noise is produced from the coil during the MST session which may potentially cause hearing loss, headache, or tinnitus in the patient and treating staff members. Thus, the use of ear plugs by both patient and health care staff delivering MST is recommended unlike that in ECT.
Safety and Efficacy of MST Use in Depression
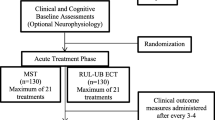
The enthusiasm surrounding the possibility of MST having a better safety profile as compared to the ECT stems from the initial studies conducted on non-human primates that indicated its favorable safety profile in terms neuropathological effects measured post MST induced seizure [24, 25]. A systematic review of published literature assessing the antidepressant effects of MST and its impact on cognitive functioning in patients with depression synthesized information from 10 different studies comprising a total of 285 patients [26]. It concluded that MST was comparable to ECT in terms of its antidepressant effects. Further, MST had a more favorable cognitive adverse effects profile than ECT. Subsequently, a recent systematic review and meta-analysis comprised exclusively of data obtained from randomized controlled trials (RCTs) comparing the safety and efficacy of MST and ECT for depression treatment also reported no significant difference in study-defined response or remission rates, as well as improvement in depression symptom severity scores between MST and ECT [27]. Three RCTs included in the above review evaluated the cognitive effects of MST compared with ECT using different assessment tools and yielded mixed findings. However, no study suggested a significantly greater degree of cognitive adverse effects with MST compared to ECT. After this meta-analysis was published, one more RCT comparing the effectiveness and safety of MST with ECT in depression was published in December 2023 [22]. This is the largest double-blind RCT to have been published to date. It compared MST (n = 35) with ultra-brief pulse right unilateral ECT (n = 38) for treatment of depression and reported no significant difference in either response or remission rates between the two treatment arms. In comparison to ECT, MST was associated with lesser frequency and intensity of subjectively reported adverse effects, especially in the physical and cognitive domains. Further, the improvement in depressive symptoms was maintained with both MST and ECT over a 6-month naturalistic follow-up period.
However, the response rates reported in the MST arm of the available RCTs ranged from 22 to 100%. This wide range is most likely because of small heterogenous sample sizes (inadequately powered to detect significant differences) and the application of different MST protocols (e.g. coil placement, stimulation parameters). At least three adequately powered non-inferiority RCTs comparing MST with ECT for the treatment of depression registered in the clinical trial registry (https://clinicaltrials.gov/) are currently ongoing in the USA (CTR id: NCT03191058), Canada (CTR id: NCT03641300), and Brazil (CTR id: NCT05054699). The findings from these trials shall help establish the safety and efficacy of MST for the treatment of depression, as well as help in identifying optimal MST stimulation parameters.
Predictors of Response to MST
A study among 38 patients with treatment resistant depression showed that the response rate with MST was 68.4%. The negative correlation with response was seen with number of previous episodes, and chronicity of the episode; whereas the positive correlation with response was seen with family history of depression, degree of depression severity and presence of fewer anxiety or somatic and melancholic symptoms [28]. When we look at the regional glucose metabolism, responders to MST exhibit an overall decrease in relative metabolism compared to the overall increase in non-responders. Response is related to a restoration of balance within limbic-cortical brain regions, rather than an overall increase in brain activity in these areas. However, these studies of predictors for response are also limited by small sample sizes [29].
The ictal EEG finding of low slow-wave amplitude and short polyspike duration been associated with good clinical outcome in MST [30]. Also positive clinical response could be indicated by reduction in EEG complexity in the occipital regions whereas greater impairment in neurocognitive function could be associated with increase in complexity in the parieto-central regions as concluded by a study done in 34 patients with treatment resistant depression [31].
MST as an Individualized Treatment Approach
MST is used to deliver time varying magnetic field, which electromagnetically induces electric current in the underlying cortex (neurons) and resultant seizure in targeted regions of the brain. With newer technology like structural and functional imaging it is possible to place a coil with precision making it a possibility to deliver current as per requirement of individual circuitry. Apart from this there is a possibility to identify biomarkers of response to MST as seen in ECT [32]. With further advancement, selecting circuits essential to produce antidepressant response and specifically targeting those based on the individual’s unique anatomy and pathophysiology could potentially enhance the safety and efficacy of MST. This personalized neuromodulation approach is a possibility which would not only provide individualized targeted effective treatment but also help us to test the causal mechanisms of antidepressant response to seizure therapy, which has not been answered till now.
Conclusions
MST in recent times has emerged as a promising non-invasive neuromodulation treatment that has good antidepressant properties and relatively benign neurocognitive adverse effects. As it is a relatively newer technique, a lot still remains to be established for MST such as the mechanism of action, optimal treatment paradigms and predictors of response. There is a need for conducting further research in order to find the mechanism of action, optimal parameters for best efficacy, use in other neuropsychiatric disorders, neurocognitive side-effects. Though there is lot of potential to develop this modality as a part of precision medicine for treatment of depression, more research is needed to optimize stimulation and safety parameters. Furthermore, comparative studies with other modalities of depression treatment such as ECT, refinement of treatment protocols, establishment of clear guidelines for patient selection, and long-term longitudinal follow-up studies for assessing the durability of effect are warranted.
Data Availability
No datasets were generated or analysed during the current study.
References
Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: Findings from the global burden of disease study. J Psychiatr Res. 2020;126:134–40. https://www.sciencedirect.com/science/article/pii/S0022395619307381. [cited 2024 Apr 21].
Voineskos D, Daskalakis ZJ, Blumberger DM. Management of treatment-resistant depression: challenges and strategies. Neuropsychiatr Dis Treat. 2020;16:221–34. https://www.tandfonline.com/doi/abs/10.2147/NDT.S198774. [cited 2024 Apr 21].
Diermen L van, Ameele S van den, Kamperman AM, Sabbe BCG, Vermeulen T, Schrijvers D, et al. Prediction of electroconvulsive therapy response and remission in major depression: meta-analysis. Br J Psychiatry. 2018;212:71–80. https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/prediction-of-electroconvulsive-therapy-response-and-remission-in-major-depression-metaanalysis/259FD7600E652E9D272481FC6D87F4F9. [cited 2024 Apr 21].
Johnson MD, Lim HH, Netoff TI, Connolly AT, Johnson N, Roy A, et al. Neuromodulation for Brain Disorders: Challenges and Opportunities. IEEE Trans Biomed Eng. 2013;60:610–24. https://ieeexplore.ieee.org/abstract/document/6428623. [cited 2024 Apr 7].
Lisanby SH. Update on magnetic seizure therapy: a novel form of convulsive therapy. J ECT. 2002;18:182–8.
Datto CJ. Side effects of electroconvulsive therapy. Depress Anxiety. 2000;12:130–4. https://onlinelibrary.wiley.com/doi/abs/10.1002/1520-6394%282000%2912%3A3%3C130%3A%3AAID-DA4%3E3.0.CO%3B2-C. [cited 2024 Apr 24].
Lisanby SH, Luber B, Finck AD, Schroeder C, Sackeim HA. Deliberate seizure induction with repetitive transcranial magnetic stimulation in nonhuman primates. Arch Gen Psychiatry. 2001;58:199–200.
Lisanby SH, Schlaepfer TE, Fisch H-U, Sackeim HA. Magnetic seizure therapy of major depression. Arch Gen Psychiatry. 2001;58:303–5. https://doi.org/10.1001/archpsyc.58.3.303. [cited 2024 Jul 1].
Lisanby SH, Luber B, Schlaepfer TE, Sackeim HA. Safety and feasibility of magnetic seizure therapy (MST) in major depression: randomized within-subject comparison with electroconvulsive therapy. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2003;28:1852–65.
Lisanby SH, Moscrip T, Morales O, Luber B, Schroeder C, Sackeim HA. Neurophysiological characterization of magnetic seizure therapy (MST) in non-human primates. Suppl Clin Neurophysiol. 2003;56:81–99.
Cycowicz YM, Rowny SB, Luber B, Lisanby SH. Differences in Seizure Expression Between Magnetic Seizure Therapy and Electroconvulsive Shock. J ECT. 2018;34:95–103.
White PF, Amos Q, Zhang Y, Stool L, Husain MM, Thornton L, et al. Anesthetic considerations for magnetic seizure therapy: a novel therapy for severe depression. Anesth Analg. 2006;103:76–80, table of contents.
Rowny SB, Cycowicz YM, McClintock SM, Truesdale MD, Luber B, Lisanby SH. Differential heart rate response to magnetic seizure therapy (MST) relative to electroconvulsive therapy: A nonhuman primate model. NeuroImage. 2009;47:1086–91. https://www.sciencedirect.com/science/article/pii/S1053811909005825. [cited 2024 Jul 1].
Smith SE, Kosik EL, van Engen Q, Kohn J, Hill AT, Zomorrodi R, et al. Magnetic seizure therapy and electroconvulsive therapy increase aperiodic activity. Transl Psychiatry. 2023;13:1–11. https://www.nature.com/articles/s41398-023-02631-y. [cited 2024 Apr 25].
Wang J, Jiang W, Yang C, Ma X. Magnetic seizure therapy modulates default mode network fluctuations of major depressive disorder. Chin J Behav Med Brain Sci. 2019;64–9. https://doi.org/10.3760/cma.j.issn.1674-6554.2019.01.012. [cited 2024 Apr 25].
Ge R, Gregory E, Wang J, Ainsworth N, Jian W, Yang C, et al. Magnetic seizure therapy is associated with functional and structural brain changes in MDD: Therapeutic versus side effect correlates. J Affect Disord. 2021;286:40–8. https://www.sciencedirect.com/science/article/pii/S0165032721001853. [cited 2024 Apr 25].
Wang J, Vila-Rodriguez F, Ge R, Gao S, Gregory E, Jiang W, et al. Accelerated magnetic seizure therapy (aMST) for treatment of major depressive disorder: A pilot study. J Affect Disord. 2020;264:215–20. https://www.sciencedirect.com/science/article/pii/S0165032719328861. [cited 2024 Apr 25].
Kayser S, Bewernick BH, Grubert C, Hadrysiewicz BL, Axmacher N, Schlaepfer TE. Antidepressant effects, of magnetic seizure therapy and electroconvulsive therapy, in treatment-resistant depression. J Psychiatr Res. 2011;45:569–76. Available from: https://www.sciencedirect.com/science/article/pii/S002239561000275X. [cited 2024 Apr 27].
Polster JD, Kayser S, Bewernick BH, Hurlemann R, Schlaepfer TE. Effects of electroconvulsive therapy and magnetic seizure therapy on acute memory retrieval. J ECT. 2015;31:13. https://journals.lww.com/ectjournal/abstract/2015/03000/effects_of_electroconvulsive_therapy_and_magnetic.5.aspx. [cited 2024 Apr 27].
Fitzgerald PB, Hoy KE, Elliot D, McQueen S, Wambeek LE, Chen L, et al. A pilot study of the comparative efficacy of 100 Hz magnetic seizure therapy and electroconvulsive therapy in persistent depression. Depress Anxiety. 2018;35:393–401.
Rowny SB, Kluisza L, Prudic J, Ly MT, Chen C-M, Casal-Roscum L. Smaller increase in delta post-ictal suppression in magnetic seizure therapy than electroconvulsive therapy in geriatric patients with severe depression: A multi-case study. Clin Neurophysiol Off J Int Fed Clin Neurophysiol. 2020;131:1219–20.
Deng Z-D, Luber B, McClintock SM, Weiner RD, Husain MM, Lisanby SH. Clinical outcomes of magnetic seizure therapy vs electroconvulsive therapy for major depressive episode: a randomized clinical trial. JAMA Psychiat. 2024;81:240–9.
Singh R, Sharma R, Prakash J, Chatterjee K. Magnetic seizure therapy. Ind Psychiatry J. 2021;30:S320–1.
Dwork AJ, Christensen JR, Larsen KB, Scalia J, Underwood MD, Arango V, et al. Unaltered neuronal and glial counts in animal models of magnetic seizure therapy and electroconvulsive therapy. Neuroscience. 2009;164:1557–64. https://www.sciencedirect.com/science/article/pii/S0306452209015553. [cited 2024 Jul 1].
Dwork AJ, Arango V, Underwood M, Ilievski B, Rosoklija G, Sackeim HA, et al. Absence of histological lesions in primate models of ECT and magnetic seizure therapy. Am J Psychiatry. 2004;161:576–8.
Chen M, Yang X, Liu C, Li J, Wang X, Yang C, et al. Comparative efficacy and cognitive function of magnetic seizure therapy vs. electroconvulsive therapy for major depressive disorder: a systematic review and meta-analysis. Transl Psychiatry. 2021;11:437.
Cai D-B, Yang X-H, Shi Z-M, Nie S, Xu R, Qin X-D, et al. Comparison of efficacy and safety of magnetic seizure therapy and electroconvulsive therapy for depression: a systematic review. J Pers Med. 2023;13:449. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10057006/. [cited 2024 Apr 25].
Kayser S, Bewernick BH, Wagner S, Schlaepfer TE. Clinical predictors of response to magnetic seizure therapy in depression: a preliminary report. J ECT. 2019;35:48. https://journals.lww.com/ectjournal/abstract/2019/03000/clinical_predictors_of_response_to_magnetic.11.aspx. [cited 2024 Apr 27].
Hoy KE, Thomson RH, Cherk M, Yap KSK, Daskalakis ZJ, Fitzgerald PB. Effect of magnetic seizure therapy on regional brain glucose metabolism in major depression. Psychiatry Res Neuroimaging. 2013;211:169–75. https://www.sciencedirect.com/science/article/pii/S0925492712001874. [cited 2024 Apr 27].
Backhouse FA, Noda Y, Knyahnytska Y, Farzan F, Downar J, Rajji TK, et al. Characteristics of ictal EEG in Magnetic Seizure Therapy at various stimulation frequencies. Clin Neurophysiol. 2018;129:1770–9. https://www.sciencedirect.com/science/article/pii/S1388245718302815. [cited 2024 Apr 27].
Farzan F, Atluri S, Mei Y, Moreno S, Levinson AJ, Blumberger DM, et al. Brain temporal complexity in explaining the therapeutic and cognitive effects of seizure therapy. Brain. 2017;140:1011–25. https://doi.org/10.1093/brain/awx030. [cited 2024 Apr 27].
Kallioniemi E, McClintock SM, Deng Z-D, Husain MM, Lisanby SH. Magnetic seizure therapy: Towards personalized seizure therapy for major depression. Pers Med Psychiatry. 2019;17–18:37–42. https://www.sciencedirect.com/science/article/pii/S2468171719300067. [cited 2024 Apr 27].
Author information
Authors and Affiliations
Contributions
Both the authors contributed equally for the final manuscript.
Corresponding author
Ethics declarations
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharma, P., Singh, S. Magnetic Seizure Therapy in Management of Depression: A Narrative Review. Curr Behav Neurosci Rep 11, 140–145 (2024). https://doi.org/10.1007/s40473-024-00283-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40473-024-00283-w