Abstract
Delayed graft function (DGF), or post-operative acute kidney injury leading to the need for dialysis within the first week after kidney transplantation, most commonly occurs in the setting of donor kidney recovery and the ischemia–reperfusion injury associated with the transplantation process. Despite advances in immunosuppressive regimens and medical management of kidney transplant recipients, the short- and long-term sequelae of DGF continue to be important determinants of kidney allograft prognosis. In this review, we will highlight the following areas as it relates to DGF: definition, pathophysiology, epidemiology, graft and patient outcomes, prediction, and some points on management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kidney transplantation has been well established as the ideal treatment modality for patients with end-stage renal disease [1]. The current era of transplantation has seen significant improvements in the perioperative care of donors, immunosuppressive regimens, and long-term medical management of recipients. These advances have been counterbalanced by the use of deceased donor kidneys at higher risk for long-term failure and the acceptance of increasingly medically complex recipients. These and other factors have likely contributed to the persistent burden of delayed graft function (DGF) (i.e., post-operative acute kidney allograft injury) in deceased donor kidney transplant recipients. Although DGF may also occur in living donor kidney transplant recipients, it is not nearly as common and the mechanism likely differs from their deceased donor counterparts.
In light of the various advancements in kidney transplant care, there is much interest in re-evaluating DGF’s impact on both short- and long-term outcomes. Prior to doing so, a review of the definitions, pathophysiology, and epidemiology of DGF would be important to put the results of outcome studies in context. Thereafter, the challenges of prediction and improving outcomes in patients with DGF will be discussed.
Definition
DGF most commonly refers to acute kidney injury with or without oliguria and has been defined by the need for dialysis within the first week after kidney transplantation [2]. As dialysis is routinely reported in large registries such as the Organ Procurement and Transplantation Network, this definition most conveniently captures DGF for the purposes of observational studies. Therefore, it is much more widely used than its 18 alternate definitions, based on creatinine level, dialysis requirement, or a combination thereof, which can also be found in the literature, as highlighted by Yarlagadda et al. in a systematic review [3]. This lack of homogeneity in identifying DGF complicates study interpretation and comparison. Previously, it had been argued that the current definition of DGF may be somewhat limited by centre-specific variations in thresholds for dialysis prescription [4]. However, its high sensitivity (89 % [95 % CI 84 %, 93 %]) and specificity (98 % [95 % CI 96 %, 99 %]) were validated in a recent prospective cohort study involving 557 deceased donor kidney transplant recipients from five centers [5]. Additionally, upon reclassifying 525 deceased donor transplant recipients according to ten different DGF definitions, Mallon et al. did not find any clinically significant differences in outcomes regardless of the dialysis and/or creatinine-based definitions used [6•]. Despite these findings, a definition based on pathophysiologic criteria would be ideal since it would reflect the underlying disease process as opposed to a physician’s response to a clinical phenotype (i.e., dialysis). However, such a definition has yet to be established.
Pathophysiology
During organ recovery, the kidney allograft is subjected to periods of warm and cold ischemia. Cellular hypoxia favors anaerobic metabolic pathways, with attendant lactic acidosis and ATP depletion (Fig. 1). This, in turn, interferes with Na/K ATPase functioning, eventually leading to cellular edema and cytoskeletal injury [7]. Following arterial anastomosis and graft reperfusion, oxidative metabolism is restored, with production of hydrogen peroxide and superoxide anions. In addition to being directly cytotoxic, these reactive oxygen species also trigger a cytokine release that directs neutrophils, macrophages, NK cells, and T cells to injure the graft tubular and endothelial cells. This potentiates the pro-inflammatory cascade and leads to local vasoconstriction, which, in turn, perpetuates cellular injury and further inflammation [8, 9].
Ischemia–reperfusion injury in delayed graft function. Cellular ischemia and hypoxia lead to anaerobic metabolism, depletion of ATP, impairment of the Na/K ATPase, and generation of reactive oxygen species, eventually culminating in tissue injury. Subsequent reperfusion enhances production of reactive oxygen species and triggers a cytokine release, recruiting inflammatory cells that damage tubular and endothelial structures. Reproduced with permission from Siedlecki et al. [9]
Moreover, it is hypothesized that the DGF-induced inflammatory cytokines heat shock protein (HSP) and high mobility group protein B-1 (HMG-1) activate Toll-like receptors and stimulate the expression of human leukocyte antigen (HLA) on the graft endothelium, thus fostering an immunogenic milieu [9–11]. With reperfusion injury, complement is activated. This recruits antigen-presenting cells and primes T cells, eventually leading to acute rejection [12, 13••].
Epidemiology and Risk Factors
DGF rates have been reported to be between 2 and 50 % [14] and are influenced by donor, transplant, and recipient-related characteristics. One of the main risk factors for DGF is donor subtype. As reported by the SRTR in 2012, living donor allograft recipients have a substantially lower risk of DGF as compared with deceased donor recipients (2.75 vs. 23.82 %, respectively) [8, 14, 15]. Additionally, subcategories of deceased donors bear different predilections for DGF. In particular, donation after circulatory death (DCD), with its obligate circulatory arrest and ensuing warm ischemia until the initiation of cold perfusion, entails a 37 % incidence of DGF [14, 16, 17]. Comparatively, neurologically declared donors (NDD) have an intermediate rate of injury: 20 % in standard criteria donors (SCD) and 31 % in expanded criteria donors (ECD) [14]. Though there is no exposure to warm ischemia in these cases, brain death itself initiates a catecholamine surge, facilitating unregulated vasoconstrictive ischemia and fostering an inflammatory milieu, which ultimately may lead to tubular necrosis [18–20].
The lowest rate of DGF is seen in living donors (3.4 %), ten times less commonly than in DCD donors [14]. This highlights the impact of cold ischemia time (CIT) or the time during which the graft is preserved in a cooled preservative solution, on or off a pump, on DGF. The cooler temperatures limit ischemic injury by slowing the graft’s cellular metabolism, and the composition of the preservation solution slows the inevitable metabolic imbalance that ensues from hypoperfusion [21, 22]. As demonstrated by Ojo et al. in a large retrospective cohort study, CIT has an adjusted odds ratio for DGF of 1.38 to 3.48. This risk increases by 23 % with every additional 6 h of CIT and seems to be more detrimental to DCD organs [23–25]. Other risk factors for DGF that have been highlighted over various studies include donor age, specifically if over 50 years old, which doubles the odds of DGF [24, 25], and the degree of HLA mismatch between donor and recipient [24, 26••, 27].
The impact of recipient factors was made evident in a retrospective cohort study looking at 5832 pairs of recipients who received kidneys from the same donor, but in whom only one of the pair developed DGF. Male sex, African American race, diabetes mellitus, prior history of sensitization, prolonged wait-listing time, and obesity (body mass index >30 kg/m2) were identified as independent recipient risk factors for DGF [28]. Though the study did not report on the impact of surgical technique or related operative issues and residual confounding may have been present, its results are supported by similar findings in a more recent study involving recipients in the Eurotransplant Senior Program [29]. Most notably, obesity has been repeatedly associated with DGF [26••, 29–32]. It is proposed to promote an inflammatory environment, thus enhancing ischemia–reperfusion injury, and also to influence the pharmacokinetics of immunosuppressive medications, thus facilitating acute rejection [33]. A 2015 systematic review and meta-analysis pooling 138,081 patients from 17 studies showed an odds ratio of 1.76 (95 % CI 1.52, 2.04) for DGF in obese patients [26••].
The influence of dialysis modality seems to be less relevant than that of the recipient’s peritransplant intravascular volume status, with avoidance of aggressive ultrafiltration preoperatively and maintenance of euvolemia post-operatively associated with more favorable outcomes [34, 35]. The care administered during cold perfusion may also be pertinent, since Excelsior preservation solutions have been associated with worse outcomes [22] and pulsatile machine perfusion with better outcomes [21, 36–39]. The role of induction agents on DGF risk remains unclear, as evidenced by contradicting results in recent randomized controlled studies comparing IL2 receptor antagonists and rATG [40, 41].
Short-Term Outcomes
By engendering a highly inflammatory milieu, DGF has been associated with an increased risk of acute rejection [42]. In a recent single-centre cohort study of 645 patients, a multivariable Cox proportional hazard model showed a relative hazard for biopsy-proven acute rejection (BPAR) of 1.55 (95 % CI 1.03, 2.32) for patients experiencing DGF (vs. no DGF). This increased risk was maintained across different definitions of DGF, as well as the type of acute rejection (T cell-mediated vs. antibody-mediated) [43]. These findings confirm a persistent immunologic impact of DGF on graft longevity, despite the recent development of more effective immunosuppressive regimens [44].
A systematic review and meta-analysis of 33 studies showed that DGF decreased graft survival at 3 years by a relative risk of 1.41 (95 % CI 1.27, 1.56; P = 0.002). This risk remained despite adjustment for episodes of acute rejection, year of publication, duration of follow-up, and donor subtype. There was a similar negative correlation with renal function, as demonstrated by a higher serum creatinine at 3.5 years post-transplant in patients with DGF. Reassuringly, this did not seem to impact patient survival, although follow-up was brief and limited to 5 years [45].
In a single-centre study of 462 kidney transplant recipients, DGF accounted for 20.9 % of rehospitalizations to acute care centers within 30 days of discharge [46]. An SRTR- and Medicare-based study of 32,961 patients transplanted between 2001 and 2005 showed a strong association between early hospital readmissions and future hospitalizations within 1 year after the initial visit, in living donor allograft recipients who had developed DGF (hazard ratio 4.56 [95 % CI 2.87, 7.25; P < 0.001]) [44]. Early readmission was also shown to be a significant independent risk factor for death-censored allograft loss, predominantly associated with chronic allograft nephropathy [47, 48] and mortality [47].
Long-Term Outcomes
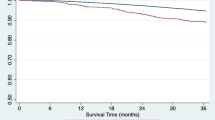
The long-term impact of DGF continues to be disputed. One of the original studies that highlighted the prognostic importance of DGF in kidney transplant recipients was the analysis of the US Renal Data System by Ojo et al. [24]. The authors showed that DGF was independently associated with a 53 % increase in the 5-year risk of allograft loss. Moreover, the subsequent occurrence of acute rejection further accentuated the adverse effect of DGF on long-term outcomes. A recent instrumental variable analysis of 80,690 deceased donor kidney transplant recipients corroborated these early findings and showed an increased risk of death-censored graft loss and mortality up to 5 years post-transplant [49•]. DGF has been reported to lead to a 40 % decrease in long-term graft survival in some reports [11, 50]. In contrast, a single-centre study of 633 deceased donor kidney transplant recipients followed for up to 13 years failed to show any significant reduction in patient or graft survival among patients with DGF vs. no DGF (P = 0.56 and P = 0.51, respectively) [51]. In general, registry-based analyses have consistently shown a detrimental impact of DGF on long-term graft survival, whereas single-center reports have been more variable. Moreover, the definitions used, the covariables included in statistical models, the populations studied, the way that intermediate events such as acute rejection are handled, and differences in post-transplant management may all play a role in the variability seen across studies.
Death with graft function (DWGF) occurs in up to 38 % of transplant recipients [52–54], but its association with DGF has not been previously well studied. In a large cohort of 86,502 patients transplanted from 1988 and 1997, DWGF represented 42.5 % of graft losses at 10 years following transplantation and was independently influenced by DGF [53]. More recently, Tapiawala studied 50,246 deceased donor kidney transplant recipients between 1998 and 2004 and demonstrated an adjusted hazard ratio of 1.53 (95 % CI 1.45, 1.63) for DWGF in patients with vs. without DGF (Table 1). This increased risk persisted in patients who showed recovery of renal function at 6 and 12 months post-transplant [55]. A retrospective cohort study of 44,630 adult living donor kidney recipients showed similar results, with an adjusted hazard ratio for DWGF in patients with DGF (vs. without DGF) of 1.48 (95 % CI 1.26, 1.73) over follow-up. In both cohorts, the causes of death were mainly sepsis, cardiovascular disease, and stroke, posited to occur due to a non-favorable recipient milieu generated by DGF, facilitating extra-renal organ dysfunction in a fashion similar to AKI-associated end-organ damage [44, 55, 56]. These findings supported the strong association between DGF and DWGF, both in the short and long terms.
A survey of 1694 kidney transplant recipients showed that the odds of patients experiencing decreased health-related quality of life was 1.67 times greater following DGF (95 % CI 1.08, 2.57; P = 0.02) than if the patients did not experience DGF. As a consequence, DGF lengthens hospitalization, engenders patient morbidity, and increases health care-associated costs [57, 58].
Prediction
In 2010, Irish et al. devised a prediction model for DGF using registry data and confirmed the most impactful risk factors to be CIT, recipient BMI, donor creatinine, DCD donors, and donor age [59]. In addition to DGF, the algorithm predicted graft survival. A patient with a greater than 50 % risk of DGF had twice the chance of developing graft failure as compared to a patient with a DGF risk <25 % [59]. Since this publication, additional prognostic clinical parameters have been identified. A retrospective cohort study of 83 patients studied time on dialysis in the post-transplant period as a surrogate for severity of renal injury and highlighted its inverse relationship with renal function at 1 year [60]. The routine use of preimplantation biopsies has been suggested, following the observation that glomerulosclerosis and vascular narrowing may portend DGF in recipients of deceased donor kidney allografts [61]. However, proposed histological scoring systems have not been externally validated [62].
When measured within 6 h post-operatively, urinary biomarkers interleukin-18 (IL-18) and neutrophil gelatinase-associated lipocalin (NGAL) discriminate the development of DGF more accurately than creatinine trends (C statistic 0.76–0.9) [63–65] and are associated with poor recovery of renal function up to 1 year post-transplant [64, 66]. On one hand, urine proteomics may be confounded by urinary volumes, while on the other, they may not add much prognostic value in an oliguric context (C statistic 0.83 for a urine output below 1 L over the first post-operative day) [63]. In this context, viability testing of the kidney allograft while on-pump has been studied. A model combining effluent biomarkers and graft perfusion pressures, as surrogates of intrarenal pressures, was shown to predict DGF but with suboptimal discrimination (C statistic 0.58, 0.67) [67]. Newer biomarkers clusterin and TNF-α-induced protein 3 (A20) show promise [68, 69] but require further validation with special attention to kinetics in relation to renal clearance and clarification of the ideal timing of their measurement.
Management
As the growing demand for organs pushes the use of kidneys from ECD and donors after circulatory death, putting more recipients at risk for DGF and its consequences, the need to convert our evolving knowledge of the mechanism of DGF into effective targeted therapies grows ever more urgent. Arguably, the prevention of DGF, if possible, would be preferable to the attenuation of established DGF.
Preventive interventions may start as early as the preoperative optimization of donors. In a multicentre randomized controlled trial of 394 NDD, inducing mild hypothermia between 34 and 35 °C significantly reduced the risk of DGF (odds ratio, 0.62; 95 % CI 0.43 to 0.92; P = 0.02) [70••]. Although remote ischemic preconditioning has shown promise in DCD [71], results have been rather disappointing in living donor kidney allografts [72], and neither study reported on long-term outcomes. Potential therapies targeting cold storage- or organ-recovery-induced tubular injury include controlled rewarming [73] and pulsatile perfusion of the graft [21]. With regard to recipient-targeted treatments, a clinical trial assessing the efficacy of eculizumab, a monoclonal antibody against complement C5, in the prevention of DGF is currently in the recruitment phase (NCT01919346). Additionally, an array of anti-oxidant and anti-inflammatory molecules is being explored as potential therapies [74–76]. They offer the potential advantage of a maintained effect on established DGF should preventive measures fail, although it is yet unclear if the long-term effects of DGF can be averted at all. As such, studies focusing on follow-up measures such as anti-HLA antibody monitoring and protocol biopsies for the early detection of the long-term sequelae of DGF are as important as trials examining candidate treatments to prevent DGF.
Calcineurin inhibitor (CNI)-associated nephrotoxicity has been purported to prolong kidney recovery after DGF. However, current guidelines suggest that CNI should be introduced without delay [77]. CNI-sparing regimens in the early post-transplant period have been explored, with sirolimus showing the most potential [78, 79]. The SMART and CONCEPT trials show that conversion to sirolimus in the months following kidney transplantation portends similar patient and graft survival with better renal function among patients who can tolerate it [80, 81]. However, in the acute post-operative period, sirolimus accelerates apoptosis of injured renal tubular epithelia [78] and podocytes [82], doubling the likelihood of prolonged DGF [83–86], when compared to a CNI-based maintenance regimen (hazard ratio 0.48, p = 0.0007) [86]. Although graft function was comparable at 1 year, sirolimus’ high rate of discontinuation, extensive side effect profile, and associated risk of acute rejection cannot be dismissed when considering its use, especially at early post-transplant [87].
ATG modulates the expression of adhesion molecules involved in the inflammatory cascades of ischemia–reperfusion injury [88]. Goggins et al. showed that the intraoperative infusion of ATG prior to reperfusion of the kidney allograft reduced the risk of DGF by more than half (14.8 vs. 35.5 %, p < 0.05) vs. post-operative ATG and led to significantly better kidney function at 14-day (but not 30) post-transplant [89]. Although the randomized trial design increases confidence in the results, the small sample size and short follow-up make it difficult to apply the findings directly to the care of kidney transplant recipients.
Conclusion
DGF is a prevalent post-transplant phenomenon, which continues to have a significant impact on allograft prognosis in the modern era of kidney transplantation. As it is mainly driven by ischemia–reperfusion injury, prevention of DGF remains a challenge. Antioxidant and anti-inflammatory agents present potential therapeutic agents that could prove effective, if coupled with effective means of predicting the occurrence of DGF. Although discovering and implementing effective preventive strategies for DGF should remain the primary goal, novel treatments or monitoring strategies that can alter the prognosis of patients with established DGF may significantly contribute to improving the outcomes for all kidney transplant recipients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wolfe RAAV, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. New England Journal of Medicine. 1999;341(23):1725–30.
Perico N et al. Delayed graft function in kidney transplantation. Lancet. 2004;364(9447):1814–27.
Yarlagadda SG et al. Marked variation in the definition and diagnosis of delayed graft function: a systematic review. Nephrol Dial Transplant. 2008;23(9):2995–3003.
Akkina SKCJ, Israni AK, et al. Similar outcomes with different rates of delayed graft function may reflect center practice, not center performance. Am J Transplant. 2009;9(6):1460–6.
Potluri VS et al. Validating early post–transplant outcomes reported for recipients of deceased donor kidney transplants. Clinical Journal of the American Society of Nephrology. 2016;11(2):324–31.
Mallon DH et al. Defining delayed graft function after renal transplantation: simplest is best. Transplantation. 2013;96(10):885–9. This study validates and describes the clinical relevance of the current definition of DGF.
Kosieradzki MRW. Ischemia/reperfusion injury in kidney transplantation: mechanisms and prevention. Transplant Proceedings. 2008;2008(40):10.
DA Shoskes HP. Delayed graft function in renal transplantation: etiology, management and long-term significance. J Urol. 1996;155(6):1831–40.
Siedlecki AIW, Brennan DC. Delayed graft function in the kidney transplant. Am J Transplant. 2011;11(11):2279–96.
Lu CYPJ, Kielar ML, et al. Hypothesis: is renal allograft rejection initiated by the response to injury sustained during the transplant process? Kidney International. 1999;55(6):2157–68.
DA Shoskes CJ. Deleterious effects of delayed graft function in cadaveric renal transplant recipients independent of acute rejection. Transplantation. 1998;66(12):1697–701.
Brennan TVFC, Fuller TF, Bostrom A, Tomlanovich SJ, Feng S. Early graft function after living donor kidney transplantation predicts rejection but not outcomes. Am J Transplant. 2004;4(6):971–9.
Decuypere J-P et al. Autophagy and the kidney: implications for ischemia-reperfusion injury and therapy. American Journal of Kidney Diseases. 2015;66(4):699–709. This review provides a thorough description of the pathophysiology of ischemia-reperfusion injury.
Kwon OJ et al. The impact of delayed graft function on graft survival in living donor kidney transplantation. Transplant Proceedings. 2003;35(1):92–3.
Matas AJ et al. OPTN/SRTR 2012 annual data report: kidney. American Journal of Transplantation. 2014;14(S1):11–44.
Rojas-Pena A et al. Extracorporeal support: improves donor renal graft function after cardiac death. Am J Transplant. 2010;10(6):1365–74.
Snoeijs MGJ et al. Kidney transplantation from donors after cardiac death: a 25-year experience. Transplantation. 2010;90(10):1106–12.
Nijboer WN et al. Effect of brain death on gene expression and tissue activation in human donor kidneys. Transplantation. 2004;78(7):978–86.
Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Critical Care Medicine. 2009;37(7):S186–202.
Pratschke JTS, Neuhaus P. Brain death associated ischemia/reperfusion injury. Annals of Transplant. 2004;2004(9):1.
Gill J et al. Pulsatile perfusion reduces the risk of delayed graft function in deceased donor kidney transplants, irrespective of donor type and cold ischemic time. Transplantation. 2014;97(6):668–74.
O’Callaghan JMKS, Morgan RD, Morris PJ. Preservation solutions for static cold storage of kidney allografts: a systematic review and meta-analysis. Am J Transplant. 2012;12(4):896–906.
Kayler LKMJ, Zendejas I, et al. Impact of cold ischemia time on graft survival among ECD transplant recipients: a paired kidney analysis. Am J Transplant. 2011;11(12):2647–56.
Ojo AO et al. Delayed graft function: risk factors and implications for renal allograft survival. Transplantation. 1997;63(7):968–74.
Summers DM et al. Effect of donor age and cold storage time on outcome in recipients of kidneys donated after circulatory death in the UK: a cohort study. Lancet. 2013;381(9868):727–34.
Hill CJ et al. Recipient obesity and outcomes after kidney transplantation: a systematic review and meta-analysis. Nephrology Dialysis Transplantation. 2015;30(8):1403–11. This study provides an in-depth review of the obesity as a risk factor for DGF.
Shoskes DA et al. HLA matching determines susceptibility to harmful effects of delayed graft function in renal transplant recipients. Transplant Proceedings. 1995;27(1):1068–9.
Doshi MD et al. Recipient risk factors associated with delayed graft function: a paired kidney analysis. Transplantation. 2011;91(6):666–71.
Bahde R et al. Prognostic factors for kidney allograft survival in the Eurotransplant Senior Program. Medical Science Monitor Basic Research. 2014;19:201–9.
Chang SHCP, McDonald SP. Effects of body mass index at transplant on outcomes of kidney transplantation. Transplantation. 2007;84(8):981–7.
Gore JL et al. Obesity and outcome following renal transplantation. Am J Transplant. 2006;6(2):357–63.
Weissenbacher A et al. Recipient and donor body mass index as important risk factors for delayed kidney graft function. Transplantation. 2012;93(5):524–9.
Khwaja AE-NM. Transplantation in the obese: separating myth from reality. Nephrol Dial Transplant. 2012;27(10):3732–5.
Molnar MZ et al. Dialysis modality and outcomes in kidney transplant recipients. Clinical Journal of the American Society of Nephrology. 2012;7(2):332–41.
Van Loo AA et al. Pretransplantation hemodialysis strategy influences early renal graft function. Journal of the American Society of Nephrology. 1998;9(3):473–81.
Buchanan PM et al. Association of lower costs of pulsatile machine perfusion in renal transplantation from expanded criteria donors. Am J Transplant. 2008;8(11):2391–401.
Jochmans I et al. Machine perfusion versus cold storage for the preservation of kidneys donated after cardiac death: a multicenter, randomized, controlled trial. Annals of Surgery. 2010;252(5):756–64.
Moers C et al. Machine perfusion or cold storage in deceased donor kidney transplantation. New England Journal of Medicine. 2009;360(1):7–19.
Treckmann J et al. Machine perfusion versus cold storage for preservation of kidneys from expanded criteria donors after brain death. Transplant International. 2011;24(6):548–54.
Liu Y et al. Basiliximab or antithymocyte globulin for induction therapy in kidney transplantation: a meta-analysis. Transplant Proceedings. 2010;42(5):1667–70.
Noel C et al. Daclizumab versus antithymocyte globulin in high-immunological-risk renal transplant recipients. Journal of the American Society of Nephrology. 2009;20(6):1385–92.
Watson CJE et al. Cold machine perfusion versus static cold storage of kidneys donated after cardiac death: a UK multicenter randomized controlled trial. Am J Transplant. 2010;10(9):1991–9.
Wu WK et al. Delayed graft function and the risk of acute rejection in the modern era of kidney transplantation. Kidney International. 2015;88(4):851–8.
Nagaraja PRG, Stephens M, et al. Influence of delayed graft function and acute rejection on outcomes after kidney transplantation from donors after cardiac death. Transplantation. 2012;94(12):1218–23.
Yarlagadda SG et al. Association between delayed graft function and allograft and patient survival: a systematic review and meta-analysis. Nephrol Dial Transplant. 2009;24(3):1039–47.
Lubetzky M et al. Early readmission after kidney transplantation: examination of discharge-level factors. Transplantation. 2016.
McAdams-DeMarco MA, Grams ME, King E, Desai NM, Segev DL. Sequelae of early hospital readmission after kidney transplantation. Am J Transplant. 2014;14(2):397–403.
Yokoyama I et al. Effect of prolonged delayed graft function on long-term graft outcome in cadaveric kidney transplantation. Clinical Transplantation. 1994;8(2):101–6.
Butala NM et al. Is delayed graft function causally associated with long-term outcomes after kidney transplantation? Instrumental variable analysis. Transplantation. 2013;95(8):1008. This study provides a thorough analysis of the association between DGF and long term outcomes to both graft and patient.
Hariharan S et al. Post-transplant renal function in the first year predicts long-term kidney transplant survival. Kidney International. 2002;62(1):311–8.
Woo YM et al. Early graft function and patient survival following cadaveric renal transplantation. Kidney International. 1999;55(2):692–9.
Hirata MCY, Cecka JM, Terasaki PI. Patient death after renal transplantation: an analysis of its role in graft outcome. Transplantation. 1996;61(10):1479–83.
Ojo AO et al. Long-term survival in renal transplant recipients with graft function. Kidney International. 2000;57(1):307–13.
West MSD, Matas AJ. Kidney transplant recipients who die with functioning grafts: serum creatinine level and cause of death. Transplantation. 1996;62(7):1029–30.
Tapiawala SN et al. Delayed graft function and the risk for death with a functioning graft. Journal of the American Society of Nephrology. 2010;21(1):153–61.
Grams MERH. The distant organ effects of acute kidney injury. Kidney International. 2012;81(10):942–8.
Almond PS et al. Economic impact of delayed graft function. Transplant Proceedings. 1991;23(1 part 2):1304.
Rosenthal JT et al. The high cost of delayed graft function in cadaveric renal transplantation. Transplantation. 1991;51(5):1115–8.
Irish WD et al. A risk prediction model for delayed graft function in the current era of deceased donor renal transplantation. Am J Transplant. 2010;10(10):2279–86.
Marek C et al. The prognostic value of time needed on dialysis in patients with delayed graft function. Nephrol Dial Transplant. 2014;29(1):203–8.
Lopes JAMF, Rierra L, et al. Evaluation of preimplantation kidney biopsies: comparison of Banff criteria to a morphometric approach. Kidney International. 2005;67(4):1595–600.
Snoeijs MGJ et al. Histological assessment of preimplantation biopsies may improve selection of kidneys from old donors after cardiac death. Am J Transplant. 2008;8(9):1844–51.
Hall IEYS, Coca SG, et al. IL-18 and urinary NGAL predict dialysis and graft recovery after kidney transplantation. Journal of the American Society of Nephrology. 2010;21(1):189–97.
Hollmen ME et al. Urine neutrophil gelatinase-associated lipocalin is a marker of graft recovery after kidney transplantation. Kidney International. 2011;79(1):89–98.
Parikh CRJA, Mishra J, et al. Urine NGAL and IL-18 are predictive biomarkers for delayed graft function following kidney transplantation. Am J Transplant. 2006;6(7):1639–45.
Hall IE et al. Association between peritransplant kidney injury biomarkers and 1-year allograft outcomes. Clinical Journal of the American Society of Nephrology. 2012;7(8):1224.
Moers C et al. The value of machine perfusion perfusate biomarkers for predicting kidney transplant outcome. Transplantation. 2010;90(9):966–73.
Avihingsanon Y et al. On the intraoperative molecular status of renal allografts after vascular reperfusion and clinical outcomes. Journal of the American Society of Nephrology. 2005;16(6):1542–8.
Pianta TJ et al. Clusterin in kidney transplantation: novel biomarkers versus serum creatinine for early prediction of delayed graft function. Transplantation. 2015;99(1):171–9.
Niemann CU et al. Therapeutic hypothermia in deceased organ donors and kidney-graft function. New England Journal of Medicine. 2015;373(5):405–14. This study tested donor cooling as a novel mechanism for the prevention of DGF in a randomized controlled trial.
Wu J et al. Remote ischemic conditioning enhanced the early recovery of renal function in recipients after kidney transplantation: a randomized controlled trial. Journal of Surgical Research. 2014;1888(1):303–8.
MacAllister R et al. REmote preconditioning for Protection Against Ischaemia–Reperfusion in renal transplantation (REPAIR): a multicentre, multinational, double-blind, factorial designed randomised controlled trial. Efficacy and Mechanism Evaluation. 2015.
Mahboub P et al. Gradual rewarming with gradual increase in pressure during machine perfusion after cold static preservation reduces kidney ischemia reperfusion injury. PloS one. 2015;10(12):e0143859.
Fuller TF et al. Protein kinase C inhibition ameliorates posttransplantation preservation injury in rat renal transplants. Transplantation. 2012;94(7):679–86.
Gueler F et al. A novel therapy to attenuate acute kidney injury and ischemic allograft damage after allogenic kidney transplantation in mice. PloS one. 2015;10(1):e0115709.
Parajuli N, et al. MitoQ blunts mitochondrial and renal damage during cold preservation of porcine kidneys. 2012. 2012;7(11):e48590
Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group. KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant. 2009;9 Suppl 3:S1–155.
Lieberthal W et al. Rapamycin impairs recovery from acute renal failure: role of cell-cycle arrest and apoptosis of tubular cells. American Journal of Physiology-Renal Physiology. 2001;281(4):F693–706.
Loverre A et al. Ischemia-reperfusion induces glomerular and tubular activation of proinflammatory and antiapoptotic pathways: differential modulation by rapamycin. Journal of the American Society of Nephrology. 2004;15(10):2675–86.
Guba M et al. Early conversion to a sirolimus‐based, calcineurin‐inhibitor‐free immunosuppression in the SMART trial: observational results at 24 and 36 months after transplantation. Transplant International. 2012;25(4):416–23.
Lebranchu Y et al. Efficacy on renal function of early conversion from cyclosporine to sirolimus 3 months after renal transplantation: concept study. American Journal of Transplantation. 2009;9(5):1115–23.
Munivenkatappa R et al. Tubular epithelial cell and podocyte apoptosis with de novo sirolimus based immunosuppression in renal allograft recipients with DGF. Histology and Histopathology. 2010;25:189–96.
Stallone G et al. Addition of sirolimus to cyclosporine delays the recovery from delayed graft function but does not affect 1-year graft function. Journal of the American Society of Nephrology. 2004;15(1):228–33.
Tahir W et al. Early sirolimus conversion as rescue therapy in kidneys with prolonged delayed graft function in deceased donor renal transplant, Transplantation proceedings, vol. 47. 2015. No. 6. Elsevier.
Simon JF et al. Induction sirolimus and delayed graft function after deceased donor kidney transplantation in the United States. American journal of nephrology. 2004;24(4):393–401.
McTaggart RA et al. Sirolimus prolongs recovery from delayed graft function after cadaveric renal transplantation. American Journal of Transplantation. 2003;3(4):416–23.
McTaggart RA et al. Comparison of outcomes after delayed graft function: sirolimus-based versus other calcineurin-inhibitor sparing induction immunosuppression regimens. Transplantation. 2004;78(3):475–80.
Beiras-Fernandez A et al. Impact of polyclonal anti-thymocyte globulins on the expression of adhesion and inflammation molecules after ischemia–reperfusion injury. Transplant immunology. 2009;20(4):224–8.
Goggins WC et al. A prospective, randomized, clinical trial of intraoperative versus postoperative thymoglobulin in adult cadaveric renal transplant recipients. Transplantation. 2003;76(5):798–802.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Emilie Chan and Joseph Kim declare that they have no conflict of interest as related to this report.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
This article is part of the Topical Collection on Kidney Transplantation
Rights and permissions
About this article
Cite this article
Chan, E., Kim, S.J. Does Delayed Graft Function Still Herald a Poorer Outcome in Kidney Transplantation?. Curr Transpl Rep 3, 236–243 (2016). https://doi.org/10.1007/s40472-016-0110-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-016-0110-0