Abstract
Purpose
In recent years, minimal intervention procedures (MIPs) for treating dental caries in children have stood out as an innovative method. Nevertheless, the treatment decision should be based on scientific evidence, professional expertise, and parents’ preference/acceptance. Evaluating the acceptance of MIPs by parents is an essential factor, but little information is available on what guides this preference.
Methods
This scoping review aims to synthesize the evidence on parents’/caregivers’ acceptance of MIP for managing cavitated caries lesions in children. A search was performed in the PubMed, Cochrane Library, Lilacs and Google Scholar databases with no restriction on date or language.
Results
A total of 19 articles were selected (6 clinical trials, 1 longitudinal and 12 cross-sectional studies). The application of silver diamino fluoride (SDF) was the most commonly evaluated procedure (n = 17), followed by the atraumatic restorative technique (ART) and the Hall Technique (HT). The acceptance of MIPs ranged from 1.4% to 100%, and the application of SDF was better accepted in posterior teeth and in uncooperative children. ART had better aesthetic acceptance than HT.
Conclusion
Application of SDF, Hall Technique and ART was well accepted by parents/caregivers. However, a gap remains in the literature regarding the acceptance of other procedures. Therefore, further studies in this area will contribute toward a better understanding of the opinion of parents/caregivers, and thus improve caries lesion management in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dental caries management has changed over time and is now founded on a better understanding of the mechanism of disease development. Since the publication of the first policy statement on minimal intervention dentistry (MID), the approach to caries lesions has developed to include noninvasive, micro invasive, and minimally invasive strategies that aim to preserve tooth structure that can be remineralized (WHO 2016). The minimally invasive procedures (also known as minimal intervention procedures) (MIPs) recommended in the guidelines and policies for caries lesions management include the application of silver diamine fluoride (SDF) in cavitated lesions, fissure and pit sealants, non-restorative approaches, and restorations using different techniques and materials, such as atraumatic restorative treatment (ART) with glass ionomer cement, and the Hall Technique (HT) (Corrêa-Faria et al. 2020).
The efficacy of MID-based procedures has been investigated in an increasing number of clinical studies and reviews (BaniHani et al. 2022). An umbrella review evaluated 18 systematic reviews on the management of caries lesions in primary teeth using these procedures and confirmed the efficacy of SDF application, selective removal of carious tissue, and HT and ART techniques in halting the progression of lesions (BaniHani et al. 2022). Results on the effectiveness of MID-based procedures are important for making decisions regarding treatment options and should be considered together with the professional’s experience (Rønneberg et al. 2017), and the preference, values and needs of the patient and his family (Jayaraman and Mallineni 2022). However, the number of studies on parents’/caregivers’ perception toward MIPs for caries lesion management in children is still limited.
The evaluation of caries lesion treatment options by patients/caregivers, and their involvement in the decision-making process is an emerging need in pediatric dentistry (Ladewig et al. 2018). Patient-reported outcome measures (PROMS), or outcomes reported by the children’s caregivers, are increasingly sought in clinical trials because they allow related therapies to be evaluated by the people with the greatest interest in the treatment (Mendes et al. 2020). Outcomes, such as parent/caregiver acceptance and preference for a certain MIP, have recently been investigated in clinical trials and observational studies, and the results have been summarized in both scoping (Magno et al. 2019) and systematic reviews (Sabbagh et al. 2020; Hu et al. 2022). These reviews have evaluated what guides the acceptance of SDF in primary teeth (Magno et al. 2019; Sabbagh et al. 2020), as well as HT (Hu et al. 2022). The literature has a gap regarding parent/caregiver acceptance of other MIPs and offers a synthesis allowing a comparative evaluation of the acceptance of these procedures, indicated for managing caries lesions in children.
To map and synthesize the scientific evidence on the acceptance of the different MPIs it is desirable to conduct a scoping review. This type of review differs from the systematic one in that it allows the elaboration of a broader question related to heterogeneous topics (Tricco et al. 2018; Munn et al. 2018). From this design, it will be possible to verify and synthesize the literature on the different MIPs.
The aim of this study was to use a scoping review to map and synthesize the evidence on parents’ and caregivers’ acceptability of MIPs for managing cavitated caries lesions in children and to identify the variables that may affect acceptability.
Material and methods
The scoping review was reported following PRISMA guidelines (Tricco et al. 2018). The study involved the following steps: (1) formulation of the research question; (2) identification of relevant studies; (3) selection of studies; (4) data mapping; (5) grouping, synthesis and reporting of results (Levac et al. 2010). The protocol was registered at the Open Science Framework in December 2022 (https://osf.io/ujdk3https://doi.org/10.17605/OSF.IO/4XNCQ).
The CoCoPop (condition, context and population) acronym was used to formulate the research question: “To what extent do parents/caregivers accept MIPs for managing cavitated caries lesions in children?” The condition investigated was the use of MIPs to manage cavitated caries lesions in deciduous teeth. The context was the acceptance of MIPs by parents/caregivers, who constituted the population in reference.
Relevant studies on the subject were searched in PubMed, Lilacs, Cochrane Library, OpenGrey through the Dans Easy Archive and Google Scholar electronic databases. The search strategy was developed using terms indexed in the Medical Subject Heading (MeSH) and synonyms and was adapted to each electronic database (Table 1). The search made no restriction to date or language of publication of the studies. The reference lists of the included articles were consulted to identify relevant studies.
The references were managed using Rayyan software (Rayyan—Intelligent Systematic Review) (Ouzzani et al. 2016). Duplicate articles were removed, and the others were evaluated by three researchers, independently and in two stages. In the first stage, the title and abstract of each article were read, and the eligibility criteria, applied. Next, the full text of the articles included in the previous stage was read and evaluated on the inclusion and exclusion criteria. Disagreements among the evaluators were resolved by consensus. The inclusion criteria of the articles were: observational studies (cross-sectional, case–control and cohort) and intervention studies (clinical trials) that investigated the acceptance of parents/caregivers toward the MIPs indicated for managing cavitated carious lesions in deciduous teeth. Guidelines, editorials, case reports, qualitative studies, reviews, animal studies, and in vitro studies were excluded.
Information was extracted from the included articles and then synthesized in a table and text. Details about the study (authors, year, and country of publication), method (study design), participants (number of participants, relationship with the child, age of the children), the MIPs investigated, method of evaluation of acceptance, results on acceptance, associated factors, and conclusion were extracted. When relevant information was not available in the articles, it was requested from the authors by email.
Results
Study selection
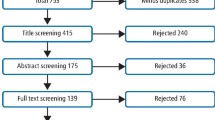
The search in the electronic databases resulted in 952 articles and was conducted in January 2023. After the removal of the duplicates, 920 were submitted to the title and abstract evaluation stage. A total of 869 documents were excluded because they did not evaluate the caregivers’ acceptance of MIPs for caries lesion management in primary teeth, and 51 were read in full. Of these, 16 were included in the scoping review. A consultation of the reference list of the articles identified 9 documents, 3 of which were included. In the end, 19 articles were included (Fig. 1).
Study characteristics
The studies were conducted in the United Arab Emirates (1), Pakistan (1), Syria (1), Saudi Arabia (4), India (4), Singapore (1), the United States (4), Egypt (2) and Brazil (1). The cross-sectional design was the most frequent (n = 12), followed by clinical trials (n = 6) and longitudinal studies (n = 1). The number of participants ranged from 26 in a longitudinal study (Chaurasiya and Gojanur 2021) to 546 in a cross-sectional study (Kumar et al. 2019). In the clinical trials, the number of participants ranged from 30 (Clemens et al. 2018) to 100 (El-Ghandour et al. 2021). The interventions compared in these trials were ART versus application of SDF (El-Ghandour et al. 2021; Ali et al. 2021), ART versus HT (Araújo et al. 2020), HT versus restoration with resin-modified glass ionomer cement (Thakkar and Jawdekar 2022), and SDF versus conventional restoration (Cleary et al. 2022).
Parent/caregiver acceptance of MIPs was assessed mainly by using a 4- to 5-point Likert scale (Ali et al. 2021; Alshammari et al. 2019; Asif and Guranathan 2020; Bagher et al. 2019; Bassam et al. 2022; Clemens et al. 2018; El-Ghandour et al. 2021; Hu et al. 2020; Thakkar and Jawdekar 2022; Walia et al. 2022). In most studies on the acceptance of SDF application, parents/caregivers were questioned after observing photographs of treated teeth that evidenced the blackening of the tooth structure (Akshita et al. 2022; Alshammari et al. 2019; Asif and Gurunathan 2020; Bagher et al. 2019; Crystal et al. 2017; Salim et al. 2021), and a video (Hu et al. 2020). In 3 cross-sectional studies, parents/caregivers were presented with different scenarios related to the management of the child’s behavior toward dental care (Crystal et al. 2017; Akshitha et al. 2022; Walia et al. 2022).
In 7 clinical trials (Clemens et al. 2018; El-Ghandour et al. 2021; Araujo et al. 2020; Ali et al. 2021; Chaurasiya and Gojanur 2021; Bassam et al. 2022; Cleary et al. 2022), acceptance was assessed immediately after treatment (Araujo et al. 2020; Bassam et al. 2022) or in follow-up sessions at 2-week (Clemens et al. 2018; El-Ghandour et al. 2021; Ali et al. 2021) to 12-month intervals (Cleary et al. 2022). The acceptance of parents/caregivers was based on criteria related to the child, such as comfort (Ali et al. 2021), discomfort caused by the procedure (Araújo et al. 2021), pain caused by the procedure (Clemens et al. 2018; Asif and Gurunathan 2020), duration of the session (Ali et al. 2021), aesthetic aspect (Alshammari et al. 2019; Ali et al. 2021; Cleary et al. 2022; El-Ghandour et al. 2021; Almarwan et al. 2021; Akshitha et al. 2022; Asif and Gurunathan 2020; Bassam et al. 2022), ease in performing the procedure (Clemens et al. 2018; Asif and Gurunathan 2020), taste of the product (Clemens et al. 2018; El-Ghandour et al. 2021), how well the restoration could protect the tooth (Araújo et al. 2020), and understanding why treatment is needed (Araújo et al. 2020).
The percentage of acceptance of MIPs ranged from 1.4% (Walia et al. 2022) to 100% (Chaurasiya and Gojanur 2021). In the studies that evaluated SDF application, the acceptance of parents was investigated according to the location of the teeth (Almarwan et al. 2021; Bagher et al. 2019; Bassam et al. 2022; Crystal et al. 2017; Salim et al. 2021; Wajahat et al. 2022; Walia et al. 2022), and to the behavior of the children (Akshitha et al. 2022; Ali et al. 2021; Bagher et al. 2019; Walia et al. 2022). The acceptance of SDF application to anterior teeth ranged from 28.7% (Akshitha et al. 2022) to 57.5% (Ali et al. 2021), versus 55.2% (Almarwan et al. 2021) to 97.5% (Ali et al. 2021) for posterior teeth. In one study, more than 90% of the participants considered SDF application unacceptable for either anterior or posterior teeth (Alshammari et al. 2019).
Acceptance of SDF application was associated with behavioral management problems (Bagher et al. 2019; Hu et al. 2020; Ali et al. 2021; Akshitha et al. 2022), pharmacological techniques indicated for behavior management (Chaurasiya and Gojanur 2021; Akshitha et al. 2022), and location of the teeth to be treated (Akshitha et al. 2022). Socioeconomic factors such as educational level (Crystal et al. 2017; Asif and Gurunathan 2020; Walia et al. 2022), income (Crystal et al. 2017; Asif and Gurunathan 2020), and treatment costs (Hu et al. 2020) were associated with the acceptance of SDF application.
When SDF was compared with ART, there was better acceptance for SDF regarding treatment duration and comfort (Ali et al. 2021). Acceptance in relation to the aesthetic aspect was similar for both treatments (Ali et al. 2021). In contrast, there was better acceptance of ART in relation to aesthetics than HT (Araújo et al. 2020). HT was investigated in only two of the 19 studies included (Araujo et al. 2020; Thakkar and Jawdekar 2022). When HT was compared with restorations using resin-modified glass ionomer cement, the mean acceptance rate for HT was higher (Thakkar and Jawdekar 2022). The information extracted from the articles has been summarized in Table 2.
Discussion
The objective of the scoping review was to synthesize the evidence on parent acceptance of MIPs for caries lesion management in children. There are a growing number of investigations on MIPs related especially to efficacy (BaniHani et al. 2022). Little is addressed concerning patient-reported outcomes (PRO), despite the emerging need for pertinent information (Ladewig et al. 2018).
The selected studies evaluated the acceptance of parents mainly toward using SDF. Only a few studies investigated the acceptance of ART (Araújo et al. 2020; El-Ghandour et al. 2021; Ali et al. 2021) and HT (Araújo et al. 2020; Thakkar and Jawdekar 2022). The reason is that acceptance of these techniques by parents/caregivers is mostly affected by their aesthetic perception. Specifically, the aesthetic aspect is more questionable in relation to SDF than other MIPs. This hypothesis is strengthened by the observation that parental acceptance was related to the aesthetic aspect in practically all the studies investigated.
The definitive change in tooth color impacted the acceptance of the parents even after clarifications were given about the benefits and efficacy of SDF in the paralysis of caries lesions. The highest acceptance rate was observed when the treatment context involved problems of managing the child’s behavior at the dentist. This result corroborates that observed in a systematic review published in 2020 (Sabbagh et al. 2020). However, this review included only eight studies that addressed the acceptance of SDF. Other MIPs were not investigated or compared.
The aesthetic perception was mentioned in the evaluations of HT acceptance. Although HT treatment is performed on posterior teeth, which are less visible than anterior teeth, the appearance of the HT outcome bothered the parents of Brazilian children, who accepted glass ionomer cement or composite resin restorations better (Araújo et al. 2020). In contrast, HT was better accepted than resin-modified glass ionomer cement restorations by parents of Indian children (Thakkar and Jawdekar 2022). In the last cited study, the question used to evaluate treatment acceptance was not detailed, thus precluding any indication of what factors caused parents to better accept HT. When comparing the acceptance means of HT versus ART, it can be observed that the numerical difference was not clinically relevant, hence leading to the conclusion that the acceptance of treatments was similar (Thakkar and Jawdekar 2022).
Acceptance of the MIP was assessed considering the parents’ perception of images, videos, and observation of their child’s teeth after treatment (Ali et al. 2021). In the post-treatment periods, the aspects evaluated included treatment duration (Ali et al. 2021), aesthetics/appearance (Araújo et al. 2020; El-Ghandour et al. 2021; Ali et al. 2021; Cleary et al. 2022), child comfort/discomfort (Clemens et al. 2018; Araújo et al. 2020; Ali et al. 2021), understanding why the treatment is needed (Araújo et al. 2020), taste (El-Ghandour et al. 2021) and pain (Cleary et al. 2022). Evaluation of acceptance after the procedure aroused doubts about the concept of acceptance adopted in the studies. According to the Health Sciences Descriptors (DECS) 2017, acceptance refers to the willingness to receive health services. Thus, it is expected that acceptance will be evaluated prior to the performance of the dental procedure. However, when considering that the study design involved clinical trials, an a posteriori evaluation would be a warranted avenue of investigation, justified by the need to maintain randomization and avoid interference of the parents’/caregivers’ preference in the allocation of children to the intervention groups. Perhaps, it would be more appropriate to evaluate satisfaction in these studies.
There are some limitations in the present scoping review. Participants in the studies included in the scoping review were approached in dental school clinics or in specialized services. The external validity of the findings of the primary studies was compromised since it did not represent other children who had dental needs and/or were treated with MIPs in private services or others. Another limitation involved the difficulty of comparing the concept of acceptance by parents of children from different countries and cultures. Cultural differences may affect the acceptance of treatment and the aesthetic perception of parents/caregivers. In future studies, it is recommended that primary studies be grouped according to geographic location and cultural similarity.
Evaluating the acceptance of MIPs by parents/caregivers is an important part of the decision-making process for pediatric dental treatment. However, this scoping review revealed that there is still little information available on the acceptance of these procedures and that the studies investigated tended to evaluate the acceptance mostly of SDF.
Conclusion
In general, it was observed that the application of silver diamine fluoride, Hall Technique and atraumatic restorative treatment are acceptable procedures for carious lesion management in children, although the evidence is still limited. A gap remains in the literature regarding the acceptance of other procedures. Therefore, further studies in this area will contribute toward a better understanding of the opinion of parents/caregivers, and thus improve caries lesion management in children.
Available of data and material
Data will be made available by email contact with the corresponding author.
Code availability
Not applicable.
References
Akshitha E, Girish SR, Shankar S, Lalithambigai G, John S. Assessment of parental perceptions and acceptance of silver diamine fluoride staining among the children with dental caries experience in a Town in South India – A cross-sectional study. J Global Oral Health. 2022;5:20–4. https://doi.org/10.25259/JGOH_36_2021
Ali AM, Abdellatif HM, Baghdady SI, Abdelaziz WE, Elkateb MA. Child discomfort and parental acceptability of silver diamine fluoride and alternative restorative treatment: a randomized controlled clinical trial. J Dent. 2021;114:103811 https://doi.org/10.1016/j.jdent.2021.103811
Almarwan M, Almawash A, AlBrekan A, Albluwi S. Parental acceptance for the use of silver diamine fluoride on their special health care-needs child’s primary and permanent teeth. Clin Cosmet Investig Dent. 2021;13:195–200. https://doi.org/10.2147/CCIDE.S307190.
Alshammari AF, Almuqrin AA, Aldakhil AM, Alshammari BH, Lopez JNJ. Parental perceptions and acceptance of silver diamine fluoride treatment in Kingdom of Saudi Arabia. Int J Health Sci (Qassim). 2019;13:25–9.
Araújo MP, Innes NP, Bonifácio CC, Hesse D, Olegário IC, et al. Atraumatic restorative treatment compared to the Hall Technique for occluso-proximal carious lesions in primary molars; 36-month follow-up of a randomised control trial in a school setting. BMC Oral Health. 2020;20:1–18. https://doi.org/10.1186/s12903-020-01298-x.
Asif A, Gurunathan D. Parental acceptance of silver diamine fluoride treatment for children. Int J Res Pharm Sci. 2020;11(4):6432–6435. https://doi.org/10.26452/ijrps.v11i4.3436
Bagher SM, Sabbagh HJ, AlJohani SM, Alharbi G, Aldajani M, Elkhodary H. Parental acceptance of the utilization of silver diamine fluoride on their child’s primary and permanent teeth. Patient Prefer Adherence. 2019;13:829–35. https://doi.org/10.2147/PPA.S205686.
BaniHani A, Santamaría RM, Hu S, Maden M, Albadri S. Minimal intervention dentistry for managing carious lesions into dentine in primary teeth: an umbrella review. Eur Arch Paediatr Dent. 2022;23:667–93. https://doi.org/10.1007/s40368-021-00675-6.
Bassam D, El Rahman DA, Kabil N. Assessing parental acceptance of silver diamine fluoride staining in anterior and posterior teeth of children in a group of Egyptian parents. Adv Dent J. 2022;4:160–7. https://doi.org/10.21608/ADJC.2022.109126.1124
Chaurasiya A, Gojanur S. Evaluation of the clinical efficacy of 38% silver diamine fluoride in arresting dental caries in primary teeth and its parental acceptance. J Indian Soc Pedod Prev Dent. 2021;39:85–9. https://doi.org/10.4103/jisppd.jisppd_34_21.
Cleary J, AL-Hadidi R, Scully A, Yahn W, Zaid Z et al. A 12-month randomized clinical trial of 38% SDF vs. restorative treatment. JDR Clin Trans Res. 2022;7:135–44. https://doi.org/10.1177/23800844211072741.
Clemens J, Gold J, Chaffin J. Effect and acceptance of silver diamine fluoride treatment on dental caries in primary teeth. J Public Health Dent. 2018;78:63–8. https://doi.org/10.1111/jphd.12241.
Corrêa-Faria P, Viana KA, Raggio DP, Hosey MT, Costa LR. Recommended procedures for the management of early childhood caries lesions – a scoping review by the Children Experiencing Dental Anxiety: Collaboration on Research and Education (CEDACORE). BMC Oral Health. 2020;20:75. https://doi.org/10.1186/s12903-020-01067-w.
Crystal YO, Janal MN, Hamilton DS, Niederman R. Parental perceptions and acceptance of silver diamine fluoride staining. J Am Dent Assoc. 2017;148:510–8. https://doi.org/10.1922/CDH_00082Salim05.
El-Ghandour RK, ElTekeya MM, Sharaf AA. Parental satisfaction after using silver diamine fluoride on their children’s primary teeth: a randomized clinical trial. Alexandria Dental J. 2021;46:157–62. https://doi.org/10.21608/adjalexu.2020.41649.1098
Health Sciences Descriptors: DeCS [Internet]. 2017 ed. São Paulo (SP): BIREME / PAHO / WHO. 2017 [updated 2017 May; cited 2017 Jun 13]. Available from: http://decs.bvsalud.org/I/homepagei.htm
Hu S, BaniHani A, Nevitt S, Maden M, Santamaria RM, Albadri S. Hall technique for primary teeth: a systematic review and meta-analysis. Jpn Dent Sci Rev. 2022;58:286–97. https://doi.org/10.1016/j.jdsr.2022.09.003.
Hu S, Meyer B, Lai BWP, Chay PL, Tong HJ. Parental acceptance of silver diamine fluoride in children with autism spectrum disorder. Int J Paediatr Dent. 2020;30:514–22. https://doi.org/10.1111/ipd.12624.
Jayaraman J, Mallineni SK. Editorial: Integration on evidence-based research and practice in preventive and pediatric dentistry. Front Oral Health. 2022;3:1017226. https://doi.org/10.3389/froh.2022.1017226.
Kumar A, Cernigliaro D, Northridge ME, Wu Y, Troxel AB, et al. A survey of caregiver acculturation and acceptance of silver diamine fluoride treatment for childhood caries. BMC Oral Health. 2019;19:228. https://doi.org/10.1186/s12903-019-0915-1.
Ladewig NM, Tedesco TK, Gimenez T, Braga MM, Raggio DP. Patient-reported outcomes associated with different restorative techniques in pediatric dentistry: A systematic review and MTC meta-analysis. PLoS ONE. 2018;13: e0208437. https://doi.org/10.1371/journal.pone.0208437.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69.
Magno MB, Silva LP, Ferreira DM, Barja-Fidalgo F, Fonseca-Gonçalves A. Aesthetic perception, acceptability and satisfaction in the treatment of caries lesions with silver diamine fluoride: a scoping review. Int J Paediatr Dent. 2019;29:257–66. https://doi.org/10.1111/ipd.12465.
Mendes FM, Braga MM, Pássaro AL, Moro BLP, Freitas RD, et al. How researchers should select the best outcomes for randomised clinical trials in paediatric dentistry? Int J Paediatr Dent. 2020;31(Suppl 1):23–30. https://doi.org/10.1111/ipd.12743.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. https://doi.org/10.1186/s12874-018-0611-x.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan – a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
Rønneberg A, Skaare AB, Hofmann B, Espelid I. Variation in caries treatment proposals among dentists in Norway: the best interest of the child. Eur Arch Paediatr Dent. 2017;18:345–53. https://doi.org/10.1007/s40368-017-0298-4.
Sabbagh H, Othman M, Khogeer L, AL-Harbi H, Al Harthi A, Abdulgader AAY. Parental acceptance of silver diamine fluoride application on primary dentition: a systematic review and meta-analysis. BMC Oral Health. 2020;20:227. https://doi.org/10.1186/s12903-020-01195-3.
Salim NA, El-Smadi LA, Sawair FA, Satterthwaite JD. Parental perception and acceptance of silver diamine fluoride treatment among Syrian refugees. Community Dent Health. 2021;38:251–5. https://doi.org/10.1922/CDH_00082Salim05.
Thakkar R, Jawdekar A. A randomized control trial of clinical success and acceptability of the Hall technique and resin-modified glass ionomer cement restorations in sealing carious primary molars. JPRI. 2022;34:35–48. https://doi.org/10.9734/jpri/2022/v34i17B35770.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–73. https://doi.org/10.7326/M18-0850.
Wajahat M, Abbas B, Tariq K, Imran E, Aslam S, Khurshid Z. Parental perception of silver diamine fluoride for the management of dental caries. J Taibah Univ Med Sci. 2022;17:408–14. https://doi.org/10.1016/j.jtumed.2021.11.010.
Walia T, Shetty RM, Al-Sammarraie LM. Parents’ and children’s acceptance of silver diamine fluoride application on primary teeth in the United Arab Emirates. Oral Health Prev Dent. 2022;20:533–40. https://doi.org/10.3290/j.ohpd.b3680331.
World Dental Federation. Minimal intervention dentistry (MID) for managing dental caries. Geneva: World Dental Federation; 2016. https://www.fdiworlddental.org/minimal-intervention-dentistry-mid-managing-dental-caries. Accessed 15 Jun 2023
Funding
The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by HSRJ, BAB and PCF. The first draft of the manuscript was written by HSRJ, BAB and PCF and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
da Silva Ribeiro Júnior, H., de Brito, B.A. & Corrêa-Faria, P. Parents’ acceptance of minimal intervention procedures for dental caries management in children: a scoping review. Eur Arch Paediatr Dent 25, 3–16 (2024). https://doi.org/10.1007/s40368-023-00833-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-023-00833-y