Abstract
Purpose
To evaluate the effect of two herbal mouthwashes containing aloe vera and tea tree oil, on the oral health of school children.
Methods
A double-blinded, placebo-controlled prospective interventional study was conducted in school children aged 8–14 years. The study participants were divided into four groups depending upon the mouthwash used: Group 1 (aloe vera), Group 2 (chlorhexidine), Group 3 (tea tree oil) and Group 4 (placebo). The variables studied included plaque index, gingival index and salivary Streptococcus mutans counts, which were recorded at baseline, 4 weeks after supervised mouth rinse and after 2 weeks of stopping the mouth rinse.
Results
A total of 89 boys and 63 girls were included. A statistically significant decrease in all variables was noted after the use of both the herbal preparations at the end of 4 weeks which was maintained after the 2-week washout period (p < 0.001). The difference in variables between groups using aloe vera, Tea tree oil and chlorhexidine, was not statistically significant.
Conclusion
The use of aloe vera and tea tree oil mouthwashes can decrease plaque, gingivitis and S. mutans in the oral cavity in children. The activity of these two agents is comparable to that of chlorhexidine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The role of dental plaque in periodontal disease and dental caries is well established (Marsh 2010). Dental plaque, an adhesive microbial mass, is a host-associated biofilm that colonises tooth surfaces and is a precursor of dental caries and gingivitis. Streptococcus mutans is one of the common microorganisms embedded in the plaque matrix (Turesky et al. 1970). A major advantage for the plaque-associated microorganisms is the protection offered to them from host defence mechanisms and systemically administered anti-microbial agents. As this matrix is not accessible to blood or interstitial fluids, topically administered antimicrobial agents with enhanced permeability can reach, and effectively control, such pathogens. In the absence of adequate mechanical debridement of plaque due to improper toothbrushing practices, as is common in the paediatric age group (Sandström et al. 2011), the use of mouth washes may have an additive role in preventing plaque formation. The efficacy of chemical agents like chlorhexidine (James et al. 2017; Bowden 1996) and triclosan (Gaffar et al. 1997) against plaque formation is known. However, they are associated with the side effects of staining of teeth and altered taste. The absence of such detrimental effects with herbal agents having antimicrobial and anti-inflammatory properties may improve patient compliance. Aloe vera is proved to have antibacterial, antifungal and antiviral effects along with an astringent effect (Wynn 2005). It has been used in alternative dentistry for the treatment of gingivitis and periodontitis. Tea tree oil, is another herbal medication composed of 1,8 cineol and terpinen-4-ol, known to have antibacterial and antifungal effects (Carson et al. 2006).
In our study, we attempt to compare the efficacy of herbal mouthwashes containing aloe vera (7%) and tea tree oil (0.2%) with chlorhexidine as the gold standard, in school children.
Materials and methods
This was a double-blinded, placebo-controlled prospective interventional study conducted at the Department of Paedodontics and Preventive dentistry, Manipal College of Dental Sciences. The study was approved by the Institutional Ethics Committee and followed the tenets of the Declaration of Helsinki. The study participants included school children in the age range of 8–14 years, from two schools located within 10 km from the institute. A written informed consent for participation in the study was obtained from the parents of the students recruited. The appropriate permissions from the school authorities were also obtained prior to initiation of the study. Children with plaque scores and gingival scores > 1 and similar oral hygiene practices were included for the study. Children who had pulp involvement due to severe caries, or those with chronic systemic illness were excluded. Those who had received any form of antibiotic or anti-inflammatory medication 1 month prior to, or during the study, were also excluded.
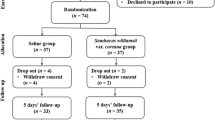
The study participants were divided into four groups depending upon the mouthwash used: Group 1 (aloe vera), Group 2 (Chlorhexidine), Group 3 (tea tree oil) and Group 4 (placebo). To achieve an 80% power and 5% significance level, using a two-sided analysis of variance (ANOVA) test, a sample size of 140 was calculated as sufficient to detect the difference between the four groups. To generate a minimum of 35 samples per group, a convenient sample of 152 children of age group between 8 and 14 years was selected who met the inclusion criteria.
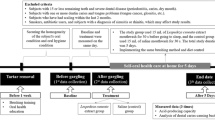
The study variables recorded include plaque index of Silness and Loe (1964), gingival index of Loe and Silness (1967), and microbiological analysis to determine the salivary S. mutans count. The recordings were performed at baseline, after 4 weeks of supervised use of mouthwash, and again after 2 weeks of stopping the mouth wash. The dental evaluation was carried out by a single examiner, trained in paediatric dentistry.
Preparation of aloe vera mouthwash
The ingredients used for the preparation of the aloe vera mouthwash were aloe vera (7 g), peppermint oil (0.025 g), tween-80 (0.5 g), benzyl alcohol (0.2 g), and Milli-Q water q.s. to 100 ml/g. The pre-weighed Tween-80, which serves as a surfactant, was added to one-fourth water and mixed well. A measured quantity of aloe vera extract (FALCON Exporters of Essential oils, Bangalore, India) was added to the above mixture and stirred. To this preparation, peppermint oil and benzyl alcohol were added. To make up the volume, water was added and mixed well.
Preparation of tea tree oil mouthwash
The ingredients used included tea tree oil (0.5 g), Glycerine (5 g), Propylene glycol (5 g), Tween-80 (2.5 g), Benzyl alcohol (0.2 g), Milli-Q water q.s. (100 ml/g). Glycerine and propylene glycol were weighed separately and mixed. Tween-80, used as a surfactant, is then weighed and added to the above mix. Tea tree oil (FALCON Exporters of Essential oils, Bangalore, India) was then weighed and mixed to it. About 50% water was added to the above preparation, followed by addition of benzyl alcohol. To make up the volume up to 100 ml, water was added and mixed well. As tea tree oil has its own flavour, no flavouring agent was added.
Chlorhexidine gluconate 0.2% mouthwash and distilled water were used for groups 2 (chlorhexidine group) and 4 (placebo group), respectively.
Coding and blinding
The mouthwashes and the placebo were made of same colour and 300 ml of each of the mouthwash was dispensed in identical bottles. The bottles were covered and coded before dispensing to the children. The coding was done by a person who was not involved in the study; so, that the double blinding design of the study was maintained. Each child in the various groups was given two bottles containing 300 ml of the respective mouthwash, of which one was kept at school and the other at home.
Administration of the mouthwash
The children were trained, and the teachers and parents were educated in the use of mouthwash so that the children could use the mouthwash under their supervision. Each participant used the respective mouthwash twice daily, once after lunch and once after dinner, from their respective bottles. For each rinse, 10 ml of mouthwash was taken in the bottle lid and swished in the mouth for 30 s, after which it was spit out. Thereafter, they were asked to refrain from eating, drinking or rinsing their mouth for 30 min. Pre-existing oral hygiene practices of the participants were continued during the study period.
Microbiological analysis
The S. mutans count was measured in Colony Forming Units (CFU)/ml to check the antimicrobial activity of the mouthwash (Prabhakar et al. 2009). Stimulated saliva from the participants was collected for microbiological analysis. After abstaining from any food, fluids or oral hygiene measures for an hour, the children were asked to chew on paraffin wax for 5 min. The saliva, thus, stimulated was allowed to pool in the mouth. At the end of 5 min, the children were made to expectorate into sterile sample collecting bottles. One ml of the stimulated saliva, thus, collected was transferred into a bottle containing 5-ml thioglycolate broth used as the transport media for the saliva. The transport medium was used to ensure viability of the organism till it was transported to the laboratory within 30 min. The Mitis salivarius agar culture media were prepared according to the manufacturer’s instructions (Hi-Media company). After streaking the saliva samples collected on this media as well as blood agar plates, and incubation for 48 h at 37 °C, the colonies were identified by their morphology, and scored depending on their number, as Colony Forming Units (CFU)/ml.
Statistical analysis
The groups were de-coded before the data were handed over to the statistician. The collected data were subjected to statistical analysis. For intra-group comparison, paired t test was applied; while for inter-group comparison, the analysis of variance (ANOVA) and Tukey’s HSD test was applied. All tests were carried out in the SPSS software (12.0, SPSS Inc., Chicago Ill, USA). A p value less than 0.05 was considered as statistically significant.
Results
A total of 152 children were equally divided by simple randomization into four groups. Among the 38 participants in each group, 25 (65.78%) in group 1, 18 (47.36%) in group 2, 19 (50%) in group 3 and 27 (71.05%) in group 4 were males. The mean age in groups 1, 2, 3 and 4 was 11.92 ± 1.84 years, 12.15 ± 1.94 years, 12.16 ± 1.97 years and 11.29 ± 2.16 years, respectively. The differences in the age and gender distribution between the four study groups were not statistically significant.
The mean values of the plaque score, gingival score and S. mutans count at the various intervals are detailed in Tables 1, 2 and 3, respectively.
The mean plaque score showed a highly significant reduction in the Groups 1, 2, and 3 with p < 0.001, between baseline and 4 weeks of mouth rinse [mean (± SD) values in Group 1: 1.18 (± 0.25); Group 2: 1.18 (± 0.25); Group 3: 1.17 (± 0.26); Group 4: 0.07 (± 0.17)] as well as between baseline and 2 weeks of washout period [mean(SD) values in Group 1: 1.09 (± 0.26); Group 2: 1.07 (± 0.24); Group 3: 1.09 (± 0.27); Group 4: 0.02 (± 0.15)] when analysed using the paired t test.
The mean gingival score showed a highly significant reduction in the Groups 1, 2, and 3 with p < 0.001, between baseline and 4 weeks of mouth rinse [mean(SD) values in Group 1: 0.91 (± 0.15); Group 2: 0.89 (± 0.16); Group 3: 0.90 (± 0.20); Group 4: 0.07 (± 0.19)] as well as between baseline and 2 weeks of washout period [mean(SD) values in Group 1: 0.82 (± 0.15); Group 2: 0.79 (± 0.15); Group 3: 0.83 (± 0.20); Group 4: − 0.01 (± 0.17)] when analysed using the paired t test.
The mean S. mutans count showed a statistically significant reduction in the Groups 1, 2, and 3 with p ≤ 0.001, between baseline and 4 weeks of mouth rinse [mean(SD) values in Group 1: 61,048.72 (± 109,159.86); Group 2: 140,131.58 (± 176,025.16); Group 3: 124,321.62 (± 168,225.70); Group 4: − 6540.54 (± 20,503.94)] as well as between baseline and 2 weeks of washout period [mean(SD) values in Group 1: 61,007.69 (± 108,610.54); Group 2: 140,284.21 (± 175,962.80); Group 3: 124,224.32 (± 168,208.57); Group 4: − 14,286.49 (± 33,290.87)] when analysed using the paired t test.
At the end of the 2-week wash out period, a statistically significant increase in the plaque score and gingival score was observed in all groups when compared to the scores after 4 weeks of mouth rinse (p ≤ 0.001). However, the S. mutans counts did not show a significant rise during the same period.
On comparing the different groups using the ANOVA followed by Tukey’s HSD test, intergroup difference in the baseline values of plaque score, gingival score and S. mutans counts was not significant. However, for all the parameters, when compared to the placebo, Groups 1, 2 and 3 showed a highly significant reduction of scores and counts (p < 0.001). There was no significant difference noted in the parameters when Groups 1, 2 and 3 were compared with each other.
Discussion
The results of our study indicate that both the herbal mouth rinses had an efficacy comparable with chlorhexidine mouthwash, in reducing plaque and gingivitis.
The population studied included school children who were old enough to cooperate for the procedures involved. They were divided into the four groups by simple randomization to avoid bias. Moreover, the parents and teachers were initially educated regarding the technique of mouth rinse to enable them to supervise the children thereby improving compliance to the methodology. The children were instructed to rinse their mouth with 10 ml of their respective mouthwashes for 30 s twice daily, once after lunch and dinner. The increase in frequency and volume of mouth rinse is known to improve the concentration of the agent in the oral cavity (Bonsvoll and Gjermo 1978). A four-week interval for the mouth rinsing activity was chosen on basis of an earlier study which describes an effective reduction of plaque and gingivitis in the same period (Villalobos et al. 2001). The substantivity of the study drug was determined after a duration of 2 weeks of stopping the mouth rinse. A similar washout period was adopted by Groppo et al. (2002).
The plaque score was found to be significantly lowered in our study, with the use of mouthwash containing aloe vera as well as tea tree oil when compared to the placebo. The scores were comparable to the use of chlorhexidine mouthwash. Such plaque reducing ability has been reported by Villalobos et al. (2001) and with the use of aloe vera dentifrice, by de Oliveira et al. (2008) Similarly, Neto et al. (2008) have demonstrated the anti-plaque activity of chlorhexidine mouthwash after 14 days of use. However, our findings differ regarding the anti-plaque activity of tea tree oil, from the results of Soukoulis and Hirsch (2004) They reported a decrease in oral bacterial level but no decrease in plaque levels. This difference may be attributed to the mode of application of the agent being a gel form in their study versus a mouth rinse used in the present study. The ability of a mouth rinse to reach site otherwise inaccessible to a dentifrice or tooth brush may aid in its ability to prevent plaque (Kleber et al. 1981).
The gingival score was also found to be significantly lowered using aloe vera and tea tree oil containing mouthwashes when compared to the placebo. The scores were comparable with those obtained with chlorhexidine mouthwash. Gingival inflammation and bleeding have been reported to have been controlled using dentifrices and mouthwashes using components including aloe vera, tea tree oil and chlorhexidine in other studies (de Oliveira et al. 2008; Soukoulis and Hirsch 2004; Botelho et al. 2009). The anti-inflammatory effect of aloe vera is attributed to the presence of peptidase bradykinase which acts against the proinflammatory mediator, bradykinin (Shelton 1991).
Streptococcus mutans is one of the organisms implicated in the development of dental caries, and its numbers in the oral cavity may be indicative of caries activity (Turesky et al. 1970). In our study, the aloe vera containing mouthwash was able to significantly reduce the counts of S. mutans compared to placebo. The antibacterial properties of aloe vera have been attributed to the negatively charged polysaccharides it contains (Van Dijk 2005), and Lee et al. (2004) found it particularly effective against S. mutans.
The mouth wash containing tea tree oil also showed significant reduction of S. mutans colonies after 4 weeks of use when compared to the placebo. Similar results have been reported by Prabhakar et al. (2009). The bactericidal activity of tea tree oil has been attributed to 1,8 cineole, which increases the permeability of the bacterial cell membranes which eventually leads to cell disruption (Carson et al. 2006).
Tandon et al. (2010) have described the efficacy of chlorhexidine mouthwash against S. mutans, and the same was reconfirmed in our study.
In our study, an intergroup comparison showed that the aloe vera, chlorhexidine and tea tree oil used in the three groups had a similar efficacy against S. mutans. At the end of the 2-week washout phase, a significant increase in the scores of plaque and gingivitis in all the groups was observed indicative of poor substantivity. However, the group in whom chlorhexidine mouth wash was used did not have an increase in S. mutans counts, as compared to the other groups, suggestive of a greater efficacy of chlorhexidine in comparison to aloe vera or tea tree oil against S. mutans.
Another interesting observation in the study was a marginal improvement in plaque and gingival scores with the placebo, at the end of the 4-week period. This can probably be attributed to the more vigorous and regular mouth rinsing with the placebo by the group than earlier, either because they were supervised or due to a behavioural modification called the Hawthorne effect (McCarney et al. 2007).
Although our study attempts to describe the efficacy of aloe vera and tea tree oil by comparing it to chlorhexidine as a gold standard, it does not address the possible outcomes after long-term use of these herbal preparations. Hence, further studies exploring the potential adverse effects of their usage are needed before presuming their safety in paediatric use.
Conclusion
The present study compared the efficacy of two herbal mouthwashes (aloe vera and tea tree oil) with chlorhexidine as a gold standard, in the paediatric, caries prone age group and found that they were as effective in controlling plaque and gingivitis as chlorhexidine. Chlorhexidine, however, had better substantivity against S. mutans.
References
Bonsvoll P, Gjermo P. A comparison between chlorhexidine and some quaternary ammonium compounds with regards to retention, salivary concentration and plaque-inhibiting effects in the human mouth after mouth rinses. Arch Oral Biol. 1978;23:289–94.
Botelho MA, dos Santos RA, Martins JG, et al. Comparative effect of an essential oil mouthrinse on plaque, gingivitis and salivary Streptococcus mutans levels: a double blind randomized study. Phytother Res. 2009;23:1214–9.
Bowden GH. Mutans streptococci caries and chlorhexidine. J Can Dent Assoc. 1996;62(700):703–7.
Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (tea tree) oil: a review of antimicrobial and other medicinal properties. Clin Microbiol Rev. 2006;19:50–62.
de Oliveira SM, Torres TC, Pereira SL, Mota OM, Carlos MX. Effect of a dentifrice containing aloe vera on plaque and gingivitis control. A double-blind clinical study in humans. J Appl Oral Sci. 2008;16:293–6.
Gaffar A, Afflitto J, Nabi N. Chemical agents for the control of plaque and plaque microflora: an overview. Eur J Oral Sci. 1997;105:502–7.
Groppo FC, Ramacciato JC, Simoes RP, Florio FM, Sartoratto A. Antimicrobial activity of garlic, tea tree oil, and chlorhexidine against oral microorganisms. Int Dent J. 2002;52:433–7.
James P, Worthington HV, Parnell C, et al. Chlorhexidine mouthrinse as an adjunctive treatment for gingival health. Cochrane Database Syst Rev. 2017;3:CD008676. https://doi.org/10.1002/14651858.cd008676.pub2.
Kleber CJ, Putt MS, Muhler JC. Duration and pattern of tooth brushing in childern using a gel or paste dentifrice. J Am Dent Assoc. 1981;103:723–6.
Lee SS, Zhang W, Li Y. The antimicrobial potential of 14 natural herbal dentifrices: results of an in vitro diffusion method study. J Am Dent Assoc. 2004;135:1133–41.
Loe H, Silness J. Periodontal disease in pregnancy 1: prevalence and severity. Acta Odontol Scand. 1967;21:533–51.
Marsh PD. Microbiology of dental plaque biofilms and their role in oral health and caries. Dent Clin N Am. 2010;54:441–54.
McCarney R, Warner J, Iliffe S, van Haselen R, Griffin M, Fisher P. The Hawthorne effect: a randomised, controlled trial. BMC Med Res Methodol. 2007;3(7):30.
Neto CAF, Parolo CCF, Rösing CK, Maltz M. Comparative analysis of the effect of two chlorhexidine mouthrinses on plaque accumulation and gingival bleeding. Braz Oral Res. 2008;22:139–44.
Prabhakar AR, Ahuja V, Basappa N. Effect of curry leaves, garlic and tea tree oil on Streptococcus mutans and Lactobacilli in children: a clinical and microbiological study. Pesq Bras Odontoped Clin Integr João Pessoa. 2009;9:259–63.
Sandström A, Cressey J, Stecksén-Blicks C. Tooth-brushing behaviour in 6–12 year olds. Int J Paediatr Dent. 2011;21:43–9.
Shelton RM. Aloe vera. Its chemical and therapeutic properties. Int J Dermatol. 1991;30:679–83.
Silness J, Loe H. Periodontal disease in children, correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–35.
Soukoulis S, Hirsch R. The effects of a tea tree oil-containing gel on plaque and chronic gingivitis. Aust Dent J. 2004;49:78–83.
Tandon S, Gupta K, Rao S, Malagi KJ. Effect of triphala mouthwash on the caries status. Int J Ayurveda Res. 2010;1:93–9.
Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol. 1970;41:41–3.
Van Dijk W. Negatively charged polysaccharides derivable from aloe vera. United States Patent, 2005. Pub. No. US 2005/0019433 A1. www.freepatentsonline.com.
Villalobos OJ, Salazar CR, De Sanchez GR. Effect of aloe vera compound mouthwash in plaque and gingival inflammation. Acta odontol Acta Odontol Venez. 2001;39:16–24.
Wynn RL. Aloe vera gel: update for dentistry. Pharmacology today. Gen Dent. 2005;5:6–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kamath, N.P., Tandon, S., Nayak, R. et al. The effect of aloe vera and tea tree oil mouthwashes on the oral health of school children. Eur Arch Paediatr Dent 21, 61–66 (2020). https://doi.org/10.1007/s40368-019-00445-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-019-00445-5