Abstract
Background
Soft-tissue sarcomas (STS) represent a diverse group of rare malignancies, underscoring the need for precise risk stratification. [18F]fluoro‑2‑deoxy‑2‑d‑glucose positron emission tomography ([18F]FDG PET) imaging parameters have been proposed as potential prognostic indicators in several cancer types, yet their significance in STS remains under investigation. This study aimed to synthesize the available evidence and assess the prognostic value of these parameters.
Methods
A systematic review and meta-analysis was conducted, employing a comprehensive literature search across multiple databases. The prognostic value of [18F]FDG PET parameters, including pre- and post- treatment standardized uptake values (SUV1, SUV2), pretreatment metabolic tumor volume (MTV1) and total lesion glycolysis (TLG1) on event-free survival (EFS) and overall survival (OS) in patients with STS was examined.
Results
Thirty-one studies with 1,932 patients were identified. The analyses demonstrated significant relationships between higher SUV1 (hazard ratio, HR 1.68 for EFS and 3.07 for OS, p < 0.001), SUV2 (HR 3.13 for EFS and 2.09 for OS, p < 0.001 and p = 0.001 respectively), MTV1 (HR 2.29 for EFS and 3.05 for OS, p = 0.011 and p < 0.001 respectively), TLG1 (HR 2.85 for EFS and 3.23 for OS, p = 0.032 and p = 0.002 respectively) and poorer survival outcomes. However, the association of these parameters with survival outcomes was non-significant in pediatric patients.
Conclusion
This study suggests that [18F]FDG PET parameters could serve as important prognostic markers in adults with STS, but not in pediatric patients. Future studies with larger cohorts and uniform methodologies are critical to confirm and build upon these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Soft-tissue sarcomas (STS) are rare tumors that present challenges in cancer management due to their diverse biological characteristics and clinical presentations, which are primarily associated with their origin from mesenchymal cells [1, 2]. Representing approximately 1% of malignancies in adults and 8–15% in children, adolescents, and young adults [3, 4], the complexity of STS challenges diagnosis, treatment planning and prognostic evaluation [5,6,7]. Despite progressive strides in surgical techniques, radiation oncology, and systemic therapies, the prognosis for patients with STS remains unsatisfactory, emphasizing the urgent necessity for enhanced prognostic markers and therapeutic strategies [8].
Traditional prognostic factors, including patient age, presence of metastasis, tumor size, histological type, and tumor grade, guide clinical decision-making in oncology [9, 10]. However, these factors have limited efficacy in accurately predicting patient outcomes, thereby highlighting the compelling need for the development and validation of more reliable and accurate prognostic tools. A reliable prognostic tool in soft-tissue sarcomas may enhance patient management by allowing for the customization of treatment strategies, such as precise surgical techniques, individualized systemic therapies, and patient-oriented follow-up schedules, thereby improving treatment outcomes and patient quality of life.
The pivotal role of [18F]fluoro‑2‑deoxy‑2‑d‑glucosepositron emission tomography ([18F]FDG PET) in oncology has been well-established, and is recognized for its substantial contribution to tumor staging and grading, monitoring treatment efficacy, detecting local or distant recurrence, and facilitating post-treatment follow-up management [11]. Despite this, the ability of [18F]FDG PET parameters to predict survival outcomes in patients with sarcoma remains a subject of debate, as research has presented both supportive and contradictory findings [12,13,14,15,16]. Prior meta-analyses have examined the prognostic value of [18F]FDG PET parameters in patients with sarcoma [17,18,19], but recent research indicates a potentially diminished prognostic efficacy of these parameters in the pediatric population [19,20,21]. Importantly, previous meta-analyses failed to consider the pediatric population separately, thereby potentially obscuring the true prognostic value of [18F]FDG PET parameters due to known biological and clinical differences between pediatric and adult sarcomas and among different sarcoma subtypes [3, 7].
To address this gap, we performed a systematic review and meta-analysis that incorporates an in-depth analysis of age subgroups and sensitivity analyses to comprehensively evaluate the relationship between [18F]FDG PET metabolic parameters and survival outcomes in patients with STS.
Materials and methods
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [22]. The study protocol was registered with the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY) under the registration number INPLASY202370087 (https://doi.org/10.37766/inplasy2023.7.0087).
Search strategy
A systematic literature search of studies published within the last 15 years (from Jan 1, 2008 to June 1, 2023, date of search: June 15, 2023) was performed in Medline, PubMed, Google Scholar, and the Cochrane Library by two independent investigators (MY and LB). The search methodology utilized Medical Subject Headings (MeSH). Both backward and forward snowballing methods were also used for an exhaustive search. Language restrictions were not applied.
The detailed search strategy and queries are available in the supplemental material (Supplemental Appendix 1).
Eligibility criteria and study selection
After automatic removal of duplicate records, the remaining studies were screened by two independent researchers (MY and YL) for eligibility. We considered studies that met the following criteria:
-
1.
Population: children, adolescents and adults with STS undergoing baseline and/or post-neoadjuvant chemotherapy (NAC) PET/CT with [18F]FDG;
-
2.
Exposure: high baseline/post-NAC maximum standardized uptake value (SUVmax), high SUV ratio (SUV2 [post-NAC] / SUV1 [baseline]), high baseline metabolic tumor volume (MTV1), high baseline total lesion glycolysis (TLG1) values;
-
3.
Comparator: low baseline/post-NAC SUVmax, low SUV ratio, low baseline MTV1, low baseline TLG1 values;
-
4.
Outcomes: event-free survival (EFS), overall survival (OS);
-
5.
Study design: prospective and retrospective cohort studies.
-
6.
The full text of potentially eligible studies was assessed by applying the inclusion and exclusion criteria.
The inclusion criteria for this study were: cohort studies involving patients diagnosed with STS, specifically investigating the association between [18F]FDG PET metabolic parameters (SUVmax, MTV, or TLG) and survival outcomes (OS or EFS).
Studies were excluded if they met one or more of the following criteria: (1) review articles, case reports; (2) other tumors (bone sarcomas, Ewing’s sarcomas); (3) no relevant outcomes; (4) animal studies; (5) outcomes reported for mixed groups (bone sarcomas and STS); (6) other radiopharmaceuticals used; (7) duplicated publications.
Any divergences were resolved through consensus, with the supervising researcher (YL) stepping in when necessary.
Data extraction
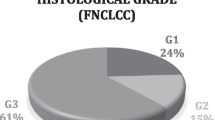
A dedicated data collection form was developed for this review, which two authors (MY and LB) used to independently assess the complete manuscripts of all included trials and extract the data. Extracted information encompassed: (1) Basic study details such as the first author, publication year, country, journal, study design, period, the number of centers involved, follow-up period, and sample size; (2) [18F]FDG PET scan data like PET scanners used, fasting duration, pre-injection blood glucose tests, post-injection interval, [18F]FDG dose, and PET/CT timing; (3) Patient and tumor specifics including cancer type, disease stage, histological grade (using the Fédération Nationale des Centres de Lutte Contre Le Cancer [FNCLCC] grading system if applicable [23]), tumor location, patient age and sex; (4) [18F]FDG PET parameters such as MTV and TLG segmentation methods, SUV type, cut-off determination method and values, and effect estimates for study outcomes. We also examined the supplementary or additional files associated with the included articles for any pertinent data.
SUV1 and SUV2 were defined as the SUV of the primary lesion pre- and post- NAC, respectively. The SUV ratio was calculated as SUV2/SUV1. TLG1 and MTV1 values were extracted from baseline [18F]FDG PET scans.
Outcome measures such as OS, EFS, Kaplan–Meier curves, and hazard ratio (HR) values were extracted. For the purpose of this meta-analysis, we consolidated progression-free survival, disease-free survival, metastasis-free survival, and event-free survival from the included studies, collectively defining them as EFS.
HR values were used to measure the association between [18F]FDG PET metabolic parameters and survival. Univariate HR values were extracted directly if available or calculated using Tierney et al. methodology for original studies [24], univariate HR were replaced with multivariable if available. This involved gathering relevant data, including p values from the log-rank test, the total count of patients in each group, and the number of events, allowing us to calculate univariate HRs indirectly. Direct HR extraction was performed from provided survival curves when present.
Data analysis and synthesis
We used STATA 17 (StataCorp LLC, Texas, US) and Cochrane tool Review Manager (RevMan version 5.3) to perform meta-analysis.
The impact of [18F]FDG PET parameters on survival outcomes was assessed by calculating the pooled HR values with its 95% confidential intervals (CIs).
Inter-study heterogeneity was evaluated using the I-squared (I2) statistic and the Cochrane Q test, as recommended by the Cochrane Handbook [25]. If the value was ≥ 40% and/or p < 0.05, an effect estimate was considered as significant for heterogeneity and random-effects model (restricted maximum–likelihood, REML) was used. Otherwise, a fixed-effects model based on the inverse-variance approach was used. Results of meta-analysis were presented using forest-plots. Statistical significance was set at 0.05 for hypothesis testing.
We conducted a meta-regression analysis, leveraging the REML random-effects model, to ascertain if the relationships between SUV1 and survival outcomes might be affected by variables such as patient age, sex, histological grade, tumor location and stage, cut-off value, and the design of the study [26]. The results of the meta-regression were graphically represented using bubble-plots. The correlation between clinical parameters of eligible studies was evaluated using Spearman’s rank correlation coefficient.
Trial sequential analysis (TSA) was applied to examine the sufficiency and currently available evidence. TSA was conducted for survival outcomes and SUV1 parameter, which is supported by the most substantial evidence. The analysis was carried out utilizing dedicated TSA software (Trial Sequential Analysis (TSA) [Computer program]. Version 0.9.5.10 Beta. The Copenhagen Trial Unit, Centre for Clinical Intervention Research, The Capital Region, Copenhagen University Hospital—Rigshospitalet, 2021). If the cumulative Z-curve crosses the monitoring boundaries, it suggests that sufficient evidence for the association between high SUV1 values (exposure) and the survival outcome may have been reached, indicating that further studies may not be needed [27]. The type I error rate was maintained at 5% (α = 0.05), and required heterogeneity adjusted information sizes were calculated with 90% power (β = 0.10), relative risk reduction was set at 30%.
Internal validity and risk of bias assessment
The internal validity and risk of bias were assessed by two independent reviewers (MY, LB) using the “Tool to assess risk of bias in cohort studies” contributed by the CLARITY Group at McMaster University [28], the explanation for risk of bias assessment is presented in Supplemental Appendix 2. Eight areas were evaluated: patient selection, exposure assessment, pre-existing exposure, control matching, confounding assessment, measurement of the outcome, follow-up assessment, and co-intervention assessment. The risk of bias was rated as low, moderate, or high. The results were presented using the “Risk-of-Bias Visualization tool” [29].
Publication bias and small-study effects were assessed using Egger’s test and funnel plot analysis [30]. We also used a GRADE systematic approach to rate the certainty of evidence. Baseline evidence level was high as for studies of prognostic factor [31].
Sensitivity analysis
We conducted a sensitivity analysis in several ways: Firstly, we analyzed the multivariable HRs obtained from the Cox multivariable regression analysis in the original studies.
Secondly, we separately examined studies focusing on pediatric and adult patients with STS. Pediatric patients were defined per the Food and Drug Administration (FDA) guidelines, which classify the pediatric population as birth through 21 years of age [32]. The patient populations in the majority of the eligible studies consisted of a diverse mix of both adults and children, in varying proportions. To clearly categorize the studies based on patient demographics, we employed a strategy wherein studies were classified as ‘pediatric’ if they comprised 75% or more pediatric patients. Conversely, studies were labeled as ‘adult’ if pediatric patients made up less than 25% of the study population.
Finally, we evaluated the results of studies with only low-to-moderate overall risk of bias.
Results
Baseline characteristics of the included studies
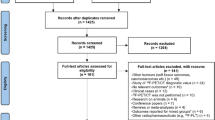
The initial literature search yielded a total of 6,775 studies across multiple databases, and an additional 41 studies were obtained through other sources (Fig. 1).
Following the removal of duplicate and irrelevant records, the remaining 1,495 articles underwent title and abstract screening. From these, 147 full-text articles were reviewed for eligibility criteria. A total of 1932 patients from 31 studies were included in this systematic review and meta-analysis [12,13,14,15, 20, 33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58] with major exclusions presented in Supplemental Table 1.
The characteristics of the included studies are shown in Table 1.
Among the 31 included studies, four were prospective observational [45, 46, 52, 55]; six studies [14, 42, 43, 45, 50, 52] were designed as multicentric, and the remaining studies followed a single-center design. The mean age of the patients within included studies ranged between 5 to 74 years, and six studies were designated as ‘pediatric’ [12, 13, 39, 41, 42, 45]. The included studies varied in aspects of metastatic disease stage, tumor location, and histological grade. The distribution of soft-tissue sarcoma types across the included studies can be found in Supplemental Table 2. Notably, all studies classified as ‘pediatric’ incorporated patients diagnosed with rhabdomyosarcomas (RMS), with a similar distribution in RMS subtypes (embryonal, alveolar).
Table 2 outlines the different methodologies of [18F]FDG PET scanning employed across the studies.
The scanning protocols administered were not uniform and varied according to the individual study design. Likewise, there was a lack of consistency in the methods used to determine the cut-off values across the studies. Sixteen studies leveraged receiver operating characteristic (ROC) curves, seven utilized median values, two applied cut-off point analyses, two others relied on the minimal p value method, and one referred to previous research for their cut-off. A comprehensive summary of the cut-off values employed in the eligible studies can be found in Supplemental Table 3. Two studies used SUVpeak [43, 46] and one study used SUVmean [20] instead of SUVmax. For MTV and TLG calculation, six studies applied a fixed absolute segmentation method (SUV 2–2.5) [36,37,38, 44, 50, 51], and three studies used a fixed relative threshold of 40% [34, 40, 42].
Prognostic value of [18F]FDG PET parameters for EFS and OS
SUV1: In a meta-analysis of 16 studies involving 1222 patients, we found a significant association between SUV1 and EFS (HR = 1.68, p < 0.001, high heterogeneity: I2 = 94%; Fig. 2; Supplemental Fig. 2, Table 3).
Forest plot for event-free survival (A) and overall survival (B) representing the Hazard ratios (HRs) for high pretreatment SUV values versus low values. The plot displays the study, HR with confidence interval (CI), heterogeneity parameters and p value. The size of the squares indicates the weight of the studies, the diamond represents the pooled HR with CI
This relationship was confirmed in multivariable data analysis (HR = 1.75, p = 0.025) and in the subgroup analysis of low-to-moderate bias studies (HR = 1.82, p = 0.004). ‘Adult’ studies (n = 610) exhibited a stronger correlation (HR = 2.49, p < 0.001, I2 = 0), whereas ‘pediatric’ studies (n = 517) found no significant association (HR = 1.14, p = 0.2, Fig. 3).
The correlation of SUV1 with OS, as confirmed by 22 studies encompassing 1,312 patients, was significant (HR = 3.07, p < 0.001, high heterogeneity: I2 = 74%; Fig. 2; Supplemental Fig. 2, Table 3). This outcome was validated by subgroup analyses based on the statistical analysis method (HR = 2.84, p = 0.002), as well as by the subgroup analysis of low-to-moderate bias studies (HR = 2.94, p < 0.001). This association was more pronounced in ‘adult’ studies (n = 964, HR = 3.95, p < 0.001, I2 = 3) and was non-significant in ‘pediatric’ studies (n = 348, HR = 1.14, p = 0.4, Fig. 3).
SUV2: A significant relationship was found between high SUV2 and poor EFS across three studies (n = 163, HR = 3.13, p < 0.001, high heterogeneity: I2 = 59%; Supplemental Fig. 3, Table 3), as was the SUV2 and OS relationship (n = 163, HR = 2.09, p = 0.001, I2 = 0%; Supplemental Fig. 3, Table 3). No subgroup analyses were conducted for these parameters.
SUV ratio: The analysis of five studies (n = 432) established a significant association between a low SUV ratio and improved EFS (HR = 0.61, p = 0.049, I2 = 22%; Supplemental Fig. 4, Table 3), particularly in ‘adult’ studies (n = 77, HR = 0.26, p = 0.003), but not in ‘pediatric’ ones (n = 260, HR = 0.87, p = 0.6, Table 3). Conversely, no significant association was found between SUV ratio and OS across five studies (n = 283, HR = 0.47, p = 0.13, high heterogeneity: I2 = 84%; Supplemental Fig. 4, Table 3).
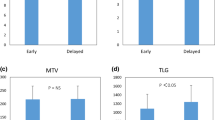
MTV1: An assessment of five studies on MTV1 and EFS encompassing 317 patients revealed a significant association (HR = 2.29, p = 0.011, high heterogeneity: I2 = 75%; Supplemental Fig. 5, Table 3), which was stronger in ‘adult’ studies (n = 153, HR = 3.54, p < 0.001, I2 = 0), but not significant in ‘pediatric’ studies (n = 164, HR = 1.54, p = 0.4, Table 3). The MTV1 and OS correlation across nine studies (n = 381) was also significant (HR = 3.05, p < 0.001, high heterogeneity: I2 = 72%; Supplemental Fig. 5, Table 3), and was significant in ‘adult’ studies (n = 217, HR = 4.06, p < 0.001) and non-significant in ‘pediatric’ studies (n = 164, HR = 1.51, p = 0.4, Table 3).
TLG1: Exploration of TLG1 and EFS in four studies with 216 patients demonstrated a significant association (HR = 2.85, p = 0.032, high heterogeneity: I2 = 77%; Supplemental Fig. 6, Table 3). The TLG1 and OS relationship across seven studies (n = 261) also revealed a significant association (HR = 3.23, p = 0.002, high heterogeneity: I2 = 67%; Supplemental Fig. 6, Table 3). Subgroup analyses were not performed for these correlations.
Risk of bias and GRADE assessment
The overall risk of bias of the 31 enrolled studies was judged as ‘low’ in three trials, ‘some concerns’ in 9 trials and ‘high’ in 16 trials (Supplemental Fig. 1). The primary sources of bias were the lack of matching for confounding variables, inconsistent follow-up, and variation in co-interventions among the studies.
Egger’s test and funnel plot analysis revealed presence of publication bias and small-study effects for the majority of the analyses (Table 3, Supplemental Figs. 7–11).
Moderate level of evidence (GRADE approach) was stated for the evidence of decreased EFS and OS in adult patients with high SUV1 and MTV1 (Supplemental Table 4). However, the certainty of evidence for other [18F]FDG PET metabolic parameters was classified as ‘very low’.
Meta-regression
The meta-regression analysis revealed patient age as the only significant modifier of the association between SUV1 and survival outcomes (Supplemental Table 5). Specifically, an elevation in the average patient age within the study was significantly tied to an amplified HR for SUV1 and survival outcomes (Coeff. 0.016 for EFS and 0.026 for OS, p < 0.001, Fig. 3, Supplemental Figs. 13, 14). An inverse correlation was observed between the average patient age in the studies and the proportion of patients diagnosed with high-grade tumors (Supplemental Table 6 and Supplemental Fig. 12).
Trial sequential analysis
For association between SUV1 and survival outcomes in adult patients with STS the TSA analysis showed that the cumulative z-curve, after crossing the O’Brien–Fleming boundary for effect, did not reach the required sample size (2007 patients for EFS and 3191 patients for OS, Supplemental Figs. 15 and 17). These TSAs suggest that, although the pooled effect is statistically significant, with regard to sample size, the result is not definitive to reach 90% study power, and future studies are necessary to be conclusive.
Conversely, when exploring the association between SUV1 and survival outcomes in pediatric patients, the cumulative z-curve lies in the zone with no statistical significance and not reach the required sample size (1475 patients for EFS and 1695 patients for OS, Supplemental Figs. 16 and 18). This implies that the sample size of the meta-analysis was too small, and it is therefore impossible to infer where the cumulative z-line will lie in future trials.
Discussion
Key findings
Our principal finding suggests that high SUV1 (moderate evidence), SUV2 (very low evidence), MTV1 (moderate evidence) and TLG1 (very low evidence) values are strongly associated with unfavorable EFS and OS in adult patients with STS (all HRs ≥ 2). According to the proposed prognostic factor categories of Hayes et al., a HR exceeding 2 might be regarded as a strong prognostic factor [59]. However, very low-level evidence suggests that no [18F]FDG PET metabolic parameter is associated with survival outcomes in pediatric patients with RMS. The SUV ratio parameter demonstrated contradictory results—it was associated with EFS in adult patients, yet showed no correlation with OS.
The meta-regression analysis revealed that patient age is a significant modifier of the association between SUV1 and survival outcomes, thus emphasizing the role of patient age in the predictive value of [18F]FDG PET metabolic parameters.
The TSA analysis indicated that further research is necessary for definitive conclusions, especially in the pediatric patient population.
Relationship with previous studies
The results of our systematic review and meta-analysis are largely consistent with previous meta-analyses highlighting the prognostic potential of various [18F]FDG PET metabolic parameters in oncological settings. Specifically, meta-analyses have indicated the utility of SUV, MTV, and TLG parameters in predicting survival outcomes in patients with STS [17,18,19].
In particular, our findings corroborate previous research suggesting that higher pre- and posttreatment SUV values can predict poor survival outcomes. This is consistent with prior studies indicating that higher SUV values, reflecting high metabolic activity of the tumor and the proliferation rate of tumor cells, are associated with aggressive tumor behavior and poorer patient outcomes [60, 61]. In the systematic review by Lim et al. (2019), it was also demonstrated that a reduction in SUVmax correlates with improved recurrence-free survival in patients with STS. Furthermore, they found a strong correlation between SUV and tumor grade, with the majority of intermediate/high-grade STS exhibiting significantly higher SUVmax values [16]. Similar to the study by Li et al., we found no significant relationship between SUV ratio and OS [17]. While the SUV ratio demonstrated a significant correlation with EFS, especially in adult patients, the lack of a significant association with OS might be attributed to high clinical and statistical heterogeneity of included studies.
Similarly, our results align with previous research demonstrating that higher MTV and TLG values are associated with poorer survival outcomes. MTV refers to the volume of the lesion that exhibits metabolic activity, while TLG represents the product of the average SUV of the lesion and the MTV. These parameters provide volumetric and functional information about tumor metabolic activity and can theoretically more accurately reflect the actual tumor burden [62], and their association with survival outcomes has been reported in numerous cancers, including sarcomas [17,18,19, 63,64,65]. It’s notable that the MTV and TLG data used in this meta-analysis was obtained from pre-chemotherapy [18F]FDG PET imaging. Currently, there is no evidence regarding the prognostic value of MTV and TLG derived from post-chemotherapy imaging in patients with STS.
However, we observed that all associations of [18F]FDG PET metabolic parameters with survival outcomes were generally stronger in adult studies compared to pediatric ones, which is an aspect not examined in previous studies.
Significance of study findings
Our findings suggest that high SUV1, SUV2, and pretreatment MTV and TLG values can serve as predictors of EFS and OS, highlighting their potential as prognostic markers in patients with STS. Thus, it might be beneficial for physicians to adopt a more stringent follow-up regimen with reduced intervals for patients exhibiting high SUV1, MTV1 or TLG1 values. Furthermore, low SUV2 values may also suggest well chemotherapy response.
In our study, pretreatment MTV and TLG parameters showed higher HR values than SUV. The predictive advantage of MTV and TLG over SUV may stem from their ability to better reflect the tumor’s overall metabolic burden, which is associated with tumor aggressiveness and patient prognosis. These parameters consider the metabolic heterogeneity within the entire tumor, rather than a single point, which can often lead to a more accurate prediction of treatment outcomes.
It should be noted that the strength of associations between PET metabolic parameters and survival outcomes varied between adult and pediatric populations. Moreover, the meta-regression analysis revealed patient age as a significant modifier of the association between SUV1 and survival outcomes, underscoring the importance of considering age-specific factors in prognostic assessments. The prognosis impact of [18F]FDG uptake might be different in adult or pediatric patients as none of the previous meta-analyses were realized in a strictly pediatric population [66]. In the literature, the prognostic relevance of patient age remains controversial, older age seems to be associated with a worse outcome in both STS [67], osteosarcoma [68] and Ewing’s sarcoma [69]. Additionally, our research indicated that younger patients tend to have tumors of a higher histological grade. This observation leads us to speculate that the contrasting impacts of SUVs on prognostic outcomes between pediatric and adult populations, as documented in our study, could be attributed to these underlying variations in tumor biology. These biological differences could lead to variable responses to systemic cytotoxic therapy across age groups.
It is crucial to emphasize that our conclusions regarding the lack of impact of [18F]FDG PET parameters on prognosis in the pediatric population were based solely on patients with rhabdomyosarcoma. Unlike "adult-type" sarcomas, rhabdomyosarcoma is characterized by high sensitivity to chemotherapy. Moreover, pediatric patients typically undergo more aggressive treatment protocols compared to adults due to their better overall health and ability to tolerate intensive therapies, which can affect the metabolic activity of the tumor and potentially the utility of [18F]FDG PET parameters.
This systematic review and meta-analysis also provide an overview of the heterogeneity present in current studies with regards to methodological aspects, such as [18F]FDG PET scanning protocols and cut-off value determination methods. These findings underscore the need for standardized protocols and analytical methods to further enhance the reliability and reproducibility of research in this field.
Strengths and limitations
To our knowledge, this is the largest meta-analysis designed to systematically explore the relationships between [18F]FDG PET parameters and survival outcomes in patients with STS. Unlike some previous studies, we avoided combining different sarcoma types. Bone sarcomas, STS and Ewing’s sarcomas are heterogeneous groups, each possessing unique histological subtypes, molecular profiles, and clinical behaviors that can influence [18F]FDG uptake patterns. For instance, some soft-tissue sarcomas (STS) may exhibit higher metabolic rates, leading to increased [18F]FDG uptake, compared to certain bone sarcomas [15, 70, 71]. Combining these groups can consequently mask the distinct correlations between [18F]FDG PET parameters and survival outcomes. In studies that included patients with various types of sarcomas, including bone sarcomas and Ewing’s sarcoma, we exclusively extracted data pertaining to patients STS.
Notably, our study is the first to investigate and highlight the differences in the prognostic value of [18F]FDG PET metabolic parameters between adult and pediatric patients with STS. We found a significant impact of age on the association between SUV1 and survival outcomes.
We performed an extensive subgroup analysis including multivariable data analysis based on Cox proportional hazards model, that reduces bias from some major confounding variables. Furthermore, we executed an additional analysis in studies with low-moderate risk of bias, complemented by meta-regression and trial sequential analysis.
In addition, some limitations of this review must be acknowledged. One of the main limitations is the high level of heterogeneity observed among the included studies. This heterogeneity could stem from factors such as variations in study design, scanning protocols, methods for determining cut-off values, and patient demographics, which could affect the findings and their interpretation. On the other hand, the robustness of the results, despite the heterogeneity of the studies, may indicate high transitivity of the results and high quality of evidence. The included studies employed various segmentation methods to derive MTV for survival prediction, potentially leading to diverse MTV estimations, and consequently, impacting the TLG values [72].
Second, considering that 14 out of the 31 studies included in our meta-analysis represented mixed cohorts of pediatric and adult patients, we opted for a cut-off point of 75% children to categorize a study as ‘pediatric’. This could, however, have introduced a potential skewness in our results.
Third, although our meta-analysis exclusively focused on STS, it incorporates diverse STS types, including RMS, synovial sarcoma, angiosarcoma, liposarcoma, leiomyosarcoma, etc. This could also have affected the results, as different STS variants depending on histologic type and histological grade may exhibit varying levels of [18F]FDG accumulation [70, 73]. Significant variability precluded a subgroup analysis for different STS subtypes; however, it should be noted that all studies classified as ‘pediatric’ were solely represented by patients with RMS.
Fourth, the presence of publication bias and small-study effects for some analyses, as revealed by Egger’s test and funnel plot analysis, suggest that those results should be interpreted with caution.
Fifth, another potential source of bias in our study may stem from our methods of HR extraction. In cases where HRs were explicitly provided, we incorporated them directly. However, when HRs were not stated, we derived them either from the outcome data given in the articles or extrapolated from survival curves using univariate analysis. Therefore, this may have potentially introduced bias into meta-analysis.
Lastly, the overall risk of bias in the included studies was either ‘high’ or of ‘some concerns’ for the majority of the trials. Most common sources of bias were the lack of matching for confounding variables, inconsistent follow-up, and variation in co-interventions among the studies. These factors may have affected the reported associations and thus, the interpretations drawn from our meta-analysis.
Future studies and prospects
Looking ahead, future research can address the limitations observed in meta-analysis. Investigating the prognostic significance of post-chemotherapy MTV and TLG, as well as examining the changes in these parameters from pre- to post-chemotherapy in the context of predicting chemotherapy response, could provide intriguing prospects for future studies. To assess the impact of baseline and post-therapy PET/CT parameters on survival rates, additional prospective clinical studies with clearly defined time points are needed for evaluating PET/CT parameters in patients with various biological types of rhabdomyosarcoma (fusion-positive and fusion-negative). Special interest may be in organizing and conducting similar studies in children and adolescents with “adult-type” soft-tissue sarcomas, which, in terms of their biology and sensitivity to chemotherapy, are much closer to similar tumors in adults compared to rhabdomyosarcoma. Results of TSA analysis suggests that there is a need for prospective, multicenter studies with a more uniform methodological design. The protocols for [18F]FDG PET scanning, segmentation methods and the methods to determine cut-off values should be standardized across these studies to ensure consistency and comparability of results. This can contribute to a more robust and generalizable evidence base regarding the prognostic value of PET parameters in patients with STS.
Conclusion
In conclusion, our systematic review and meta-analysis provide evidence that [18F]FDG PET parameters of SUV1, SUV2, MTV1, and TLG1, hold significant prognostic value for event-free survival and overall survival in adult patients with STS. Notably, we found that the association of these parameters with survival outcomes was non-significant in pediatric patients, underscoring the necessity of age-specific considerations in future research focused on investigating [18F]FDG PET prognostic parameters and their clinical application for patients with STS. Future well-designed prospective multicenter studies with uniform methodology are needed to validate our findings and further explore the value of clinical use of [18F]FDG PET imaging in improving outcomes of patients with STS.
Availability of data and materials
The authors declare that all data supporting the findings of this study are available within the article.
Abbreviations
- [18F]FDG:
-
[18F]fluoro‑2‑deoxy‑2‑d‑glucose
- CI:
-
Confidence interval
- EFS:
-
Event-free survival
- FNCLCC:
-
Fédération Nationale des Centres de Lutte Contre Le Cancer Sarcoma Group
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- M:
-
Multicenter
- Me:
-
Median
- MTV:
-
Metabolic tumor volume
- NA:
-
Not applicable
- NAC:
-
Neoadjuvant chemotherapy
- NR:
-
Not reported
- OS:
-
Overall survival
- PET:
-
Positron emission tomography
- Pro:
-
Prospective
- Prov:
-
Provided
- REML:
-
REstricted Maximum–Likelihood
- Retro:
-
Retrospective
- RMS:
-
Rhabdomyosarcoma
- ROC:
-
Receiver operating characteristic curve
- S:
-
Single center
- SD:
-
Standard deviation
- STS:
-
Soft-tissue sarcoma
- SUV:
-
Standardized uptake value
- TLG:
-
Total lesion glycolysis
- TSA:
-
Trial sequential analysis
References
Seldon C, Shrivastava G, Al-Awady A et al (2021) Variation in management of extremity soft-tissue sarcoma in younger vs older adults. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2021.20951
Ferrari A, Brennan B, Casanova M et al (2022) Pediatric non-rhabdomyosarcoma soft tissue sarcomas: standard of care and treatment recommendations from the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG). Cancer Manag Res 14:2885–2902. https://doi.org/10.2147/CMAR.S368381
Kunisada T, Nakata E, Fujiwara T et al (2023) Soft-tissue sarcoma in adolescents and young adults. Int J Clin Oncol 28:1–11. https://doi.org/10.1007/s10147-022-02119-7
Burningham Z, Hashibe M, Spector L, Schiffman JD (2012) The epidemiology of sarcoma. Clin Sarcoma Res 2:1–16. https://doi.org/10.1186/2045-3329-2-14
Ray-Coquard I, Serre D, Reichardt P et al (2018) Options for treating different soft tissue sarcoma subtypes. Futur Oncol 14:25–49. https://doi.org/10.2217/fon-2018-0076
Grünewald TG, Alonso M, Avnet S et al (2020) Sarcoma treatment in the era of molecular medicine. EMBO Mol Med. https://doi.org/10.15252/emmm.201911131
Ducimetière F, Lurkin A, Ranchère-Vince D et al (2011) Incidence of sarcoma histotypes and molecular subtypes in a prospective epidemiological study with central pathology review and molecular testing. PLoS ONE. https://doi.org/10.1371/journal.pone.0020294
Jacobs AJ, Michels R, Stein J, Levin AS (2015) Improvement in overall survival from extremity soft tissue sarcoma over twenty years. Sarcoma. https://doi.org/10.1155/2015/279601
Zagars GK, Ballo MT, Pisters PWT et al (2003) Prognostic factors for patients with localized soft-tissue sarcoma treated with conservation surgery and radiation therapy: an analysis of 1225 patients. Cancer 97:2530–2543. https://doi.org/10.1002/cncr.11365
Toulmonde M, Bonvalot S, Méeus P et al (2014) Retroperitoneal sarcomas: Patterns of care at diagnosis, prognostic factors and focus on main histological subtypes: a multicenter analysis of the French Sarcoma Group. Ann Oncol 25:735–742. https://doi.org/10.1093/annonc/mdt577
Uslu L, Donig J, Link M et al (2015) Value of18F-FDG PET and PET/CT for evaluation of pediatric malignancies. J Nucl Med 56:274–286. https://doi.org/10.2967/jnumed.114.146290
El-Kholy E, El Nadi E, Hafez H et al (2019) Added predictive value of 18F-FDG PET/CT for pediatric rhabdomyosarcoma. Nucl Med Commun 40:898–904. https://doi.org/10.1097/MNM.0000000000001040
Casey DL, Wexler LH, Fox JJ et al (2014) Predicting outcome in patients with rhabdomyosarcoma: role of [18F]fluorodeoxyglucose positron emission tomography. Int J Radiat Oncol Biol Phys 90:1136–1142. https://doi.org/10.1016/j.ijrobp.2014.08.005
Park JY, Lee JW, Lee HJ et al (2017) Prognostic significance of preoperative 18F-FDG PET/CT in uterine leiomyosarcoma. J Gynecol Oncol 28:28. https://doi.org/10.3802/jgo.2017.28.e28
Hack RI, Becker AS, Bode-Lesniewska B et al (2021) When suv matters: Fdg pet/ct at baseline correlates with survival in soft tissue and ewing sarcoma. Life. https://doi.org/10.3390/life11090869
Lim HJ, Johnny Ong CA, Tan JWS, Ching Teo MC (2019) Utility of positron emission tomography/computed tomography (PET/CT) imaging in the evaluation of sarcomas: a systematic review. Crit Rev Oncol Hematol 143:1–13. https://doi.org/10.1016/j.critrevonc.2019.07.002
Li YJ, Dai YL, Cheng YS et al (2016) Positron emission tomography (18)F-fluorodeoxyglucose uptake and prognosis in patients with bone and soft tissue sarcoma: a meta-analysis. Eur J Surg Oncol 42:1103–1114. https://doi.org/10.1016/j.ejso.2016.04.056
Kubo T, Furuta T, Johan MP, Ochi M (2016) Prognostic significance of 18F-FDG PET at diagnosis in patients with soft tissue sarcoma and bone sarcoma; systematic review and meta-analysis. Eur J Cancer 58:104–111. https://doi.org/10.1016/j.ejca.2016.02.007
Chen L, Wu X, Ma X et al (2017) Prognostic value of 18F-FDG PET-CT-based functional parameters in patients with soft tissue sarcoma a meta-analysis. Med (United States). https://doi.org/10.1097/MD.0000000000005913
Okazumi S, Dimitrakopoulou-Strauss A, Schwarzbach MHM, Strauss LG (2009) Quantitative, dynamic 18F-FDG-PET for the evaluation of soft tissue sarcomas: relation to differential diagnosis, tumor grading and prediction of prognosis. Hell J Nucl Med 12:223–228
Lyra V, Chatziioannou S, Kallergi M (2022) Clinical perspectives for18 F-FDG PET imaging in pediatric oncology: μetabolic tumor volume and radiomics. Metabolites. https://doi.org/10.3390/metabo12030217
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. https://doi.org/10.1371/journal.pmed.1000100
Khoury JD, Coffin CM, Spunt SL et al (2010) Grading of nonrhabdomyosarcoma soft tissue sarcoma in children and adolescents: a comparison of parameters used for the Fédération Nationale des Centers de Lutte Contre le Cancer and Pediatric Oncology Group systems. Cancer 116:2266–2274. https://doi.org/10.1002/cncr.24929
Tierney JF, Stewart LA, Ghersi D et al (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16. https://doi.org/10.1186/1745-6215-8-16
Higgins JPT, Thomas J, Chandler J et al (2019) Cochrane handbook for systematic reviews of interventions. Cochrane Handb Syst Rev Interv. https://doi.org/10.1002/9781119536604
Harbord RM, Higgins JPT (2008) Meta-regression in Stata. Stata J 8:493–519. https://doi.org/10.1177/1536867x0800800403
De Cassai A, Tassone M, Geraldini F et al (2021) Explanation of trial sequential analysis: using a post-hoc analysis of meta-analyses published in Korean Journal of Anesthesiology. Korean J Anesthesiol 74:383–393. https://doi.org/10.4097/KJA.21218
CLARITY-group. Tool to Assess Risk of Bias in Case Control Studies Hamilton, Ontario: McMaster University. https://www.evidencepartners.com/wp-content/uploads/2021/03/Tool-to-Assess-Risk-of-Bias-in-Case-Control-Studies-DistillerSR.pdf. Accessed 14 Jul 2023
McGuinness LA, Higgins JPT (2021) Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 12:55–61. https://doi.org/10.1002/jrsm.1411
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Foroutan F, Guyatt G, Zuk V et al (2020) GRADE Guidelines 28: use of GRADE for the assessment of evidence about prognostic factors: rating certainty in identification of groups of patients with different absolute risks. J Clin Epidemiol 121:62–70. https://doi.org/10.1016/j.jclinepi.2019.12.023
FDA (2019) Pediatric Medical Devices | FDA. https://www.fda.gov/medical-devices/products-and-medical-procedures/pediatric-medical-devices. Accessed 14 Jul 2023
Andersen KF, Fuglo HM, Rasmussen SH et al (2015) Semi-quantitative calculations of primary tumor metabolic activity using F-18 FDG PET/CT as a predictor of survival in 92 patients with high-grade bone or soft tissue sarcoma. Med (United States). https://doi.org/10.1097/MD.0000000000001142
Andersen KF, Fuglo HM, Rasmussen SH et al (2015) Volume-Based F-18 FDG PET/CT imaging markers provide supplemental prognostic information to histologic grading in patients with high-grade bone or soft tissue sarcoma. Med (United States). https://doi.org/10.1097/MD.0000000000002319
Andreou D, Boldt H, Pink D et al (2014) Prognostic relevance of 18F-FDG PET uptake in patients with locally advanced, extremity soft tissue sarcomas undergoing neoadjuvant isolated limb perfusion with TNF-α and melphalan. Eur J Nucl Med Mol Imaging 41:1076–1083. https://doi.org/10.1007/s00259-013-2680-8
Annovazzi A, Ferraresi V, Covello R et al (2023) Prognostic value of pre-treatment [18F]FDG PET/CT texture analysis in undifferentiated soft-tissue sarcoma. J Clin Med. https://doi.org/10.3390/jcm12010279
Chang KJ, Lim I, Park JY et al (2010) The role of 18F-FDG PET/CT as a prognostic factor in patients with synovial sarcoma. Nucl Med Mol Imaging 49:33–41. https://doi.org/10.1007/s13139-014-0301-5
Chen D, Tang M, Lv S et al (2022) Prognostic usefulness of clinical features and pretreatment 18F-FDG PET/CT metabolic parameters in patients with angiosarcoma. Quant Imaging Med Surg 12:2792–2804. https://doi.org/10.21037/qims-21-563
Cheriyalinkal Parambil B, Shah S, Prasad M et al (2023) Can 18F-FDG-positron emission tomography be a prognostic tool in children with rhabdomyosarcoma treated with definitive radiotherapy? J Pediatr Hematol Oncol 45:E363–E369. https://doi.org/10.1097/MPH.0000000000002565
Choi ES, Ha SG, Kim HS et al (2013) Total lesion glycolysis by 18F-FDG PET/CT is a reliable predictor of prognosis in soft-tissue sarcoma. Eur J Nucl Med Mol Imaging 40:1836–1842. https://doi.org/10.1007/s00259-013-2511-y
Dharmarajan KV, Wexler LH, Gavane S et al (2012) Positron emission tomography (PET) evaluation after initial chemotherapy and radiation therapy predicts local control in rhabdomyosarcoma. Int J Radiat Oncol Biol Phys 84:996–1002. https://doi.org/10.1016/j.ijrobp.2012.01.077
Fayolle H, Jehanno N, Lauwers-Cances V et al (2022) PET metabolic tumor volume as a new prognostic factor in childhood rhabdomyosarcoma. PLoS ONE. https://doi.org/10.1371/journal.pone.0261565
Fendler WP, Lehmann M, Todica A et al (2015) PET response criteria in solid tumors predicts progression-free survival and time to local or distant progression after chemotherapy with regional hyperthermia for soft-tissue sarcoma. J Nucl Med 56:530–537. https://doi.org/10.2967/jnumed.114.152462
Ha SC, Oh JS, Roh JL et al (2017) Pretreatment tumor SUVmax predicts disease-specific and overall survival in patients with head and neck soft tissue sarcoma. Eur J Nucl Med Mol Imaging 44:33–40. https://doi.org/10.1007/s00259-016-3456-8
Harrison DJ, Chi YY, Tian J et al (2021) Metabolic response as assessed by 18F-fluorodeoxyglucose positron emission tomography-computed tomography does not predict outcome in patients with intermediate- or high-risk rhabdomyosarcoma: a report from the Children’s Oncology Group Soft Tissue Sarcom. Cancer Med 10:857–866. https://doi.org/10.1002/cam4.3667
Herrmann K, Benz MR, Czernin J et al (2012) 18F-FDG-PET/CT imaging as an early survival predictor in patients with primary high-grade soft tissue sarcomas undergoing neoadjuvant therapy. Clin Cancer Res 18:2024–2031. https://doi.org/10.1158/1078-0432.CCR-11-2139
Hong SP, Lee SE, La CY et al (2014) Prognostic value of 18F-FDG PET/CT in patients with soft tissue sarcoma: comparisons between metabolic parameters. Skeletal Radiol 43:641–648. https://doi.org/10.1007/s00256-014-1832-7
Jo SJ, Kim KD, Lim SH et al (2022) The role of preoperative 18F-fluorodeoxyglucose positron emission tomography/computed tomography in retroperitoneal sarcoma. Front Oncol. https://doi.org/10.3389/fonc.2022.868823
Kalisvaart GM, Grootjans W, Bovée JVMG et al (2021) Prognostic value of quantitative [18 f]fdg-pet features in patients with metastases from soft tissue sarcoma. Diagnostics. https://doi.org/10.3390/diagnostics11122271
Kato A, Nakamoto Y, Ishimori T et al (2020) Prognostic value of quantitative parameters of 18F-FDG PET/CT for patients with angiosarcoma. Am J Roentgenol 214:649–6549. https://doi.org/10.2214/AJR.19.21635
Kitao T, Shiga T, Hirata K et al (2019) Volume-based parameters on FDG PET may predict the proliferative potential of soft-tissue sarcomas. Ann Nucl Med 33:22–31. https://doi.org/10.1007/s12149-018-1298-0
Lisle JW, Eary JF, O’Sullivan J, Conrad EU (2009) Risk assessment based on FDG-PET imaging in patients with synovial sarcoma. Clin Orthop Relat Res 467:1605–1611. https://doi.org/10.1007/s11999-008-0647-z
Rhu J, Hyun SH, Lee KH et al (2019) Maximum standardized uptake value on 18 F-fluorodeoxyglucose positron emission tomography/computed tomography improves outcome prediction in retroperitoneal liposarcoma. Sci Rep 9:1–10. https://doi.org/10.1038/s41598-019-43215-5
Sambri A, Bianchi G, Longhi A et al (2019) The role of F-FDG PET/CT in soft tissue sarcoma. Nucl Med Commun 40:626–631. https://doi.org/10.1097/MNM.0000000000001002
Tateishi U, Kawai A, Chuman H et al (2011) PET/CT allows stratification of responders to neoadjuvant chemotherapy for high-grade sarcoma: a prospective study. Clin Nucl Med 36:526–532. https://doi.org/10.1097/RLU.0b013e3182175856
Umemura H, Yamasaki O, Kaji T et al (2017) Prognostic value of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in patients with cutaneous angiosarcoma: a retrospective study of 18 cases. J Dermatol 44:1046–1049. https://doi.org/10.1111/1346-8138.13839
Wakamatsu T, Imura Y, Tamiya H et al (2021) 18F-fluorodeoxyglucose positron emission tomography is useful in the evaluation of prognosis in retroperitoneal sarcoma. Cancers (Basel). https://doi.org/10.3390/cancers13184611
Yamamoto M, Tsujikawa T, Yamada S et al (2017) 18F-FDG/18F-FES standardized uptake value ratio determined using PET predicts prognosis in uterine sarcoma. Oncotarget 8:22581–22589. https://doi.org/10.18632/oncotarget.15127
Hayes DF, Isaacs C, Stearns V (2001) Prognostic factors in breast cancer: current and new predictors of metastasis. J Mammary Gland Biol Neoplasia 6:375–392. https://doi.org/10.1023/A:1014778713034
Vesselle H, Turcotte E, Wiens L et al (2004) Relationship between non-small cell lung cancer fluorodeoxyglucose uptake at positron emission tomography and surgical stage with relevance to patient prognosis. Clin Cancer Res 10:4709–4716. https://doi.org/10.1158/1078-0432.CCR-03-0773
Oprea-Lager DE, Kramer G, Van De Ven PM et al (2016) Repeatability of quantitative 18F-fluoromethylcholine PET/CT studies in prostate cancer. J Nucl Med 57:721–727. https://doi.org/10.2967/jnumed.115.167692
Song H, Jiao Y, Wei W et al (2019) Can pretreatment 18F-FDG PET tumor texture features predict the outcomes of osteosarcoma treated by neoadjuvant chemotherapy? Eur Radiol 29:3945–3954. https://doi.org/10.1007/s00330-019-06074-2
Rijo-Cedeño J, Mucientes J, Álvarez O et al (2020) Metabolic tumor volume and total lesion glycolysis as prognostic factors in head and neck cancer: systematic review and meta-analysis. Head Neck 42:3744–3754. https://doi.org/10.1002/hed.26461
Wen W, Piao Y, Xu D, Li X (2021) Prognostic value of MTV and TLG of 18F-FDG PET in patients with stage I and II non-small-cell lung cancer: a meta-analysis. Contrast Media Mol Imaging. https://doi.org/10.1155/2021/7528971
Pak K, Cheon GJ, Nam HY et al (2014) Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer: a systematic review and meta-analysis. J Nucl Med 55:884–890. https://doi.org/10.2967/jnumed.113.133801
Bailly C, Leforestier R, Campion L et al (2017) Prognostic value of FDG-PET indices for the assessment of histological response to neoadjuvant chemotherapy and outcome in pediatric patients with Ewing sarcoma and osteosarcoma. PLoS ONE 12:e0183841. https://doi.org/10.1371/journal.pone.0183841
Pan M, Merchant M (2018) Risk factors including age, stage and anatomic location that impact the outcomes of patients with synovial sarcoma. Med Sci. https://doi.org/10.3390/MEDSCI6010021
Janeway KA, Barkauskas DA, Krailo MD et al (2012) Outcome for adolescent and young adult patients with osteosarcoma: a report from the Children’s Oncology Group. Cancer 118:4597–4605. https://doi.org/10.1002/CNCR.27414
Cotterill SJ, Ahrens S, Paulussen M et al (2000) Prognostic factors in Ewing’s tumor of bone: analysis of 975 patients from the European Intergroup Cooperative Ewing’s Sarcoma Study Group. J Clin Oncol 18:3108–3114. https://doi.org/10.1200/JCO.2000.18.17.3108
Macpherson RE, Pratap S, Tyrrell H et al (2018) Retrospective audit of 957 consecutive 18F-FDG PET–CT scans compared to CT and MRI in 493 patients with different histological subtypes of bone and soft tissue sarcoma. Clin Sarcoma Res. https://doi.org/10.1186/s13569-018-0095-9
Li CP, Liu DN, Zhou NN et al (2021) Prediction of histologic subtype and FNCLCC grade by SUVmax measured on 18F-FDG PET/CT in patients with retroperitoneal liposarcoma. Contrast Media Mol Imaging. https://doi.org/10.1155/2021/7191363
Im HJ, Bradshaw T, Solaiyappan M, Cho SY (2018) Current methods to define metabolic tumor volume in positron emission tomography: which one is better? Nucl Med Mol Imaging 52:5. https://doi.org/10.1007/S13139-017-0493-6
Reyes Marlés RH, Navarro Fernández JL, Puertas García-Sandoval JP et al (2021) Clinical value of baseline 18F-FDG PET/CT in soft tissue sarcomas. Eur J Hybrid Imaging. https://doi.org/10.1186/S41824-021-00110-5
Acknowledgements
None
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
MY, YL contributed to the design and implementation of the research. MY, LB, ER preformed the analysis of the results. MY, LB, ER, DK, YL wrote of the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yadgarov, M.Y., Berikashvili, L.B., Rakova, E.S. et al. Prognostic significance of [18F]FDG PET metabolic parameters in adults and children with soft-tissue sarcoma: a meta-analysis. Clin Transl Imaging (2024). https://doi.org/10.1007/s40336-024-00620-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40336-024-00620-9