Abstract
Background
Meningiomas, which are the most common of CNS tumours in adults, show a high expression of the somatostatin receptor subtype 2 (SSR). Visualization of these receptors with specific PET ligands augments contrast-enhanced MRI and CT of the brain in resolving several clinical issues related to differential diagnosis, evaluation of meningioma extent, and therapy planning or follow-up. Moreover, SSR-directed radioligands labeled with beta-emitters serve for radiopeptide therapy (RPT) in patients with recurrent or refractory meningioma. In the light of recent developments in radiochemistry, neuropathology/molecular genetics, and emerging systemic treatments, we present our perspective on future directions of SSR-directed imaging and therapy in meningioma.
Methods
We conducted a search in the PubMed literature database until June 2019 using the terms “meningioma”, “PET”, “somatostatin receptor”, “SS(T)R”, “DOTATATE”, “DOTATOC”, “radiopeptide therapy”, “imaging”, “therapy”, “classification” alone and in combination, compiled with relevant literature from the authors’ own files.
Results/conclusion
Our review identifies important emerging applications of SSR-directed imaging and therapy in patients with meningioma. We summarize the state of development novel SSR-directed radio-ligands, meningioma classifications and systemic treatment options.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Current status of SSR-directed imaging and therapy
Meningiomas are the most common category of tumours of the central nervous system in adults. Clinical work-up of suspected meningiomas is vulnerable to several diagnostic uncertainties, which are not easily resolved by standard morphological imaging methods such as contrast-enhanced MRI and CT [1]. Consequently, molecular imaging by modalities such as positron emission tomography (PET) has an emerging role for diagnosis of meningiomas, by exploiting their characteristically high expression of the somatostatin receptor subtype 2 (SSR). PET imaging with selective SSR ligands can visualize and quantify this expression in tumours against a low background signal in healthy brain structures. This pharmacologically selective PET imaging of SSR can contribute importantly to the clinical workup. For example, SSR PET has higher sensitivity for meningioma detection at initial diagnosis, revealing larger numbers of lesions than are evident to structural imaging methods [2, 3]. Although current SSR PET methods are unfit to distinguish between the different WHO grades of meningioma, the intensity of lesional uptake does correlate with the tumoural growth rate [4]. Moreover, PET can contribute to the differentiation of leptomeningeal metastases from meningioma [5]. These features also enable better tumour delineation, even at diagnostically difficult locations, such as the optic nerve sheath or the skull base [6,7,8], where diagnosis is particularly challenging on standard imaging such as MRI. Particularly, PET is significantly superior to contrast enhanced MRI for evaluating the extent of osseous involvement of meningiomas [9], a feature of PET that can inform the planning of subsequent surgery or radiotherapy [8, 10,11,12]. Post therapy SSR PET follow-up examinations are useful for the differentiation of recurrent/residual tumour tissue and post-therapeutic scar tissue [13].
Besides these diagnostic uses of SSR-directed PET radioligands, labelling with high energy beta-emitters (predominantly [177Lu] and [90Y]) gives effective agents for targeted radiopeptide therapy (RPT) in patients with recurrent or refractory meningioma. RPT shows a good risk profile and clinical response rates in previously treated meningioma patients, often evoking stabilization or deceleration of tumour growth [14,15,16,17,18,19,20,21]. However, international harmonization of treatment regimens and results from controlled, randomized trials are needed to further foster the use of RPT in meningioma. We have recently presented a dedicated review article on the current status of SSR-directed imaging and therapy in meningioma [22], which we now augment with an account of future prospects for SSR-directed imaging and therapy in the light of current developments in radiochemistry, neuropathology/molecular genetics, and novel systemic treatments.
Novel radioligands
Currently, there are several promising radioligands targeting SSR, including not only somatostatin structural analogs (with agonist action), but also SSR antagonists, which might be suitable for improved diagnostic or theranostic approaches in patients with meningioma. By way of example, we note some promising agents (see also [23] for an detailed overview of novel SSR-ligands with emphasis on neuroendocrine tumors (NET)):
[68Ga]-OPS202/[177Lu]-OPS201 (a.k.a [68Ga]-DOTA-JR-11/[177Lu]-DOTA-JR11) is a novel theranostic pair of SSR-antagonists; PET studies with [68Ga]-OPS202 ([68Ga]-DOTA-JR-11) show significantly higher uptake and distinctly improved detection rate of tumour lesions in patients with NET compared to [68Ga]-DOTATOC [24]. Moreover, evaluation of the therapeutic twin [177Lu]-OPS201 ([177Lu]-DOTA-JR11) in murine NET models gave up to 4.4-fold higher tumour dosimetry per injected activity (1.8 ± 0.7 Gy/MBq vs. [177Lu]-DOTATATE, 0.36 ± 0.07 Gy/MBq) [25, 26], without increased exposure to healthy organs. Ongoing studies evaluating this theranostic SSR-ligand pair have given promising preliminary data with regard to the efficacy and safety in human patients with NET [27, 28].
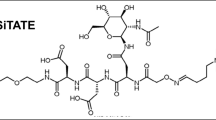
[177Lu]-DOTA-EB-TATE is a structural modification of the commonly applied radioligand [177Lu]-DOTATATE incorporating a special Evans blue derivatization, which imparts higher efficacy by favouring it binding to serum albumin. This interferes with renal clearance, thus resulting in a longer half-life in the blood, and consequently higher intra-tumoural retention in animal models [29]. In humans, [177Lu]-DOTA-EB-TATE had nearly eightfold higher delivered doses to the tumours compared to conventional [177Lu]-DOTATATE [30]. In a comparative therapy setting, a group of (n = 8) NET patients received a single dose of up to 0.7 GBq of [177Lu]-DOTA-EB-TATE only. Their response rates to this treatment as assessed with [68Ga]-DOTATATE PET were comparable to those achieved with [177Lu]-DOTATATE. However, the whole body radiation exposure with [177Lu]-DOTA-EB-TATE was only about a sixth of that obtained with [177Lu]-DOTATATE [31].
Besides the commonly applied therapeutic radioligands labeled with beta-emitters, there are also therapeutic approaches targeting the SSR-bearing tumors with alpha-emitting isotopes such as [213Bi] and [225Ac]. The novel radioligand [213Bi]-DOTATOC had significant tumoural response rates and a moderate side effect profile after intraarterial application in patients (n = 7) with predominantly liver metastases from NET. Radiopeptide therapy with this and other alpha-emitters might be of particular interest in patients previously treated with beta-emitting radioligands, who showed insufficient clinical response or even refractory disease [32]. Modifications with other labeling agents might further improve their efficacy and therapeutic effects [33]. Despite promising experience with NET, there are so far no reports of SSR-directed therapy with alpha-emitters in patients suffering from meningioma.
In sum, emerging SSR-directed radioligands show promising benefits compared to the currently applied, standard theranostic ligands for NET such as DOTATOC or DOTATATE. However, there is limited data about these novel radioligands in meningioma animal models or indeed in patients suffering from meningioma. Nonetheless, their well-documented imaging or therapeutic properties in animal models and humans suffering from NET bode well for the effectiveness of new SSR ligands in future studies of meningioma.
Novel meningioma classifications
In clinical routine, risk stratification of meningiomas takes into account the individual histology, clinical presentation, localization, and the individual extent of resection. However, prediction models are imperfect instruments for reliable prognostication of tumour behavior and the individual risk of tumour recurrence. Patients typically undergo MRI based follow-up to assess the status of individual residual tumours. Besides established clinical factors, there is increasing evidence that certain features of tumoral molecular biology and genetics might contribute to an individualized and “patient-tailored” approach in patients suffering from meningioma [34]. The relevant molecular genetic profiles comprise genomic alterations such as copy number alterations [35,36,37], but also extend to changes of the gene mutation signature, which drive meningiomagenesis and aggressive tumour behaviour. In brief, these mutations can be designated as neurofibromatosis type 2 (NF2) or non-NF2 based changes [34], in addition to numerous additional mutations of genes with varying diverging individual relevance such as tumour necrosis factor (TNF), receptor associated factor 7 (TRAF7), and the hedgehog signaling pathway (Hh) [38]. Besides specific gene mutations, the regulation of gene transcription through DNA-methylation is also increasingly implicated in meningioma classification, evaluation of tumour recurrence and prognostication, which is a matter extending beyond the current WHO classification, as it relies on histopathological criteria for meningioma classification [39]. For a more detailed overview see also [34].
PET examination of gliomas using radiolabelled amino acids such as [18F]fluoroethyltyrosine has already been evaluated in relation to different molecular genetic tumour classes, which delivers additive prognostic value along with molecular genetic information [40, 41]. It remains unknown whether this shall also hold for SSR-directed imaging in meningioma. Irrespective of any potential prognostic value of parameters such as tracer uptake intensity or volume in SSR-directed PET, patients identified as having an unfavourable molecular genetic profile and aggressive tumoural behaviour might profit from an optimized PET-based staging at initial diagnosis. Such an approach could help to exclude the presence of additional tumour sites, tumour remnants, or undetected osseous involvement.
In analogy to the recent glioma studies establishing the value of amino acid PET for the non-invasive prediction of molecular genetic parameters, future meningioma studies should test the potential value of SSR-directed PET imaging to identify high-risk patients with currently indolent course and absent symptoms, despite unfavourable molecular genetic features such as TERT-promoter methylation [42]. Importantly, novel classifications such as the DNA-methylation profile might also identify meningioma patients apt to enjoy the greatest benefit from radioligand therapy. This might include patients with a certain molecular genetic profile predicting a good response to RPT at an earlier disease stage. Conversely, molecular genetic analyses might eventually identify meningioma patients likely to benefit more from an experimental therapy other than RPT. Thus, we suppose that combining molecular genetic meningioma classification and molecular imaging/therapy may be a promising approach for additional tumour characterization, potentially contributing to individualized clinical management of meningioma patients.
Novel systemic treatments
Systemic treatment in meningioma may be beneficial in patients with recurrent or progressive disease after failure or unsatisfactory response to conventional treatment options such as radiotherapy and surgery. Unfortunately, systemic cytostatic treatments such as temozolomide and irinotecan show only limited benefits or palliative effects [43]. Systemic treatment with trabectedin, an antiproliferative agent derived from the mangrove tunicate, is finding some success in sarcoma patients [44]. This agent has also shown efficacy in meningioma studies conducted in vitro [45], and is currently being evaluated in a randomized multicenter trial of patients with recurrent meningioma WHO grade II/III (EORTC-1320-BTG). However, preliminary findings with trabectedin do not indicate clear superiority over current standards of care in human meningioma patients [46]. Moreover, there are numerous potential novel targets and treatments arising from the comprehensive understanding of the underlying molecular genetic changes involving signaling pathways (SMO, AKT1, and NF2) occurring in meningiomas (NCT02523014/A071401). For a more detailed overview, see also [43].
As is established for the treatment of numerous cancer entities, immunotherapy is also under investigation in patients suffering from meningioma. Current literature suggests a high expression of programmed death ligand 1 (PD-L1) in anaplastic meningioma WHO grade III [47, 48]. These observations inspired several clinical studies investigating the efficacy of checkpoint inhibitors such as nivolumab or pembrolizumab in atypical WHO grade II and anaplastic WHO grade III meningiomas (NCT03279692, NCT02648997).
In considering the effectiveness of novel drugs and treatments, one must take into account the question of “what constitutes activity of systemic therapy in […] meningioma?” [49]. The RANO Working group previously stated that “No standard criteria exist for assessing response and progression in clinical trials involving patients with meningioma, and there is no consensus on the optimal endpoints for trials currently under way.” [50]. Moreover, it is often rather technically difficult even to assess or estimate the ‘real morphological extension’ of meningiomas by MRI, particularly at inaccessible localizations, such as the skull base. Therefore, the correct evaluation of the size and extent of meningiomas as an endpoint in experimental therapies is even more challenging. Therefore, molecular imaging with PET is a promising instrument for assessment of treatment response, which is particularly important for the evaluation of novel systemic treatments.
With regard to the application of SSR-directed RPT in patients with meningioma, novel antineoplastic drugs such as those mentioned above might also show synergistic effects in combination with RPT. Pretreatment may prove to have radiosensitizing effects in addition to inherent antineoplastic properties, as is reported for capecitabine and temozolomide in patients with NET/paraganglioma [51, 52], or nutlin-3 and topotecan in patients with neuroblastoma [53]. In light of the emerging systemic treatment options mentioned above, there is scope for exploring potentially synergistic effects with SSR-directed RPT. i.e. a two-hit approach targeting vulnerable aspects of the meningiomas.
Summary
Extending beyond morphological imaging using MRI and CT, SSR-directed molecular PET imaging of meningiomas distinctly contributes to diagnostic uncertainties arising due to uncertainties in tumor boundaries and extent. Moreover, RPT using beta-emitting radioligands is a well-tolerated therapy option in patients with recurrent meningioma. Starting from the knowledge base established in NET investigations with ligands such as DOTATOC or DOTATATE, several new theranostic ligands with improved binding properties as well as therapeutic SSR ligands using alpha-emitters are under investigation. Augmentation of histological classification of meningiomas by molecular genetic classifications is proving effective for risk stratification and prognostication in clinical routine. Thus, SSR PET can bring additional diagnostic information in high-risk patients, and might contribute to the clinical prognostication. Due to the well-known inadequacy of structural imaging as an endpoint for meningioma therapy, SSR PET may be instrumental in the assessment of novel systemic treatments such as immune therapy. Promising initial results with RPT in patients with meningioma call attention to the need randomized controlled trials of this approach, either alone, in a theranostic setting, or in conjunction with potentially synergistic therapy options, especially keeping in mind the radiosensitizing effects of certain systemic treatments.
References
Galldiks N, Albert NL, Sommerauer M, Grosu AL, Ganswindt U, Law I et al (2017) PET imaging in patients with meningioma—report of the RANO/PET Group. Neuro-oncology 19(12):1576–1587
Afshar-Oromieh A, Giesel FL, Linhart HG, Haberkorn U, Haufe S, Combs SE et al (2012) Detection of cranial meningiomas: comparison of 68Ga-DOTATOC PET/CT and contrast-enhanced MRI. Eur J Nucl Med Mol Imaging 39(9):1409–1415
Henze M, Schuhmacher J, Hipp P, Kowalski J, Becker DW, Doll J et al (2001) PET imaging of somatostatin receptors using [68GA] DOTA-D-Phe1-Tyr3-octreotide: first results in patients with meningiomas. J Nucl Med 42(7):1053–1056
Sommerauer M, Burkhardt J-K, Frontzek K, Rushing E, Buck A, Krayenbuehl N et al (2016) 68Gallium-DOTATATE PET in meningioma: a reliable predictor of tumor growth rate? Neuro-oncology 18(7):1021–1027
Unterrainer M, Ruf V, Ilhan H, Vettermann FJ, Cyran CC, Niyazi M et al (2019) 68Ga-DOTATOC PET/CT differentiates meningioma from dural metastases. Clin Nucl Med 44(5):412–413
Al Feghali KA, Yeboa DN, Chasen B, Gule MK, Johnson JM, Chung C (2018) The use of 68Ga-DOTATATE PET/CT in the non-invasive diagnosis of optic nerve sheath meningioma: a case report. Front Oncol 8:454
Milker-Zabel S, Zabel-du Bois A, Henze M, Huber P, Schulz-Ertner D, Hoess A et al (2006) Improved target volume definition for fractionated stereotactic radiotherapy in patients with intracranial meningiomas by correlation of CT, MRI, and [68Ga]-DOTATOC-PET. Int J Radiat Oncol Biol Phys 65(1):222–227
Nyuyki F, Plotkin M, Graf R, Michel R, Steffen I, Denecke T et al (2010) Potential impact of 68Ga-DOTATOC PET/CT on stereotactic radiotherapy planning of meningiomas. Eur J Nucl Med Mol Imaging 37(2):310–318
Kunz WG, Jungblut LM, Kazmierczak PM, Vettermann FJ, Bollenbacher A, Tonn JC et al (2017) Improved detection of transosseous meningiomas using 68Ga-DOTATATE PET/CT compared with contrast-enhanced MRI. J Nucl Med 58(10):1580–1587
Gehler B, Paulsen F, Öksüz MÖ, Hauser T-K, Eschmann SM, Bares R et al (2009) [68Ga]-DOTATOC-PET/CT for meningioma IMRT treatment planning. Radiat Oncol 4(1):56
Graf R, Nyuyki F, Steffen IG, Michel R, Fahdt D, Wust P et al (2013) Contribution of 68Ga-DOTATOC PET/CT to target volume delineation of skull base meningiomas treated with stereotactic radiation therapy. Int J Radiat Oncol Biol Phys 85(1):68–73
Zollner B, Ganswindt U, Maihöfer C, Corradini S, Albert NL, Schichor C et al (2018) Recurrence pattern analysis after [68Ga]-DOTATATE-PET/CT-planned radiotherapy of high-grade meningiomas. Radiat Oncol 13(1):110
Galldiks N, Albert NL, Sommerauer M, Grosu AL, Ganswindt U, Law I et al (2017) PET imaging in patients with meningioma—report of the RANO/PET Group. Neuro-Oncology. 19(12):1576–1587
Bartolomei M, Bodei L, De Cicco C, Grana CM, Cremonesi M, Botteri E et al (2009) Peptide receptor radionuclide therapy with 90Y-DOTATOC in recurrent meningioma. Eur J Nucl Med Mol Imaging 36(9):1407
Kreissl MC, Hänscheid H, Löhr M, Verburg FA, Schiller M, Lassmann M et al (2012) Combination of peptide receptor radionuclide therapy with fractionated external beam radiotherapy for treatment of advanced symptomatic meningioma. Radiat Oncol 7(1):99
Marincek N, Radojewski P, Dumont RA, Brunner P, Müller-Brand J, Maecke HR et al (2015) Somatostatin receptor-targeted radiopeptide therapy with 90Y-DOTATOC and 177Lu-DOTATOC in progressive meningioma: long-term results of a phase II clinical trial. J Nucl Med 56(2):171–176
Sabet A, Ahmadzadehfar H, Herrlinger U, Wilinek W, Biersack H-J, Ezziddin S (2011) Successful radiopeptide targeting of metastatic anaplastic meningioma: case report. Radiat Oncol 6(1):94
Seystahl K, Stoecklein V, Schüller U, Rushing E, Nicolas G, Schäfer N et al (2016) Somatostatin receptor-targeted radionuclide therapy for progressive meningioma: benefit linked to 68Ga-DOTATATE/-TOC uptake. Neuro-Oncology 18(11):1538–1547
van Essen M, Krenning EP, Kooij PP, Bakker WH, Feelders RA, de Herder WW et al (2006) Effects of therapy with [177Lu-DOTA0, Tyr3]Octreotate in patients with paraganglioma, meningioma, small cell lung carcinoma, and melanoma. J Nucl Med 47(10):1599–1606
Gerster-Gilliéron K, Forrer F, Maecke H, Mueller-Brand J, Merlo A, Cordier D (2015) 90Y-DOTATOC as a therapeutic option for complex recurrent or progressive meningiomas. J Nucl Med 56(11):1748–1751
Backhaus P, Huss S, Kösek V, Weckesser M, Rahbar K (2018) Lung metastases of intracranial atypical meningioma diagnosed on posttherapeutic imaging after 177Lu-DOTATATE therapy. Clin Nucl Med 43(6):e184–e185
Unterrainer M, Niyazi M, Tonn JC, Ilhan H, Bartenstein P, Albert NL (2019) Current status of SSR-directed imaging and therapy in meningioma. Clin Transl Imaging 7:171–180
Werner R, Weich A, Kircher M, Solnes L, Javadi M, Higuchi T et al (2018) The theranostic promise for neuroendocrine tumors in the late 2010s-where do we stand, where do we go? Theranostics 8(22):6088–6100
Nicolas GP, Beykan S, Bouterfa H, Kaufmann J, Bauman A, Lassmann M et al (2018) Safety, biodistribution, and radiation dosimetry of 68Ga-OPS202 in patients with gastroenteropancreatic neuroendocrine tumors: a prospective phase I imaging study. J Nucl Med 59(6):909–914
Dalm SU, Nonnekens J, Doeswijk GN, de Blois E, Van Gent DC, Konijnenberg MW et al (2016) Comparison of the therapeutic response to treatment with a 177Lu-labeled somatostatin receptor agonist and antagonist in preclinical models. J Nucl Med 57(2):260–265
Nicolas GP, Mansi R, McDougall L, Kaufmann J, Bouterfa H, Wild D et al (2017) Biodistribution, pharmacokinetics, and dosimetry of 177Lu-, 90Y-, and 111In-labeled somatostatin receptor antagonist OPS201 in comparison to the agonist 177Lu-DOTATATE: the mass effect. J Nucl Med 58(9):1435–1441
Nicolas G, Baum R, Herrmann K, Lassmann M, Hicks R, Haug A et al (2017) Phase 1/2 open-label trial to assess the safety and preliminary efficacy of 177Lu-OPS201 as peptide receptor radionuclide therapy in patients with somatostatin receptor-positive, progressive neuroendocrine tumours. In: UKI NETS 15th national conference, vol 52. BioScientifica
Reidy DL, Pandit-Taskar N, Krebs S, O’Donoghue JA, Raj NP, Cruz E et al (2017) Theranostic trial of well differentiated neuroendocrine tumors (NETs) with somatostatin antagonists 68Ga-OPS202 and 177Lu-OPS201. J Clin Oncol 35(15_suppl):4094
Tian R, Jacobson O, Niu G, Kiesewetter DO, Wang Z, Zhu G et al (2018) Evans blue attachment enhances somatostatin receptor subtype-2 imaging and radiotherapy. Theranostics 8(3):735
Zhang J, Wang H, Jacobson O, Cheng Y, Niu G, Li F et al (2018) Safety, pharmacokinetics, and dosimetry of a long-acting radiolabeled somatostatin analog 177Lu-DOTA-EB-TATE in patients with advanced metastatic neuroendocrine tumors. J Nucl Med 59(11):1699–1705
Wang H, Cheng Y, Zhang J, Zang J, Li H, Liu Q et al (2018) Response to single low-dose 177Lu-DOTA-EB-TATE treatment in patients with advanced neuroendocrine neoplasm: a prospective pilot study. Theranostics 8(12):3308
Kratochwil C, Giesel F, Bruchertseifer F, Mier W, Apostolidis C, Boll R et al (2014) 213 Bi-DOTATOC receptor-targeted alpha-radionuclide therapy induces remission in neuroendocrine tumours refractory to beta radiation: a first-in-human experience. Eur J Nucl Med Mol Imaging 41(11):2106–2119
Šimeček J, Hermann P, Seidl C, Bruchertseifer F, Morgenstern A, Wester H-J et al (2018) Efficient formation of inert Bi-213 chelates by tetraphosphorus acid analogues of DOTA: towards improved alpha-therapeutics. EJNMMI Res 8(1):78
Suppiah S, Nassiri F, Bi WL, Dunn IF, Hanemann CO, Horbinski CM et al (2019) Molecular and translational advances in meningiomas. Neuro-oncology 21(Supplement_1):i4–i17
Lee Y, Liu J, Patel S, Cloughesy T, Lai A, Farooqi H et al (2010) Genomic landscape of meningiomas. Brain Pathol 20(4):751–762
Zack TI, Schumacher SE, Carter SL, Cherniack AD, Saksena G, Tabak B et al (2013) Pan-cancer patterns of somatic copy number alteration. Nat Genet 45(10):1134
Zang K (2001) Meningioma: a cytogenetic model of a complex benign human tumor, including data on 394 karyotyped cases. Cytogenet Genome Res 93(3–4):207–220
Yuzawa S, Nishihara H, Tanaka S (2016) Genetic landscape of meningioma. Brain Tumor Pathol 33(4):237–247
Sahm F, Schrimpf D, Stichel D, Jones DT, Hielscher T, Schefzyk S et al (2017) DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol 18(5):682–694
Albert NL, Weller M, Suchorska B, Galldiks N, Soffietti R, Kim MM et al (2016) Response assessment in neuro-oncology working group and European association for neuro-oncology recommendations for the clinical use of PET imaging in gliomas. Neuro-oncology 18(9):1199–1208
Suchorska B, Giese A, Biczok A, Unterrainer M, Weller M, Drexler M et al (2017) Identification of time-to-peak on dynamic 18F-FET-PET as a prognostic marker specifically in IDH1/2 mutant diffuse astrocytoma. Neuro-oncology 20(2):279–288
Verger A, Stoffels G, Bauer EK, Lohmann P, Blau T, Fink GR et al (2018) Static and dynamic 18 F-FET PET for the characterization of gliomas defined by IDH and 1p/19q status. Eur J Nucl Med Mol Imaging 45(3):443–451
Brastianos PK, Galanis E, Butowski N, Chan JW, Dunn IF, Goldbrunner R et al (2019) Advances in multidisciplinary therapy for meningiomas. Neuro-Oncology 21(Supplement_1):i18–i31
Demetri GD, Chawla SP, Mv Mehren, Ritch P, Baker LH, Blay JY et al (2009) Efficacy and safety of trabectedin in patients with advanced or metastatic liposarcoma or leiomyosarcoma after failure of prior anthracyclines and ifosfamide: results of a randomized phase II study of two different schedules. J Clin Oncol 27(25):4188–4196
Preusser M, Spiegl-Kreinecker S, Lötsch D, Wöhrer A, Schmook M, Dieckmann K et al (2012) Trabectedin has promising antineoplastic activity in high-grade meningioma. Cancer 118(20):5038–5049
Preusser M, Silvani A, Rhun EL, Soffietti R, Lombardi G, Sepúlveda JM et al (2019) Trabectedin for recurrent WHO grade II or III meningioma: a randomized phase II study of the EORTC Brain Tumor Group (EORTC-1320-BTG). J Clin Oncol 37(15_suppl):2007
Du Z, Abedalthagafi M, Aizer AA, McHenry AR, Sun HH, Bray M-A et al (2015) Increased expression of the immune modulatory molecule PD-L1 (CD274) in anaplastic meningioma. Oncotarget 6(7):4704
Han SJ, Reis G, Kohanbash G, Shrivastav S, Magill ST, Molinaro AM et al (2016) Expression and prognostic impact of immune modulatory molecule PD-L1 in meningioma. J Neurooncol 130(3):543–552
Chamberlain MC (2015) What constitutes activity of systemic therapy in recurrent meningioma? Neurology 85:1090
Huang RY, Bi WL, Weller M, Kaley T, Blakeley J, Dunn I et al (2019) Proposed response assessment and endpoints for meningioma clinical trials: report from the Response Assessment in Neuro-Oncology Working Group. Neuro-Oncology 21(1):26–36
Thakral P, Sen I, Pant V, Gupta SK, Dureja S, Kumari J et al (2018) Dosimetric analysis of patients with gastro entero pancreatic neuroendocrine tumors (NETs) treated with PRCRT (peptide receptor chemo radionuclide therapy) using Lu-177 DOTATATE and capecitabine/temozolomide (CAP/TEM). Br J Radiol 91(1091):20170172
Yadav MP, Ballal S, Bal C (2019) Concomitant 177Lu-DOTATATE and capecitabine therapy in malignant paragangliomas. EJNMMI Res 9(1):13
Tesson M, Vasan R, Hock A, Nixon C, Rae C, Gaze M et al (2018) An evaluation in vitro of the efficacy of nutlin-3 and topotecan in combination with 177Lu-DOTATATE for the treatment of neuroblastoma. Oncotarget 9(49):29082
Acknowledgements
We acknowledge Inglewood Biomedical Editing for professional manuscript editing.
Author information
Authors and Affiliations
Contributions
MU: conception and design of the article, drafting of the article, final approval. MN: conception and design of the article, critical revision for important intellectual content, final approval. JCT: conception and design of the article, critical revision for important intellectual content, final approval. HI: conception and design of the article, critical revision for important intellectual content, final approval. PB: conception and design of the article, critical revision for important intellectual content, final approval. NLA: conception and design of the article, critical revision for important intellectual content, final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights statement
This article does not contain any studies with animals or human participants performed by any of the authors; therefore, the local ethics committee of the LMU Munich waived the requirement for additional approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Unterrainer, M., Niyazi, M., Tonn, J.C. et al. A look ahead: future directions of SSR-directed imaging and therapy in meningioma. Clin Transl Imaging 7, 357–362 (2019). https://doi.org/10.1007/s40336-019-00333-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-019-00333-4