Abstract
Purpose
Since meningiomas show a high expression of somatostatin receptor subtype 2, PET with 68Ga-DOTATOC was proposed as an additional imaging modality beside CT and MRI for planning radiotherapy. We investigated the input of 68Ga-DOTATOC-PET/CT on the definition of the “gross tumour volume” (GTV) in meningiomas, in order to assess the potential value of this method.
Methods
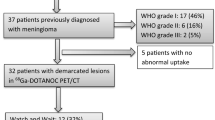
Prior to radiotherapy, 42 patients with meningiomas (26 f, 16 m, mean age 55) underwent MRI and 68Ga-DOTATOC-PET/CT examinations. History: operated n = 24, radiotherapy n = 1, operation and radiotherapy n = 8, no treatment n = 9. PET/CT and MRI data were co-registered using a BrainLAB workstation. For comparison, the GTV was defined first under consideration of CT and MRI data, then using PET data.
Results
3/42 patients were excluded from the analysis (two with negative PET results, one with an extensive tumour, not precisely delineable by MRI or PET/CT). The average GTVCT/MRI was 22(±19)cm³; GTVPET was 23(±20)cm³. Additional GTV, obtained as a result of PET was 9(±10)cm³ and was observed in patients with osseous infiltration. In some pre-treated patients there were intratumoural areas (as identified in CT/MRI) without SR-expression (7(±11)cm³). Common GTV as obtained by both CT/MRI and PET was 15(±14)cm³. The mean bi-directional difference between the GTVCT/MRI and GTVPET accounted to 16(±15)cm³ (93%, p < 0.001). In a subgroup of seven patients with multiple meningiomas, PET showed a total of 19 lesions; nine of them were not recognizable by CT or MRI.
Conclusion
68Ga-DOTATOC-PET enables delineation of SR-positive meningiomas and delivers additional information to both CT and MRI regarding the planning of stereotactic radiotherapy. The acquisition on a PET/CT scanner helps to estimate the relation of PET findings to anatomical structures and is especially useful for detection of osseous infiltration. 68Ga-DOTATOC-PET also allows detection of additional lesions in patients with multiple meningiomas.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Meningiomas are mesodermal tumours originating in the arachnoid membrane and situated in the skull or spinal canal. With a yearly incidence of approximately 2.5–6 /100,000 they constitute 13–26% of primary intracranial tumours [1, 2]. Even with apparent total removal, the recurrence rate varies from 9–19% at 10 years and up to 44% in the case of subtotal resection [2]. Because of the high rate of recurrence, a complete surgical resection is generally the treatment of choice, but is not always possible, especially when the tumour is located in the vicinity of critical intracranial structures like nerves or blood vessels impairing accessibility, or, for tumours located at the skull base, with possible infiltration of osseous structures. Radiotherapy offers a valuable therapeutic option and finds routine application in the therapy of anaplastic, atypical, malignant meningiomas, inoperable and residual tumours, recurrent meningiomas as well as in the therapy of meningiomatosis. In lesions smaller than 4 cm in diameter, a stereotactic radiotherapy is particularly helpful. An accurate delineation of the tumour from its surrounding structures is a premise for successful stereotactic radiotherapy.
Cerebral magnetic resonance imaging (MRI) and computer tomography (CT) are standard modalities for the planning of stereotactic radiotherapy. It has been shown that CT and MRI complement each other in the diagnosis of meningiomas [3]. CT has proven to be more effective than MRI in diagnosing bone infiltrations at the anterior region of the skull base [4, 5]. MRI has a higher soft-tissue contrast and allows much better differentiation between gray and white brain substance. Moreover, the meningeal structures can be visualised by MRI and the meningiomas can be easily detected with the use of intravenous contrast media [6, 7]. However, MRI is of limited specificity when distinguishing between tumour residues/recurrences and post-therapeutic changes such as scarring of the meningeal layers and tumour.
Receptor imaging offers an interesting additional tool for imaging of meningiomas. Meningiomas show a high expression of several receptors, among these, somatostatin receptor subtype 2 (SSTR 2) [8, 9]. The SSRT ligand [111In]-DTPA-D-Phe1-octreotide (111In-octreotide) was shown to be valuable for differentiating meningiomas from other intracranial or intraspinal tumours like neurinomas, neurofibromas, and for post-surgical control and diagnosis of re-growth [10]. Because of a poor resolution of single photon emission computed tomography (SPECT), meningiomas with a diameter of less than 2.7 cm or a volume smaller than 10 ml cannot be detected [11]. Recently, another somatostatin analogue 1,4,7,10-tetraazacyclododecane-N,N′,N″,N″′-tetraacetic-acid-D-Phe1-Tyr3-octreotide (DOTATOC) capable of being labelled with the positron emitter 68Ga (half-life, 68 min), was developed. 68Ga-DOTATOC is a positron emission tomography (PET) tracer and shows an up to a nine-fold higher affinity to SSTR 2, as compared to 111In-DTPA-octreotide [12].
In the present study we performed PET/CT using 68Ga-DOTATOC in a group of 42 patients with meningiomas and retrospectively investigated the potential influence of PET on the definition of GTV, as compared to CT (as a part of PET/CT) and MRI. The purpose of the study was to assess the potential value of 68Ga-DOTATOC PET/CT for planning stereotactic radiation therapy.
Material and methods
Patients
Enrolled in this study were 42 consecutive patients with known meningiomas (26 females; 16 males; age 21 to 73 years; mean age 55), who were referred for stereotactic radiation therapy to our centre between August 2006 and February 2008 (Table 1). In 33/42 patients who were pre-treated by surgery and/or radiation therapy (surgery n = 24; radiation therapy n = 1, both surgery and radiation therapy n = 8), a recurrent/residual tumour was suspected based on MRI. Nine patients had no prior treatment. Since magnetic resonance imaging (MRI) was one of the imaging modalities to be compared with PET, patients who could not be examined with MRI (for example patients with metal implants) or patients not eligible for a PET examination (for example pregnant women) were not enrolled in the study. All patients were investigated by 68Ga-DOTATOC PET/CT prior to radiation therapy.
The study was based on the Declaration of Helsinki and the principles of ‘good clinical practice’. The protocol was approved by the ethics committee of our institution. Written informed consent was obtained from all patients before enrolment into the study.
Methods
MR imaging
MRI of the skull was performed using a head coil in a 1.5 T scanner (1.5 T Signa, General Electric, Milwaukee, USA, or 1.5 T Philips Gyroscan ACS NT, Philips, Best, The Netherlands). T2-weighted spin-echo sequences (TR 2,500 ms/TE 80 ms; Matrix 256 × 256; one acquisition, 5-mm slice thickness) as well as T1-weighted spin-echo sequences (TR 700 ms/TE 15 ms; Matrix 512 × 512; one acquisition; 4–5 mm slice thickness) without and at least in two different dimensions after intravenous application of Gadolinium-DTPA (Magnevist, Schering AG, Berlin) at a dosage of 0.1 mmol/kg of body weight were obtained.
PET/CT imaging
PET data were obtained in three-dimensional mode using a hybrid PET/CT system (Biograph 16 Siemens; Erlangen; Germany). 68Ga was obtained from a 68Ge/68Ga radionuclide generator (Eckert & Ziegler, Berlin, Germany). For the synthesis of 68Ga-DOTATOC, the method previously described by Zhernosekov et al. was used [13]. Labelling yields of >95% were achieved. The radiochemical purity was >99%. 68Ga-DOTATOC was applied intravenously followed by a tracer uptake phase of 60 min as recommended by Henze et al. [14]. The applied dose of 68Ga-DOTATOC was between 70 and 120 MBq. The patient was positioned in a dedicated positioning device for the head with an additional cushion and bandages for fixation. An unenhanced CT scan (detector collimation, 16 × 1.5 mm; tube current, 100 mA; tube voltage, 120 kV; gantry rotation time 0.8 s) covering the entire head was performed for attenuation correction. PET was acquired in a single bed position with a 16-cm axial FOV from the base of the skull to the vertex over 20 min. PET emission data were reconstructed iteratively (OSEM algorithm) using a 128 × 128 matrix.
Image fusion and data analysis
MRI and PET/CT data were transferred to a computer that supports a commercially available software package for radiation therapy planning (Brain SCAN 5.1, BrainLAB AG) and fused automatically using a mutual information algorithm. A detailed description of the method for image fusion was previously published by Grosu et al. who equally tested the validity of the software [15]. The analysis of the data and the delineation of the tumour margins were performed manually by an experienced radiation therapist and nuclear medicine physician.
We followed the definition of the gross tumour volume (GTV) recommended by report No. 50 (1993) of the international commission on radiation units and measurements(ICRU) and later on modified report No. 62 (1999) of the same commission [16, 17]. Hereby, the GTV is considered as the tumour volume detectable with diagnostic or operative methods. For the delineation of the “composite volume” (GTVCT/MRI), data of both MRI and CT were considered: CT in bone and soft-tissue windowing as well as T1-weighted, fat-saturated MRI with and without gadolinium enhancement. The “composite volume” (GTV CT/MRI) was therefore the volume that enclosed the tumour tissue, detectable by CT and/or MRI. In a separate step, the target volume was delineated using 68Ga-DOTATOC-PET (GTVPET). The volume GTVPET was defined manually under consideration of areas with high 68Ga-DOTATOC accumulation, following the method published by Astner et al. [18]. The threshold of PET windowing was adapted in regions where the tumour bordered to anatomical structures or normal brain tissue, which could be easily outlined in fused MR/PET images. Further, the GTVPET and GTVCT/MRI were compared using fused PET/CT and MR images. GTV was defined enclosing all tumour areas visualized in all the three imaging modalities, i.e., CT, MRI and 68Ga-DOTATOC-PET (GTVCT/MRI/PET). We calculated the additional tumour volume with high receptor expression, shown by 68Ga-DOTATOC-PET \( \left( {{\text{GT}}{{\text{V}}_{\text{PET}}}{\text{plus}} = {\text{GT}}{{\text{V}}_{{\text{CT}}/{\text{MRI}}/{\text{PET}}}} - {\text{GT}}{{\text{V}}_{{\text{CT/MRI}}}}} \right) \), as well as volume of areas, which were not recognizable in PET, but detectable by CT and/or MRI \( \left( {{\text{GT}}{{\text{V}}_{{\text{CT/MRI}}}}{\text{plus}} = {\text{GT}}{{\text{V}}_{{\text{CT/MRI/PET}}}} - {\text{GT}}{{\text{V}}_{\text{PET}}}} \right) \). Moreover, we calculated the bi-directional difference between the GTVCT/MRI and GTVPET. The additional information, caused by the inclusion of PET in the radiation therapy planning was noted (e.g., invasion or infiltration of critical structures like the sinuses by the tumour, infiltration of osseous structures as well as detection of additional lesions).
Statistics
Statistical analysis was performed using R (Version 2.8.1; The R Foundation for Statistical Computing). Continuous data were described with mean (± standard deviation) and median (interquartile range [25th/75th percentiles]). Due to the small sample sizes, non-parametric distribution of data was assumed. Volumetric results of the PET, CT, and MRI in the same patient group were tested by the Wilcoxon test, whereas the Mann-Whitney-U-test was used for comparisons between the subgroups of pretreated and untreated patients.
Results
The determination of GTV was possible in MRI and/or CT in 41 out of 42 studied patients. Forty patients out of 42 showed areas with a high 68Ga-DOTATOC uptake. Two patients (Nos. 39 and 40, Table 1), both with pre-treated tumours (surgery), were excluded from the study because the 68Ga-DOTATOC-PET showed no SR-positive tumour in the Gd-enhancing lesions detected in post-surgical MRI. Another patient (No. 17) with an extensive tumour was excluded from the analysis, because the GTV could neither be precisely delineated by MRI nor by PET/CT. Thus, the final analysis was based on the comparison of 39 patients with the GTV definable in all modalities (MRI, CT, and PET).
The GTVCT/MRI equalled GTVPET in 11/39 patients (28%). Consideration of 68Ga-DOTATOC-PET led to a modification of GTV in 28/39 studied patients. GTVCT/MRI was larger than GTVPET in 9/39 patients (23%) and smaller than GTV PET in 19 patients (49%) (see example presented in Fig. 1). Interestingly, in all 28 patients, the differences in GTVPET and GTVCT/MRI were bi-directional (both 68Ga-DOTATOC-accumulating, CT/MRI-negative and non 68Ga-DOTATOC-accumulating, CT/MRI-positive areas in the same patient). The mean GTVCT/MRI encompassing the volumes defined under consideration of CT and MRI was 22(±19)cm3. The mean GTVPET was 23(±20)cm3 and showed no significant difference to GTVCT/MRI (p = 0.199). The implementation of 68Ga-DOTATOC-PET data led to a mean increase of the final GTV by 9(±10)cm3, as compared to volumes defined with CT and MRI only. On the other side, there were also areas categorized in CT or MRI as tumourous which did not show any SR expression (Fig. 2). Such areas without 68Ga-DOTATOC accumulation had an average volume of 7(±11)cm3. The intersection of GTVCT/MRI and GTVPET averaged 15(±14)cm3. The mean bi-directional difference between the GTVCT/MRI and GTVPET was 16(±15)cm3, which corresponds to a mean alteration of GTVCT/MRI of 93(±77)% (p < 0.001). If looking at the subgroups of pretreated and untreated patients separately, the mean bi-directional difference between the GTVCT/MRI and GTVPET was 87(±73)% in pretreated patients (n = 30) and 113(±92)% in untreated patients (n = 9). A comparison of the amplitude of these bi-directional changes between both groups delivered no significant difference (p = 0.589).
A 58-year-old male patient (pat. No. 4) with relapse of an anaplastic meningioma (WHO III) in the left parieto-occipital convexity at left falx: Image fusion of 68Ga-DOTATOC-PET and Gd-enhanced MRI demonstrates an infiltration of the superior sinus sagittalis, which is not clearly differentiated from a physiological Gd-enhancement in the sinus on MRI
In nine patients, the GTVCT/MRI was larger than GTVPET. Remarkably, six out of these nine patients had undergone previous treatment. On the other hand, GTVPET was larger than GTVCT/MRI in 19 patients. 68Ga-DOTATOC-PET/CT revealed an infiltration of the skull base in 29/39 patients. In eight out of these 29 patients, 68Ga-DOTATOC-PET showed an infiltration of osseous structures, which was not detectable by CT (Fig. 1). An infiltration of the venous sinus, which was hardly (equivocal findings) detectable in MRI, was suggested by 68Ga-DOTATOC-PET in five patients (Fig. 2). A high uptake of 68Ga-DOTATOC was found in the pituitary glands of all the patients, hampering the PET-based demarcation of tumours in some cases.
In the subgroup of seven patients with multiple meningiomas, we performed an additional analysis on a lesional basis. 68Ga-DOTATOC-PET demonstrated a total of 19 lesions in this subgroup, nine of which were not detectable by CT or by MRI (Fig. 3).
Discussion
This simulation study evaluated the potential role of 68Ga-DOTATOC PET/CT in the radiation planning of meningiomas. If considering the PET data, the mean bi-directional percentage of GTV alteration (as compared to the composite volume) amounted to 93%. The GTV was modified based on 68Ga-DOTATOC-PET data in 28/39 patients with positive PET scans (72%). In nine of the patients, the GTVPET was smaller than the GTVCT/MRI. Six of these nine patients have initially been pre-treated probably presenting areas with therapy-induced changes (post-radiation necrosis, scars) which in Gd-enhanced MRI are difficult to differentiate from viable tumour. On the other hand, GTVPET was larger than the composite volume (GTVCT/MRI) in 19 cases, 17 of which were skull base meningiomas. This observation confirms an earlier study revealing 68Ga-DOTATOC-PET as being particularly valuable in providing additional information with regard to the extent of tumour infiltration into osseous structures at the skull base [14]. Moreover, an infiltration of the venous sinuses was detected with the help of 68Ga-DOTATOC PET in five patients which was judged equivocal on MRI because of physiological gadolinium enhancement in the sinuses. Constrictively, it should be noted that in our study the 1.5 Tesla scanner was used for MR imaging. The 3.0 Tesla MRI allows performing a high-spatial resolution 3D cerebral contrast-enhanced MR venography, which could have some advantages for detection of venous sinus invasion by meningiomas [19].
The results of the present PET/CT study confirm data published by Milker-Zabel et al., whereby in 19 out of 26 patients (73%), the planning target volume was significantly modified by the use of fused 68Ga-DOTATOC-PET, CT, and MRI [20]. The high sensitivity and specificity of PET in the diagnosis of meningiomas can only be useful if a reliable topographic correlation/mapping with anatomical landmarks are available. In contrast to previous studies [14, 20, 21], we used a hybrid PET/CT system that allows a simultaneous acquisition of precisely co-registered PET and CT scans and facilitates implementation of 68Ga-DOTATOC-PET data in radiation therapy planning. Since MRI compared to CT has some advantages in the diagnosis of meningiomas, an additional fusion of the MRI and PET/CT data offers additional clinically valuable information, as shown by our simulation study.
PET with radio-labelled amino acids represents an alternative approach for metabolic imaging of meningiomas [18, 22–26]. Astner et al. [18] showed that 11C-methionine PET can influence the radiotherapy planning in the majority (29/32) of patients with base skull meningiomas resulting in both increase, as well as in a decrease of GTV. Interestingly, in the study by Astner et al. the MET-PET was able to detect small tumour portions that were not identified by CT or MRI. The intensity of the 11C-MET uptake has been shown to correlate with the Ki67 index. Unfortunately, the 11C-methionine is of limited availability due to the short physical half-life (20 min) of the isotope 11C and can be used only in a few PET centres equipped with a cyclotron. Rutten et al. reported the use of a fluorinated amino acid tracer, 18F-TYR for GTV estimation in 11 patients with skull base meningiomas (n = 13 lesions) and found that the 18F-TYR uptake extended beyond the MRI lesion in 38% of the tumours, and were smaller in 8% of the tumours [23]. Another 18F-labelled synthetic tyrosine derivate, 18F-FET, which was thoroughly validated in the diagnosis of gliomas [27–29], might be useful in the diagnostic evaluation of meningiomas. In contrast to the 11C-methionine, the 18F-FET does not accumulate in the pituitary gland and might therefore have potential advantages over the 68Ga-DOTATOC for detecting intrasellar invasion of meningiomas. Indeed, in some patients in our study, the meningiomas with close proximity to the sella turcica could not be reliably differentiated from the adjacent pituitary gland, showing a physiologically high expression of somatostatin receptors. On the other hand, a high accumulation of 18F-FET in sinuses could hamper the detection of sinus infiltration, which can be easily visualised using 68Ga-DOTATOC. Up to now, no clinical studies have compared 18F-FET with 68Ga-DOTATOC and no studies have investigated 18F-FET uptake in meningiomas. This issue should be a matter of further comparative investigations.
Similar to many studies on target volume definition of meningiomas, the main limitation of our study, being a simulative study is the lack of histological verification. Thus, the reason for negative PET results in two patients (Nos. 39 and 40) cannot be estimated because of the lack of an in-depth verification. These patients (who both underwent radiation therapy) were excluded from the final analysis. On the other hand, false-positive findings cannot be totally excluded, but appear unlikely since the uptake of DOTATOC to SSTR is known to be highly specific. Before a definite recommendation for the adjustment of radiation therapy to GTVPET, histological correlations of 68Ga-DOTATOC uptake patterns in meningiomas has to be performed, this is a current project at our medical centre.
Conclusion
68Ga-DOTATOC-PET enables a delineation of the SR-positive tumour volume of meningiomas, delivering valuable additional information on tumour size and extent to both CT and MRI. We conclude that 68Ga-DOTATOC-PET represents a very promising imaging tool for planning stereotactic radiotherapy. The acquisition of 68Ga-DOTATOC-PET data on a PET/CT scanner helps to estimate the relation of PET findings to anatomical structures and seems to be especially useful for detection of bone infiltrations. Moreover, 68Ga-DOTATOC-PET seems useful in patients of multiple meningiomas presenting with a higher sensitivity of lesion detection than CT or MRI.
References
Preston-Martin S. Descriptive epidemiology of primary tumors of the brain, cranial nerves and cranial meninges in Los Angeles County. Neuroepidemiology. 1989;8:283–95.
Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957;20:22–39.
Khoo VS, Adams EJ, Saran F, Bedford JL, Perks JR, Warrington AP, et al. A comparison of clinical target volumes determined by CT and MRI for the radiotherapy planning of base of skull meningiomas. Int J Radiat Oncol Biol Phys. 2000;46:1309–17.
Tomura N, Hirano H, Sashi R, Hashimoto M, Kato K, Takahashi S, et al. Comparison of MR imaging and CT in discriminating tumour infiltration of bone and bone marrow in the skull base. Comput Med Imaging Graph. 1998;22:41–51.
Paling MR, Black WC, Levine PA, Cantrell RW. Tumor invasion of the anterior skull base: a comparison of MR and CT studies. J Comput Assist Tomogr. 1987;11:824–30.
Weingarten K, Ernst RJ, Jahre C, Zimmerman RD. Detection of residual or recurrent meningioma after surgery: value of enhanced vs. unenhanced MR imaging. Am J Roentgenol. 1992;158:645–50.
Schörner W, Schubeus P, Henkes H, Lanksch W, Felix R. “Meningeal sign”: a characteristic finding of meningiomas on contrast-enhanced MR images. Neuroradiology. 1990;32:90–3.
Dutour A, Kumar U, Panetta R, Ouafik L, Fina F, Sasi R, et al. Expression of somatostatin receptor subtypes in human brain tumors. Int J Cancer. 1998;76:620–7.
Schulz S, Pauli SU, Schulz S, Händel M, Dietzmann K, Firsching R, et al. Immunohistochemical determination of five somatostatin receptors in meningioma reveals frequent over expression of somatostatin receptor subtype sst2A. Clin Cancer Res. 2000;6:1865–74.
Schmidt M, Scheidhauer K, Luyken C, Voth E, Hildebrandt G, Klug N, et al. Somatostatin receptor imaging in intracranial tumours. Eur J Nucl Med. 1998;25:675–86.
Bohuslavizki KH, Brenner W, Braunsdorf WE, Behnke A, Tinnemeyer S, Hugo HH, et al. Somatostatin receptor scintigraphy in the differential diagnosis of meningioma. Nucl Med Commun. 1996;17:302–10.
Reubi JC, Schär JC, Waser B, Wenger S, Heppeler A, Schmitt JS, et al. Affinity profiles for human somatostatin receptor subtypes SST1-SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med. 2000;27:273–82.
Zhernosekov KP, Filosofov DV, Baum RP, Aschoff P, Bihl H, Razbash AA, et al. Processing of generator-produced 68Ga for medical application. J Nucl Med. 2007;48:1741–8.
Henze M, Schuhmacher J, Hipp P, Kowalski J, Becker DW, Doll J, et al. PET imaging of somatostatin receptors using [68GA]DOTA-D-Phe1-Tyr3-octreotide: first results in patients with meningiomas. J Nucl Med. 2001;42:1053–6.
Grosu AL, Lachner R, Wiedenmann N, Stärk S, Thamm R, Kneschaurek P, et al. Validation of a method for automatic image fusion (BrainLAB System) of CT data and 11C-methionine-PET data for stereotactic radiotherapy using a LINAC: first clinical experience. Int J Radiat Oncol Biol Phys. 2003;56:1450–63.
ICRU Report 50. Prescribing, recording and reporting photon beam therapy. Bethesda, MD: International Commission on Radiation Units and Measurements; 1993.
ICRU Report 62. Prescribing, recording and reporting photon beam therapy. Supplement to ICRU Report 50. Bethesda, MD: International Commission on Radiation Units and Measurements; 1999.
Astner ST, Dobrei-Ciuchendea M, Essler M, Bundschuh RA, Sai H, Schwaiger M, et al. Effect of 11C-Methionine-Positron emission tomography on gross tumor volume delineation in stereotactic radiotherapy of skull base meningiomas. Int J Radiat Oncol Biol Phys. 2008;15:1161–7.
Nael K, Fenchel M, Salamon N, Duckwiler GR, Laub G, Finn JP, et al. Three-dimensional cerebral contrast-enhanced magnetic resonance venography at 3.0 Tesla: initial results using highly accelerated parallel acquisition. Invest Radiol. 2006;41(10):763–8.
Milker-Zabel S, Zabel-du Bois A, Henze M, Huber P, Schulz-Ertner D, Hoess A, et al. Improved target volume definition for fractionated stereotactic radiotherapy in patients with intracranial meningiomas by correlation of CT, MRI, and [68Ga]-DOTATOC-PET. Int J Radiat Oncol Biol Phys. 2006;65:222–7.
Henze M, Dimitrakopoulou-Strauss A, Milker-Zabel S, Schuhmacher J, Strauss LG, Doll J, et al. Characterization of 68Ga-DOTA-D-Phe1-Tyr3-octreotide kinetics in patients with meningiomas. J Nucl Med. 2005;46:763–9.
Grosu AL, Weber WA, Astner ST, Adam M, Krause BJ, Schwaiger M, et al. 11C-methionine PET improves the target volume delineation of meningiomas treated with stereotactic fractionated radiotherapy. Int J Radiat Oncol Biol Phys. 2006;66:339–44.
Rutten I, Cabay JE, Withofs N, Lemaire C, Aerts J, Baart V, et al. PET/CT of skull base meningiomas using 2–18F-fluoro-L-tyrosine: initial report. J Nucl Med. 2007;48:720–5.
Iuchi T, Iwadate Y, Namba H, Osato K, Saeki N, Yamaura A, et al. Glucose and methionine uptake and proliferative activity in meningiomas. Neurol Res. 1999;21:640–4.
Nyberg G, Bergstrom M, Enblad P, Lilja A, Muhr C, Langstrom B. PET-methionine of skull base neuromas and meningiomas. Acta Otolaryngol. 1997;117:482–9.
Gudjonsson O, Blomquist E, Lilja A, Ericson H, Bergström M, Nyberg G. Evaluation of the effect of high-energy proton irradiation treatment on meningiomas by means of 11C-L-methionine PET. Eur J Nucl Med. 2000;27:1793–9.
Weber W, Wester HJ, Grosu AL, Herz M, Dzewas B, Feldmann HJ, et al. O-(2-[18F] fluoroethyl)-L-tyrosine and L-[methyl-11C] methionine uptake in brain tumours: initial results of a comparative study. Eur J Nucl Med. 2000;27:542–9.
Pauleit D, Floeth F, Hamacher K, et al. O-(2-[18F]fluoroethyl)-L-tyrosine PET combined with MRI improves the diagnostic assessment of cerebral gliomas. Brain. 2005;128:678–87.
Stockhammer F, Plotkin M, Amthauer H, van Landeghem FK, Woiciechowsky C. Correlation of F-18-fluoro-ethyl-tyrosin uptake with vascular and cell density in non-contrast-enhancing gliomas. J Neuro Oncol. 2008;88:205–10.
Author information
Authors and Affiliations
Corresponding author
Additional information
Fonyuy Nyuyki and Michail Plotkin contributed equally to this work.
Rights and permissions
About this article
Cite this article
Nyuyki, F., Plotkin, M., Graf, R. et al. Potential impact of 68Ga-DOTATOC PET/CT on stereotactic radiotherapy planning of meningiomas. Eur J Nucl Med Mol Imaging 37, 310–318 (2010). https://doi.org/10.1007/s00259-009-1270-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-009-1270-2