Abstract
The aim of this paper is to review the role of 18F-choline or 11C-cholinePET/CT in prostate cancer patients for diagnosis, staging and restaging in case of biochemical recurrence and on the use of 18F-choline or 11C-choline PET/CT for metastases directed salvage therapies and in castrate-resistant patients treated with systemic therapy. A literature search was performed, and articles related to 11C-choline and 18F-choline PET/CT in prostate cancer staging and biochemical relapse were identified. Search terms were: “PET” and “PET/CT”, “11C-choline”, “18F-choline”, “prostate cancer staging”, “lymph node staging” “biochemical recurrence”. We have reported the results of the most relevant publications following the criteria of clinical relevance, confirmations of choline PET/CT findings with histology, other imaging methods or clinical follow-up. Moreover, we have briefly reported about the use of 18F-choline or 11C-choline PET/CT for prostate cancer diagnosis and to monitor castrate-resistant prostate cancer (CRPC) patients treated with systemic therapy. In lymph node and distant staging choline, PET/CT showed low sensitivity but, in most of the cases, a relatively high specificity. In case of biochemical recurrence, PSA absolute value and PSA kinetics confirmed their strict correlation with choline PET/CT findings. Choline PET/CT resulted to be very useful to address salvages therapies, especially in the early phases of biochemical recurrence. The use of choline PET/CT in CRPC should be more deeply investigated. At the moment, its use in the diagnosis of prostate cancer is not recommended. 18F-choline or 11C-choline PET/CT provides useful information to clinicians mostly in case of biochemical recurrence, while the low sensitivity limits its use during staging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most common cancer in men [1]. Suspicion for PCa is most commonly based on digital rectal examination (DRE), serum levels of prostate-specific antigen (PSA) and trans-rectal ultrasound (TRUS) [2]. When histology confirms the presence of PCa, patients can be staged with different imaging procedures to evaluate tumor extension and to exclude the presence of distant spread [2]. Trans-rectal ultra-sound (TRUS), magnetic resonance imaging (MRI), computerized tomography (CT) and bone scintigraphy (BS) are the most used imaging modalities in PCa patients. 18F or 11C labeled choline is the most worldwide used radiopharmaceutical in molecular imaging, for the diagnosis, staging and re-staging of PCa patients. Positron emission tomography (PET) using choline labeled with 11C or 18F provides additional information compared to other imaging methods [3].
The aim of this paper is to review the role of 18F-choline or 11C-choline PET/CT in PCa patients for staging and restaging in case of biochemical recurrence after primary treatments.
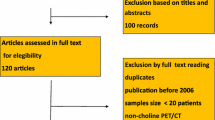
A comprehensive PubMed literature search was performed, and articles related to 11C-choline and 18F-choline PET/CT in prostate cancer staging and biochemical relapse were identified, up to April 2016. Search terms were: “PET”, “PET/CT” or “positron emission tomography/computed tomography”, “11C-choline”, “18F-choline”, “prostate cancer staging”, “lymph node staging” and “biochemical recurrence”. Overall, 320 studies were retrieved.
We have analyzed the results of the most relevant publications who reported data about the performance of 18F-choline or 11C-choline PET/CT in prostate cancer diagnosis, lymph node staging or restaging in case of biochemical recurrence. We analysed the publications were patient populations were accurately selected (prospectively or retrospectively) and were results of 18F-choline or 11C-choline PET/CT were validated by histology, by other imaging methods or by clinical follow up. According to these criteria, we finally selected 33 works that were judged clinically relevant. Of these 33 studies, 13 were focused on staging (7 on the use of PET/CT in prostate cancer diagnosis and 6 were focused on lymph node staging) and 20 on (Fig. 1) biochemical recurrence after primary treatment.
Sixty-one-year-old patient; GS 4 + 4; T3N1Mx; PSA 10 ng/ml at presentation radical prostatectomy (RP) as primary treatment. Biochemical recurrence 18 months after RP. PSA increased up to 1.2 ng/ml (PSAdt 4.5 months) when a 11C-choline PET/CT has been performed. 11C-choline PET/CT shows one area of intense uptake in an osteoblastic lesion in D12 (SUVmax 6.3). a MIP images; b CT images; c fused images. 11C-choline PET/CT performed after PET-guided EBRT (60 Gy) shows complete metabolic response (d MIP images; f fused images), while the osteoblastic lesion evident on CT images e increased in volume and density. PSA dropped to 0.2 ng/ml after EBRT
Moreover, we have briefly focused our attention on the use of 18F-choline or 11C-choline PET/CT for prostate cancer diagnosis, and to monitor castrate-resistant prostate cancer (CRPC) patients treated with systemic therapy.
Finally, we would like to underline that in this field the validation of choline-PET/CT findings stills remains a major problem. As for all the others imaging methods, the validation of choline-PET/CT findings should be performed with histology as reference standard. However, this is feasible and available only in certain circumstances, such as lymph node staging before surgery, local relapse or some bone or some lymph node (Fig. 2) lesions located in accessible regions. That is why criteria of selection only based on histology as validation standard are not possible.
Sixty-two-year-old patient; GS 4 + 3; T3N0Mx; PSA 9 ng/ml at presentation. Radical prostatectomy (RP) as primary treatment. Biochemical recurrence 28 months after RP. At the time of 11C-choline PET/CT PSA was 0.9 ng/ml; PSAdt 5 months. Area of increased uptake in a left external iliac lymph node consistent with relapse confirmed after salvage pelvic lymph node dissection. a MIP images, b fused images, c CT images
PET/CT in prostate cancer staging
Staging prostate cancer is crucial to establish the correct treatment strategy, since it should guide further decisions [2]. The detection of nodal or distant metastases should select patients who might benefit the most from a curative treatment, and those who should receive systemic therapies [2]. In lymph-nodal staging, Schiavina et al. [4] showed that 11C-choline PET/CT has low sensitivity but high specificity (60–98 %, respectively) in a population of 57 intermediate- and high-risk patients.
These data were confirmed by Contractor et al. [5] who showed a sensitivity of 40 % and a specificity of 98 % in nodal staging using 11C-choline PET/CT. Poulsen et al. [6] used 18F-choline-PET/CT to stage 210 intermediate- or high-risk patients. Authors showed a patient based sensitivity and specificity of 73 % and 87 % respectively, while a sensitivity and specificity of 56 % and 94 % have been found on a lymph node basis. Van den Bergh et al. [7] prospectively assessed sensitivity, specificity, PPV of 11C-choline PET/CT and DW-MRI for nodal staging in patients with high risk for nodal involvement. The authors enrolled 75 patients who were N0 at CT. Thirty seven of 75 patients (49 %) resulted positive at histology. On a patient-based analysis, 11C-choline PET/CT showed a sensitivity of 18.9 % and a PPV of 63.6 %, while DW-MRI showed a sensitivity of 36.1 % and a PPV of 86.7 %. On a region-based analysis, 11C-choline PET/CT showed a sensitivity of 8.2 % and a PPV of 50.0 % while DW-MRI showed a sensitivity of 9.5 % and a PPV of 40.0 %.
Recently, Evangelista et al. [8] published a meta-analysis evaluating the role of 18F-choline or 11C-choline PET/CT in staging prostate cancer. Most of the papers analyzed confirm preliminary findings assessing a low sensitivity but high specificity for 18F-choline or 11C-choline PET/CT for nodal staging. Pooled sensitivity and specificity were respectively 49 and 95 % on a patient basis.
According to the most relevant literature, the use of 18F-choline or 11C-choline PET/CT for lymph node staging should be reserved to high and very high-risk patients according to nomograms to minimize the number of false-negative results. This approach has been recently suggested by Evangelista et al. [9] who reported an overall accuracy of 18F-choline PET/CT for lymph node involvement of 83 % for high-risk patients compared to only 33 % for intermediate-risk patients.
However, in conclusions of this chapter, it should be taken into consideration that even in patients with high risk for positive lymph nodes at presentation and even in highly selected patient population (for example in the study published by Van den Bergh [7]), poor sensitivity and poor PPV may occur either on a patient- or lymph node-based analysis. The main reason for choline PET/CT false-negative findings is the size of nodal metastatic deposit, since it is very unlikely that PET/CT may detect lesions smaller than 5 mm. On the contrary, the main reason for false-positive findings is the presence of reactive lymph nodes that may show (Fig. 3) increased choline uptake.
Sixty-nine-year-old patient; GS 4 + 4 (biopsy); T3a; PSA 12 ng/ml at presentation. Staging 11C-choline PET/CT in an high risk patient. a MIP images; 11C-choline PET/CT shows intense uptake (SUVmax 5.8) in the prostate (b fused images of the prostate gland); 11C-choline PET/CT shows no significant increased uptake in two right iliac lymph nodes (c and d fused images of the right iliac lymph nodes). After surgery, 3/18 lymph nodes removed resulted positive: two in the right iliac chain and one in the left iliac chain
PET/CT in prostate cancer re-staging: PET/CT in the detection of local, lymph node and bone lesions
When a biochemical relapse (BR) occur, differentiation between the two patterns of relapse, local and/or distant is crucial to choose the proper treatment strategy [10]. The role of imaging should be to discriminate patients with single or oligo-metastatic disease that may benefit from salvage treatments with curative intent, from those affected by multi-spread of the disease that are ideal candidates for systemic therapy. None of the most used imaging modalities gave satisfactory results to identify the site of recurrence and guide further treatments [2], except MRI in the detection of local relapse in the prostatic fossa [11]. Thus, therapeutic approaches are radiotherapy in the prostatic fossa, complete or intermittent androgen deprivation therapy (ADT), or chemo-hormonal treatments [2]. In the last years, however, there is an increasing evidence of the role of image-guided salvage therapies in patients showing single or oligo-metastatic disease [12, 13].
Choline-PET/CT showed low sensitivity in the detection of local relapse after primary treatment, especially at low PSA values. A sensitivity, specificity and accuracy of 54, 92 and 65 %, respectively, have been demonstrated in a population of 115 patients who underwent 11C-choline PET/CT after radical prostatectomy in comparison with a sensitivity, specificity and accuracy of 88, 84 and 87 %, respectively, as shown by MRI [14].
These results are in line with previous findings reported by many authors [11, 15, 16] in which the sensitivity for local recurrence either using 18F-choline or 11C-choline PET/CT ranges from 50 to 60 % approximately.
On the contrary, the sensitivity for choline PET/CT for the detection of lymph-nodal involvement after primary treatment seems to be higher than other imaging methods. Kitajima and colleagues showed a better accuracy of 11C-choline PET/CT compared to MRI (92 vs 70 %) in pelvic lymph node metastasis detection, regardless of PSA values [14].
Reliable information about the sensitivity of 18F-choline or 11C-choline PET/CT in the detection of pelvic or abdominal LNs is provided by some works performed with the aim to guide salvage pelvic lymph node dissection (S-PLND) after RP [12, 17, 18].
Tilki et al. [17] studied, with 18F-choline PET/CT, 56 PCa patients with BR after radical prostatectomy who subsequently underwent bilateral pelvic and/or retroperitoneal lymph-adenectomy based on positive 18F-cholinePET/CT findings. Of 1149 lymph nodes that were removed and histological evaluated, 282 (24.5 %) harbored metastasis. On a lesion-based analysis, 18F-cholinePET/CT showed sensitivity, specificity, PPV, and NPV of 39, 95, 75, and 83 %, respectively.
The performance of 11C-choline PET/CT and bone scan was compared by Picchio et al. [19] in 78 patients with BR. The author showed a little lower sensitivity for 11C-cholinePET/CT compared to bone scan (89 vs 100 %), but a significant higher specificity (98 vs 75 %).
Fuccio and colleagues [20] performed a comparison between 11C-choline PET/CT and bone scan in 25 patients with BR showing only one lesion on bone scintigraphy. 11C-choline PET/CT detected multiple sites of relapse in 44 % of patients, with a sensitivity and specificity of 86 and 100 %, respectively. Beheshti et al. [21] studied 38 patients with the aim to compare the accuracy of 18F-choline and 18F-fluoride PET/CT for detecting bone metastases. The authors reported a sensitivity, specificity and accuracy of 74, 99 and 85 % for 18F-choline-PET/CT, and a sensitivity, specificity and accuracy of 81, 93 and 86 % for 18F-fluoride PET/CT.
It is interesting to underline that the uptake of choline in bone lesions may vary depending on the type of lesions. Beheshti et al. [22] compared the uptake of 18F-choline-PET/CT in 70 patients during staging or restaging PCa and compared these results with morphological changes identified on CT. The authors showed that lytic lesions had higher metabolism than sclerotic lesions.
Ceci and colleagues [23] confirmed these results in a group of 140 patients during BR studied with 11C-choline PET/CT. The authors analyzed 304 bone lesions (184 osteoblastic, 99 osteolytic, and 21 bone marrow lesions), showing a significant difference of SUVmax between osteosclerotic (lower values) and osteolytic (higher values) lesions.
In case of biochemical recurrence, 18F-choline or 11C-choline PET/CT demonstrated a significant clinical impact on patients’ management. In three papers recently published from three different single institution series, it was demonstrated that choline-PET/CT led to a change in the decision-making process in approximately the 50 % of cases [24–26].
Finally, in a recent meta-analysis by Fanti et al. [27], the authors analyzed (Table 1) 29 studies that enrolled 2686 patients. The authors reported for 11C-choline PET/CT a detection rate for any site of relapse of 62 % (95 % CI 53–71 %) with a pooled sensitivity of 89 % and a pooled specificity of 87 %.
PET/CT in prostate cancer re-staging: PET/CT as a guide for salvage therapies
The first large prospective study has been published by Rigatti et al. [18]. The authors performed a 11C-choline-PET/CT guided salvage lymph node dissection (S-LND) in a series of 79 patients. Patients had no more than two positive lymph node lesions at 11C-choline-PET/CT. The authors reported an early biochemical response after S-LND in 41 out of 79 patients (56.9 %) showing that PSA <4 ng/ml, time to relapse (TTR) <24 months and N0 at the time of RP were predictive of PSA response with biochemical relapse-free survival rates at 3 years of 27.5 % and biochemical relapse-free survival rates at 5-year of 10.3 %. Five-years clinical recurrence-free survival was lower for patients with positive retroperitoneal LNs at 11C-choline-PET/CT versus patients with only pelvic 11C-choline-PET/CT positive nodes (11 vs 53 %; p < 0.001).
Suardi et al. [12] performed further analysis on a subgroup of 56 patients of this series. The authors showed an overall 8-year clinical relapse- and cancer-specific mortality-free survival rates of 38 and 81 %, respectively. Multivariate analysis showed that PSA higher than 2 ng/ml at S-LND and the presence of retroperitoneal positive lymph nodes on 11C-choline-PET/CT were predictors of clinical relapse. Karnes and colleagues [28] had encouraging results in a group of 52 patients treated with S-LND after primary RP. After a median follow-up of 20 months, 57.7 % (30 of 52) patients had a PSA value lower than 0.2 ng/ml, while 75 % (39 of 52) were free of systemic progression and 96.2 % (50 of 52) were alive.
18F-choline or 11C-choline PET/CT-guided salvage radiation therapy (S-RT) using high conformal technique by intensity-modulated RT (IMRT), or helical tomotherapy (HTT), can be also performed in patients showing single or oligometastatic disease [29, 30]. The optimal timing for S-RT to obtain the best chance of cure would be when the tumor burden is low, that is, when PSA first reaches detectable levels during biochemical recurrence [10].
Würschmidt et al. [31] performed an S-RT on 11C-choline PET/CT positive findings of 19 patients during biochemical recurrence. Almost the half of the patients (49 %) were biochemical relapse free after 28 months of follow-up.
Picchio et al. [32] used 11C-choline PET/CT to guide HTT in 83 patients showing LN relapse after primary treatment. The authors achieved an early biochemical response in 70 % of cases. The same group of authors recently published [33] a study about a cohort of 68 patients with BCR after radical therapy and treated with HTT in correspondence of the pathologic choline LN uptake. The 24 months overall survival, loco-regional relapse-free survival, clinical relapse-free survival and BFS were 87, 91, 51, and 40 %, respectively.
Berkovic et al. [34] investigated whether repeated stereotactic body RT (SBRT) of oligometastatic disease is able to defer the initiation of ADT in patients with low-volume metastases. They enrolled 24 recurrent PCa patients with BCR after radical therapy and 1–3 synchronous metastases (bone and/or LNs) assessed by 18F-choline-PET/CT. Patients were treated with repeated SBRT and the ADT-free survival defined as the time interval between the first day of SBRT and the initiation of ADT was the primary end point. They concluded that repeated salvage SBRT is feasible, well tolerated and defers palliative ADT with a median of 38 months in patients with limited bone or LN PCa metastases.
In conclusion, despite S-RT or S-LND, many patients will experience disease progression soon after treatment [12, 13, 18, 31–33]. For this reason, all efforts should be attempted to exclude the presence of metastasis already present at the time of salvage treatments and not included in the planned target volume (PTV) or that could not be removed by an S-LND. In this regards, Castellucci et al. [35] a cohort 605 recurrent PCa patients showing low PSA values (PSA range 0.2-2 ng/mL) studied with 11C-choline-PET/CT after RP and listed for S-RT in the prostatic bed. 11C-choline-PET/CT detected a disease limited to the pelvis in the 13.7 % of patients, while the presence of an extra-pelvic disease was observed in the 14.7 %. The authors observed that the 11C-choline-PET/CT detection rate increased dramatically in patients with a PSAdt lower than 6 months (11C-choline-PET/CT detection rate 47 %) and in patients with ongoing ADT (11C-choline-PET/CT detection rate 46 %). The authors concluded that 11C-choline-PET/CT should be performed before salvage therapies, especially in those patients showing fast PSA kinetics to exclude the presence of distant lesions that could not be removed with an SLND or included in the planned PTV.
In conclusions of this chapter, the use of 18F-choline or 11C-choline PET/CT to guide aggressive therapies in patients with limited disease is increasing. We would like to stress, once again, that an early detection of metastatic disease is crucial for the outcome of the patients. So, despite the limitation that choline PET/CT may result negative in a significant number of patients in the early phases of BCR when PSA values are low, this is the situation where the patients have still many open options and where the decision of a systemic or aggressive therapy should be taken. The detection of few lymph node or bone metastasis by 18F-choline or 11C-choline PET/CT (oligometastatic patients) should guide the most appropriate treatment and may lead to a better outcome of these patients. This has to be assessed in future prospective studies.
PET/CT in prostate cancer diagnosis
Multi-parametric MRI using T2-weighted–diffusion weighted and dynamic contrast enhanced imaging has the highest accuracy among any other modality in the evaluation of intra-prostatic cancer [36]. A study on a sextant-based comparison with histology was performed for the first time by Farsad et al. [37] in 2005. The authors investigated the potential usefulness of 11C-choline PET/CT for detection and localization of tumors within the prostate in 36 patients scheduled for surgery. 11C-choline PET/CT showed a sensitivity of 66 %, a specificity of 81 %, an accuracy of 71 %, a positive predictive value (PPV) of 87 % and a negative predictive value (NPV) of 55 %. In conclusion, 11C-choline PET/CT was able to demonstrate foci of prostate cancer in all patients, but with a high false-negative rate on a sextant basis. In the following years, many other works substantially confirmed these findings [38–40], assessing for 11C-choline PET/CT a sub-optimal sensitivity (especially in the presence of small foci of cancer) and also a sub-optimal specificity, mainly due to the very frequent presence of non-neoplastic conditions within the prostate gland. More recently, these data were confirmed by Bundschuh et al. [41], who correlated the uptake of 11C-choline PET/CT in the prostate gland with histopathology. The results were relatively poor since only 46 % of histo-pathological positive lesions showed an increased choline uptake. Also Grosu et al. [42] could not discriminate with 11C-choline PET/CT between the presence of malignant versus normal prostate tissue. 11C-choline uptake has been found in both neoplastic and non-neoplastic tissue and often the uptake was even higher in non neoplastic-tissue.
Finally, Van den Bergh et al. [43] compared 11C-choline PET/CT and MRI for the detection of intra-prostatic tumor. The authors showed that sensitivity increased, but specificity decreased combining both modalities indicating that additional information provided by 11C-choline PET/CT is of limited value.
In conclusion, according to these poor results, 18F-choline or 11C-choline PET/CT cannot be recommended as the first-line screening imaging procedure in patients with high risk of prostate cancer or in patient candidates for active surveillance. 18F-choline or 11C-choline PET/CT showed moderate sensitivity, particularly when small carcinomas are present (below the limits of choline PET/CT resolution), but it also has shown moderate specificity since differentiation between benign changes (for example prostatitis or benign prostatic hyperplasia BPH) and malignant tissue is not always possible.
PET/CT in castrate resistant prostate cancer
Prostate cancer patients may develop a resistance to the ADT and, consequently, the hormonal blockade loses its protective effect on the tumor cells growth [10]. This condition of castrate resistant prostate cancer (CRPC), when metastatic (mCRPC), is associated with a median overall survival that ranges between 2 and 3 years and at this stage, palliation is the goal of any treatment [10]. Many different palliative therapies could be used, including systemic chemotherapy (e.g., docetaxel and cabazitaxel) and new antiandrogenic therapies (e.g., abiraterone and enzalutamide) [10]. However, a consensus about the optimal timing and different scheme treatments has not been reached [10]. The main problem for clinicians is the lack of accuracy demonstrated by PSA for predicting the response to therapy in mCRPC [10].
Ceci et al. [44] investigated a cohort of 61 mCRPC patients with 11C-choline-PET/CT performed before and after treatment to assess the response to docetaxel. The authors compared the response assessed by 11C-choline-PET/CT to docetaxel to the response assessed with PSA. The progression disease (PD) was defined as the appearance of a new 11C-choline-PET/CT positive lesion, while the PSA response was defined as a decrease of ≥50 % of the PSA values before and after chemotherapy. The main finding of the study was that 11C-choline-PET/CT PD was observed in the 44 % of patients presenting PSA response after docetaxel. It is to underline that a higher tumor burden (expressed as more than ten PET-positive bone lesions before docetaxel) was significantly associated with an increased probability of PD after treatment. Recently, abiraterone and enzalutamide were proposed as new generation ADT, with good results in terms of biochemical response and pharmacological related effects [18]. De Giorgi et al. [45] used 18F-choline-PET/CT for evaluating the early response to treatment with abiraterone and enzalutamide in two cohorts of mCRPC patients. The authors confirmed that the response assessed with 18F-choline PET/CT was associated with a more favorable overall survival than a PSA response of ≥50 %. Maines et al. [46] studied with 18F-choline-PET/CT 30 mCRPC patients treated with enzalutamide. The authors observed that SUVmax values measured at 18F-choline-PET/CT performed before enzalutamide were significantly related with biochemical, radiological and overall survival. In the next future, prospective well-designed trials should answer the question if 18F-choline or 11C-choline PET/CT could be able to predict the response to treatment and predict the progression-free survival, beyond the poor information provided by the variation of PSA levels. The information that 18F-choline or 11C-choline PET/CT could give, when performed before the administration of therapy (evaluation of the tumor burden) or during and after treatment (assess the objective response), could provide very useful information for the clinicians to choose the most appropriate treatment strategy.
References
ESMO Guidelines Task Force (2005) ESMO minimum clinical recommendations for diagnosis, treatment and follow-up of prostate cancer. Ann Oncol 16(suppl 1):i34–i36
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, Mason M, Matveev V, Wiegel T, Zattoni F, Mottet N (2014) EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 65(1):124–137
Farsad M, Schwarzenböck S, Krause BJ (2012) PET/CT and choline: diagnosis and staging. Q J Nucl Med Mol Imaging 56(4):343–353
Schiavina R, Scattoni V, Castellucci P et al (2008) 11C-choline positron emission tomography/computerized tomography for preoperative lymph-node staging in intermediate-risk and high-risk prostate cancer: comparison with clinical staging nomograms. Eur Urol 54:392–401
Contractor K, Challapalli A, Barwick T et al (2011) Use of [11C] choline PET-CT as a noninvasive method for detecting pelvic lymph node status from prostate cancer and relationship with choline kinase expression. Clin Cancer Res 17:7673–7683
Poulsen MH, Bouchelouche K, Hoilund-Carlsen PF et al (2012) [18F] fluoromethylcholine(FCH) positron emission tomography/computed tomography (PET/CT) for lymphnode staging of prostate cancer: a prospective study of 210 patients. BJU Int 110:1666–1671
Van den Bergh L, Lerut E, Haustermans K, Deroose CM, Oyen R, Isebaert S, Budiharto T, Ameye F, Mottaghy FM, Bogaerts K, Van Poppel H, Joniau S (2015) Final analysis of a prospective trial on functional imaging for nodal staging in patients with prostate cancer at high risk for lymph node involvement. Urol Oncol 33(3):109.e23–109.e31
Evangelista L, Guttilla A, Zattoni F, Muzzio PC (2013) Utility of choline positron emission tomography/computed tomography for lymph node involvement identification in intermediate- to high-risk prostate cancer: a systematic literature review and metaanalysis. Eur Urol 63:1040–1048
Evangelista L, Cimitan M, Zattoni F, Guttilla A, Saladini G (2015) Comparison between conventional imaging (abdominal-pelvic computed tomography and bone scan) and[(18)F]choline positron emission tomography/computed tomography imaging for the initial staging of patients with intermediate- to high-risk prostate cancer: a retrospective analysis. Scand J Urol 49:345–353
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, Mason M, Matveev V, Wiegel T, Zattoni F, Mottet N (2014) EAU guidelines on prostate cancer. part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol 65(2):467–479
Panebianco V, Sciarra A, Lisi D et al (2012) Prostate cancer: 1HMRS-DCEMR at 3T versus [(18)F]choline PET/CT in the detection of local prostate cancer recurrence in men with biochemical progression after radical retropubic prostatectomy (RRP). Eur J Radiol 81(4):700–708
Suardi N, Gandaglia G, Gallina A et al (2015) Long-term outcomes of salvage lymph node dissection for clinically recurrent prostate cancer: results of a single-institution series with a minimum follow-up of 5 years. Eur Urol 67(2):299–309
Ost P, Bossi A, Decaestecker K et al (2015) Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: a systematic review of the literature. Eur Urol 67(5):852–863
Kitajima K, Murphy RC, Nathan MA et al (2014) Detection of recurrent prostate cancer after radical prostatectomy: comparison of 11C-choline PET/CT with pelvic multiparametric MR imaging with endorectal coil. J Nucl Med 55(2):223–232
Castellucci P, Fuccio C, Rubello D et al (2011) Is there a role for 11C-choline PET/CT in the early detection of metastatic disease in surgically treated prostate cancer patients with a mild PSA increase of 1.5 ng/ml? Eur J Nucl Med Mol Imaging 38(1):55–63
Mamede M, Ceci F, Castellucci P et al (2013) The role of 11C-choline PET imaging in the early detection of recurrence in surgically treated prostate cancer patients with very low PSA level <0.5 ng/mL. Clin Nucl Med 38(9):e342–e345
Tilki D, Reich O, Graser A et al (2013) 18F-fluoroethylcholine PET/CT identifies lymph node metastasis in patients with prostate-specific antigen failure after radical prostatectomy but underestimates its extent. Eur Urol 63(5):792–796
Rigatti P, Suardi N, Briganti A et al (2011) Pelvic/retroperitoneal salvage lymph node dissection for patients treated with radical prostatectomy with biochemical recurrence and nodal recurrence detected by [11C]choline positron emission tomography/computed tomography. Eur Urol 60(5):935–943
Picchio M, Spinapolice EG, Fallanca F, Crivellaro C, Giovacchini G, Gianolli L, Messa C (2012) [11C]Choline PET/CT detection of bone metastases in patients with PSA progression after primary treatment for prostate cancer: comparison with bone scintigraphy. Eur J Nucl Med Mol Imaging 39(1):13–26. doi:10.1007/s00259-011-1920-z (Epub 2011 Sep 20)
Fuccio C, Castellucci P, Schiavina R, Guidalotti PL, Gavaruzzi G, Montini GC, Nanni C, Marzola MC, Rubello D, Fanti S (2012) Role of 11C-choline PET/CT in the re-staging of prostate cancer patients with biochemical relapse and negative results at bone scintigraphy. Eur J Radiol 81(8):e893–e896
Beheshti M, Vali R, Waldenberger P, Fitz F, Nader M, Loidl W, Broinger G, Stoiber F, Foglman I, Langsteger W (2008) Detection of bone metastases in patients with prostate cancer by 18F fluorocholine and 18F fluoride PET-CT: a comparative study. Eur J Nucl Med Mol Imaging 35(10):1766–1774
Beheshti M, Vali R, Waldenberger P, Fitz F, Nader M, Hammer J, Loidl W, Pirich C, Fogelman I, Langsteger W (2010) The use of F-18 choline PET in the assessment of bone metastases in prostate cancer: correlation with morphological changes on CT. Mol Imaging Biol 12(1):98–107. doi:10.1007/s11307-009-0239-7 [(Epub 2009 Jul 9. Erratum in: Mol Imaging Biol. 2010 Jun;12(3):360)]
Ceci F, Castellucci P, Graziani T, Schiavina R, Chondrogiannis S, Bonfiglioli R, Costa S, Virgolini IJ, Rubello D, Fanti S, Colletti PM (2015) 11C-choline PET/CT identifies osteoblastic and osteolytic lesions in patients with metastatic prostate cancer. Clin Nucl Med 40(5):e265–e270
Ceci F, Herrmann K, Castellucci P et al (2014) Impact of 11C-choline PET/CT on clinical decision making in recurrent prostate cancer: results from a retrospective two-centre trial. Eur J Nucl Med Mol Imaging 41(12):2222–2231 [(Erratum in: Eur J Nucl Med Mol Imaging. 2014 Dec;41(12):2359)]
Soyka JD, Muster MA, Schmid DT et al (2012) Clinical impact of 18F-choline PET/CT in patients with recurrent prostate cancer. Eur J Nucl Med Mol Imaging 39(6):936–943
Goldstein J, Even-Sapir E, Ben-Haim S et al (2014) Does choline PET/CT change the management of prostate cancer patients with biochemical failure? Am J Clin Oncol [Epub ahead of print]
Fanti S, Minozzi S, Castellucci P et al (2016) PET/CT with (11)C-choline for evaluation of prostate cancer patients with biochemical recurrence: meta-analysis and critical review of available data. Eur J Nucl Med Mol Imaging 43(1):55–69
Karnes RJ, Murphy CR, Bergstralh EJ et al (2015) Salvage lymph node dissection for prostate cancer nodal recurrence detected by 11C-choline positron emission tomography/computerized tomography. J Urol 193(1):111–116
Bolla M, Van Tienhoven G, Warde P et al (2010) External irradiation with or without long-term androgen suppression for prostate cancer with high metastatic risk: 10-year results of an EORTC randomised study. Lancet Oncol 11:1066–1073
Stephenson AJ, Bolla M, Briganti A et al (2012) Postoperative radiation therapy for pathologically advanced prostate cancer after radical prostatectomy. Eur Urol 61(3):443–451
Wurschmidt F, Petersen C, Wahl A, Dahle J, Kretschmer M (2011) [18F] fluoroethylcholine-PET/CT imaging for radiation treatment planning of recurrent and primary prostate cancer with dose escalation to PET/CT-positive lymph nodes. Radiat Oncol 1(6):44
Picchio M, Berardi G, Fodor A et al (2014) 11C-choline PET/CT as a guide to radiation treatment planning of lymph-node relapses in prostate cancer patients. Eur J Nucl Med Mol Imaging 41(7):1270–1279
Incerti E, Fodor A, Mapelli P et al (2015) Radiation treatment of lymph node recurrence from prostate cancer: is 11C-choline PET/CT predictive of survival outcomes? J Nucl Med 56(12):1836–1842
Berkovic P, De Meerleer G, Delrue L et al (2013) Salvage stereotactic body radiotherapy for patients with limited prostate cancer metastases: deferring androgen deprivation therapy. Clin Genitourin Cancer 11(1):27–32
Castellucci P, Ceci F, Graziani T, Schiavina R, Brunocilla E, Mazzarotto R, Pettinato C, Celli M, Lodi F, Fanti S (2014) Early biochemical relapse after radical prostatectomy: which prostate cancer patients may benefit from a restaging 11C-choline PET/CT scan before salvage radiation therapy? J Nucl Med 55(9):1424–1429
Metzger GJ, Kalavagunta C, Spilseth B, Bolan PJ, Li X, Hutter D, Nam JW, Johnson AD, Henriksen JC, Moench L, Konety B, Warlick CA, Schmechel SC, Koopmeiners JS (2016) Detection of prostate cancer: quantitative multiparametric MR imaging models developed using registered correlative histopathology. Radiology 29:151089
Farsad M, Schiavina R, Castellucci P, Nanni C, Corti B, Martorana G, Canini R, Grigioni W, Boschi S, Marengo M, Pettinato C, Salizzoni E, Monetti N, Franchi R, Fanti S (2005) Detection and localization of prostate cancer: correlation of (11)C-choline PET/CT with histopathologic step-section analysis. J Nucl Med 46:1642–1649
Giovacchini G, Picchio M, Coradeschi E, Scattoni V, Bettinardi V, Cozzarini C et al (2008) [(11)C]Choline uptake with PET/CT for the initial diagnosis of prostate cancer: relation to PSA leves, tumour stage and anti-androgenic therapy. Eur J Nucl Med Mol Imaging 35:1065–1073
Martorana G, Schiavina R, Corti B, Farsad M, Salizzoni E, Brunocilla E, Bertaccini A, Manferrari F, Castellucci P, Fanti S, Canini R, Grigioni WF, D’Errico Grigioni A (2006) 11C-choline positron emission tomography/computerized tomography for tumor localization of primary prostate cancer in comparison with 12-core biopsy. J Urol 176:954–960
Testa C, Schiavina R, Lodi R, Salizzoni E, Corti B, Farsad M et al (2007) Prostate cancer: sextant localization with MR imaging, MR spectroscopy, and 11C-choline PET/CT. Radiology 244(3):797–806 (Epub 2007 Jul 24)
Bundschuh RA, Wendl CM, Weirich G et al (2013) Tumour volume delineation in prostate cancer assessed by [11C]choline PET/CT: validation with surgical specimens. Eur J Nucl Med Mol Imaging 40:824–831
Grosu AL, Weirich G, Wendl C et al (2014) 11C-choline PET/pathology image coregistration in primary localized prostate cancer. Eur J Nucl Med Mol Imaging 41:2242–2248
Van den Bergh L, Koole M, Isebaert S et al (2012) Is there an additional value of (11)C-choline PET-CT to T2-weighted MRI images in the localization of intraprostatic tumor nodules? Int J Radiat Oncol Biol Phys 83:1486–1492
Ceci F, Castellucci P, Graziani T et al (2016) 11C-choline PET/CT in castration-resistant prostate cancer patients treated with docetaxel. Eur J Nucl Med Mol Imaging 43(1):84–91
De Giorgi U, Caroli P, Burgio SL et al (2014) Early outcome prediction on 18F-fluorocholine PET/CT in metastatic castration-resistant prostate cancer patients treated with abiraterone. Oncotarget 5(23):12448–12458
Maines F, Caffo O, Donner D et al (2016) Serial (18)F-choline-PET imaging in patients receiving enzalutamide for metastatic castration-resistant prostate cancer: response assessment and imaging biomarkers. Future Oncol 12(3):333–342
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was not funded.
Conflict of interest
Paolo Castellucci, Francesco Ceci, Tiziano Graziani and Stefano Fanti declare that they do not have any conflict of interest.
Retrospective studies
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Castellucci, P., Ceci, F., Graziani, T. et al. PET imaging in prostate cancer, state of the art: a review of 18F-choline and 11C-choline PET/CT applications. Clin Transl Imaging 4, 449–456 (2016). https://doi.org/10.1007/s40336-016-0191-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-016-0191-x