Abstract
Introduction
This study was designed to evaluate the results of unilateral laparoscopic adrenalectomy in patients with subclinical hypercortisolism (SH) due to adrenal incidentaloma (AI) concerning the main cardiometabolic disorders.
Methods
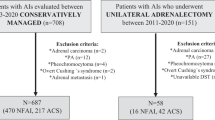
We have studied between January 2000 to December 2015, 645 patients with AI (283 males and 362 females; mean age 61.9 ± 10 years) and we found 70 patients with SH (27 males and 43 females; mean age 61.9 ± 8.4 years). Twenty-six (37%) SH patients (6 males and 20 females; mean age 58.7 ± 7.1 years) underwent unilateral laparoscopic adrenalectomy, whereas 44 SH patients (21 males and 23 females; mean age 63.9 ± 9.9 years) performed a conservative treatment. All SH patients were evaluated at diagnosis and after follow-up (mean 12 months; range 9–15 months).
Results
In only SH patients undergoing unilateral adrenalectomy we found a statistical significant reduction of the arterial hypertension and metabolic syndrome (p < 0.05, respectively). In particular we observed a reduction of 24-h systolic blood pressure and “non-dipper” pattern (p < 0.05, respectively) evaluated with ambulatory blood pressure monitoring (ABPM).
Conclusions
Our study confirm the high prevalence of SH in AI, and the unilateral laparoscopic adrenalectomy seemed to have a beneficial effect on some cardiometabolic disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The term of adrenal incidentaloma (AI) covers a wide range of adrenal pathologies unexpectedly found during a work-up performed for an indication unrelated to suspected adrenal disease, with an estimated prevalence between 0.4 and 0.7%, and increases with age [1].
The major clinical concerns in AI are the risk of malignancy and hormone overproduction. Although most of the tumors are non-functioning adrenocortical adenoma, 5–30% of patients with AI show some degree of hypercortisolism without signs or symptoms of overt Cushing’s syndrome (CS) (central obesity, striae rubrae, facies lunaris, prominence of dorsal, supraclavicular fat pads, paroxysmal myopathy, bruising), and it is called “subclinical hypercortisolism” (SH) [2]. Despite the clinical implications remain elusive, various abnormalities such as obesity, arterial hypertension, dyslipidemia, glucose metabolism disorders and bone alterations are frequently observed in these patients [3]. On the other hand, SH is associated with multiple cardiovascular complications similar to CS, but most evidence derive from retrospective studies carried out several homogeneous samples and findings relative to the diagnostic criteria used [4, 5]. At today, the optional treatment of SH due to AI is not yet defined and remains challenge [6, 7]. In particular, the most appropriate treatment for SH associated with benign AI remains controversial and surgery or follow-up with conservation treatment is recommended [2, 3].
This study was designed to evaluate the results of unilateral laparoscopic adrenalectomy in SH patients concerning the main cardiometabolic abnormalities compared to SH patients following conservative treatment.
2 Material and Methods
Between January 2000 to December 2015, from a total of 645 patients with AI, 70 patients were diagnosed with SH. The patients were evaluated at the Specialized Center of Secondary Arterial Hypertension, Department of Internal Medicine and Medical Specialties, University “Sapienza” of Rome, Italy. The diagnosis of AI was based on detection of an adrenal mass by abdominal computed tomography (CT) or magnetic nuclear resonance (RMN) imaging performed for reasons not related to adrenal diseases. SH was defined when two or more of the following hypothalamic-pituitary-adrenal (HPA) axis function tests were abnormal: (1) urinary free cortisol (UFC) level >100 mcg/24 h; (2) serum cortisol levels after 1 mg of dexamethasone suppression test (DST) greater than 1.8 mcg/dl; and (3) morning (8:00 h) plasma ACTH levels <10 pg/ml [5]). ACTH was measured with radioimmunoassay method (RIA), normal limit 10–90 pg/ml, inter/intra-assay CV 8.3/6.2; plasma cortisol was measured with radioimmunoassay method (RIA), normal limit 9.6–26 μg/dl, inter/intra-assay CV 5.5/4.5; urinary free cortisol was measured with radioimmunoassay method (RIA), normal limit 1.37–7.53 μg/24 h, inter/intra-assay CV 5.5/4.5.
In 36 (51.4%) patients with AI and SH we performed an adrenocortical scintigraphy using radiopharmaceuticals 131-I-6β-iodio-methyl-nor-cholesterol, specific for the adrenal cortex. In particular, unilateral uptake on the side of the adrenal mass (concordant up-take) has been associated with unappropriated cortisol secretion [8, 9].
Patients with known malignancies and with other renal disease, such as primary aldosteronism and pheochromocytoma were excluded out after the measurement of 24-h metanephrines urinary excretion, plasma renin activity (PRA) and plasma aldosterone (PAC) in the supine position. Patients with overt clinical signs of hypercortisolism or hyperandrogenism were excluded. All hormone assays were performed with commercially available kits. The study protocol was in accordance to the ethical guidelines of the Declaration of Helsinki, and all participants signed informed consent before the study.
All 70 patients with SH, 26 SH patients with evidence of unilateral hypersecretion of cortisol who accepted the surgical treatment, and 44 patients pharmacologically treated) were followed up for a mean period of 12 months (range 9–15 months). Anthropometric and laboratory data (age, gender, BMI, waist circumference, office clinical systolic (S) and diastolic (D) blood pressure (BP), fasting glucose, cholesterol and triglycerides) were retrieved in all patients at baseline and during follow-up (Tables 1, 2). The metabolic syndrome was defined by ATPIII-NCEP criteria [10].
Ambulatory blood pressure monitoring (ABPM) was performed using the oscillometric technique, which involves a portable lightweight, non-invasive monitor with self-insufflating cuff (Spacelabs Medical, 90207, Issequah, WA, USA). ABPM readings were obtained at 15-min intervals from 6 AM to midnight and at 30-min intervals from midnight to 6 AM. The following ABPM parameters were evaluated: average daytime SBP, average daytime DBP and average daytime heart rate (when awake); average nighttime SBP, average nighttime DBP and average nighttime hear rate (when asleep); average 24-h SBP, average 24-h DBP and average 24-h heart rate. Periods were determined by the subjects’ diaries. The definitions of ”dipper” and “non-dipper” were established where nighttime SBP and DBP decrease was >10% and <10%, respectively. Ambulatory hypertension was defined as 24-h BP >125/80 mmHg [11]. Subjects without a complete 24-h BP measurement (14 diurnals and 7 nocturnal measurements) were excluded from the study.
2.1 Statistical Analysis
Patients results were analyzed in order to assess the impact of the unilateral adrenalectomy on arterial hypertension and metabolic syndrome. All data were entered into an electronic database (Microsoft Excel 2003 for windows, Microsoft Corporation, Redmond, WA, USA). Data analysis were performed with SPSS software (SPSS Inc. Chicago, IL, USA). Comparisons of the different characteristics of the study population were performed with the Χ2 test for the categorical variables and one-way analysis of variance (ANOVA test) for continuous variables. The test was employed to compare in the same patient the hemodynamic, metabolic and biochemical values at the time of the diagnosis and at the last follow-up. The results are expressed as mean ± standard deviation (SD). Two-tailed P values <0.05 were considered significant.
3 Results
A total of 645 patients with AI (283 males and 362 females; mean age 60 ± 10 years) were studied, and 70 (11%) patients with SH (27 males and 43 females; mean age 61 ± 10 years) were diagnosed. Twenty-six (37%) patients (6 males and 20 females; mean age 58.7 ± 7.1 years) with SH underwent unilateral laparoscopic adrenalectomy at the Department of Surgery “P. Valdoni”, Sapienza University of Rome, Italy and the histological findings were consistent with adrenal adenoma.
We have performed adrenalectomy of left side in 15 cases and 11 on right side; mean size of adrenal tumor was 2.4 ± 1.4 cm; mean duration of surgery 79.3 ± 27.8 min; mean hospital stay was 4.1 ± 2.8 days; we have reported only 5 cases of complications (4 with grade I and 1 of grade II) [12]. In all patients (both on right and left) a lateral transabdominal approach was utilized. The adrenal tumor was always removed with minimal dissection of the gland proper tissue, but removing the adrenal gland and the surrounding fibroadipous tissue in order to not cause any injury to the tumor that could lead to cell spread. The adrenal vein was always divided before gland mobilization, by titanium or absorbable clips and ultrasound-energy sealing devices, that was also used to divide adrenal arteries branches and to achieve emostasis. After adrenal gland removal a suction drain was left in the adrenal space for 24–48 h. All patients started oral food intake within 24 h after surgery.
After adrenalectomy, a precautionary steroid therapy with hydrocortisone 100 mg iv, during surgery, and cortisone acetate per os (at weight related doses ranging between 25 and 37.5 mg/day in two subdivided doses during the day), immediately after surgery, was administer. The commonly used cortisone acetate dose was 25 mg/day. In all patients, cortisol secretion was revaluated after 2 months by ACTH stimulation test. The mean duration of the substitution therapy was 5.6 months. No adrenal insufficiency crisis were reported. In all SH patients at diagnosis the arterial hypertension was observed in 82%, obesity in 38.5%, diabetes 30% and metabolic syndrome in 45% (Table 3). In particular, in 26 SH patients before adrenalectomy the arterial hypertension, obesity, diabetes and metabolic syndrome was present in 85, 53.8, 38 and 54%, respectively (Table 3). In these patients after adrenalectomy (mean follow-up 12 months) the arterial hypertension, obesity, diabetes and metabolic syndrome reduced significantly (p < 0.05) to 58.8, 24.5, 23.4 and 23%, respectively (Table 3). Whereas, the 44 patients with SH undergoing to conservative treatment (21 males and 23 females; mean age 63.9 ± 9.9 years) the arterial hypertension, obesity, diabetes and metabolic syndrome, respect to baseline, showed an increase during the follow-up (63.1, 33, 25, 39 vs 72.5, 42.7, 38.5 and 45%, respectively) (Table 3). Moreover, in this group of patients during the follow-up we observed a significant increase of the adrenal mass in diameter (2.25 ± 0.9 vs 2.5 ± 0.9 cm, p < 0.05) evaluated by CT.
In Table 4 we reported all mean values deriving from ABPM in overall SH patients and in SH patients distinguished by surgical or pharmacological treatment, revaluated after follow-up. In the SH patients after adrenalectomy, we have observed a significant reduction of 24-h SBP (133.4 ± 14.9 vs 128.5 ± 12.2 mmHg; p < 0.05). Moreover, in overall SH patients we have observed the lack of nocturnal fall of BP (“non-dipper pattern”) in 60%, and only in the group of SH patients which underwent to adrenalectomy, this prevalence was significantly reduced after follow-up (60 vs 40%; p < 0.05) (Table 3). Interestingly, at baseline the SH patients were treated with a mean of 2.1 anti-hypertensive drugs that significantly reduced (to 1.2; p < 0.05) after adrenalectomy (Table 4).
4 Discussion
SH is a subtle cortisol hypersecretion that causes hypothalamic-pituitary-adrenal (HPA) axis dysfunction without the typical stigmata of CS. It is frequent in patients with AI and found in 5–20% [2]. In our study, conducted in a large cohort of patients with AI, the prevalence of SH was 11%.
There is lack of consensus on the best diagnostic criteria for the evaluation of SH. Available hormonal tests used in the diagnostic work-up of SH are not able to detect with sufficient accuracy the presence of slight hypercortisolism. To date, there are some clinical practice guidelines available [2, 4], all published guidelines agree with the use of 1 mg DST for the screening of hypercortisolism, with the cortisol threshold of 1.8 mcg/dl used to define adequate suppression [5]. Most authors recommended the presence of an abnormal 1 mg DST and at least one of the following: low ACTH levels (<10 pg/ml), higher UFC excretion (over the upper limit of reference values) or a blunted circadian rhythm of cortisol [5, 6]. In our study we have performed these guidelines for the diagnosis of SH in patients with AI, and besides we have performed in much patients the adrenal scintigraphy. Adrenal scintigraphy represents a valid method to detect functionally autonomy of adrenal masses and it has also been suggested that unilateral and/or predominant unilateral uptake is associated with an autonomous cortisol overproduction and can be predictive the recurrence of SH [13]. Consequently, a precocious diagnosis of SH and early removal of the adrenal mass could reduce the onset of clinical complications related to this pathological condition [14].
At today, the optional treatment of SH is not yet defined and remains challenge. Probably most patients should be observed conservatively and surgical treatment should be reserved for patients with poorly controlled cardiometabolic complications [2, 4, 6, 15]. Focusing on patients with SH clarified whether surgery is preferable to a non-surgical approach to improve these cardiometabolic disorders. Our study suggests that unilateral laparoscopic adrenalectomy in patients with SH is associated with improving BP and some components of metabolic syndrome, suggesting that surgery is beneficial. These results are in accord with a recent prospective randomized study [16, 17] that showed in 26 surgically treated patients with SH, an improvement in obesity, hypertension, diabetes and dyslipidemia in 50, 66.7, 62.5 and 37.5% of patients, respectively. Moreover, in another retrospective longitudinal study Chiodini et al. [7] have showed an improvement of BP, glycaemia, and body weight in 25 surgically treated patients with SH, compared to 16 conservatively managed patients. Another important results of our study revealed regard the ABPM (all patients enrolled in the study had good technical quality of ABPM recordings) in these patients. In particular, we showed an attenuation in circadian BP variations in patients with SH and the “non dipper” profile reduced only in patients with SH surgically treated (60 vs 40%; p < 0.05). Our data, regarding the lack of reduction of the nighttime BP in SH patients, are similar to results reported in the literature in several pathologic conditions, such as CS [18], autonomic failure [19], severe renal failure [20], pheochromocytoma [21], hyperthyroidism [22]), hyperparathyroidism [23] and diabetes [24]. These data seem to indicate that the SH in patients with AI may modify the circadian BP profile. We hypothesize that the disturbance in the HPA-axis may affect sympathetic nerve function [25] and also that the sodium-retaining action of cortisol may contribute to the alteration of the circadian BP rhythm in these patients. “Non-dipper” pattern, revealed in our patients with SH, could be an independent cardiovascular risk. Regarding this, it was reported in the literature that the lack of a resting time BP decrease >10% was associated with increased cardiovascular risk [12].
SH is probably not an early stage of CS because development of overt Cushing’s disease rarely occurs in patients with AI and mild hypertension [26]. In a study of Libe et al. [27] none of 12 patients with SH developed overt CS during 25.5 months of follow-up. At the same time, a gradual increase of hormonal activity, even in the absence or recognized criteria for CS can be a sign of progression toward this condition. In our study, none of 44 SH patients, who did not undergo adrenalectomy and followed for mean 12 months, developed clinically symptomatic CS, nevertheless an increase of adrenal mass size was found.
5 Conclusions
In summary, besides confirming the deleterious effects of SH persistence on the risk of cardiometabolic disorders, this study suggests that in AI patients with SH the surgical treatment it is able to significantly reduce the BP, restore the circadian BP rhythm, reduced the numbers of antihypertensive drugs and some components of the metabolic syndrome. Limitation of this study can be considered the retrospective method of evaluation of these patients. Further studies are needed in order to definitively demonstrate the beneficial effects of the unilateral adrenalectomy in adrenal SH and to personalize the treatment of choice in patients with SH due to AI.
References
Kloos RT, Gross MD, Francis IR, Korobkin M, Shapiro B. Incidentally discovered adrenal masses. Endocr Rev. 1995;16:460–84.
Terzolo M, Pia A, Reimondo G. Subclinical Cushing’s syndrome: definition and management. Clin Endocrinol (Oxf). 2012;76:12–8.
Debono M, Newell-Price J. Subclinical hypercortisolism in adrenal incidentaloma. Curr Opin Endocrinol Diabetes Obes. 2015;22:185–92.
Zeiger MA, Thompson GB, Duh QY, Hamrahian AH, Angelos P, Elaraj D, Fishman E, Kharlip J. American Association of Clinical Endocrinologists; American Association of Endocrine Surgeons. Endocr Prac. 2009;15(Suppl):1–20.
Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, Tabarin A, Terzolo M, Tsagarakis S, Dekkers OM. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016;175(2):G1–34.
Iacobone M, Citton M, Scarpa M, Viel G, Boscaro M, Nitti D. Systematic review of surgical treatment of subclinical Cushing’s syndrome. Br J Surg. 2015;102(4):318–30.
Chiodini I, Morelli V, Salcuni AS, Eller-Vainicher C, Torlontano M, Coletti F, Iorio L, Cuttitta A, Ambrosio A, Vicentini L, Pellegrini F, Copetti M, Beck-Peccoz P, Arosio M, Ambrosi B, Trischitta V, Scillitani A. Beneficial metabolic effects of prompt surgical treatment in patients with an adrenal incidentaloma causing biochemical hypercortisolism. J Clin Endocrinol Metab. 2012;95:2736–45.
Dominguez-Gadea L, Diez L, Piedrola-Maroto G, Crespo A. Scintigraphic diagnosis of subclinical Cushing’s syndrome in patients with adrenal incidentalomas. Nucl Med Commun. 1996;17:29–32.
Fagour C, Bardet S, Rohmer V, Arimone Y, Lecomte P, Valli N, Tabarin A. Usefulness of adrenal scintigraphy in the follow-up of adrenocortical incidentalomas: a prospective multicenter study. Eur J Endocrinol. 2009;160:257–64.
Executive Summary of the Third Report of the. National Cholesterol Education Program (NCEP) Expert Panel on Detection; evaluation; and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Ceruti M, Petramala L, Cotesta D, Cerci S, Serra V, Caliumi C, Iorio M, De Toma G, Ciardi A, Vitolo D, Letizia C. Ambulatory blood pressure monitoring in secondary arterial hypertension due to adrenal diseases. J Clin Hypertens (Greenwich). 2006;8:642–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Ricciato MP, Di Donna V, Perotti G, Pontecorvi A, Bellantone R, Corsello SM. The role of adrenal scintigraphy in the diagnosis of subclinical Cushing’s syndrome and the prediction of post-surgical hypoadrenalism. World J Surg. 2014;38:1328–35.
Di Dalmazi G, Vicennati V, Rinaldi E, Morselli-Labate AM, Giampalma E, Mosconi C, Pagotto U, Pasquali R. Progressively increased patterns of subclinical cortisol hypersecretion in adrenal incidentalomas differently predict major metabolic and cardiovascular outcomes: a large cross-sectional study. Eur J Endocrinol. 2012;166:669–77.
Grumbach MM, Biller BM, Braunstein GD, Campbell KK, Carney JA, Godley PA, Harris EL, Lee JK, Oertel YC, Posner MC, Schlechte JA, Wieand HS. Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann Intern Med. 2003;138:424–9.
Toniato A, Erante-Boschin I, Opocher G, Pelizzo MR, Schiavi F, Ballotta E. Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized study. Ann Surg. 2009;249:388–91.
Perogamvros I, Vassiliadi DA, Karapanou O, Botoula E, Tzanela M, Tsagarakis S. Biochemical and clinical benefits of unilateral adrenalectomy in patients with subclinical hypercortisolism and bilateral adrenal incidentalomas. Eur J Endocrinol. 2015;173:719–25.
Rebellato A, Grillo A, Dassie F, Sonino N, Maffei P, Martini C, Paoletta A, Fabris B, Carretta R, Fallo F. Ambulatory blood pressure monitoring-derived short-term blood pressure variability is increased in Cushing’s syndrome. Endocrine. 2014;47:557–63.
Liu M, Takahashi H, Morita Y, Maruyama S, Mizuno M, Yuzawa Y, Watanabe M, Toriyama T, Kawahara H, Matsuo S. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction in haemodialysis patients. Nephrol Dial Transplant. 2003;18:563–9.
Wu Z, Wu X, Xing F, Zhou S, Luo B, Wang L. Blood pressure characteristics in moderate to severe renal insufficiency. Kidney Blood Press Res. 2015;40:478–89.
Zinnamosca L, Petramala L, Cotesta D, Marinelli C, Schina M, Cianci R, Giustini S, Sciomer S, Anastasi E, Calvieri S, De Toma G, Letizia C. Neurofibromatosis type 1 (NF1) and pheochromocytoma: prevalence; clinical and cardiovascular aspects. Arch Dermatol Res. 2011;303:317–25.
Iglesias P, Acosta M, Sánchez R, Fernández-Reyes MJ, Mon C, Díez JJ. Ambulatory blood pressure monitoring in patients with hyperthyroidism before and after control of thyroid function. Clin Endocrinol (Oxf). 2015;63:66–72.
Letizia C, Ferrari P, Cotesta D, Caliumi C, Cianci R, Cerci S, Petramala L, Celi M, Minisola S, D’Erasmo E, Mazzuoli GF. Ambulatory monitoring of blood pressure (AMBP) in patients with primary hyperparathyroidism. J Hum Hypertens. 2005;19:901–6.
Hermida RC, Moyá A, Ayala DE. Ambulatory blood pressure monitoring in diabetes for the assessment and control of vascular risk. Endocrinol Nutr. 2015;62:400–10.
Hawkins UA, Gomez-Sanchez EP, Gomez-Sanchez CM, Gomez-Sanchez CE. The ubiquitous mineralocorticoid receptor: clinical implications. Curr Hypertens Rep. 2012;14:573–80.
Barzon L, Fallo F, Sonino N. Development of overt Cushing’s syndrome in patients with adrenal incidentaloma. Eur J Endocrinol. 2002;146:61–6.
Libè R, Dall’Asta C, Barbetta L, Baccarelli A, Beck-Peccoz P, Ambrosi B. Long-term follow-up study of patients with adrenal incidentalomas. Eur J Endocrinol. 2002;147:489–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Petramala, L., Cavallaro, G., Galassi, M. et al. Clinical Benefits of Unilateral Adrenalectomy in Patients with Subclinical Hypercortisolism Due to Adrenal Incidentaloma: Results from a Single Center. High Blood Press Cardiovasc Prev 24, 69–75 (2017). https://doi.org/10.1007/s40292-017-0182-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-017-0182-7