Abstract
Mineralocorticoid receptors (MR) exist in many tissues, in which they mediate diverse functions crucial to normal physiology, including tissue repair and electrolyte and fluid homeostasis. However, inappropriate activation of MR within these tissues, and especially in the brain, causes hypertension and pathological vascular, cardiac, and renal remodeling. MR binds aldosterone, cortisol and corticosterone with equal affinity. In aldosterone-target cells, co-expression with the 11β-hydroxysteroid dehydrogenase 2 (HSD2) allows aldosterone specifically to activate MR. Aldosterone levels are excessive in primary aldosteronism, but in conditions with increased oxidative stress, like CHF, obesity and diabetes, MR may also be inappropriately activated by glucocorticoids. Unlike thiazide diuretics, MR antagonists are diuretics that do not cause insulin resistance. Addition of MR antagonists to standard treatment for hypertension and cardiac or renal disease decreases end-organ pathology and sympathetic nerve activation (SNA), and increases quality of life indices.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The search for a sodium-retaining hormone believed to have a role in edematous conditions [1] ultimately resulted in the isolation of aldosterone (electrocortin) in 1953 by Simpson and Tait in collaboration with the Swiss chemists Wettstein and Reichstein [2]; this discovery was followed very soon thereafter with the description of the syndrome of primary aldosteronism [3, 4]. For the next two decades, the physiological and biochemical actions of aldosterone, and the less expensive and more easily synthesized mineralocorticoid deoxycorticosterone acetate (DOCA), were characterized. In 1972 it was recognized that they acted through a steroid receptor called the mineralocorticoid receptor (MR) [5]. An effective mineralocorticoid receptor antagonist, spironolactone, had been introduced in the early 1960’s before the existence of the MR was certain [6]. The MR was cloned in 1987 by the group of Ronald Evans, introducing an era of greater understanding of MR signaling in health and disease [7]. Our purpose is to review recent developments in regards to the clinical implications of the MR, as well as to provide a future prospectus of novel roles of this ever-evolving system.
Background
The MR is encoded by the NR3C2 gene localized in the chromosome 4 q31.1 region [8]. Like other members of the nuclear receptor superfamily, the MR acts as a ligand-activated transcription factor; its biological actions are mediated by the proteins whose synthesis it regulates. It has three major functional domains: an N-terminal domain (NTD), a central DNA-binding domain (DBD), and a C-terminal ligand-binding domain (LBD) linked to the others by a hinge region. There are many co-activators and co-repressors of MR gene transactivation [8] that differ between each cell type; thus, some MR-mediated functions are specific for different types of cells and may be influenced by physiological conditions that alter co-regulator expression [8]. Ultimately, MR-mediated actions are the result of a multitude of interactions, involving both transcriptional and posttranscriptional mechanisms [8].
Though most of the early studies of MR function focused on transporting epithelia, such as in the distal convoluted tubule and collecting duct of the kidney, salivary gland, distal colon, airway epithelia, etc. [9–11], the MR is expressed and acts in a wider variety of cells [8], including non-epithelial tissues like the brain, heart, arteries, ovaries, pancreas and others [12–17]. Early studies in transport epithelia suggested that the MR bound aldosterone specifically [5], but it was subsequently found that the MR binds with similar affinity to the primary glucocorticoids, cortisol, and corticosterone (in some species) [18]. These steroids circulate at concentrations 1,000 (total plasma) and 100 (free steroid) times the concentration of aldosterone in plasma [19, 20]. Specificity of the MR for aldosterone in transporting epithelia was found to be due to the co-expression of an enzyme, 11β-hydroxysteroid dehydrogenase 2 (11β-HSD2), which metabolizes the active glucocorticoids cortisol and corticosterone to the inactive metabolites cortisone and 11-dehydrocorticosterone [21–23]. There are some doubts about whether this protective mechanism is sufficient to completely explain the MR selectivity for aldosterone, and it is proposed that the alteration in redox potential produced by the actions of the enzyme may alter the transcriptional activity of the MR [19]. In tissues that do not express the 11β-HSD2, such as the cardiomyocyte and specific neurons in the brain [24–26], cortisol or corticosterone occupy the receptor almost entirely.
In addition to its effects regulating specific gene transcription, the MR mediates rapid non-genomic effects that do not involve gene transcription, though they may alter gene expression secondarily [27–29]. Recently GPR30, a 7 trans-membrane G-protein-associated receptor also called GPER, was found to mediate some of the non-genomic actions of aldosterone and perhaps to represent a membrane-bound MR [30]. This receptor is also mostly blocked by the MR blocker spironolactone [30]. As inappropriate MR activation is associated with cardiovascular, cerebrovascular, and renal damage, MR antagonists may ameliorate the outcome of these disorders. Whether some of the benefits of MR antagonists in these conditions are due also to direct effect on GPR30 signaling or to interruption of an interaction of the MR with GPR30 or GPR30-initiated events is not clear.
Aldosterone and the Heart
Seventy years ago, Hans Selye first demonstrated that the administration of deoxycorticosterone with increased salt intake was associated with hypertension, cardiac hypertrophy, and heart failure [31]. Many decades later, K.T. Weber’s group demonstrated that the cardiac hypertrophy and fibrosis in rats produced by high aldosterone plus salt is associated with fibroblast proliferation, cardiomyocyte hypertrophy, and increased accumulation of collagen types I and II [32, 33], and is prevented by the concurrent administration of the MR antagonist spironolactone [34]. Chronic administration of aldosterone to rats on a high-sodium diet results in early macrophage infiltration of the myocardium and vasculature with increased expression of inflammatory markers, followed a few weeks later with vascular and cardiac remodeling and fibrosis [35, 36]. This cardiac response to aldosterone-salt is a direct effect on the heart independent of blood pressure [37–39].
Both angiotensin II and aldosterone are increased in congestive heart failure (CHF), and the persistent elevation of both has clearly deleterious consequences on cardiac and vascular structures. Treatment of patients with CHF with a converting enzyme inhibitors (ACEi) became a major modality of treatment, as decreasing angiotensin II would decrease the direct effect on the heart and vessels, as well as the indirect effect through reduction in aldosterone levels. However, aldosterone escapes from the inhibitory effects of ACEi and angiotensin II receptor blockers (ARB) after chronic treatment in CHF and returns to or above its initial baseline [40]. Given the association between plasma aldosterone levels and mortality in patients with CHF and left ventricular hypertrophy (LVH) [41, 42], and the knowledge that there is an aldosterone escape in patients with CHF treated with ACEi, the Randomized Aldactone Evaluation (RALES) trial was designed to test the effect of the addition of mineralocorticoid receptor blockade with spironolactone to standard treatment of patients with CHF [43]. The RALES trial tested the hypothesis that daily treatment with ~25 mg of spironolactone would significantly reduce the risk of death from all causes among patients who had severe heart failure as a result of systolic left ventricular dysfunction and who were receiving standard therapy, including an ACE inhibitor [43]. The primary end point of the study was death from any cause, and the secondary end points included death from cardiac causes, hospitalization for cardiac causes, the combined incidence of death from cardiac causes or hospitalization for cardiac causes, and a change in the NYHA class [43]. The trial was stopped early because of a significant, 30 % reduction in the risk of death in the spironolactone group, as well as a 31 % reduction in the risk of death from cardiac causes and 30 % reduction in the risk of hospitalization for cardiac causes among patients in the spironolactone group.
These results led to a similar clinical trial of the effect of mineralocorticoid receptor blockade in patients with acute myocardial infarction complicated by left ventricular dysfunction and heart failure, the Eplerenone Post-AMI Heart Failure Efficacy and Survival (EPHESUS) trial [44]. Eplerenone was used rather than spironolactone because it does not inhibit the androgen receptor, and because it was still on patent at the time. The primary endpoints of the EPHESUS trial were time to death from any cause, time to death from cardiovascular causes, and first hospitalization for a cardiovascular event, including heart failure, recurrent MI, stroke, or ventricular arrhythmia. The secondary end points were death from cardiovascular causes, death from any cause, or any hospitalization. There were significant reductions in overall mortality, rate of death from cardiovascular causes, and hospitalization for cardiovascular events among those receiving the MR antagonist.
As inferred from laboratory animal studies, the RALES and EPHESUS trials confirmed the crucial role of the MR in the pathogenesis of heart disease. The remaining question was whether MR antagonists could improve survival among patients with chronic systolic heart failure and mild symptoms. The Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure (EMPHASIS-HF) trial was designed to address this issue in patients with systolic heart failure and mild symptoms (NYHA II) [45••]. The primary outcome was death from cardiovascular causes or a first hospitalization for heart failure. There were significant reductions in the rate of death from a cardiovascular cause, hospitalization for heart failure, and rates of death from any cause.
These clinical trials confirmed the involvement of the mineralocorticoid receptor in CHF originating from both ischemic and non-ischemic causes, and also demonstrated that these effects are unrelated to changes in potassium [46•]. The latter finding was crucial. Serum potassium is generally lower in CHF, so it was proposed by some that the ameliorative effect of spironolactone in the RALES trial was partly due to increased potassium, which decreased cardiac arrhythmias. While excessive MR inhibition has a risk of hyperkalemia through decreased potassium secretion, hyperkalemia was never a problem in the studies.
In the 4E-Left Ventricular Hypertrophy Study, the MR antagonist eplerenone was compared with the angiotensin converting inhibitor enalapril, and their combination in patients with hypertension and LVH. Eplerenone had comparable effects to enalapril in decreasing BP and LVH; the combination was more effective than each individually [47]. As the evidence for the value of MR antagonists in the management of cardiac disease accrues, it is essential that the clinician recognize that indiscriminate use of these agents could lead to severe hyperkalemia, so patients should be properly monitored [48]. New trials of MR antagonists are currently being conducted in other subgroups with heart failure, including the TOPCAT study in patients with preserved ejection fraction congestive heart failure [49] and the ALBATROSS study to assess the effects of MR blockade early after myocardial infarction [50], and the results should be available soon.
As described above, the MR has equal affinity for cortisol and aldosterone. The expression of 11β-hydroxysteroid dehydrogenase in the heart is very low and appears to be limited to vessels. Thus, it is unclear how aldosterone can have a deleterious effect in the heart when MR in the cardiomyocytes are occupied by the far more abundant glucocorticoid cortisol, with aldosterone binding only a small portion of the MR [51]. It has been hypothesized that under basal conditions cardiomyocyte MR occupied by the glucocorticoids are inactive, and that changes in the NAD/NADH ratio induced by oxidative stress cause the MR to be activated by glucocorticoids [51, 52]. It may also be that oxidative stress causes a change in MR conformation and/or in co-activators that allows the MR to be activated by glucocorticoids, aldosterone or even independently of ligand and causes the increased and ultimately excessive transcription of genes normally associated with repair [32, 33, 35].
Kidney
The most well understood effects of MR activation by aldosterone are in the kidney, where they result in the vectorial transfer of sodium, potassium, and protons essential for the maintenance of sodium, potassium, and water homeostasis. Excessive action of aldosterone in the kidney results in increased reabsorption of sodium, loss of potassium and protons, and, in combination with actions at other levels, hypertension and target organ damage including in the kidney. Kidney damage due to excessive MR activation goes beyond the elevation of blood pressure [36] and involves direct and indirect effects, including those mediated by MR within the kidney, the central nervous sytem, and immune system [53–55].
Abnormal activation of the renin-angiotensin system participates in the progression of kidney disease, and most studies have focused on the deleterious effects of angiotensin II, leading to the extensive use of ACEi or angiotensin receptor blockers (ARB) as first line therapy for patients with renal disease. Studies by Greene demonstrated that the protective effects of ACEi or ARB in a renal ablation model of renal disease were reversed by administration of aldosterone [56]. Aldosterone, in the presence of excessive sodium intake, affects almost all the renal parenchyma, including the vasculature, glomeruli and the tubulointerstitium [57]. The renal vasculature is directly affected by aldosterone with the induction of inflammation, fibrosis, and impaired vascular reactivity; MR in myeloid cells appear to play a significant role in this process [39, 58, 59]. In addition, aldosterone-salt treated animals develop proteinuria and severe glomerular injury [60•] due to dysfunction of podocytes with decreased expression of nephrin and podocin, the main components of the slit diaphragm in podocytes, and increased expression of desmin, a marker for podocyte damage. These changes are almost completely prevented by MR antagonists [61]. Aldosterone also increases the proliferation of mesangial cells, which contributes to glomerular damage and proteinuria [62].
Guo et al. demonstrated reduced renal injury with MR blockade in studies of rodents with both type 1 and type 2 diabetes mellitus [63]. MR blockade improved albuminuria, glomerular hypertrophy, early mesangial matrix expansion, and glomerular inflammatory infiltrates. The overall effect was reduced vascular injury, inflammation, and renal fibrosis. Furthermore, markers of tubulointerstitial disease were reduced by MR blockade [63]. Similar findings have also been demonstrated in human studies. Aldosterone antagonists reduce renal injury and albuminuria in persons with diabetes mellitus and nephropathy [64•, 65, 66]. In patients with type 2 diabetes and nephropathy, albuminuria was reduced by 33 % in the MR antagonist group [66], and the fractional clearance of albumin was reduced by 40 %. Although both the systolic and diastolic blood pressures were significantly lower in the MR antagonist treated group, the improvement in albuminuria was independent of the blood pressure lowering effects [64•, 66]. This observation demonstrates the non-hemodynamic actions of MR blockade and, consistent with studies in experimental models, the results suggest a reduction of pro-sclerotic growth factors.
Current recommendations for the treatment of hypertensive diabetics include the use of ACEi or ARB to block the renin-angiotensin system; however, in diabetics with proteinuria incompletely corrected with an ACEi, the addition of spironolactone has clear additive effects on decreasing protein excretion, with an additional benefit of reducing cardiac hypertrophy [67]. The potential for the induction of hyperkalemia, especially in diabetic patients on an ACEi is real, though uncommon. These patients benefit from the use of MR antagonists as long as their potassium levels are monitored. Spironolactone administration to patients with mild to moderate renal failure had a very low incidence of serious hyperkalemia (<1 %) and mild intermittent hyperkalemia in 11 of 115 patients [68].
MR in Adipose Tissue
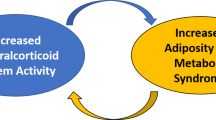
MR are expressed in preadipocytes, including those that become brown fat, and are crucial in the differentiation into adipocytes and in mitochondrial function [69, 70]. Aldosterone is also increased in obesity and the metabolic syndrome. The cause of this increase is uncertain, but there is evidence for an adipocyte factor that stimulates aldosterone synthesis by the adrenal gland [71, 72]. While the identity of this factor is unknown, the adiponectin receptor is expressed in the human adrenal cortex, as well as in aldosterone-producing adenomas [73]. There is also recent evidence that adipose tissue synthesizes aldosterone directly [74]. In in vitro models, aldosterone decreases insulin-induced glucose uptake and the expression of uncoupling protein-1 in brown fat, and increases synthesis of the adipokines leptin and monocyte chemoattractant protein-1 [75]. MR antagonists reverse obesity-related changes in expression of adiponectin, peroxisome proliferator-activated receptor-gamma, and proinflammatory adipokines in experimental animals and human adipocytes in culture [76, 77].
MR in the Brain
Mineralocorticoid receptors are highly expressed in specific neurons in several regions of the CNS, most prominently the hippocampus, discrete nuclei of the hypothalamus, amygdala, nucleus tractus solitarius (NTS), cerebral cortex, and Purkinje cells of the cerebellum [14, 17, 78, 79]. Little is known about the function of MR in most of these neurons, particularly those of the cerebral cortex and cerebellum. Aldosterone target neurons of the NTS coexpress the 11β-hydroxysteroid dehydrogenase 2 that confers specificity to the MR for aldosterone [80]. These MR and those in the amygdala are involved in the regulation of sodium appetite [81, 82].
MR in the paraventricular nucleus of the hypothalamus (PVN) are associated with the modulation of the blood pressure and renal function, primarily by increasing sympathetic output to the vessels, heart, and kidney [79]. As in experimental mineralocorticoid excess hypertension, inappropriately high aldosterone levels in humans increases sympathetic drive. Some of these studies were done in primary aldosteronism patients before and after the removal of the aldosterone-producing adenoma [83]. In normal human volunteers, infusion of aldosterone to induce a 4-fold increase basal plasma aldosterone concentration, (which is within the pathophysiologic range) resulted in increased muscle sympathetic nerve activity (SNA) and impaired baroreflex responses [84].
In a comparison between the effects of chlorthalidone and spironolactone on hypertension, SNA, and insulin resistance, the thiazide diuretic consistently increased sympathetic nerve activity in non-diabetic hypertensive patients, while the MR antagonist similarly decreased the blood pressure but had no effect on the SNA. After 3 months of treatment, the thiazide diuretic increased insulin resistance; spironolactone had no effect [85]. In another study, SNA was measured in hypertensive patients before initiating treatment with chlorthalidone, 12 weeks later, then 12 weeks after either the ARB irbesartan or spironolactone was added to the chlorthalidone in a randomized cross-over trial. Chlorthalidone effectively lowered the BP, but at the expense of a significant and persistent increase in SNA and insulin resistance. Spironolactone, but not irbesartan, reversed both the increase in SNA and insulin resistance associated with the chlorthalidone [86•].
The highest concentration of MR anywhere in the body is in the hippocampus, where it is thought to be bound primarily by glucocorticoids and is essential for normal neuronal function, including serotonergic metabolism [19, 87]. The hippocampus is the major integrative center for the formation of memories, learning, cognition, and coping with stress. Derangements in hippocampal function are implicated in major depression and posttraumatic stress disorder. Primary aldosteronism is associated with depression and a decline in cognitive abilities. Successful treatment is reported to improve quality of life, cognition, and depression in these patients [88–91]. Given the prevalence of primary aldosteronism, between 4-12 % of persons with hypertension [92], the affective aspect of inappropriate MR activation in the brain may be significant and underappreciated.
In addition to their crucial role in electrolyte and fluid homeostasis, MR also mediate tissue repair processes as well as trophic functions in the brain [93], and the interplay between MR and glucocorticoid receptors (GR) complicates these processes. GR are expressed in most cells, including those that express MR, although GR has about 1/10 the affinity for aldosterone as for cortisol. In cells that do not express 11β-HSD2, MR are primarily occupied by cortisol, even at the nadir of the circadian cycle, while GR are occupied at the zenith of the cycle. Conditions of stress and uncontrolled diabetes are associated with chronically elevated glucocorticoid levels and a significant reduction in cognitive and hippocampal neuron function in rats. Aldosterone, but not corticosterone, restored normal neuronal function in a diabetic rat model [94]. A study in humans who were receiving antidepressant therapy and were treated with either spironolactone or the potent mineralocorticoid fludrocortisone identified a group of patients with an MR polymorphism in whom the mineralocorticoid enhanced and accelerated the effect of the SSRI antidepressant, while decreasing cortisol values. In non-responders, fludrocortisone had no effect on cortisol levels [95]. It is now clear that, while limited, neurogenesis, differentiation, and migration occur in the adult human [96], and that MR are critically important in these processes [97].
Mineralocorticoid Receptor Antagonists, Present and Future
Two generations of MR antagonists are currently available. The first generation includes spironolactone and canrenone (a metabolite available in Europe). These are potent steroidal compounds with multiple active metabolites, some of which are concentrated in the kidney and have long half-lives. Unfortunately they are also antagonists of the androgen receptor and agonists of the progesterone receptor, although these effects can be useful for the treatment of PCOS. Eplerenone, a relatively new steroidal MR antagonist, is less potent, has no active metabolites, and has a short half-life, but it is more selective for the MR, and is also concentrated in the kidney. Currently there are clinical trials of third- and fourth-generation MR antagonists that are non-steroidal, potent, selective for the MR, and have a more balanced tissue distribution with significant concentration in the cardiovascular system, as well as the kidney [98•]. The hope that these will have a lower risk for excessive potassium retention remains to be seen.
Conclusions
MR are crucial to normal physiology of many systems, including repair and trophic functions in neurons. However, when inappropriately activated, they are associated with hypertension and pathological remodeling of vessels, heart, and kidney, mediated both by MR within these tissues and by MR in the brain leading to unremitting increased sympathetic nerve activation and decreased baroreceptor sensitivity. Aldosterone itself may be high in relation to need in some conditions, particularly primary aldosteronism and CHF, but in other conditions of chronic increases in oxidative stress, the MR appears to be activated primarily by glucocorticoids. Clinical trials demonstrate that the addition of MR antagonists to standard treatment for hypertension, cardiac, and renal disease decreases end-organ pathology and SNA, and increases quality of life indices. A particularly germane issue in the battle against metabolic syndrome and diabetes is that MR antagonists act as diuretics without causing the insulin resistance associated with thiazide diuretics and can counteract the glycemic derangements caused by the thiazides. The potential for hyperkalemia should not be dismissed; however, judicious use of mineralocorticoid receptor antagonists can be an important adjunct to treatment regimens for hypertension, heart, and kidney disease, particularly in the obese and diabetic patient.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Deming QB, Luetscher Jr JA. Increased sodium-retaining corticoid excretion in edema, with some observations on the effects of cortisone in nephrosis. J Clin Invest. 1950;29:808.
Simpson SA, Tait JF, Wettstein A, et al. Konstitution des aldosterons, des neuen mineralocorticoids. Experientia. 1953;10:132–3.
Conn JW. Primary aldosteronism, a new clinical syndrome. J Lab Clin Med. 1955;45:3–7.
Funder JW. Aldosterone and mineralocorticoid receptors: a personal reflection. Mol Cell Endocrinol. 2012;350:146–50.
Funder JW, Feldman D, Edelman I. Specific Aldosterone binding in rat kidney and parotid. J Steroid Biochem. 1972;3:209–18.
Hood Jr WG, Hill Jr R, Pittman Jr JA, Farmer Jr TA. Studies on the metabolic effects of spironolactone in man. Ann N Y Acad Sci. 1960;88:864–80.
Arriza JW, Weinberger C, Cerelli G, et al. Cloning of human mineralocorticoid receptor complementary DNA: structural and functional kinship with the glucocorticoid receptor. Science. 1987;237:268–75.
Viengchareun S, Le Menuet D, Martinerie L, et al. The mineralocorticoid receptor: insights into its molecular and (patho)physiological biology. Nucl Recept Signal. 2007;5:e012.
Farman N, Bonvalet JP. Aldosterone binding in isolated tubules. III. Autoradiography along the rat nephron. Am J Physiol. 1983;245:F606–614.
Farman N, Oblin ME, Lombes M, et al. Immunolocalization of gluco- and mineralocorticoid receptors in rabbit kidney. Am J Physiol. 1991;260:C226–233.
Funder JW. Mineralocorticoid receptors: distribution and activation. Heart Fail Rev. 2005;10:15–22.
Reul JMH, De Kloet ER. Two receptor systems for coticosterone in rat brain: microdistribution and differential occupation. Endocrinology. 1985;117:2505–11.
De Kloet ER, Vreugdenhil E, Oitzl MS, Joels M. Brain corticosteroid receptor balance in health and disease. Endocr Rev. 1998;19:269–301.
Gomez-Sanchez CE, de Rodriguez AF, Romero DG, et al. Development of a panel of monoclonal antibodies against the mineralocorticoid receptor. Endocrinology. 2006;147:1343–8.
Gomez-Sanchez EP. Brain mineralocorticoid receptors: orchestrators of hypertension and end-organ disease. Curr Opin Nephrol Hypertens. 2004;13:191–6.
Gomez-Sanchez EP, Gomez-Sanchez MT, de Rodriguez AF, et al. Immunohistochemical Demonstration of the Mineralocorticoid Receptor, 11{beta}-Hydroxysteroid Dehydrogenase-1 and -2, and Hexose-6-phosphate Dehydrogenase in Rat Ovary. J Histochem Cytochem. 2009;57:633–41.
Gomez-Sanchez CE, Warden M, Gomez-Sanchez MT, et al. Diverse immunostaining patterns of mineralocorticoid receptor monoclonal antibodies. Steroids. 2011;76:1541–5.
De Kloet ER, Versteeg DHG, Kovacs GL. Aldosterone blocks the response to corticosterone in the raphe-hippocampal serotonin system. Brain Res. 1983;264:323–7.
Funder J, Myles K. Exclusion of corticosterone from epithelial mineralocorticoid receptors is insufficient for selectivity of aldosterone action: in vivo binding studies. Endocrinology. 1996;137:5264–8.
Krozowski ZS, Funder JW. Renal mineralocorticoid receptors and hippocampal corticosterone-binding species have identical intrinsic steroid specificity. Proc Natl Acad Sci U S A. 1983;80:6056–60.
Funder JW, Pearce PT, Smith R, Smith AI. Mineralocorticoid action: target tissue specificity is enzyme, not receptor, mediated. Science. 1988;242:583–5.
Edwards CRW, Burt D, McIntyre MA, et al. Localisation of 11b-hydroxysteroid dehydrogenase-tissue specific protector of the mineralocorticoid receptor. Lancet. 1988;ii:986–9.
Stewart PM, Wallace AM, Valentino R, et al. Mineralocorticoid activity of liquorice: 11-Beta-hydroxysteroid dehydrogenase deficiency comes of age. Lancet. 1987;ii:821–4.
van Leeuwen N, Bellingrath S, de Kloet ER, et al. Human mineralocorticoid receptor (MR) gene haplotypes modulate MR expression and transactivation: implication for the stress response. Psychoneuroendocrinology. 2011;36:699–709.
Joels M, Karst H, DeRijk R, de Kloet ER. The coming out of the brain mineralocorticoid receptor. Trends Neurosci. 2008;31:1–7.
Gomez-Sanchez EP. The mammalian mineralocorticoid receptor: tying down a promiscuous receptor. Exp Physiol. 2010;95:13–8.
Grossmann C, Benesic A, Krug AW, et al. Human mineralocorticoid receptor expression renders cells responsive for nongenotropic aldosterone actions. Mol Endocrinol. 2005;19:1697–710.
Funder JW. The nongenomic actions of aldosterone. Endocr Rev. 2005;26:313–21.
Groeneweg FL, Karst H, de Kloet ER, Joels M. Mineralocorticoid and glucocorticoid receptors at the neuronal membrane, regulators of nongenomic corticosteroid signalling. Mol Cell Endocrinol. 2011.
Gros R, Ding Q, Sklar LA, et al. GPR30 expression is required for the mineralocorticoid receptor-independent rapid vascular effects of aldosterone. Hypertension. 2011;57:442–51.
Selye H, Hall CE. Production of nephrosclerosis and cardiac hypertrophy in the rat by desoxycorticosterone acetate overdosage. Am Heart J. 1943;27:338–44.
Weber KT, Brilla CG, Janicki JS. Myocardial fibrosis: functional significance and regulatory factors. Cardiovasc Res. 1993;27:341–8.
Robert V, Van Thiem N, Cheav SL, et al. Increased cardiac types I and III collagen mRNAs in aldosterone-salt hypertension. Hypertension. 1994;24:30–6.
Brilla CG, Matsubara LS, Weber KT. Antifibrotic effects of spironolactone in preventing myocardial fibrosis in systemic arterial hypertension. Am J Card. 1993;71:12A–6A.
Rocha R, Rudolph AE, Frierdich GE, et al. Aldosterone induces a vascular inflammatory phenotype in the rat heart. Am J Physiol Heart Circ Physiol. 2002;283:H1802–1810.
Rocha R, Stier CT, Kifor I, et al. Aldosterone: a mediator of myocardial necrosis and renal arteriopathy. Endocrinology. 2000;141:3871–8.
Young M, Fullerton M, Dilley R, Funder J. Mineralocorticoids, hypertension, and cardiac fibrosis. J Clin Invest. 1994;93:2578–83.
Gomez-Sanchez EP. Mineralocorticoid modulation of central control of blood pressure. Steroids. 1995;60:69–72.
Young MJ, Rickard AJ. Mechanisms of mineralocorticoid salt-induced hypertension and cardiac fibrosis. Mol Cell Endocrinol. 2012;350:248–55.
Pitt B. "Escape" of aldosterone production in patients with left ventricular dysfunction treated with an angiotensin converting enzyme inhibitor: implications for therapy. Cardiovasc Drugs Ther. 1995;9:145–9.
Swedberg K, Eneroth P, Kjekshus J, Wilhelmsen L. Hormones regulating cardiovascular function in patients with severe congestive heart failure and their relation to mortality. CONSENSUS Trial Study Group. Circulation. 1990;82:1730–6.
Rossi GP, Sacchetto A, Pavan E, et al. Remodeling of the left ventricle in primary aldosteronism due to Conn's adenoma. Circulation. 1997;95:1471–8.
Pitt B, Zannad F, Cody R, et al. The effect of spironolactone on mobidity and mortality in patients with severe heart failure. Randomized Aldactone evaluation study investigators. N Engl J Med. 1999;341:709–17.
Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309–21.
•• Zannad F, McMurray JJ, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11–21. This paper extended the benefit of the use of mineralocorticoid receptor antagonists in patients with mild systolic congestive heart failure.
• Rossignol P, Menard J, Fay R, et al. Eplerenone survival benefits in heart failure patients post-myocardial infarction are independent from its diuretic and potassium-sparing effects. Insights from an EPHESUS (Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study) substudy. J Am Coll Cardiol. 2011;58:1958–66. This study clarified that the beneficial effects of mineralocorticoid receptor antagonists were more direct rather than just as a potassium-sparing diuretic.
Pitt B, Reichek N, Willenbrock R, et al. Effects of eplerenone, enalapril, and eplerenone/enalapril in patients with essential hypertension and left ventricular hypertrophy: the 4E-left ventricular hypertrophy study. Circulation. 2003;108:1831–8.
Juurlink DN, Mamdani MM, Lee DS, et al. Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N Engl J Med. 2004;351:543–51.
Desai AS, Lewis EF, Li R, et al. Rationale and design of the treatment of preserved cardiac function heart failure with an aldosterone antagonist trial: a randomized, controlled study of spironolactone in patients with symptomatic heart failure and preserved ejection fraction. Am Heart J. 2011;162:966–72. e910.
Beygui F, Vicaut E, Ecollan P, et al. Rationale for an early aldosterone blockade in acute myocardial infarction and design of the ALBATROSS trial. Am Heart J. 2010;160:642–8.
Messaoudi S, Azibani F, Delcayre C, Jaisser F. Aldosterone, mineralocorticoid receptor, and heart failure. Mol Cell Endocrinol. 2012;350:266–72.
Mihailidou AS, Le Loan TY, Mardini M, Funder JW. Glucocorticoids activate cardiac mineralocorticoid receptors during experimental myocardial infarction. Hypertension. 2009;54:1306–12.
Herrada AA, Campino C, Amador CA, et al. Aldosterone as a modulator of immunity: implications in the organ damage. J Hypertens. 2011;29:1684–92.
Rahmouni K, Barthelmebs M, Grima M, et al. Involvement of brain mineralocorticoid receptor in salt-enhanced hypertension in spontaneously hypertensive rats. Hypertension. 2001;38:902–6.
Young MJ, Morgan J, Brolin K, et al. Activation of mineralocorticoid receptors by exogenous glucocorticoids and the development of cardiovascular inflammatory responses in adrenalectomized rats. Endocrinology. 2010;151:2622–8.
Greene EL, Kren S, Hostetter TH. Role of aldosterone in the remnant kidney model in the rat. J Clin Invest. 1996;98:1063–8.
Blasi ER, Rocha R, Rudolph AE, et al. Aldosterone/salt induces renal inflammation and fibrosis in hypertensive rats. Kidney Int. 2003;63:1791–800.
Bienvenu LA, Morgan J, Rickard AJ, et al. Macrophage mineralocorticoid receptor signaling plays a key role in aldosterone-independent cardiac fibrosis. Endocrinology. 2012;153:3416–25.
Rickard AJ, Morgan J, Tesch G, et al. Deletion of mineralocorticoid receptors from macrophages protects against deoxycorticosterone/salt-induced cardiac fibrosis and increased blood pressure. Hypertension. 2009;54:537–43.
• Shibata S, Fujita T. Mineralocorticoid receptors in the pathophysiology of chronic kidney diseases and the metabolic syndrome. Mol Cell Endocrinol. 2012;350:273–80. This is an excellent review of the mechanisms and clinical importance of mineralocorticoid receptor antagonists in kidney diseases, including diabetes and the metabolic syndrome.
Shibata H, Itoh H. Mineralocorticoid receptor-associated hypertension and its organ damage: clinical relevance for resistant hypertension. Am J Hypertens. 2012.
Nishiyama A, Yao L, Fan Y, et al. Involvement of aldosterone and mineralocorticoid receptors in rat mesangial cell proliferation and deformability. Hypertension. 2005;45:710–6.
Guo C, Martinez-Vasquez D, Mendez GP, et al. Mineralocorticoid receptor antagonist reduces renal injury in rodent models of types 1 and 2 diabetes mellitus. Endocrinology. 2006;147:5363–73.
• Nielsen SE, Persson F, Frandsen E, et al. Spironolactone diminishes urinary albumin excretion in patients with type 1 diabetes and microalbuminuria: a randomized placebo-controlled crossover study. Diabet Med. 2012. This study demonstrates the effects of spironolactone improving the excretion of markers of renal dysfunction.
Schjoedt KJ, Rossing K, Juhl TR, et al. Beneficial impact of spironolactone on nephrotic range albuminuria in diabetic nephropathy. Kidney Int. 2006;70:536–42.
Rossing K, Schjoedt KJ, Smidt UM, et al. Beneficial effects of adding spironolactone to recommended antihypertensive treatment in diabetic nephropathy: a randomized, double-masked, cross-over study. Diabetes Care. 2005;28:2106–12.
Sato A, Hayashi K, Naruse M, Saruta T. Effectiveness of aldosterone blockade in patients with diabetic nephropathy. Hypertension. 2003;41:64–8.
Edwards NC, Steeds RP, Chue CD, et al. The safety and tolerability of spironolactone in patients with mild to moderate chronic kidney disease. Br J Clin Pharmacol. 2012;73:447–54.
Penfornis P, Viengchareun S, Le Menuet D, et al. The mineralocorticoid receptor mediates aldosterone-induced differentiation of T37i cells into brown adipocytes. Am J Physiol Endocrinol Metab. 2000;279:386–94.
Viengchareun S, Penfornis P, Zennaro MC, Lombes M. Mineralocorticoid and glucocorticoid receptors inhibit UCP expression and function in brown adipocytes. Am J Physiol Endocrinol Metab. 2001;280:E640–649.
Ehrhart-Bornstein M, Lamounier-Zepter V, Schraven A, et al. Human adipocytes secrete mineralocorticoid-releasing factors. Proc Natl Acad Sci U S A. 2003;100:14211–6.
Ehrhart-Bornstein M, Arakelyan K, Krug AW, et al. Fat cells may be the obesity-hypertension link: human adipogenic factors stimulate aldosterone secretion from adrenocortical cells. Endocr Res. 2004;30:865–70.
Rossi GP, Sticchi D, Giuliani L, et al. Adiponectin receptor expression in the human adrenal cortex and aldosterone-producing adenomas. Int J Mol Med. 2006;17:975–80.
Briones AM, Cat AN, Callera GE, et al. Adipocytes produce aldosterone through calcineurin-dependent signaling pathways: implications in diabetes mellitus-associated obesity and vascular dysfunction. Hypertension. 2012;59:1069–78.
Kraus D, Jager J, Meier B, et al. Aldosterone inhibits uncoupling protein-1, induces insulin resistance, and stimulates proinflammatory adipokines in adipocytes. Horm Metab Res. 2005;37:455–9.
Guo C, Ricchiuti V, Lian BQ, et al. Mineralocorticoid receptor blockade reverses obesity-related changes in expression of adiponectin, peroxisome proliferator-activated receptor-gamma, and proinflammatory adipokines. Circulation. 2008;117:2253–61.
Caprio M, Antelmi A, Chetrite G, et al. Antiadipogenic effects of the mineralocorticoid receptor antagonist drospirenone: potential implications for the treatment of metabolic syndrome. Endocrinology. 2011;152:113–25.
Stumpf WE, Sar M. Glucocorticosteroids and mineralocorticosteroid hormone target sites in the brain. Autoradiographic studies with corticosterone, aldosterone, deoxycorticosterone: in interaction within the brain-pituitary-adrenocortical system. In: Jones MT, Gillham B, Dallman MF, Chattopadhyay S. Interactions within the Brain–Pituitary–Adrenocortical System. London, New York: Academic Press; 1979. pp. 137-147.
Gomez-Sanchez EP, Gomez-Sanchez CE. Central regulation of blood pressure by the mineralocorticoid receptor. Mol Cell Endocrinol. 2012;350:289–98.
Geerling JC, Engeland WC, Kawata M, Loewy AD. Aldosterone target neurons in the nucleus tractus solitarius drive sodium appetite. J Neurosci. 2006;26:411–7.
Sakai RR, Nicolaidis S, Epstein AN. Salt appetite is suppressed by interference with angiotensin II and aldosterone. Am J Physiol. 1986;251:R762–8.
Sakai RR, Ma LY, Zhang DM, et al. Intracerebral administration of mineralocorticoid receptor antisense oligonucleotides attenuate adrenal steroid-induced salt appetite in rats. Neuroendocrinology. 1996;64:425–9.
Kontak AC, Wang Z, Arbique D, et al. Reversible sympathetic overactivity in hypertensive patients with primary aldosteronism. J Clin Endocrinol Metab. 2010;95:4756–61.
Monahan KD, Leuenberger UA, Ray CA. Aldosterone impairs baroreflex sensitivity in healthy adults. Am J Physiol Heart Circ Physiol. 2007;292:H190–197.
Menon DV, Arbique D, Wang Z, et al. Differential effects of chlorthalidone versus spironolactone on muscle sympathetic nerve activity in hypertensive patients. J Clin Endocrinol Metab. 2009;94:1361–6.
• Raheja P, Price A, Wang Z et al. Spironolactone Prevents Chlorthalidone-Induced Sympathetic Activation and Insulin Resistance in Hypertensive Patients. Hypertension. 2012;60:319–25. This study demonstrates the effects of spironolactone improving the excretion of markers of renal dysfunction.
De Kloet ER. Hormones and the stressed brain. Ann N Y Acad Sci. 2004;1018:1–15.
Sukor N, Kogovsek C, Gordon RD, et al. Improved quality of life, blood pressure, and biochemical status following laparoscopic adrenalectomy for unilateral primary aldosteronism. J Clin Endocrinol Metab. 2010;95:1360–4.
Yagi S, Akaike M, Aihara K, et al. High plasma aldosterone concentration is a novel risk factor of cognitive impairment in patients with hypertension. Hypertens Res. 2011;34:74–8.
Sonino N, Fallo F, Fava GA. Psychological aspects of primary aldosteronism. Psychother Psychosom. 2006;75:327–30.
Emanuele E, Geroldi D, Minoretti P, et al. Increased plasma aldosterone in patients with clinical depression. Arch Med Res. 2005;36:544–8.
Gomez-Sanchez CE, Rossi GP, Fallo F, Mannelli M. Progress in primary aldosteronism: present challenges and perspectives. Horm Metab Res. 2010;42:374–81.
Gomez-Sanchez CE, Gomez-Sanchez EP. The protective side of the mineralocorticoid receptor. Endocrinology. 2012;153:1565–7.
Stranahan AM, Arumugam TV, Lee K, Mattson MP. Mineralocorticoid receptor activation restores medial perforant path LTP in diabetic rats. Synapse. 2010;64:528–32.
Otte C, Hinkelmann K, Moritz S, et al. Modulation of the mineralocorticoid receptor as add-on treatment in depression: a randomized, double-blind, placebo-controlled proof-of-concept study. J Psychiatr Res. 2010;44:339–46.
Goritz C, Frisen J. Neural stem cells and neurogenesis in the adult. Cell Stem Cell. 2012;10:657–9.
Munier M, Law F, Meduri G et al. Mineralocorticoid receptor overexpression facilitates differentiation and promotes survival of embryonic stem cell-derived neurons. Endocrinology. 2012.
• Kolkhof P, Borden SA. Molecular pharmacology of the mineralocorticoid receptor: prospects for novel therapeutics. Mol Cell Endocrinol. 2012;350:310–7. This is an excellent review of the pharmacology of mineralocorticoid receptor antagonists, old and new.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hawkins, U.A., Gomez-Sanchez, E.P., Gomez-Sanchez, C.M. et al. The Ubiquitous Mineralocorticoid Receptor: Clinical Implications. Curr Hypertens Rep 14, 573–580 (2012). https://doi.org/10.1007/s11906-012-0297-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-012-0297-0