Abstract
Background
Kirsten-Ras (KRAS) mutations are widely accepted negative predictive factors for anti-EGFR therapies in metastatic colorectal cancer (mCRC), while their prognostic significance is still under discussion.
Objective
This mono-institutional retrospective study aims to investigate the real-life impact of exon 2 codon 12 and 13 mutations in mCRC.
Methods
All mCRC patients treated at our institution between 2008 and 2014 carrying KRAS exon 2 mutations were included. The primary endpoint was to determine any significant difference in overall survival (OS) between codon 12 and 13 mutations. Secondary endpoints included progression-free survival (PFS), OS in both populations according to antiangiogenic treatment, and OS in liver-limited disease (LLD).
Results
Of 620 mCRC patients, 218 carried KRAS exon 2 mutations (35.1 %): 162 (26.1 %) at codon 12 and 56 (9.0 %) at codon 13. Median OS results were similar: 32.0 months (codon 12) and 31.0 months (codon 13). PFS was also comparable, reaching 10.8 months in both populations. The addition of bevacizumab to chemotherapy conferred a trend toward survival advantage in codon 12 but not codon 13 mutation (p = 0.058). A high proportion of LLD patients underwent hepatic surgery with radical purpose (62.3 %): in these patients, median OS has not yet been reached, while OS in non-LLD patients was 30.2 months.
Conclusions
No difference in OS between KRAS codon 12/13 mutated disease was found. This analysis showed a very prolonged OS for KRAS-mutated patients, even when LLD patients were excluded; OS of our real-life series favorably compares with OS of all-RAS wild-type patients in recent randomized studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients with KRAS codon 12 and 13 mutated metastatic colorectal cancer (mCRC) had long and comparable survival. |
Surgery for metastases confers a comparable survival gain in codon 12 and 13 mutations. |
Bevacizumab seems to confer a survival advantage in codon 12 but not 13 mutation. |
1 Introduction
Kirsten-Ras (KRAS) is a proto-oncogene member of the RAS proteins family (KRAS, NRAS, HRAS) encoding for a guanosine diphosphate/triphosphate (GDP/GTP)-binding protein component of the EGFR signaling pathway. Its gene mutations are involved in the origination and progression of several solid tumors [1]. KRAS gene mutations lead to a reduced GTPase activity of the protein, which causes a persistent GTP-bound active status independent from the upstream signal, resulting in a constitutive activation of the RAS-RAF-MAPK pathway [2]. KRAS mutations occur mostly in early phases of colorectal carcinogenesis [3] and can be detected in 30–50 % of colorectal cancer patients [4, 5]. KRAS exon 2 mutations in codons 12 and 13 account for the large majority—approximately 90 %—of all-RAS mutations, while other mutations in KRAS exon 3 (codons 59, 60, 61), exon 4 (codons 119, 146, 147), or NRAS mutations represent a small proportion of these mutations [6, 7]. Thus, it can be reasonably argued that the clinical relevance of RAS gene mutations in colorectal cancer (CRC) is mainly due to KRAS codon 12 and 13 mutational status.
In metastatic CRC (mCRC), KRAS mutation is an established predictive factor of resistance to anti-epidermal growth factor receptor (EGFR) therapies, either in monotherapy or in association with chemotherapy [8, 9], whereas the significance of KRAS mutational status as an independent biomarker of prognosis is less clear, since no definitive data have been produced that clearly demonstrate a poorer prognosis in KRAS-mutated patients compared with the wild-type population, especially when advanced-stage disease is considered, as opposed to BRAF mutational status, which is nowadays a recognized independent prognostic factor in advanced CRC [10]. Large series show a potentially negative prognostic role for KRAS mutations in terms of cancer-specific mortality, but all stages (I–IV) at diagnosis have been considered, and this leaves nebulous the specific issue of prognostic impact on a stage IV population [4].
The landscape is even more confused by preclinical data showing that specific KRAS mutations may confer major transforming power, thus potentially influencing prognosis of diseases characterized by different KRAS mutations. In particular, some in vitro studies have demonstrated that codon 12 mutations, especially p.G12V and p.G12D mutations, are able to determine a more stable bond between Ras protein and GTP molecule, conferring a higher resistance to GTPase activity compared with p.G13D mutation of codon 13 [11, 12]. These results suggest that codon 12 mutations confer more aggressive behavior to CRC than do codon 13 mutations. Several authors tried to confirm these preclinical findings in clinical studies, investigating the potential prognostic weight of specific KRAS codon 12 in comparison with 13 mutations, but results were quite discordant. A large collaborative study conducted among 3439 patients with CRC at any stage found a significant association between codon 12 p.G12V mutation and risk of death only in Duke’s stage C patients, while this association was not found in Duke’s B or in advanced-stage disease [13]. This association was confirmed by a more recent study conducted by Imamura et al. [14], in which codon 12 mutations (hazard ratio [HR] 1.30), and specifically p.G12V mutations (HR 2.00), were associated with a significantly higher cancer-related mortality than in KRAS/BRAF wild-type patients, whereas no specific impact on cancer mortality was seen in patients bearing codon 13 mutations [14]. However, only 13 % of the population considered had stage IV disease, thus reducing the significance of these findings in patients with mCRC. In contrast with these reports, a large study conducted over 1413 CRC patients showed no association between KRAS mutations and survival when all mutations were analyzed together, but a 40 % higher risk of cancer-related death was seen only in patients bearing codon 13 mutations [15]; again, in this study, only 16.7 % of patients had advanced disease, while the vast majority of the cohort comprised patients with local or locoregional disease (Duke’s stage B or C).
Indeed, these studies neither specifically addressed the issue of metastatic disease nor evaluated the possible role of treatment strategies used in these patients, thereby precluding any clinical impact of these mutations in ‘real-life’ practice. Therefore, we conducted a retrospective study on a consecutive series of KRAS exon 2-mutated patients affected by advanced (stage IV) CRC, with the aim of evaluating any prognostic difference between codon 12 and codon 13 mutations. Overall survival (OS) was also analyzed according to each mutation and treatment received, given that several trials have reported very low survival for KRAS-mutated populations [16–18], especially when compared with OS of all-RAS wild-type patients in recent trials [19–22].
2 Patients and Methods
2.1 Patients
This retrospective study was conducted at the Catholic University of Sacred Heart in Rome, Italy. Clinical records of all patients affected by advanced CRC (stage IV according to TNM [tumor, node, metastases]) and treated at the Medical Oncology Unit between 2008 and 2014 were reviewed. Eligibility criteria included histologically confirmed CRC, metastatic disease, confirmed KRAS exon 2 mutation (codon 12 or codon 13), detected in specimens of primary tumor and/or metastases. All procedures were conducted in accordance with the rules of the local ethics committee and the declaration of Helsinki; consent for chemotherapy was obtained from all patients, as was consent for retrospective analysis of all clinical data. A separate consent for molecular analysis was obtained. Patients were excluded in case of KRAS mutational status discrepancies between primary tumor and metastases or in case of RAS/RAF mutations other than KRAS exon 2. Moreover, patients were also excluded in case of serious concomitant illness that could have affected survival at the time of diagnosis, or in case of other cancers (with the exception of non-melanoma skin cancers and in situ cervical cancer) within the previous 5 years. All eligible patients were consecutively included.
2.2 KRAS Assessment
Tumor was identified in hematoxylin and eosin-stained sections of formalin-fixed, paraffin embedded archival blocks. DNA was extracted by 5-μm sections of paraffin-embedded tissue, containing at least 70 % tumor, using QIAamp DNA mini Kit (Qiagen, Milan, Italy). KRAS codons 12 and 13 were amplified in one polymerase chain reaction (PCR). Thermal cycling conditions were 95 °C for 12 min followed by 40 cycles of 95 °C for 10 s, 55 °C for 20 s, and 72 °C for 20 s. PCR conditions were primer concentration 200 nmol/l, MgCl2 concentration 2 mmol/l; 30 ng of genomic DNA and 12.5 μl of Eppendorf Prime mastermix in a final reaction volume of 25 μl. PCR products were electrophoresed in a 2.5 % agarose gel, stained with ethidium bromide and visualized under ultraviolet light. Thereafter, 5 μl of PCR product was treated with ExoSAP-IT (GE Healthcare, Milan, Italy) following the manufacturer’s protocol, amplified with BigDye Terminator version 3.1 cycle sequencing kit (Applied Biosystems, Milan, Italy) using the same primers as in the amplification, and sequenced with an ABI PRISM 3100-Avant Genetic Analyzer (Applied Biosystems).
2.3 Systemic Treatments
All patients had histologically proven and radiologically confirmed mCRC. The patient population was divided in two groups according to the codon (12 vs. 13) where the KRAS exon 2 mutation was detected. To avoid any confounding from systemic treatments administered, patients treated with anti-EGFR antibodies or any investigational drug not previously approved were not included. Backbone chemotherapy regimens for both groups consisted of fluoropyrimidines (endovenous 5-fluorouracil given by bolus and continuous infusion, in association with folinic acid or oral capecitabine), administered alone or in combination with oxaliplatin (Folfox/XelOx regimens) and/or irinotecan (Folfiri/Xeliri/Folfoxiri regimens). Bevacizumab was added to chemotherapy according to clinical evaluation.
2.4 Study Endpoints
The primary endpoint of the study was to determine whether OS differed in patients with codon 12 KRAS mutations compared with patients with codon 13 KRAS mutations. Secondary endpoints included difference in objective response rate (ORR) according to RECIST (Response Evaluation Criteria in Solid Tumours) 1.1 criteria [23], progression-free survival (PFS), OS according to treatment received (chemotherapy only vs. chemotherapy plus bevacizumab), OS in liver-limited disease (LLD) according to codon mutation and surgery of metastases. A subgroup analysis of the prognostic impact of bevacizumab treatment given in a first- versus a second-line setting was conducted, as was a subset exploratory analysis of potential prognostic impact for the specific subgroup of codon 12 mutations.
2.5 Statistical Analysis
We used χ 2 test to compare clinical and biological characteristics according to KRAS mutational status. For each group, OS was calculated as the time interval between the diagnosis of metastatic disease until death or last follow-up contact. PFS was defined as the time interval between the beginning of chemotherapy and documented disease progression. OS and PFS were estimated according to the Kaplan–Meier method, and survival curves were compared using the log-rank test. HRs were estimated at a confidence interval (CI) of 95 %, with outcome differences considered statistically significant at a p value ≤0.05 for a bilateral test. The correlation of KRAS mutational status and clinical and pathological characteristics with survival was assessed in univariate analyses. All statistical analyses were performed using IBM SPSS Statistics 22.0 software and MedCalc software.
3 Results
3.1 Patient Characteristics
Of 620 total patients affected by mCRC treated at our institution whose KRAS mutational status was known, 218 (35.1 %) had a KRAS exon 2 mutation and were eligible for this study: 162 at codon 12 (26.1 %), 56 (9.0 %) at codon 13. Five patients were excluded from this series since they had been treated with anti-EGFR drugs, and 13 patients were excluded because they had been treated with experimental agents in clinical trial settings. All patients in the codon 13 mutation group carried a p.G13D mutation, while seven different point mutations were identified in the codon 12 group: p.G12D (65 patients), p.G12V (53 patients), p.G12A (18 patients), p.G12C (11 patients), p.G12S (ten patients), p.G12R (four patients), p.G12F (one patient). Median age at diagnosis was similar in both groups: 66 years in the codon 12 group (range 37–83), 65 years in the codon 13 group (range 41–84). A total of 92 (56.8 %) patients were male in the codon 12 group, and 28 (50 %) were male in the codon 13 group. No significant statistical differences in site distribution of primary CRC was found between the two groups (codon 12 and codon 13 groups, respectively): 32.7 and 39.3 % had a tumor arising from the ascending colon, 4.9 and 1.7 % from the transverse, 39.5 and 28.6 % from the descending or the sigmoid colon, and 22.9 and 30.4 % from the rectum. In both groups, quite a high percentage of patients had synchronous metastatic disease: 70.4 % in the codon 12 group, 75.0 % in the codon 13 group, without significant statistical difference. Percentage of LLD, defined as a macroscopic metastatic spread confined to the liver at diagnosis, was similar between the groups: 52 patients (32.1 %) in the codon 12 group, 17 patients (30.4 %) in the codon 13 group, with no statistical difference. More than one metastatic site was found in 84 (51.8 %) and 29 (51.8 %) patients in the codon 12- and codon 13-mutated groups, respectively. The baseline characteristics of patients are summarized in Table 1.
3.2 Treatment Allocation
Patients in both groups received chemotherapy regimens as described above. A total of 59 (36.4 %) patients in the codon 12 group and 18 (32.1 %) patients in the codon 13 group received only one line of systemic therapy, while 99 (61.1 %) and 36 (64.3 %) patients, respectively, received two or more lines of chemotherapy. Only four patients (2.5 %) in the codon 12 group and two patients (3.6 %) in the codon 13 group did not receive any systemic treatment. In both groups, more than 50 % of patients received both oxaliplatin- and irinotecan-based regimens (53.1 and 58.9 % among codon 12 and 13 mutated patients, respectively). Moreover, a very high percentage of patients received bevacizumab in association with chemotherapy: 106 (65.4 %) patients in the codon 12 group vs. 40 (71.4 %) patients in the codon 13 group, mostly as first-line treatment.
3.3 Surgery for Metastases
A high percentage of patients from both groups underwent surgery for metastases: 61 (37.6 %) and 20 (35.7 %) patients in the codon 12 and 13 groups, respectively. A total of 15 (9.3 %) patients in the codon 12 group and eight (14.3 %) patients in the codon 13 group received more than one surgical intervention during the disease course. The most practiced surgery was hepatic metastectomy, performed by dedicated liver surgeons, in a similar percentage of patients: 46 (28.4 %) and 16 (28.6 %) patients in the codon 12 and 13 mutation groups, respectively. Surgery of metastases other than hepatic was less frequent: in 22 (13.6 %) and 10 (17.9 %) patients among the codon 12 and 13 groups, respectively. Among these, 22 patients received lung metastectomy (15 in the codon 12 group, seven in the codon 13 group), while ten patients received lymph node, cutaneous/subcutaneous, or peritoneal metastectomy.
3.4 Endpoint Data
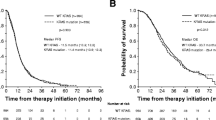
OS did not differ between the two groups of patients, both being longer than 30 months, with a median value of 32.0 months (95 % CI 26.3–37.7) in codon 12-mutated patients and 31.0 months (95 % CI 24.3–37.8) in codon 13-mutated patients (Fig. 1). Similarly, no substantial differences were seen between the two groups for PFS (10.8 months for each group for first-line therapy; 95 % CI 9.5–12.1 for the codon 12 group, 95 % CI 8.3–13.4 for the codon 13 group) and ORR (50.6 % and 50.0 % for codon 12 and codon 13 groups, respectively; p = 0.907, odds ratio [OR] 0.98; 95 % CI 0.5–1.89). No first-line chemotherapy regimen showed superior activity. During the course of the disease, patients who received oxaliplatin- and irinotecan-based regimens experienced significantly longer survival than those treated with only one agent (36.7 vs. 24.6 months, respectively; 95 % CI 14.8–34.4 and 95 % CI 31.0–42.5, respectively; p < 0.001). The difference in survival also remained significant when codon 12 and codon 13 mutations were considered separately. The addition of bevacizumab to chemotherapy improved survival, with a trend toward a statistically significant difference only in the codon 12-mutated population (33.6 vs. 21.8 months; 95 % CI 28.8–38.3 and 95 % CI 5.2–38.5, respectively; p = 0.058, Fig. 2), whereas no difference was seen when bevacizumab was added to chemotherapy in codon 13-mutated patients. No difference in survival benefit in codon 12-mutated patients was seen between bevacizumab given either in a first- or a second-line setting.
As expected, patients with LLD experienced significantly longer survival than those with non-LLD, but even this subgroup experienced a good outcome. In fact, OS in non-LLD patients (149) from the whole study population was 30.2 months (95 % CI 26.2–34.1), whereas median OS has not yet been reached in the LLD group (69), after a median follow-up time of 25.1 months (estimate 62.7 months after 28/69 events: 95 % CI 38.7–86.7; hazard ratio 0.50; 95 % CI 0.35–0.72, p = 0.001). The significance was maintained in both mutational subgroups, despite the small population of codon 13-mutated patients with LLD. Even excluding patients from the non-LLD subgroup undergoing lung metastectomy, OS still reached 27.3 months (95 % CI 22.2–32.3). Strong differences were also seen among patients who underwent surgery for metastases compared with those treated with chemotherapy ± bevacizumab therapy only, regardless of the specific mutation analyzed. No differences were seen when survival of patients affected by synchronous versus metachronous disease was compared (OS for synchronous metastatic disease: 31.0 months, 95 % CI 25.9–36.2; OS for metachronous disease: 32.0 months, 95 % CI 27.0–37.0, p = 0.41), also considering the codon 12 and codon 13 groups separately. All endpoint data reported are summarized in Table 2.
3.5 Subset Analysis for Specific Mutations
More frequent specific point mutations in codon 12 and codon 13 were analyzed separately [24]. No significant differences in distribution of metastatic sites were observed among different amino-acidic substitutions. OS was uniformly longer than 30 months in all patients except those with p.G12C (11 patients) or p.G12S mutation (ten patients), who had lower OS, at 24.4 and 25.1 months, respectively. Although the small sample size probably did not allow for any statistical comparison, some specific mutations, such as p.G12A or p.G12D, potentially seem able to confer a better prognosis (OS 39.1 and 36.7 months, respectively). This was confirmed when OS was adjusted for each mutation according to the number of metastatic sites involved at diagnosis. Median OS for all specific mutations were as follows: p.G12A 39.1 months (18 patients, 95 % CI 27.3–50.9); p.G12C 24.4 months (11 patients, 95 % CI 10.6–38.2); p.G12D 36.7 months (65 patients, 95 % CI 26.2–47.2); p.G12F 5.7 months (one patient); p.G12R not estimable (four patients, one event occurred); p.G12S 25.1 months (ten patients, 95 % CI 5.0–45.2); p.G12V 30.2 months (53 patients, 95 % CI 25.7–34.7); p.G13D 31.0 months (56 patients, 95 % CI 24.3–37.8).
4 Discussion
Looking back on the last ten years of trials in mCRC, studies designed for the KRAS-mutated patient population are lacking even though it is, numerically, as important as its wild-type counterpart. In addition, it might be plausible that different mutations induce different disease behaviors, suggesting some uncertainty on what could be—if there is only one—the best therapeutic approach for this disease.
Unlike previous studies, our series of patients included only stage IV disease, showing no prognostic differences between patients with codon 12 and codon 13 mutations. To our knowledge, this is the first report attaining a very prolonged OS for this subset of patients (over 30 months in both codon 12- and codon 13-mutated populations), quite comparable to that reached not only in a KRAS exon 2 wild-type population, but also in all-RAS wild-type populations. Looking at these unexpected data, we wonder whether KRAS mutation must always be considered a bad prognostic factor in mCRC. Indeed, the prolonged survival observed in our patients might be related to the high percentage of patients receiving second and further lines of therapy or to the high number of patients receiving surgery with radical intent.
In our analysis, duration of survival in both mutation groups was not affected so much by the sequence of treatments given as by the ability to receive all available treatments. According to a well-known systematic review, patients who received both oxaliplatin- and irinotecan-based regimens survived significantly longer than those receiving only one of these drugs [25]. These findings are even more suggestive when the clinical setting of our study is considered; in fact, unlike randomized clinical trials, exclusion criteria such as performance status or life expectancy were not taken into account, thereby describing the disease behavior of codon 12 and codon 13 mutation that is closer to the real world.
Concerning surgery, irrespective of mutation subgroup, a high percentage of patients in this series underwent surgical treatment of metastases, especially those with LLD. This approach contributed to increased OS in resected patients, confirming that an integrated loco-regional and systemic treatment is also feasible and effective in KRAS-mutated patients, delivering results comparable to those obtained in wild-type populations [27]. Even in patients affected by disease that has spread outside the liver, surgery of metastases in addition to chemotherapy resulted in a significant survival benefit [28]. In light of these considerations, it is possible that, even if codon 12 and 13 mutations were responsible for a worse biological behavior, our aggressive therapeutic approach, from both surgical and medical viewpoints, could also eventually have been effective in improving survival.
Another interesting result of our analysis concerns the role of bevacizumab in these mutated patients. The addition of bevacizumab to chemotherapy improved survival only in the codon 12-mutated population, whereas anti-vascular endothelial growth factor (VEGF) treatment did not seem to provide an advantage to codon 13-mutated patients. The role of bevacizumab in RAS-mutated patients has recently been questioned, but no randomized study has considered the outcomes in different codons, and this might prevent the recognition of distinct effects. Although the retrospective nature and the sample size of our study cannot lead to definitive assumptions, an intriguing explanation of the results obtained in the present study might reside in a stronger upregulation of VEGFs in patients with codon 12 mutations rather than in those with codon 13 mutation, as has been shown in previous preclinical studies [12, 26]. This hypothesis warrants confirmation in larger and possibly prospective studies.
The incidence of specific codon 12 mutations was similar as found in previously published data [14, 15]; however, subset survival analysis did not confirm previous results showing a worse prognosis for patients with p.G12V mutations. The small sample size of this subgroup in our study probably did not allow us to reach a statistically significant difference, but it should be highlighted that OS among the most common codon 12 point mutations was longer than 30 months, except in two low-frequency mutations (p.G12C and p.G12S), in which OS was about 25.0 months.
5 Study Limitations
We can identify three main biases in our study. First, its retrospective nature could have concealed some confounding factors, such as comorbidities influencing the choice of chemotherapy, although codon 12 and 13 arms were well balanced for burden of disease and allocation of systemic treatments. Second, despite the large number of patients in the overall population, some subgroups might have been particularly small samples when subdividing codon 12 mutations according to specific point mutations. Finally, even in a retrospective survey, a control arm including the KRAS wild-type population would have made it possible to better evaluate the prognostic impact of codon 12–13 KRAS mutation. A prospective trial to address this issue might be too complex to design, so larger retrospective studies would be helpful.
6 Conclusions
The present study shows that mCRC patients with codon 12–13 mutations in real-life clinical practice may take advantage of aggressive multidisciplinary treatments, achieving OS comparable to that of all-RAS wild-type patients in randomized studies, although study biases cannot lead to definitive assumptions. In that regard, the comparison of present data with data of all-RAS wild-type patients treated at our institution in the same period could be very helpful to better clarify the prognostic role of a KRAS mutation; we are working on this issue. No difference has been found in OS of patients with codon 12 mutations compared with those with codon 13 mutations. However, it is possible that bevacizumab could affect the outcome of patients with codon 12 mutations differently from those with codon 13 mutations. This hypothesis warrants further study, as it is possible that some point mutation in the KRAS gene can have a detrimental impact on prognosis. Irrespective of KRAS mutation, patients with LLD experience very long survival.
References
Bos JL. Ras oncogenes in human cancer: a review. Cancer Res. 1989;1989(49):4682–9.
Schubbert S, Shannon K, Bollag G. Hyperactive ras in developmental disorders and cancer. Nat Rev Cancer. 2007;2007(7):295–308.
Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, Nakamura Y, White R, Smits AM, Bos JL. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319(9):525–32.
Andreyev HJN, Norman AR, Cunningham D, Oates JR, Clarke PA. Kirsten Ras mutations in patients with colorectal cancer: the multicenter ‘RASCAL’ study. J Natl Cancer Inst. 1998;90(9):675–84.
Roock WD, Vriendt VD, Normanno N, Ciardiello F, Tejpar S. KRAS, BRAF, PIK3CA, and PTEN mutations: implications for targeted therapies in metastatic colorectal cancer. Lancet Oncol. 2011;2011(12):594–603.
Douillard JY, Oliner KS, Siena S, Tabernero J. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369(11):1023–34. doi:10.1056/NEJMoa1305275.
Schirripa M, Cremolini C, Loupakis F, Morvillo M, Bergamo F, Zoratto F, Salvatore L, Antoniotti C, Marmorino F, Sensi E, Lupi C, Fontanini G, De Gregorio V, Giannini R, Basolo F, Masi G, Falcone A. Role of NRAS mutations as prognostic and predictive markers in metastatic colorectal cancer. Int J Cancer. 2015;136(1):83–90. doi:10.1002/ijc.28955 (Epub 2014 May 28).
Peeters M, Douillard JY, Van Cutsem E, Siena S. Mutant KRAS codon 12 and 13 alleles in patients with metastatic colorectal cancer, assessment as prognostic and predictive biomarkers of response to Panitumumab. J Clin Oncol. 2012;2012(31):759–65.
Van Cutsem E, Kohne CH, Lang I, Folprecht G. Cetuximab plus irinotecan, fluorouracil and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol. 2011;2011(29):2011–9.
Yokota T, Ura T, Shibata N, Takahari D, Shitara K, Nomura M, Kondo C, Mizota A, Utsunomiya S, Muro K, Yatabe Y. BRAF mutation is a powerful prognostic factor in advanced and recurrent colorectal cancer. Br J Cancer. 2011;104(5):856–62.
Al-Mulla F, Milner-White EJ, Going JJ, Birnie GD. Structural differences between valin-12 and aspartate-12 Ras proteins may modify carcinoma aggression. J Pathol. 1999;1999(187):433–8.
Guerrero S, Casanova I, Farrè L, Mazo A, Capellà G, Mangues R. K-ras codon 12 mutation induces higher level of resistance to apoptosis and predisposition to anchorage-independent growth than codon 13 mutation or proto-oncogene overexpression. Cancer Res. 2000;2000(60):6750–6.
Andreyev HJN, Norman AR, Cunningham D, Oates J, Dix BR. Kirsten ras mutations in patients with colorectal cancer: the ‘RASCAL II’ study. Br J Cancer. 2001;85(5):692–6.
Imamura Y, Morikawa T, Liao X, Lockhead P, Kuchiba A, Yamauchi M, Qian ZR, Nishihara R, Meyerhardt JA, Haigis KM, Fuchs CS, Ogino S. Specific mutations in KRAS codons 12 and 13, and patient prognosis in 1075 BRAF wild-type colorectal cancers. Clin Cancer Res. 2012;18(17):4753–63. doi:10.1158/1078-0432.CCR-11-3210.
Samowitz WS, Curtin K, Schaffer D, Robertson M, Leppert M, Slattery ML. Relationship of Ki-ras mutations in colon cancers to tumor location, stage, and survival: a population-based study. Cancer Epidemiol Biomarkers Prev. 2000;9(11):1193–7.
Maughan TS, Adams RA, Smith CG, Meade AM, Seymour MT. Addition of cetuximab to oxaliplatin-based first-line combination chemotherapy for treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet. 2011;377(9783):2103–14. doi:10.1016/S0140-6736(11)60613-2.
Petrelli F, Coinu A, Cabiddu M, Ghilardi M, Barni S. KRAS as prognostic biomarker in metastatic colorectal cancer patients treated with bevacizumab: a pooled analysis of 12 published trials. Med Oncol. 2013;2013(30):650.
Bokemeyer C, Bondarenko I, Hartmann JT, de Braud F, Schuch G, Zubel A, Celik I, Schlichting M, Koralewski P. Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol. 2011;22(7):1535–46. doi:10.1093/annonc/mdq632.
Van Cutsem E, Lenz HJ, Kohne CH, Heinemann V. Fluorouracil, Leucovorin, and Irinotecan plus Cetuximab treatment and RAS mutations in colorectal cancer. J Clin Oncol. 2015;33(7):692–700. doi:10.1200/JCO.2014.59.4812.
Stintzing S, Modest DP, Fischer von Weikersthal L, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran S, Heintges T, Lerchenmueller C, Kahl C, Seipelt G, Kullmann F, Scheithauer W, Held S, Giessen C, Moehler M, Jagenburg A, Jung A, Kirchner T, Heinemann V. Independent radiological evaluation of objective response, early tumor shrinkage, and depth of response in FIRE-3 (AIO KRK-0306) in the final RAS evaluable population. ESMO 2014 Congress, Proffered Paper Session—ref. LBA11; 2014.
Schwartzberg LS, Rivera F, Karthaus M, Fasola G, Canon JL, Hecht JR, Yu H, Oliner KS, Go WY. PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J Clin Oncol. 2014;32(21):2240–7. doi:10.1200/JCO.2013.53.2473.
Lenz H, Niedzwiecki D, Innocenti F, Blanke C, Mahony MR, O’Neil BH, Shaw JE, Polite B, Hochster H, Atkins J, Goldberg R, Mayer R, Schilsky R, Bertagnolli M, Venook A. CALGB/SWOG 80405: PHASE III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (mFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with expanded ras analyses untreated metastatic adenocarcinoma of the colon or rectum (mCRC)—ESMO 2014 Congress, Proffered Paper Session—ref. 501O; 2014.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. doi:10.1016/j.ejca.2008.10.026.
Bruera G, Cannita K, Tessitore A, Russo A, Alesse E, Ficorella C, Ricevuto E. The prevalent KRAS exon 2 c.35G>A mutation in metastatic colorectal cancer patients: A biomarker of worse prognosis and potential benefit of bevacizumab-containing intensive regimens? Crit Rev Oncol Hematol. 2015;93(3):190–202. doi:10.1016/j.critrevonc.2014.10.004.
Grothey A, Sargent D. Overall survival of patients with advanced colorectal cancer correlates with availability of fluorouracil, irinotecan, and oxaliplatin regardless of whether doublet or single-agent therapy is used first line. J Clin Oncol. 2005;23(36):9441–2.
Rak J, Mitsuhashi Y, Sheehan C, Tamir A, Viloria-Petit A, Filmus J, Shirasawa S, Sasazuki T. Mutant ras oncogenes upregulate VEGF/VPF expression: implications for induction and inhibition of tumor angiogenesis. Cancer Res. 1995;1995(55):4575–80.
Venook A, Niedzwiecki D, Lenz H, Mahoney M, Innocenti F, O’Neil B, Hochster H, Goldberg R, Schilsky R, Mayer R, Polite B, Atkins J, Shaw JE, Bertagnolli M, Blanke C. CALGB/SWOG 80405: Analysis of patients undergoing surgery as part of treatment strategy. ESMO 2014 Congress, Proffered Paper Session—ref. LBA10; 2014.
Renaud S, Romain B, Falcoz PE, Olland A, Santelmo N, Brigand C, Rohr S, Guenot D, Massard G. KRAS and BRAF mutations are prognostic biomarkers in patients undergoing lung metastasectomy of colorectal cancer. Br J Cancer. 2015;112(4):720–8. doi:10.1038/bjc.2014.499.
Acknowledgments
All the authors contributed to the article without any external involvement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
VD, MB, SR, TC, SC, AS, AO, EC, GS, AC, MM, and CB declare no funding has been received for the conduct of this study.
Conflicts of interest
VD, MB, SR, TC, SC, AS, AO, EC, GS, AC, MM, and CB declare no conflicts of interest that are directly relevant to the content of this article.
Ethical approval and informed consent
This study was conducted in accordance with the rules of the local ethics committee and the declaration of Helsinki. All patients provided written consent for use of their clinical data; a separate consent for molecular analysis was obtained.
Rights and permissions
About this article
Cite this article
Dadduzio, V., Basso, M., Rossi, S. et al. KRAS Exon 2 Mutations as Prognostic Indicators in Advanced Colorectal Cancer in Clinical Practice: A Mono-Institutional Study. Mol Diagn Ther 20, 65–74 (2016). https://doi.org/10.1007/s40291-015-0178-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-015-0178-8