Abstract
Background
Athletes experience various situations and conditions that can interfere with their sleep, which is crucial for optimal psychological and physiological recovery as well as subsequent performance. Conventional sleep screening and intervention approaches may not be efficacious for athletes given their lifestyle, the demands of training and travel associated with interstate/international competition.
Objectives
The present systematic review aimed to summarize and evaluate sleep intervention studies targeting subsequent performance and recovery in competitive athletes. Based on the findings, a secondary aim was to outline a possible sleep intervention for athletes, including recommendations for content, mode of delivery and evaluation.
Methods
A systematic review was conducted based on the PRISMA guidelines in May 2016 with an update completed in September 2017. Ten studies met our inclusion criteria comprising a total of 218 participants in the age range of 18–24 years with athletes from various sports (e.g., swimming, soccer, basketball, tennis). A modified version of the quality assessment scale developed by Abernethy and Bleakley was used to evaluate the quality of the studies.
Results
The included studies implemented several sleep interventions, including sleep extension and napping, sleep hygiene, and post-exercise recovery strategies. Evidence suggests that sleep extension had the most beneficial effects on subsequent performance. Consistent with previous research, these results suggest that sleep plays an important role in some, but not all, aspects of athletes’ performance and recovery.
Conclusion
Future researchers should aim to conduct sleep interventions among different athlete populations, compare results, and further establish guidelines and intervention tools for athletes to address their specific sleep demands and disturbances.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adequate sleep is crucial for optimal recovery and subsequent performance in athletes. |
Athletes may face sleep disturbances due to their unique lifestyle; thus, results from sleep intervention studies in the general population may be limited in their applicability. |
Sleep extension had the most beneficial effects on subsequent performance measures (e.g., sport-specific skill execution), while napping, sleep hygiene, and post-exercise recovery strategies provided mixed results. |
1 Introduction
An athlete’s ability to reach his or her peak potential and achieve a high level of success is determined by several factors. In addition to well-known influences such as physical conditioning [1] and nutrition [2], sleep plays an equally important role, and is widely considered to be essential for optimal performance and recovery outcomes [3, 4]. Likewise, physical activity can promote nocturnal sleep, resulting in a reciprocal relationship between sleep and sporting participation [5]. As research on sleep in athlete populations has expanded over the years, findings have become more accessible to those competing and working within the sporting industry [6]. Consequently, there is an emerging awareness among athletes, coaches, and trainers about the importance of sleep and the need to incorporate sleep-enhancing strategies into their planning and preparation [7].
Several studies investigating the impact of sleep loss and accumulated sleep debt on athletes have shown negative consequences for both physical and cognitive performance. However, most studies have simulated extreme cases of sleep loss, in which participants do not sleep for long periods of time (e.g., one night and day). These studies are generally not reflective of the sleep disturbances most athletes face in real life [3], namely, partial sleep deprivation, which refers to reduced sleep over consecutive nights (e.g., falling asleep later or waking earlier than required for adequate sleep). The few studies to date that have examined the effects of partial sleep deprivation on physical performance show that single bouts of aerobic exercise and maximal measures of strength are minimally affected [3]. In comparison, sports-specific skill execution, submaximal sustained exercise bouts, and muscular and anaerobic power appear to be more prone to impairment [3, 4, 8]. Cognitive consequences include deficits in most aspects of functioning, such as reaction time, fine motor movement, memory (e.g., consolidation of motor tasks) and decision-making, and also greater variation in mood stability [3]. In addition, poor mood states have been linked to over-reaching and over-training [9, 10]. Overall, the evidence to date suggests that sleep loss impacts the performance of athletes via physical and cognitive pathways.
Parallel to the effects of sleep loss on the body`s response to exercise, several studies have shown an adverse effect on physiological mechanisms involved in post-exercise recovery. Consequently, sleep has been suggested to be the best recovery strategy available to an athlete [4, 11]. However, knowledge of the mechanisms behind the relationship between sleep and recovery in athletic populations is still being developed. It has been theorized that optimal conditions for cell growth and repair occur during slow wave sleep (SWS; often referred to as deep sleep [12]), with reduced sleep duration also contributing to an inability for the body to adequately break down cells required for future repair and growth [13]. In other words, sleep loss in athletes reduces the muscle protein resynthesis mechanism and stimulates processes resulting in muscle degradation. Moreover, even with a normalized carbohydrate intake, muscle glycogen stores are reduced during sleep deprivation [14]. This is likely a result of energy consumption by athletes during their forced wakefulness [14]. Considering that significant energy expenditure occurs, it is vital that athletes get enough sleep, as depletion of glycogen reserves is a direct cause of the onset of overreaching [15]. Whilst 7–9 h of sleep is recommended for healthy adults [16, 17], research suggests that athletes need 9–10 h of total sleep time [18, 19] to reach their full potential. Athletes’ higher need for sleep was first recorded among collegiate tennis players. The novel study by Mah et al. [20] was the first to specifically investigate the impact of additional bed time on sleep duration and subsequent performance.
Despite the clear need for athletes to obtain adequate sleep, evidence suggests that sleep disturbances are common [21] and typically occur at two time points. During regular training periods, disturbed sleep can occur due to poor sleep hygiene (e.g., late game or training sessions and late caffeine intake to improve post exercise recovery [22]), chronic sleep complaints (e.g., insomnia), or as a response to heavy training workloads (i.e., functional over-reaching [23, 24]). In contrast, temporary sleep disturbances may arise prior to competitions because of disruption to usual sleep routines (e.g., travel, jet-lag, hotel bed, noise) or pre-competition anxiety [25, 26]. Thus, there are multiple reasons why an athlete may experience sub-optimal sleep, which is a cause for concern given the implications for performance and recovery outcomes.
In response to research highlighting the poor sleep habits of some athletes, researchers have begun to develop and evaluate sleep interventions aimed at optimizing performance and recovery outcomes. Broadly speaking, these interventions can be categorized into three sub-types based on the process used to modify sleep, namely, sleep extension and napping, sleep hygiene, and post-exercise recovery strategies. Sleep extension and napping interventions aim to increase the amount of sleep obtained via total sleep duration or brief targeted naps [19]. Sleep hygiene practices have also been used and aim to improve sleep related behaviors to promote a good night’s sleep [27]. Finally, post-exercise recovery strategies that affect sleep as a consequence are evident in the literature [28]. Currently, only a small number of published studies have investigated each of these interventions among athlete populations.
Importantly, there are two key methodological issues that limit the applicability of the findings, and the recommendations derived, from some studies evaluating sleep interventions targeted at athletes. Specifically, participant samples have either not comprised athletes [29,30,31], or performance and recovery outcomes have not been measured [32]. Consequently, these design flaws may lead to erroneous assumptions about the effectiveness of these interventions for both improving sleep and optimizing performance and recovery outcomes. This presents a potential problem for athletes, coaches, and trainers, who try to access and interpret evidence from the literature to determine best practice. Thus, there is a need to consolidate existing evidence from sleep intervention studies that have used athlete samples and those that have also measured the impact on performance and/or recovery.
The focus of the present systematic literature review was to evaluate the effectiveness of sleep interventions for athletes specifically aimed at improving performance and/or recovery outcomes. To the best of the authors’ knowledge, no research article to date has conducted a review based on these parameters. Hence, the primary aim of the present systematic review was to bridge this gap in knowledge by synthesizing data from selected studies and providing a critical analysis of their results and methodology. Additionally, as a natural extension of the findings generated by this systematic review, a secondary aim was to outline a possible sleep intervention for athletes, including recommendations for content, mode of delivery and evaluation.
2 Methods
2.1 Search Strategy
A systematic review was conducted based on the PRISMA guidelines [33]. Three electronic databases (PubMed, PsycINFO and Web of Science) were initially searched using Endnote X7.2.1 (Thomas Reuters, USA) in May 2016, with an updated search completed in September 2017. Searches were conducted using “any field” (PubMed and PsycINFO) and “title/keyword/abstract” (Web of Science; discrepancies in search fields are due to differences in available field options in Endnote) to identify publications that contained at least one term from each of the three categories of search terms used: (1) athlet*/sport, (2) AND Sleep education/sleep extension/nap*/sleep therapy, (3) AND performance/competition/recovery/sleepiness/fatigue.
2.2 Inclusion/Exclusion Criteria
For studies to be included, they needed to implement an intervention aimed at improving (1) sleep (i.e., could be a part of the intervention or affected as a consequence of the intervention) and (2) performance/recovery/sleepiness/fatigue. Samples were required to consist of competitive athletes or sports players (from amateur through to elite levels), with a mean participant age of 18 years or older. Articles needed to be published in English and be peer reviewed.
Articles were excluded if they presented a review article or case study, focused on medication (due to the strict stance on anti-doping regulations making it beneficial for athletes to abstain from medication where possible [34]), or focused on sleep apnea (a medical disorder applying to a subset of athletes and simultaneously affecting both sleep and performance [35]). No study was excluded based on study quality.
2.3 Study Selection
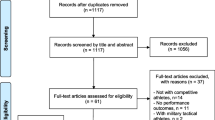
Study selection was completed between May and June 2016 and in September 2017 by authors DB and KB, with CL consulted as required. In total, 1438 studies were retrieved and 591 remained after duplicates were removed by EndNote’s auto-deduplication function (followed by a manual check). A further three studies were identified for potential inclusion through reference searches of relevant studies, which brought the total to 594. After titles and abstracts were screened, 562 studies were initially excluded, which left 32. Forward searching of these identified an additional three potentially relevant studies. Thirty-five full texts were analyzed, with a further 25 studies excluded due to not meeting the inclusion criteria (e.g., performance measures were not assessed and/or reported for all assessment time points). Thus, a total of ten studies were included in the final review (Fig. 1 represents a detailed flow chart of the study selection), nine of which were identified via the original search and one via the updated search.
2.4 Quality Assessment
The methodological quality of included studies was assessed using a modified version of the quality assessment scale developed by Abernethy and Bleakley [36] (see Table 1 for a description of the quality scoring key). The scale was used to assess the quality of study design; description of the participants, intervention, and outcome measures; blinding of assessors and measurement period.
One item of the original tool was omitted, as it was not relevant for any of the included studies (i.e., none of the studies appeared to have attrition, which the item aimed to evaluate). Wording of items and/or item responses (question numbers 1, 4, 5, 6, 8, 9 in the original scale) were altered to increase relevance of items for included studies (i.e., the original scale aimed to evaluate randomized controlled trials, but none of the included studies used this study design).
Authors DB and KB conducted the assessment independently, with CL consulted as required to obtain consensus in cases of uncertainty (i.e., [37] (item 8); [28] (item 1); [38] (item 6). Included studies were scored 0, 1, or 2 for each of the eight scale items with a maximum total score of 16 points. Overall quality scores were converted to a percentage value and rated (0–49% = poor, 50–89% = moderate, and > 90% = good [36]). Raters were not blind to study authors, place of publication or results.
3 Results
3.1 Study Characteristics
Detailed information was extracted from the ten studies that met the inclusion criteria for this review (see Table 2). Included studies were reviewed based on the following characteristics: population (i.e., country, age, sample size, sex, sport), method (i.e., intervention, design, measurements of sleep and performance), and results (i.e., sleep and subsequent performance and/or recovery outcomes). Sample populations consisted of athletes from a small number of countries (n = 6), with a narrow age range (18–24 years; mean = 21.41), from at least five different types of sports (not all studies reported this sample characteristic). Furthermore, the number of participants per study ranged from 6 to 84. Seven out of ten studies used male athletes only [19, 27, 37, 39,40,41,42]. In terms of methodology, included studies implemented interventions that either used sleep extension or napping, sleep hygiene, or a post-exercise recovery strategy that affected sleep as a consequence. Usually, a mixed design (randomized and counterbalanced) or a within-subjects design was employed, with a wide range of sleep, performance and recovery measures (i.e., subjective vs. objective). As per the inclusion criteria, all studies reported the results of their sleep interventions in relation to subsequent performance and/or recovery outcomes.
3.2 Sleep Extension and Napping
3.2.1 Total Sleep Duration
Two studies investigated the effect of increasing athletes’ total sleep duration on general and sport-specific performance measures. Mah et al. [19] compared a 2- to 4-week habitual sleep–wake schedule with a subsequent 5- to 7-week sleep extension phase in a sample of college varsity basketballers. During the sleep extension phase, participants were instructed to obtain as much nocturnal sleep as possible and spend a minimum of 10 h in bed each night. Napping was also encouraged. Results showed that participants’ objective sleep duration increased from an average of 6.6–8.4 h (approximately 110.9 ± 79.7 min) with a corresponding reduction in self-reported daytime sleepiness (mean = 9.64 ± 3.8 vs. 3.36 ± 1.69). With regard to performance and mood measures, results showed improvements in sprint times (mean = 16.2 ± 0.61 vs. 15.5 ± 0.54 s), free throw and 3-point shooting accuracy (mean = 9 and 9.2%, respectively), reaction times as measured by the psychomotor vigilance task (mean = 310.84 ± 77.13 vs. 274.51 ± 42.01 ms), and mood state (mean = 13.76 ± 17.17 vs. − 10.36 ± 9.62) and fatigue levels (mean = 8.24 ± 5.28 vs. 1.45 ± 2.46).
Schwartz and Simon [43] conducted a similar study to Mah et al. [19], but the former used a shorter intervention period. In their sample of college varsity tennis players, a 1-week habitual sleep–wake schedule was compared to a 1-week sleep extension period. During the sleep extension phase, participants were instructed to obtain at least 9 h of sleep per day, including naps. Results showed that participants’ subjective sleep duration increased from an average of 7.14–8.85 h (approximately 102 min), with a corresponding reduction in daytime sleepiness and improved objective serving accuracy in a non-competition setting (mean = 14.3% increase from pre- to post-intervention). In summary, the findings suggest that a minimum of 1-week of increased sleep duration leads to improvements on a range of performance measures among sleep deprived athletes.
3.2.2 Napping
Two studies explored the effect of napping on performance and/or recovery outcomes in athletes. Davies et al. [37] evaluated the effectiveness of 90-min daytime naps as a recovery tool from endurance training, which specifically included optimal circadian timing and the interval time between training and naps. With respect to circadian timing, results showed greater slow-wave sleep duration for the 11:30 a.m. naps compared to the 10:30 a.m. naps. However, no differences were noted for any other sleep parameters or measures of subjective alertness and preparedness to train post-nap. In terms of interval timing between training and naps, a post training nap taken 2 h after benefited preparedness to train compared to the 1-h post-training nap. No other differences for any variables were found.
In a more recent study, Petit et al. [41] investigated possible beneficial effects of a 20-min post-lunch nap on a subsequent bike ergometer sprint test and night-time sleep during a simulated jet-lag condition (5 h advanced). Results showed that napping among non-regular nappers induced longer sleep onset times during the post-trial night, although this was reduced in the sleep deprivation condition. They also found that a 20-min post-lunch nap did not improve maximum exercise performance, either before or after the simulated jet-lag condition.
The current evidence suggests that naps taken later in the day and at an appropriately timed interval after previous exercise may positively influence an athlete’s mental disposition towards subsequent performance tasks. However, a 20-min nap may be too short to influence subsequent performance measures among partially sleep-deprived athletes, and may also disturb sleep on the subsequent night for some athletes.
3.3 Sleep Hygiene
Three studies examined the effect of sleep hygiene practices on sleep and subsequent performance and/or recovery outcomes in athletes. Fullagar and colleagues [40] compared acute sleep hygiene strategies with a normal post-game routine following a late-night match in a sample of highly trained amateur soccer players. Participants in the intervention condition were instructed to go to their bedroom at 11:45 p.m., in a dimly lit and cool environment, with optional sleeping aids (e.g., ear plugs), no access to technology 15–30 min prior to bedtime, and a lights-out time of 12 a.m. In contrast, participants in the control condition maintained their usual activities but were not permitted to have a lights-out time until 2 a.m. (average bedtime following night matches). Results showed that participants in the intervention condition achieved greater sleep duration, but with more wake-episodes, compared to those in the control condition on match night. There was no difference in sleep onset latency or efficiency. However, this lack of differences could be due to the lack of an adequate control group. That is, the 2 a.m. bedtime for the control group may have resulted in increased sleep pressure, thus decreasing sleep latency, increasing sleep efficiency and shortening total sleep. Despite longer sleep duration in the intervention condition, there were no improvements in physical performance (i.e., CMJ, Yo–Yo intermittent recovery level 2 test), perceptual recovery (i.e., short version of the Acute Recovery and Stress Questionnaire), or levels of blood borne markers indicative of muscle damage and inflammation (i.e., C-reactive protein, creatine kinase, and urea).
Extending the findings of acute sleep hygiene strategies, Harada and colleagues [27] employed a longer sleep hygiene intervention over a period of 1 month. The 85 university soccer players received a leaflet that outlined eight different sleep hygiene recommendations (e.g., decreasing technology use at night). Results revealed that participants implementing more sleep hygiene changes were found to show greater subjective improvement in soccer performance. At the 3-month follow-up, participants had better sleep quality compared to baseline. Participants shifting towards an earlier chronotype (i.e., morning types) throughout the intervention period also reported significant improvements in their soccer performance.
Ryswyk et al. [42] implemented a 6-week sleep program in a team of Australian Rules Football players. At the beginning of the program, a qualified sleep physician provided a 1-h sleep education session that outlined sleep hygiene practices, including techniques on how to achieve increased sleep duration and quality. Weekly electronic feedback was provided (e.g., sleep duration averages) and a mid-program education and feedback session was also conducted. Individual consultations with the sleep physician were offered to clarify any further questions. Results showed no improvements for objective measures of participants’ sleep, although subjective benefits for sleep duration and efficiency were found. Furthermore, subjective daytime sleepiness, sleep quality and chronotype were unaffected. With respect to performance and mood measures, no benefits were observed for the psychomotor vigilance task; however, fatigue (mean = 6.2 ± 3.5 vs. 4.1 ± 3.8) and vigor (mean = 11.6 ± 6.4 vs. 15.9 ± 4.9) improved from pre- to post-intervention.
3.3.1 Sleep Hygiene and Circadian Adjustment
One study combined sleep hygiene with bright light therapy. Fowler et al. [39] investigated whether sleep hygiene strategies combined with bright light therapy mitigated the negative effects of international air travel on physical performance. In their study, all participants completed 24 h of simulated international air travel (i.e., a normobaric, hypoxic room was used to simulate the mild hypoxia and cramped conditions of typical commercial air travel). In the intervention condition, bright light therapy and sleep hygiene strategies were implemented during travel and 2 days post-travel, while the control condition maintained a typical travel routine for the entire 3 days. Results revealed no benefits for sleep duration at any time point for the intervention condition, but participants did show improved subjective sleep quality on day one post-travel. On day two post-travel, participants in the intervention condition reported reduced fatigue, while those in the control condition reported increased subjective jet-lag symptoms and poorer mood states. In contrast, no differences were reported for any performance measures (i.e., reaction time, Yo–Yo intermittent recovery level 1 test, 20-m sprint, loaded and unloaded countermovement jump [CMJ]).
3.3.2 Summary
Overall, it appears that acute sleep hygiene strategies increase athletes’ sleep duration, but not subsequent performance and recovery. In contrast, long-term sleep hygiene implementation might prove to be more beneficial. Furthermore, sleep hygiene in addition to bright light therapy seems to reduce the negative effects of jet lag to a small extent.
3.4 Post-exercise Recovery Strategies to Improve Nocturnal Sleep
Based on the idea that good quality sleep at nighttime is a key contributor to athletes’ recovery and performance, two studies implemented post-training recovery strategies to improve athletes’ sleep and assessed subsequent performance/recovery. Schaal and colleagues [28] implemented their recovery strategy among synchronized swimmers during an intensified training period. In a randomized cross-over design, participants received either daily dry air whole-body cryostimulation over 2 weeks, or no recovery strategy (control condition). After a taper period, participants switched conditions. Sleep actigraphy results showed that most sleep parameters (i.e., sleep duration, onset, and efficiency, but not quality) were preserved in the whole-body cryostimulation condition but deteriorated in the control condition. The physiological response to exercise was improved in the whole-body cryostimulation condition (i.e., reduced blood lactate, heart rate, alpha-amylase) indicating reduced physical fatigue. However, it remains unclear if this is a direct effect of the whole-body cryostimulation or due to longer sleep durations and efficiency.
In contrast to Schaal et al. [28], Zhao et al. [38] implemented their recovery strategy during a regular training period. In a sample of female basketball players, participants received either red light irradiation every night for 30 min or a placebo non-red light irradiation over 2 weeks. Results showed that participants in the intervention condition demonstrated improved subjective sleep quality (Pittsburgh Sleep Quality Index), but also higher morning serum melatonin levels compared to placebo (the latter aspect might be an indication of a circadian delay induced by the red light). With respect to performance, there was a trend showing that participants in the intervention group improved on the distant running task (Cooper 12-min run), whereas no change was observed in the placebo group. At this point it remains unclear whether the red-light irradiation had a direct effect on post-training recovery, or whether improved sleep led to a greater overall recovery. One can also speculate that the better post-intervention running results were a consequence of the circadian shift, in that the assessment now took place in a circadian peak-performance phase (i.e., a time when the testing was more suited to the timing of the body clock).
In summary, two studies applied post-training recovery strategies, aimed at inducing a number of physiological effects thought to be beneficial for recovery, sleep initiation, and sleep maintenance (e.g., enhanced parasympathetic reactivation). Results revealed a positive influence on subjective and objective sleep patterns, and minor improvements in performance measures.
3.5 Quality Assessment
Table 3 describes study quality scores in relation to the quality scoring key (see Table 1). Overall, one study achieved a good quality rating, eight studies received a moderate quality rating, and one study was determined to have a poor-quality rating. Most studies (6/10) employed a mixed design, randomized and counterbalanced between conditions. Alternatively, a within-subjects design was used. These common study designs also allowed most studies to have groups which were comparable at baseline. Adequate descriptions of inclusion/exclusion criteria were lacking in some studies; however, intervention and outcome measures were generally well defined, and the study duration was often adequate. This was largely due to the temporal nature sleep has on performance, thus long follow-up periods were not required. Zhao and colleagues [38] concealed the intervention to participants prior to allocation; however, for all other studies concealment of allocation was either unclear, impossible, or not reported. In turn, assessors were only blind to treatment in one study [37].
Thus, overall, quality of studies could generally be improved by ensuring the use of randomization and a crossover study design, concealing the intervention to participants and assessors where possible, designing plausible placebo treatments for comparison, and including consistent and clear reporting of inclusion and exclusion criteria.
4 Discussion
4.1 Interventions Targeting Sleep and Subsequent Performance on Athletes
This is the first systematic literature review to summarize and evaluate intervention studies that aimed to improve the sleep and subsequent performance and/or recovery outcomes of athletes. To this end, ten studies with a total of 218 participants in the age range of 18–24 years were identified. Consistent with previous research, the results suggest that sleep plays an important role in some, but not all, aspects of athletes’ performance and recovery [3, 44]. This finding not only supports the previously established relationship between sleep, performance and recovery, but it also reinforces the need for athletes to have access to knowledge and skills which enables them to effectively manage their sleep.
Extending the amount of sleep athletes obtain, through either nocturnal sleep or napping, appears to improve sports-specific skill execution and cognitive related tasks, such as reaction time and shooting accuracy. Positive effects were also found for improved mood and reduced daytime sleepiness. This finding is in line with research on partial sleep deprivation, indicating impaired cognitive functioning and mood in particular, which may lead to poorer overall performance. Poor mood states have been linked to over-reaching and over-training [9, 10]. Moreover, psychological fatigue would appear to create a neurocognitive state detrimental for either optimal decision making (e.g., in team ball games) or maintaining a high level of motivation (e.g., running a marathon) [3]. The positive findings of the prolonged sleep-extension period (5–7 weeks of 10 h of time-in-bed) among college basketball players [19] support the assumption that athletes require 9–10 h of sleep [18]. However, it remains unclear as to how much additional sleep is sufficient to produce these outcomes, as sleep needs vary considerably between individuals [45]. Furthermore, it also needs to be investigated how athletes experience possible wakefulness in bed during sleep extension periods. This may be particularly relevant on nights preceding competition when athletes are prone to worry [25]. Thus, although these findings suggest that sleep extension is a promising intervention for improving athletes’ performance, the appropriate amount for each individual needs to be defined, rather than a one size fits all approach of 10 h in bed.
Currently, sleep hygiene is not recommended as a standalone treatment for behavioral sleep problems [46, 47]. However, research among athletes has shown that sleep hygiene improves self-rated sports performance and can assist in moving the body clock earlier, which may help with early morning training and competitions [27]. Therefore, introducing sleep hygiene among athletes may encourage earlier bedtimes, thus lengthening sleep duration and subsequently further improving performance. However, the studies that evaluated sleep hygiene were somewhat vague as to the precise strategies that were employed and how many were taken up by athletes. Furthermore, athlete individual differences (e.g., motivation) that influenced whether such strategies were adopted are also unknown. Hence, it is difficult to draw conclusions as to which strategies and individual differences are most relevant and important for athletes in general and for different sports.
Studies investigating recovery strategies produced less conclusive results than sleep extension and sleep hygiene, mainly due to methodological shortcomings. The study by Zhao and colleagues [38] showed improved sleep and subsequent performance following red light irradiation in the evening. The authors proposed that an increase in melatonin secretion caused by the red-light irradiation may have facilitated increased sleepiness. Yet, it is also possible that the evening light induced a delay in circadian rhythm timing (later bed- and rise-times), as indicated by increased morning melatonin levels post-intervention. Hence, improved running performance post-intervention may have occurred due to assessment taking place in a circadian peak-performance phase (i.e., a time when the testing was more suited to the timing of the body clock).
A second recovery strategy reviewed here involved whole-body cyrostimulation, which consists of acute exposure to very cold air in special cryochambers [28]. The authors hypothesized that whole-body cryostimulation may decrease the negative effects of over-reaching on sleep and performance, via enhanced post-exercise parasympathetic re-activation at the cardiac level. However, while the current literature supports an association between poor sleep and functional overreaching in athletes, it remains unclear whether decreased sleep quality is a cause or a symptom of overreaching [48]. Overall, further investigation is required to determine the efficacy of these interventions before they are recommended as sleep promoting strategies.
Overall, it is important to note that the vast majority of research has investigated the impact of total sleep deprivation on performance measures. However, athletes are more likely to face partial sleep deprivation (e.g., a bad night’s sleep, jet lag) rather than not attempting sleep for long periods (e.g., one night and day [3]). This is an important consideration towards the generalization of interpretation of intervention outcomes. While reduced aerobic exercise and maximal measures of strength have been shown to be impaired by total sleep deprivation, this is not the case for partial sleep deprivation. Hence, this may explain why sleep extension strategies did not show improvements on aerobic exercise bouts and maximal strength. In contrast, sports-specific skill execution, submaximal sustained exercise bouts, and muscular and anaerobic power have been shown to be impaired by partial sleep deprivation [3, 4, 44]. This pattern of results was confirmed among our reviewed studies. In other words, the reported performance improvements were mainly present in areas that are impaired by partial, but not total, sleep deprivation. Hence, future studies targeting athletes’ recovery and performance through improved sleep should focus on performance measures that are most likely to be impaired by poor sleep as present in an athlete’s real-life.
It is also worth noting that four out of ten studies had a sample size ≤ 15, which makes it difficult to generalize conclusions to a broader set of athletes (e.g., individual vs. team sport, type of sport, collegiate vs. Olympic athletes). Given that the heterogeneous nature of the population itself makes it hard to draw conclusions, it is particularly important that future studies aim to use larger sample sizes. Moreover, most studies reviewed in the current paper (7/10) used samples comprising male athletes only, while one was mixed and two were female athletes only. Hence, there is a clear reporting bias toward the inclusion of male athletes. Consequently, potential sex differences cannot be properly evaluated and accounted for when developing sleep interventions for athletes. This point is of particular relevance given that in the general sleep literature, females report poorer sleep outcomes compared to males, meaning there is a differential risk for sleep disturbance [49]. To address this methodological issue, future research investigating sleep interventions for athletes should make more effort to include females, which will help to ensure that the efficacy of sleep interventions is adequately investigated in the full range of athletes who receive these interventions.
A strength of the current literature review was that, to the best of the authors’ knowledge, it was the first to evaluate sleep intervention studies that used only athlete samples. However, it should be recognized that samples from included studies comprised athletes involved in amateur through to elite levels of competition. There are a number of differences between these types of athletes (e.g., time commitment) that may influence the capacity to generalize findings from amateur to elite athletes. Furthermore, not all athletes are representative of one another (e.g., gymnasts vs. team athletes). Hence, future research should aim to incorporate samples of elite athletes and endeavor to evaluate sleep interventions in a range of athletes and types of sports.
In summary, the studies included in the present review highlight novel approaches designed to help athletes in specific sports manage their sleep. Instead of focusing on the detrimental effects of sleep loss, the studies emphasize not only the importance of sufficient sleep for recovery and performance in athletes, but also highlight feasible strategies to promote sleep. However, and not unexpectedly, a general conclusion about the multiple, differing sleep needs of athletes during individual training and competition schedules cannot be drawn. Thus, we argue for the development of an intervention framework that incorporates individual therapeutic strategies known to be effective for improving athletes’ sleep, which can be delivered to athletes as a holistic program.
4.2 Designing a Sleep Intervention for Athletes
The idiosyncratic nature of sleep that athletes experience, as specified in Sect. 1 of this review, necessitates an eclectic approach to intervention planning and delivery. Specifically, the present review has identified the need to develop a more comprehensive sleep intervention for athletes. In accordance with the second aim of this paper, an outline for a potential athlete sleep intervention is provided below, which is based upon and extends the findings of the present review.
4.2.1 Mode of Delivery
An ideal athlete sleep intervention program should aim to address the individual needs of athletes. The aim of such a program would be to both prevent sleep loss during extensive training periods and prior to important competitions as well as to improve sleep parameters. Content would include a combination of educational material, motivational tasks, and cognitive and behavioral strategies delivered in a series of seminar-type classes by a trained sleep educator (see Table 4 for a suggested structure). A similar mode of delivery has previously been successfully implemented in schools [50]. It therefore stands to reason that using this type of framework, but with athlete-specific content, may be effective for improving the sleep of elite athletes. The educational component, at a minimum, should also involve coaches and other team management staff [51]. Classes would be approximately 1 h in length and held once per week for 4 consecutive weeks. As the benefits of improved sleep on performance apply to all athletes, not only to those with clinical sleep disorders, it is suggested that the sleep program would be delivered to all athletes. Additionally, baseline and follow-up assessments would not only provide feedback on the effectiveness of the delivered program, but also screen for athletes with sleep problems that require individualized treatment (e.g., pre-competition anxiety, general insomnia symptoms, obstructive sleep apnea). This approach prevents an overload of the educational contents provided for all athletes, yet identifies individuals in need for further treatment.
4.2.2 Assessment
Self-report measures of sleep, such as sleep diaries, and, where possible, objective measures such as actigraphy (set to high sleep–wake threshold [52]) should be used for both assessment and monitoring of sleep pre-, during, and post-intervention. Monitoring of sleep, via a sleep diary and actigraphy, should commence at least 1 week prior to the first session, including regular training and competition days. A sleep questionnaire specific to athletes, such as the Athlete Sleep Screening Questionnaire [53], may be used at the beginning of the first session to identify sleep disturbance, sleep related impairment, and the extremely difficult to screen sleep behaviors of athletes given their lifestyle, the demands of training and travel associate with international competition. Athletes identified through this questionnaire as having abnormal sleep could then receive additional treatment, specific to their sleep disorder.
4.2.3 Sleep Education
Knowledge acquisition is essential to the process of making sleep related behavioral change. Indeed, this is the reason why sleep education is a cornerstone of treatments for clinical sleep disorders such as insomnia [54]. Surprisingly, there was a notable lack of sleep education material present in the studies reviewed. Although some education was provided in the form of sleep hygiene recommendations, information pertaining to other areas of sleep knowledge that may be relevant and useful to athletes (e.g., common sleep issues in athlete populations) was omitted.
Sleep education content should focus on the nature of sleep, common sleep issues faced by athletes, importance of sleep for optimal performance/recovery [42], and methods to improve overall sleep. It should be noted that realistic expectations about sleep should be clearly established, so as not to create worry amongst athletes regarding individual differences. Preferably, content would be sport specific, to increase relevance and therefore engagement and interest for athletes. A work booklet or mobile phone application could be used to complement sleep education provided to athletes in light of the study by Harada et al. [27] showing that sleep hygiene information provided over a longer period of time was helpful.
4.2.4 Motivation
A search of the literature revealed no published research to date investigating the level of motivation in athlete populations to make sleep related behavioral change. Despite an absence of formal evidence, the possibility of athletes being ambivalent to this type of change, and that sleep education alone may be an insufficient motivator, should not be discounted. Ambivalence could potentially develop due to having to make a decision between sleep interfering behaviors that are rewarding in the short term, and opposing healthy sleep choices that are perceived to be less appealing [51]. For example, on the night following a competitive event, some athletes may prefer to stay out late to socialize and consume alcohol, rather than prepare for an early night to obtain adequate sleep quantity and quality to aid recovery. In contrast, coaches may favor additional early morning training sessions to increase frequency of training; yet, and in particular for adolescent athletes, sleep duration is often the first thing to be cut as both training and homework load peak during high school years, which may limit the effectiveness of training [55]. Hence, there may be a need to consider motivation levels for behavioral change, on both the athlete and coach level, when delivering a sleep intervention.
One therapeutic modality that could be used to promote sleep-related behavioral change in athletes is motivational interviewing (MI). The overarching aim of MI is to enhance intrinsic motivation by reducing ambivalence to change [56]. MI has been used in clinical settings with both individuals and groups [57] across a range of domains, including sleep [50]. With respect to athletes, the key to reducing ambivalence would be to help them evaluate how the consequences of engaging in sleep interfering behaviors are inconsistent with the goal of achieving success, due to the negative impact of reduced sleep on performance and recovery. A decisional matrix is one example of an MI technique that assists individuals in identifying the pros and cons for both changing and maintaining an unhelpful behavior [58].
4.2.5 Behavioral Strategies
In regards to behavioral strategies, sleep extension, particularly through increasing nocturnal sleep, has provided the most consistent evidence for improving sleep and subsequent physical performance, as well as decreasing daytime tiredness [19, 43]. Napping may also provide an appropriate means of extending sleep, thus improving performance, but this is likely dependent on the timing of the nap [37]. Thus, the suggested sleep intervention should work with athletes and coaches to strategize how increasing sleep opportunities may be feasible (e.g., by delaying morning training by 30 min to allow longer morning sleep, or how to facilitate earlier bedtimes). If extending nocturnal sleep is not possible, then napping at least 2 h post-training may provide the most benefit in terms of motivation to train a second time later that day.
Of note, sleeping-in on weekends, although allowing extended sleep, should be limited to within 1 h of normal weekday wake-up time. Sleeping-in dissipates sleep pressure, making it more difficult to fall asleep at the usual time the following night, as well as preventing exposure to morning bright light, which assists with circadian rhythm regulation. Combined, these two factors mean sleep that could be gained through a consistent earlier bedtime (between weekdays and weekends) is lost, and that waking for the next morning training session may be difficult. Although a regular wake time, extending to weekends, is recommended, athletes often face situations (e.g., travel, late night-games, pool lane hours), which make it hard to maintain a regular sleep schedule during particular times. Thus, it is important to work on alternatives, such as choosing appropriate nap times, or preparing an individual’s body clock for a travel across time zones.
Furthermore, good sleep hygiene involves easy to implement techniques, such as making sure the bedroom environment is a comfortable temperature, dark and quiet (e.g., by providing earplugs and eye masks), restricting physically, cognitively and emotionally stimulating activities prior to bed (e.g., plan wind-down time after late-night games), and using dim light up to 2 h prior to bedtime. Extending from the findings of the studies included in the current review, implementation of these measures consistently over 1–3 months will likely result in sleep and performance benefits [27]. Practicing these techniques requires no specialized training or equipment, and they are relatively easy to employ both at home and when away for competition. Thus, good sleep hygiene is recommended as beneficial for athletes, and should be discussed early on in a sleep intervention program.
4.2.6 Cognitive Strategies
No studies included in the present review evaluated cognitive techniques for improving sleep and subsequent performance/recovery outcomes. Nevertheless, it is well established that athletes often worry whilst in bed at various times during training and competition schedules (e.g., the nights preceding a competition [25]). Cognitive models suggest that worry can activate the sympathetic nervous system, thereby increasing physiological arousal and delaying sleep onset. Moreover, exercise adaptation and recovery requires parasympathetic activation. Hence, introducing techniques that reduce the dominance of the sympathetic nervous system response is necessary for any comprehensive athlete sleep intervention. There are several methods by which athletes could be taught to manage worry that are consistent with cognitive therapy approaches. Initially, athletes should be assisted in identifying unhelpful worry strategies they may be currently using (e.g., pre-sleep competition worries). Subsequently, athletes should be provided with a range of alternative, more helpful worry strategies, such as using thought records to deal with negative automatic thoughts [54], progressive muscle relaxation [32], and imagery [58].
4.2.7 Travel and Adjustment of Circadian Rhythms
The circadian rhythm regulates times of alertness and sleep. Moreover, deep sleep assists in recovery, hence obtaining sufficient sleep is vital for athletes for optimal performance. With this in mind, it stands to reason that traveling across multiple time zones will disrupt an athlete’s circadian rhythm and alter performance. Additionally, as the body is synchronized to sleep at night, and wake during the day, sleep needed for recovery and optimal performance at the destination time may be impaired [39].
Athletes who are traveling across multiple time zones can minimize the negative effects of circadian rhythm misalignment through non-pharmacological interventions. These include appropriately timed bright light and sleep hygiene [39]. The timing of bright light is complex, yet is relative to an athlete’s core body temperature minimum, as well as in which direction they are traveling (i.e., eastward vs. westward). Moreover, evening light, such as that used during red light irradiation [38], may delay the circadian rhythm. Although we cannot recommend evening light as a means to promote sleep and performance in general, evening light to delay circadian rhythm timing may benefit athletes in the lead up to a competition, to allow the competition to occur during a peak-performance phase.
4.2.8 Evaluation
For best practice, program evaluation should occur via a randomized, mixed-design experiment, whereby one group (including athletes and their management team) are allocated to receive the intervention, and the other group are allocated to a waitlist or control (e.g., a group which receives minimal sleep education, and no information on how to improve sleep). Figure 2 displays a flow chart detailing how the program could be evaluated. To evaluate the impact of the intervention on sleep, it is recommended that sleep diaries (i.e., a daily self-report measure) are used, in conjunction with actigraphy or polysomnography (i.e., an objective measure of sleep). Measurement of sleep needs to commence in the week preceding the first session, to obtain a valid baseline assessment. Sleep should be measured throughout the intervention period, to monitor and assess changes to sleep parameters such as bedtime, sleep duration, sleep timing or sleep quality.
Performance should be evaluated using sports specific outcome measures which tap into multiple domains of performance, including those which assess single bouts of aerobic exercise, maximal measures of strength, sports-specific skill execution, submaximal sustained exercise bouts, and muscular and anaerobic power, cognitive processes (e.g., reaction time, fine motor movement, memory, and decision-making), and mood. Thus, the impact of any improvements to sleep could be ascertained. Furthermore, performance during competitions should also be evaluated whenever possible to include more meaningful outcome variables. A sleep questionnaire, specific to athletes, should also be used at baseline and post-intervention to measure improvements in the diagnosis of clinical sleep disorders or improvements in sleep habits. A follow-up period, with measurements taken at 1 and 3 months, would also allow for the assessment of change over a longer time-period, and whether possible sleep intervention effects on sleep and performance persist in the long term.
5 Conclusion
Insufficient sleep can have significant effects on athletic performance, with a particular decline in sports-specific skill execution and submaximal sustained exercise bouts. From the reviewed articles, it appears that athletes benefit from both sleep extension and sleep hygiene strategies, while studies on recovery strategies produced less conclusive results. Thus, future sleep intervention programs in athletes should provide an eclectic approach to intervention planning and delivery to address athletes’ often unique sleep–wake behaviors and disruptions.
References
Harries SK, Lubans DR, Callister R. Systematic review and meta-analysis of linear and undulating periodized resistance training programs on muscular strength. J Strength Cond Res. 2015;29:1113–25. https://doi.org/10.1519/JSC.0000000000000712.
Spriet LL. Nutritional support for athletic performance. Sports Med. 2015;45:S3–4. https://doi.org/10.1007/s40279-015-0402-z.
Fullagar HHK, Skorski S, Duffield R, et al. Sleep and athletic performance: The effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015;45:161–86. https://doi.org/10.1007/s40279-014-0260-0.
Halson SL. Recovery techniques for athletes. Sport Sci Exch. 2013;26:1–6. https://doi.org/10.1136/jmg.2003.014902.
Brand S, Beck J, Gerber M, et al. “Football is good for your sleep”: favorable sleep patterns and psychological functioning of adolescent male intense football players compared to controls. J Health Psychol. 2009;14:1144–55. https://doi.org/10.1177/1359105309342602.
Samuels C. Sleep, recovery, and performance: the new frontier in high-performance athletics. Phys Med Rehabil Clin N Am. 2009;20:149–59. https://doi.org/10.1016/j.pmr.2008.10.009.
Venter RE. Perceptions of team athletes on the importance of recovery modalities. Eur J Sport Sci. 2014;14:1–8. https://doi.org/10.1080/17461391.2011.643924.
Reilly T, Edwards B. Altered sleep-wake cycles and physical performance in athletes. Physiol Behav. 2007;90:274–84. https://doi.org/10.1016/j.physbeh.2006.09.017.
Coutts AJ, Reaburn ÆP, Piva ÆTJ, et al. Monitoring for overreaching in rugby league players. Eur J Appl Physiol. 2007;99:313–24. https://doi.org/10.1007/s00421-006-0345-z.
Jürimäe J, Mäestu J, Purge P, et al. Changes in stress and recovery after heavy training in rowers. J Sci Med Sport. 2004;7:335–9. https://doi.org/10.1016/S1440-2440(04)80028-8.
Halson SL. Nutrition, sleep and recovery. Eur J Sport Sci. 2008;8:119–26. https://doi.org/10.1080/17461390801954794.
Shapiro CM, Bortz R, Mitchell D, et al. Slow-wave sleep: a recovery period after exercise. Science. 1981;214:1253–4. https://doi.org/10.1126/science.7302594.
Obal F, Krueger JM. GHRH and sleep. Sleep Med Rev. 2004;8:367–77. https://doi.org/10.1016/j.smrv.2004.03.005.
Skein M, Duffield R, Edge J, et al. Intermittent-sprint performance and muscle glycogen after 30 h of sleep deprivation. Med Sci Sports Exerc. 2011;43:1301–11. https://doi.org/10.1249/MSS.0b013e31820abc5a.
Costill DL, Flynn MG, Kirwan JP, et al. Effects of repeated days of intensified training on muscle glycogen and swimming performance. Med Sci Sports Exerc. 1988;20:249–54. https://doi.org/10.1249/00005768-198806000-00006.
Ferrara M, De Gennaro L. How much sleep do we need? Sleep Med Rev. 2001;5:155–79. https://doi.org/10.1053/smrv.2000.0138.
National Sleep Foundation. National Sleep Foundation 2013 poll [Internet]. 2013. https://www.sleepfoundation.org/2013pol. Accessed 13 Jan 2018.
Calder A. Recovery strategies for sports performance. Strategies. 2002;15:8–11.
Mah CD, Mah KE, Kezirian EJ, et al. The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep. 2011;34:943–50. https://doi.org/10.5665/sleep.1132.
Mah CD, Mah KE, Dement WC. Athletic performance and sleep extension in collegiate tennis players. Sleep. 2009;32:A155.
Gupta L, Morgan K, Gilchrist S. Does elite sport degrade sleep quality? A systematic review. Sports Med. 2016; pp 1–17. https://doi.org/10.1007/s40279-016-0650-6.
Pedersen DJ, Lessard SJ, Coffey VG, et al. High rates of muscle glycogen resynthesis after exhaustive exercise when carbohydrate is coingested with caffeine. J Appl Physiol. 1985;2008(105):7–13. https://doi.org/10.1152/01121.2007.
Fietze I, Strauch J, Holzhausen M, et al. Sleep quality in professional ballet dancers. Chronobiol Int. 2009;26:1249–62. https://doi.org/10.3109/07420520903221319.
Leeder J, Glaister M, Pizzoferro K, et al. Sleep duration and quality in elite athletes measured using wristwatch actigraphy. J Sports Sci. 2012;30:541–5. https://doi.org/10.1080/02640414.2012.660188.
Erlacher D, Ehrlenspiel F, Adegbesan OA, et al. Sleep habits in German athletes before important competitions or games. J Sports Sci. 2011;29:859–66. https://doi.org/10.1080/02640414.2011.565782.
Silva A, Queiroz SS, Winckler C, et al. Sleep quality evaluation, chronotype, sleepiness and anxiety of Paralympic Brazilian athletes: Beijing 2008 Paralympic Games. Br J Sports Med. 2012;46:150–4. https://doi.org/10.1136/bjsm.2010.077016.
Harada T, Wada K, Tsuji F, et al. Intervention study using a leaflet entitled ‘Three benefits of “Go to bed early! Get up early! And intake nutritionally rich breakfast!” a message for athletes’ to improve the soccer performance of university soccer team. Sleep Biol Rhythms. 2016;14:S65–74. https://doi.org/10.1007/s41105-015-0035-5.
Schaal K, Le Meur Y, Louis J, et al. Whole-body cryostimulation limits overreaching in elite synchronized swimmers. Med Sci Sports Exerc. 2015;47:1416–25. https://doi.org/10.1249/MSS.0000000000000546.
Morita Y, Ogawa K, Uchida S. Napping after complex motor learning enhances juggling performance. Sleep Sci. 2016;9:112–6. https://doi.org/10.1016/j.slsci.2016.04.002.
Pelka M, Kölling S, Ferrauti A, et al. Acute effects of psychological relaxation techniques between two physical tasks. J Sports Sci. 2016;pp 1–8. https://doi.org/10.1080/02640414.2016.1161208
Waterhouse J, Atkinson G, Edwards B, et al. The role of a short post-lunch nap in improving cognitive, motor, and sprint performance in participants with partial sleep deprivation. J Sports Sci. 2007;25:1557–66. https://doi.org/10.1080/02640410701244983.
McCloughan LJ, Hanrahan SJ, Anderson R, et al. Psychological recovery: progressive muscle relaxation (PMR), anxiety, and sleep in dancers. Perform Enhanc Health. 2016;4:12–7. https://doi.org/10.1016/j.peh.2015.11.002.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Ann Intern Med. 2009;151:264–9. https://doi.org/10.1371/journal.pmed1000097.
World Anti-Doping Agency. World Anti-Doping Code 2015. https://www.wada-ama.org/en/resources/the-code/world-anti-doping-code. Accessed 13 Jan 2018.
Emsellem HA, Murtagh KE. Sleep apnea and sports performance. Clin Sport Med. 2005;24:329–41. https://doi.org/10.1016/j.csm.2005.01.002.
Abernethy L, Bleakley C. Strategies to prevent injury in adolescent sport: a systematic review. Br J Sports Med. 2007;41:627–38. https://doi.org/10.1136/bjsm.2007.035691.
Davies DJ, Graham KS, Chow CM. The effect of prior endurance training on nap sleep patterns. Int J Sports Physiol Perform. 2010;5:87–97.
Zhao J, Tian Y, Nie J, et al. Red light and the sleep quality and endurance performance of Chinese female basketball players. J Athl Train. 2012;47:673–8. https://doi.org/10.4085/1062-6050-47.6.08.
Fowler PM, Duffield R, Morrow I, et al. Effects of sleep hygiene and artificial bright light interventions on recovery from simulated international air travel. Eur J Appl Physiol. 2014;115:541–53. https://doi.org/10.1007/s00421-014-3043-2.
Fullagar H, Skorski S, Duffield R, et al. The effect of an acute sleep hygiene strategy following a late-night soccer match on recovery of players. Chronobiol Int. 2016;528:1–16. https://doi.org/10.3109/07420528.2016.1149190.
Petit E, Mougin F, Bourdin H, et al. A 20-min nap in athletes changes subsequent sleep architecture but does not alter physical performances after normal sleep or 5-h phase-advance conditions. Eur J Appl Physiol. 2014;114:305–15. https://doi.org/10.1007/s00421-013-2776-7.
Van Ryswyk E, Weeks R, Bandick L, et al. A novel sleep optimisation programme to improve athletes’ well-being and performance. Eur J Sport Sci. 2016;1391:1–8. https://doi.org/10.1080/17461391.2016.1221470.
Schwartz J, Simon RD. Sleep extension improves serving accuracy: a study with college varsity tennis players. Physiol Behav. 2015;151:541–4. https://doi.org/10.1016/j.physbeh.2015.08.035.
Reilly T, Piercy M. The effect of partial sleep deprivation on weight-lifting performance. Ergonomics. 1994;37:107–15. https://doi.org/10.1080/00140139408963628.
Schneerson JM. Handbook of sleep. Cambridge: Blackwell Science; 2000.
Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29:1415–9.
Buysse DJ, Germain A, Moul DE, et al. Efficacy of brief behavioral treatment for chronic insomnia in older adults. Arch Intern Med. 2011;171:887–95. https://doi.org/10.1001/archinternmed.2010.535.
Meeusen R, Duclos M, Foster C, et al. Prevention, diagnosis and treatment of the overtraining syndrome: joint consensus statement of the European College of Sport Science (ECSS) and the American College of Sports Medicine (ACSM). Eur J Sport Sci. 2012;13:1–24. https://doi.org/10.1080/17461391.2012.730061.
Mallampalli MP, Carter CL. Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. J Womens Health (Larchmt). 2014;23:553–62. https://doi.org/10.1089/jwh.2014.4816.
Bonnar D, Gradisar M, Moseley L, et al. Evaluation of novel school-based interventions for adolescent sleep problems: does parental involvement and bright light improve outcomes? Sleep Health. 2015;1:66–74. https://doi.org/10.1016/j.sleh.2014.11.002.
Halson SL. Stealing sleep: is sport or society to blame? Br J Sports Med. 2016;50:381. https://doi.org/10.1136/bjsports-2015-094961.
Sargent C, Lastella M, Halson SL, et al. The validity of activity monitors for measuring sleep in elite athletes. J Sci Med Sport. 2016;19:848–53. https://doi.org/10.1016/j.jsams.2015.12.007.
Samuels C, James L, Lawson D, et al. The Athlete Sleep Screening Questionnaire: a new tool for assessing and managing sleep in elite athletes. Br J Sports Med. 2015; pp 1–5. https://doi.org/10.1136/bjsports-2014-094332.
Harvey AG, Sharpley AL, Ree MJ, et al. An open trial of cognitive therapy for chronic insomnia. Behav Res Ther. 2007;45:2491–501. https://doi.org/10.1016/j.brat.2007.04.007.
Sargent C, Halson S, Roach GD. Sleep or swim? Early-morning training severely restricts the amount of sleep obtained by elite swimmers. Eur J Sport Sci. 2014;14:S310–5. https://doi.org/10.1080/17461391.2012.696711.
Miller WR, Rollnick S. Motivational interviewing: helping people change. New York: Guildford Press; 2012.
Cassoff J, Knäuper B, Michaelsen S, et al. School-based sleep promotion programs: effectiveness, feasibility and insights for future research. Sleep Med Rev. 2013;17:207–14. https://doi.org/10.1016/j.smrv.2012.07.001.
Kaplan KA, Harvey AG. Treatment of sleep disturbance. In: Barlow DH, editor. Clinical handbook of psychological disorders. 5th ed. New York: Guilford Press; 2014. p. 640–69.
Author information
Authors and Affiliations
Contributions
Daniel Bonnar, Kate Bartel, Christin Lang, and Naomi Kakoschke conceived and designed the study. Daniel Bonnar and Kate Bartel performed the literature search, were responsible for decisions on inclusion/exclusion of articles, quality assessment and data extraction (with Christin Lang as the decider if there was disagreement). Naomi Kakoschke drafted and critically revised the study. Christin Lang and Daniel Bonnar wrote the Introduction section; Kate Bartel wrote the Methods section; Daniel Bonnar, Christin Lang, and Kate Bartel wrote the Results section; Daniel Bonnar, Kate Bartel, Christin Lang, and Naomi Kakoschke wrote the Discussion section.
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
Daniel Bonnar, Kate Bartel, Naomi Kakoschke, and Christin Lang declare that they have no conflicts of interest relevant to the content of this review.
Rights and permissions
About this article
Cite this article
Bonnar, D., Bartel, K., Kakoschke, N. et al. Sleep Interventions Designed to Improve Athletic Performance and Recovery: A Systematic Review of Current Approaches. Sports Med 48, 683–703 (2018). https://doi.org/10.1007/s40279-017-0832-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-017-0832-x