Abstract
Pediatric Crohn’s disease commonly presents with moderate-to-severe intestinal inflammation with a greater risk of complications if remission is not achieved. Anti-tumor necrosis factor therapies have offered the possibility of deep and durable remission; however, many children do not respond or no longer respond over time. Further, some children do not require broader systemic immunosuppression to achieve remission and are better served by an alternative treatment strategy. Proper utilization of advanced biologic and small-molecule therapies, which have become available for adult patients since anti-tumor necrosis factor medications, is paramount for tighter disease control for a large proportion of children. Newer advanced therapies such as anti-integrin and anti-interleukin biologics, and several small-molecule agents capitalize on various mechanisms through narrower immunologic targets and reduced immunogenicity. Given limited regulatory approvals of these agents for use in children with Crohn’s disease, clinicians continue to rely on data extrapolated from clinical trials in adult patients, sparse pediatric studies, and a growing real-world experience for treatment selection and optimization. In this article, we discuss currently available treatment options, pipeline drugs, and relevant data as they pertain to some of the most pressing clinical challenges faced in treating pediatric Crohn’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pediatric Crohn’s disease is associated with high rates of severe disease and complicated disease behavior requiring the use of biologic and small-molecule medications. |
Newer advanced therapies are becoming increasingly utilized off-label in children previously exposed, or naïve to, anti-tumor necrosis factor therapies in attempts to achieve more robust treatment targets while potentially minimizing adverse effects related to broad immunosuppression. |
The significant delay in dedicated pediatric clinical trials limits available efficacy and safety data available to the pediatric clinician to determine the optimal treatment selection and sequencing in children with Crohn’s disease. |
1 Introduction
Pediatric Crohn’s disease (PCD) is a chronic, immune-mediated gastrointestinal condition often requiring long-term immunosuppressive therapy. It is associated with a higher disease burden including increased rates of disease extension, development of penetrating and/or stricturing disease, perianal disease, and biologic use compared with adult counterparts [1,2,3]. Patients with PCD may also have increased rates of colorectal cancer in their lifetime because of an extended disease duration [2], and significant impacts in health-related quality of life have been reported [4]. In the absence of a long-term follow-up of untreated cohorts, the natural history of PCD is likely best represented by those who were treated only with 5-aminosalicylate and corticosteroids, when disease was often characterized by unchecked intestinal inflammation and subsequent malnutrition, growth failure, corticosteroid dependence, and multiple surgeries [5].
The discovery and widespread use of biologic medications, in particular anti-tumor necrosis factor (TNF) medications such as infliximab and adalimumab, have dramatically shifted the goalpost in treating PCD to allow for tighter disease control, with higher rates of disease response, remission, and more stringent treatment targets [6, 7]. Current clinical practice now often considers biologic therapies early in patients’ treatment course rather than a gradual step-up approach [8]. However, therapeutic success with anti-TNF medication is commonly tempered by a primary or secondary loss of response, or partial responses, and a wider side-effect profile related to having a broad immunologic target leading to greater immunosuppression, and its increased risk of immunogenicity [9, 10].
Immunomodulators have long been utilized in the management of Crohn’s disease (CD). Methotrexate in combination with anti-TNF especially in the setting of immunogenicity to establish therapeutic drug concentrations has been shown to be safe and efficacious in adults and children [11, 12]. Additionally, the use of azathioprine in combination with anti-TNF is well described [13, 14]. Anti-TNF in combination with azathioprine, while possibly effective, should be carefully considered owing to published data indicating an increased risk of lymphoma in children [15, 16]. This must be weighed against its treatment efficacy, availability, cost effectiveness, and the potentially more desirable side-effect profiles of other advanced therapies.
The advent of newer advanced therapies, such as anti-integrin, anti-interleukin (IL), and several small-molecule agents, has once again shifted treatment from broader immunosuppression to a narrower targeting of the disease biology [17]. Currently, infliximab and adalimumab are the only biologic medications approved by the US Food and Drug Administration and the European Medicines Agency for the pediatric population in PCD, which significantly limits the use of more recently developed therapies in children and necessitates off-label administration. In this review, we discuss currently available pharmacologic treatment options in relation to various challenges in treating children with CD. We highlight four specific challenges that are some of the most encountered in clinical practice when treating CD with agents other than conventional immunomodulators and anti-TNF drugs. A literature review was conducted through PubMed using relevant search terms including but not limited to drug names in conjunction with CD. No specific inclusion criteria were utilized; however, randomized controlled trials were preferentially used when available.
2 Targeted Biologic and Small-Molecule Therapies
Beyond thiopurine and methotrexate immunomodulation, and anti-TNF therapies, a number of immunologically targeted therapies are newly approved, or in the late stages of the investigational pipeline, for the treatment of CD. The below sections review data from adult and pediatric clinical trials as well as impactful real-world pediatric use of these medications, which is often available before dedicated pediatric clinical trials are completed. The data are summarized in Table 1.
2.1 Anti-Integrin
2.1.1 Vedolizumab
Vedolizumab (VDZ) is a humanized, immunoglobulin G1 monoclonal antibody targeted to an α4β7 integrin that modulates intestinal lymphocyte trafficking and is currently approved for adults with moderate-to-severe CD and ulcerative colitis. The first pediatric prospective trial of VDZ was a phase II dose-ranging study evaluating pharmacokinetics, safety, and efficacy. Enrolled patients (n = 89) with moderate-to-severe CD or ulcerative colitis and weight > 10 kg were randomized by weight to receive either low-dose or high-dose VDZ. The study concluded that VDZ exposure increased in a dose-proportional manner. At week 14, clinical response was observed in 33.3–63.6% of patients with CD across weight groups, with no correlation between clinical response and drug concentration in this limited cohort [18]. A pediatric, multicenter prospective cohort study was completed in 17 centers across six countries with the primary outcome being in corticosteroid-free and exclusive enteral nutrition (EEN)-free clinical remission at 14 weeks. The study reported a 32% (n = 21) remission rate for children with CD [19]. All trials reflect similarly low rates of adverse events given the drug’s gut-specific mechanism and a significant decrease in efficacy in anti-TNF-exposed patients. While anti-TNF agents are considered first line for perianal fistulizing CD, one study has reported 43% of patients (n = 32) taking intravenous (IV) VDZ had a 100% fistula closure by week 30 [20].
2.1.2 Etrolizumab
Etrolizumab is a dual integrin receptor inhibitor of the α4β7 and αEβ7 integrins, thereby controlling the trafficking of immune cells into the intestine. The randomized, placebo-controlled, double-blind, phase III BERGAMOT study investigated the use of the drug in adult patients with moderate-to-severe CD. At the end of the 14-week induction phase, there was no statistical difference in clinical remission (33% vs 29%) or endoscopic improvement (27% vs 22%) between treatment and placebo groups. However, at the end of the 52-week maintenance phase, a significantly higher percentage of patients achieved clinical remission and endoscopic improvement compared with placebo (35% vs 24% and 24% vs 12%, respectively). Similar percentages of patients reported adverse events in treatment and placebo groups during both induction and maintenance phases [21]. No pediatric data are yet available.
2.2 Anti-Cytokine
2.2.1 Ustekinumab
Ustekinumab (UST) is a monoclonal antibody to the p40 subunit of IL-12 and IL-23 currently approved for adults with moderate-to-severe CD and ulcerative colitis. An observational study in pediatrics demonstrated similar efficacy and safety to adults, with approximately 58% of patients (n = 30) in corticosteroid-free clinical remission by week 52. Like the experience with VDZ, higher remission rates were seen in biologic-naive patients compared with those who were biologic exposed (90% vs 50% respectively) [22, 23]. The pharmacokinetics of UST were considered comparable in pediatric patients in a multicenter, double-blind phase I study, although additional studies may be required in patients weighing less than 40 kg. In lower and higher dose groups, endoscopic response was identified in 32% and 28% of patients, respectively, at week 16. Low immunogenicity and a favorable side-effect profile were also demonstrated [24]. Patients enrolled in the long-term extension trial (n = 34) administered subcutaneous UST every 8 weeks were followed up to 4 years and demonstrated results consistent with published adult data [25].
In the only randomized, double-blind, parallel, phase IIIb trial comparing UST and adalimumab in adults, both therapies were considered highly effective as monotherapy with no statistical difference in the primary outcome between the two drugs, prompting greater consideration to an IL-2/23 blockade prior to the use of anti-TNF [26]. In patients not achieving remission with the IV induction dose followed by standard maintenance dosing, dose intensification options have been studied. An open-label, multicenter, randomized, phase IIIb trial investigating a treat-to-target strategy in adults (n = 440) receiving UST was conducted. Endoscopic outcomes were assessed for all patients at week 16 prior to randomization to either the standard-of-care or treat-to-target arm. Patients in the treat-to-target arm were dose optimized to receive the drug as often as every 4 weeks if pre-specified clinical and biomarker targets were not met. At week 48, there was no statistically significant difference in endoscopic response, endoscopic remission, or clinical remission between groups. Clinical response was not better in the treat-to-target group than in the standard-of-care group (68% vs 78%) [27]. A retrospective multicenter study conducted in primarily biologic-exposed children (n = 69, 98.6% biologic exposed) has reported a 67% clinical response rate 3 months after dose escalation. However, this study is limited by a lack of comparator [28]. Additionally, the use of IV reinduction in the setting of a secondary loss of response has been effective in up to 50% of adult patients [29]. Although there are some data to indicate the limited efficacy of UST in healing perianal fistulae with a remission rate of 17%, this is largely dwarfed by the efficacy of anti-TNF medications [30,31,32].
2.2.2 Risankizumab
Risankizumab is a monoclonal antibody that binds to the IL-23 p19 subunit, inhibiting the inflammatory cytokine. Its phase III induction and maintenance trials in adults demonstrated a statistically significant clinical and endoscopic response when compared with placebo. Of the induction trials, ADVANCE included a mixed population of biologic-naïve and biologic-exposed patients, while MOTIVATE was comprised entirely of a biologic-exposed population; endoscopic response at week 12 in the mixed and bio-exposed-only populations was 40% and 29%, respectively. Its phase III maintenance trial, FORTIFY, was the first to assess an endoscopic response in all enrolled patients, delineating the importance of utilizing more stringent patient outcomes to measure pharmacologic success. Rates of endoscopic remission at 1 year were 41% in a mixed population, with a post-hoc subgroup analysis demonstrating endoscopic remission rates of 53% and 36% in biologic-naïve and biologic-exposed populations [33, 34]. A retrospective study completed in adult patients with severe and refractory disease who were exposed to at least three biologics reported approximately 50% corticosteroid-free clinical remission [35]. Risankizumab is not yet studied in children, although a few adolescents (n = 14) aged 16–17 years were enrolled in induction trials. Given its narrow immunologic target with a favorable short-to-moderate term safety profile in adults, combined with optimistic efficacy in anti-TNF-exposed patients make this agent a potentially valuable addition to the treatment toolbox for PCD.
2.2.3 Mirikizumab and Guselkumab
Mirikizumab and guselkumab are anti-IL-23 monoclonal antibodies currently undergoing investigation for patients with active CD. Both medications have demonstrated clinical and endoscopic responses compared with placebo in phase II studies [36, 37]. Mirikizumab is the only anti-IL-23 medication currently recruiting for a pediatric randomized controlled trial, which may serve to further validate the use of this molecular target earlier in treatment positioning and increase the availability of the other in-class agents for children.
2.3 Janus Kinase Inhibitors
2.3.1 Tofacitinib
Tofacitinib is an oral pan Janus kinase (JAK) inhibitor approved for adults with ulcerative colitis. It is no longer under investigation for the treatment of CD. The only existing induction and maintenance randomized controlled trials in adults did not demonstrate statistically significant clinical efficacy of tofacitinib for the treatment of CD [38]. Some retrospective studies demonstrated clinical responses in patients with CD; however, these are limited by a small sample size and the lack of a comparator [39, 40].
2.3.2 Upadacitinib
Upadacitinib (UPA) is an oral selective JAK-1 inhibitor currently approved for adults with moderate-to-severe ulcerative colitis and CD after previous use of anti-TNF therapy. At the time of this writing, data in children with CD are not available other than a case report of rapid improvement with UPA after failure with other therapies [41]. The agent has performed well in a phase II trial including a medically refractory CD population, with 96% of patients having not responded to at least one anti-TNF [42]. It has demonstrated significant and sustained endoscopic remission in comparison with placebo in a 30-month open-label extension in adults with CD [43]. In its two phase III induction trials, U-EXCEL and U-EXCEED, a mixture of biologic-exposed and biologic-naïve adult patients underwent randomization to either UPA 45 mg or placebo for 12 weeks. Clinical responders after induction were then randomized to the maintenance trial to receive UPA 15 mg or 30 mg, or placebo (1:1:1 ratio) once daily for 52 weeks. Patients undergoing induction with UPA had statistically significant higher rates of clinical remission (U-EXCEL, 49.5% vs 29.1%; U-EXCEED, 38.9% vs 21.1%) and endoscopic response (U-EXCEL, 45.5% vs 13.1%; U-EXCEED, 34.6% vs 3.5%) compared with placebo. At the end of the maintenance trial, a higher percentage of patients had clinical remission with UPA 15 mg (37.3%) or 30 mg (47.6%) compared with placebo (15.1%), and a higher percentage had an endoscopic response with UPA 15 mg (27.6%) or 30 mg (40.1%) compared with placebo (7.3%) [44].
In terms of safety, both phase II and phase III trials reported an increased risk of herpes zoster; however, it did not demonstrate a statistically significant increased risk of venous thromboembolism when compared to the placebo group [42,43,44]. In the phase III trials, serious infections, opportunistic infections, anemia, neutropenia, and creatine kinase elevation were seen more frequently in patients who received UPA. Gastrointestinal perforation occurred in four patients receiving UPA 45 mg; one case of perforation was also reported in each of the maintenance groups (UPA 30 mg, 15 mg, and placebo). All patients with gastrointestinal perforation had active CD with deep ulceration or other complications of disease including but not limited to an obstruction or fistula [44]. While the clinical and endoscopic results are encouraging, further studies are needed to shape our understanding of its efficacy and safety in children. For at least the short term, JAK inhibitor positioning remains in patients previously treated with an anti-TNF medication.
2.3.3 Filgotinib
Filgotinib is an oral JAK 1 preferential inhibitor approved for the treatment of ulcerative colitis in Europe, and of rheumatoid arthritis in Europe and Japan. The phase IIb/III SELECTION trial, was considered effective for the induction and maintenance of clinical remission compared with placebo [45]. In a randomized double-blind, placebo-controlled phase II study evaluating filgotinib for adults with ileal, colonic, or ileocolonic CD, filgotinib induced clinical remission in significantly more patients with active CD compared with placebo (47 vs 23%, respectively). Nine percent of patients reported serious treatment-emergent adverse effects compared with 4% of patients treated with placebo [46]. An exploratory phase II, double-blind, placebo-controlled, multicenter trial evaluating small-bowel CD in adults through magnetic resonance enterography showed that treatment with filgotinib did not result in statistically significant differences versus placebo in the proportion of patients who achieved clinical or radiographic remission [47]. There are currently no studies evaluating filgotinib in pediatric patients.
2.4 Sphingosine-1-Phosphate Receptor Modulator
2.4.1 Ozanimod
Ozanimod is an oral sphingosine-1 phosphate receptor modulator that selectively targets sphingosine-1 phosphate receptors, inhibiting the migration of lymphocytes out of lymphoid tissues into circulation. It is currently approved for the treatment of moderate-to-severe adult ulcerative colitis. The phase II trial for patients with CD demonstrated clinical and endoscopic responses in 40% and 25% of patients, respectively. There were no severe adverse effects or dose-limiting toxicities, although clinically significant bradycardia with dose escalation is well described [48]. Phase III induction, maintenance, and open-label extension studies in adults are currently underway [49].
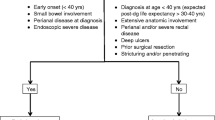
3 Therapy Selection in Pediatrics
Following the integration of anti-TNF therapies as the standard of care in pediatrics, a common decision-making paradigm focused on “bottom-up” versus “top-down” therapy based on the patient’s and clinician’s perceptions of disease severity and medication risk. With the newer drugs described above being increasingly utilized in children, this paradigm has largely been replaced by a treat-to-target model, which ideally emphasizes strategic therapy positioning to select the right medication for the right patient at the right time—concepts coalesced by The Selecting Therapeutic Targets in Inflammatory Bowel Disease Endpoints (STRIDE) Consortium [7]. The aspiration of true precision medicine using genetic, gut microbial, and other biologic signatures to pre-select the optimal therapy remains out of reach in current practice. At the time of CD diagnosis, the author’s current practice is to ask the question: does the patient have a disease feature that warrants an anti-TNF therapy? Complicated disease behavior such as stricturing, internally penetrating or perianal fistulizing disease, moderate-to-severe proximal small bowel/upper tract disease, growth failure, certain extraintestinal manifestations (such as uveitis, arthritis), or hospitalization with more severe symptoms requiring rapid response would lead to an anti-TNF therapy in most circumstances. Below, we discuss some of the common challenges faced by clinicians today regarding initial therapy selection or when anti-TNF medication is unsuccessful in achieving the desired treatment target.
3.1 Challenge 1
3.1.1 Selecting a Non-Anti-Tumor Necrosis Factor First-line Advanced Therapy in the Pediatric Patient with Moderate-to-Severe Inflammatory Disease
The importance of therapy positioning based on patient-specific phenotypes has come to the forefront as treatment options have increased, and quite importantly, a recognition that efficacy rates change with prior anti-TNF medication exposure. With a majority of patients with PCD presenting with moderate-to-severe disease, clinicians must weigh the safety benefits of a medication with a narrower immunologic target as a first-line treatment against the risk of drug failure in the setting of moderate-to-severe, and possibly progressive disease activity. Patients with relatively stable clinical disease may benefit from therapeutic agents with more narrow immunologic targets such as VDZ, UST, and risankizumab. An important consideration for VDZ and UST in the initial position is the potential for decreased efficacy following anti-TNF exposure.
If choosing a non-anti-TNF advanced therapy, an important phenotypic consideration is the geography of a patient’s disease. In both children and adults, VDZ has been found to be more effective in isolated/predominant colonic disease compared with ileal disease [50, 51]. When disease location is ileal or ileocolonic, a drug with IL-23 antagonism (UST or risankizumab) is our preferred choice over VDZ. In a report on the real-world experience of using UST in children with IBD, which included 42 patients with CD, 60% achieved corticosteroid-free clinical remission after 1 year. No significant difference was seen in those with isolated colonic disease (31%) compared with those with ileal involvement [22]. In the near future, it would be useful to have a validated, pediatric-derived, clinical decision support tool to help predetermine the likelihood of a response to these medications in PCD, as has been shown possible in adults for both VDZ and UST [52, 53]. Projecting further to the future, we anticipate the use of gut microbial analyses to predict medication response; this has been promising in early investigational studies in adults with CD starting VDZ or UST [54, 55].
While salvage therapy for hospitalized patients has historically been limited to IV corticosteroids and infliximab, oral JAK inhibitors may be an additional consideration given their rapid onset of action in the setting of corticosteroid-refractory and anti-TNF-refractory disease. There are not any robust data currently to report on the efficacy of UPA as a first-line therapy in PCD or adult-onset CD. From a regulatory perspective, patients with rapidly progressive disease or hospitalized will likely require treatment with anti-TNF, as JAK inhibitors are currently reserved for anti-TNF-refractory patients.
3.2 Challenge 2
3.2.1 Pediatric Patient with Partial Response to Anti-Tumor Necrosis Factor
A common clinical dilemma is deciding how to best guide patients who achieve clinical remission taking an anti-TNF medication, yet do not achieve endoscopic and/or histologic healing despite optimized drug dosing [56]. Discontinuation of the anti-TNF medication in favor of another medication class may prove ineffective, leading to clinical deterioration and possible immunogenicity to the initial anti-TNF drug, risking the inability to return after discontinuation. Prior to drug discontinuation, it is imperative that both dosing and the interval are appropriately optimized, lending importance to the ongoing study of therapeutic drug monitoring. Following drug optimization, addition of a second therapeutic agent must be considered. The use of an immunomodulator, either thiopurine or methotrexate, is well studied in this setting with variable results. Concerning safety signals with anti-TNF and thiopurine in combination has led pediatric clinicians to often look elsewhere for treatment options including the use of methotrexate [57]. In a recently published, large, pediatric prospective clinical trial evaluating the use of concomitant methotrexate with anti-TNF therapy, combination with adalimumab but not infliximab was shown to increase treatment efficacy [58]. Emerging data combining two advanced therapies are now available and an important area of future research. The discussion below focuses on both drug optimization and combination therapy of two advanced therapy molecules (biologic and small molecule).
3.2.2 Pharmacokinetics and Therapeutic Drug Monitoring
Proactive therapeutic drug monitoring is the systematic measurement of drug trough concentrations with a subsequent dose adaptation to meet goal therapeutic drug concentrations. Reactive therapeutic drug monitoring is completed in the setting of treatment failure or symptom recurrence. Prior to defining treatment failure, adequate drug exposure should be established. Exposure–outcome relationship data from prospective studies and post hoc data from randomized controlled trials have consistently shown that higher induction and maintenance anti-TNF drug concentrations are associated with improved outcomes [32, 59, 60]. Optimized anti-TNF drug concentrations are of special consideration in pediatric patients who often require increased dosing because of a high disease burden, leading to rapid drug clearance and the potential for inadequate drug exposure, immunogenicity, and drug failure [56, 61, 62]. Given this, our experience suggests exceeding a maintenance dose of 10 mg/kg of infliximab is a common off-label clinical practice amongst pediatric clinicians and further research is needed to investigate these dosing considerations in children. While there are few data on therapeutic drug monitoring for VDZ and UST, specific trough concentration targets have been shown to correlate with endoscopic remission [63,64,65].
3.2.3 Combination of Two Advanced Therapies
As already reviewed, some currently available therapies have a decreased effectiveness after anti-TNF exposure. In some children, switching from anti-TNF to another drug class is unsuccessful as monotherapy. When utilizing combination therapy, the risk-benefit ratio considering the need for better clinical efficacy and deeper disease remission is balanced with the potential for further adverse effects related to broader immunosuppression and medical costs. Because of this, the addition of an advanced therapy with a narrow immunologic target is desired. Additional consideration to the combination of therapies should be given for patients with extraintestinal manifestations not resolved with the IBD therapeutic agent such as psoriasis, arthritis, or alopecia. Ahmed et al. conducted a systematic review and meta-analysis of patients with IBD (n = 279, 76% CD) on dual therapy and reported a pooled 31% rate of adverse events, with clinical and endoscopic remission of 59% and 34%, respectively [66]. The majority (81%) were initiated on combination therapy for medically refractory disease and the most common combination was anti-TNF and anti-integrin (48%), although other combinations included anti-TNF and UST, VDZ and UST, and VDZ and tofacitinib [66]. Other smaller studies have also reported clinical and endoscopic success with combination treatment as well as the potential adverse effects of infection and malignancy [67, 68].
To our knowledge, the only available literature specific to the use of combination advanced therapy in pediatrics consists of case reports, case series, and small retrospective reviews. These studies do report that the use of combination therapy is relatively safe and effective in the use of refractory pediatric inflammatory bowel disease. Dolinger et al. reported a 75% (n = 12) corticosteroid-free clinical remission and a statistically significant improvement in biomarkers at 6 months in children who did not respond to two or more biologic monotherapies. One patient taking VDZ/tofacitinib with concomitant prednisone use developed septic arthritis and deep vein thrombosis, but later achieved mucosal healing following a prednisone wean [69]. Another study reported a rate of 73% (n = 10) clinical improvement and a statistically significant decrease in calprotectin after 4 months of combination treatment [70]. In a retrospective report on UST plus VDZ combination therapy, three pediatric patients with severe CD had a significant clinical benefit after not responding to one or the other as monotherapy [71].
3.3 Challenge 3
3.3.1 Pediatric Patient with Medically Refractory Disease
Despite a growing number of available pharmacological options to treat CD, unfortunately some patients develop complicated disease behaviors that do not respond to conventional therapies. No anti-fibrotic therapy is readily available to manage strictures medically, and some patients develop recalcitrant perianal fistulizing disease. Surgical resection often remains a needed strategy for refractory disease. Outcomes after ileocolic resection and pharmacologic prevention of post-operative recurrence are outside the scope of this discussion. Below, we highlight mesenchymal stem cell therapy and hyperbaric oxygen therapy as part of a growing list of tools being investigated for these and other challenging situations.
3.3.2 Mesenchymal Stem Cell Therapy
Mesenchymal stem cell treatment (MSCT) has been shown in preclinical studies to have an immunomodulatory and anti-inflammatory effect. Treatment efficacy of MSCT in several inflammatory conditions, including CD, has been shown. The utility of mesenchymal stem cell injections in patients with CD is focused specifically on stricturing and fistulizing disease with some efficacy demonstrated in clinical trials. In a recently published first pediatric report using MSCT for perianal fistulae, seven patients aged 13–17 years were treated, and 83% had complete clinical and radiographic healing without any serious adverse events [72]. The ADMIRE study, a phase III randomized controlled trial evaluating the long-term efficacy and safety of MSCT in adults with perianal fistulizing CD, found significant efficacy compared with placebo without concerning safety signals [73, 74]. In a phase I–II study investigating the injection of mesenchymal stem cells into short fibrotic strictures reachable by ileocolonoscopy, 50% (n = 5) of adult patients had a complete or partial resolution of the stricture at week 12. Of the seven patients who were re-evaluated at week 48, four patients had maintained complete endoscopic resolution, indicating the possible utility of MSCT for fibrotic strictures secondary to CD. Overall, the procedure was well tolerated in all patients [75].
3.3.3 Hyperbaric Oxygen
The use of hyperbaric oxygen has been investigated for patients with CD with complicated disease behavior. A systematic review reported an 85% response rate for CD (n = 243), although primary endpoints were highly variable between individual studies [76]. Significant clinical and endoscopic improvements are reported in patients with chronic antibiotic refractory pouchitis [77]. An initial pilot study completed in patients with small-bowel stricturing disease (n = 14) was completed with a radiographic improvement seen in 50% of patients at the 6-month follow-up [78]. Efficacy in the treatment of hyperbaric oxygen for patients with perianal fistulas has also been demonstrated with clinical remission at 16 weeks and a 1-year follow-up in 60% (n = 12) and 20% (n = 4) of patients, respectively [79, 80]. This method was shown to be ineffective in the treatment of recto-vaginal fistulas [81]. Adverse events reported included ear barotrauma (25%) and myopic vision changes (10%) [77, 79]. In a case report of two pediatric patients with inflammatory CD, both experienced disease improvement after cycles of hyperbaric oxygen [82].
3.4 Challenge 4
3.4.1 Pediatric Patient with Mild Disease
While the focus of this paper has centered on pharmacologic advances, there is a subset of patients with PCD with uncomplicated, minimal-to-mild inflammatory luminal disease and who are limited in the extent for whom biologic and small-molecule therapies are not indicated. These advanced therapies may seem like excessive treatment and carry too high a risk from clinician or patient perspectives. However, there are scant data available from placebo-controlled trials on treating this population, as clinical trial programs typically concentrate on the moderate to severely active patient population. Historically, aminosalicylates, corticosteroids, antibiotics, and nutritional therapies have been tried. Corticosteroids and antibiotics carry negative consequences and the long-term use and efficacy of aminosalicylates are questionable at best, leaving little pharmaceutical options to confidently use as first-line therapy in the patient with truly mild CD. Given some children with mild luminal CD can go years without disease progression [83], use of a non-immunomodulating therapy with potential anti-inflammatory effects would be ideal.
3.4.2 Nutritional Therapy
Nutritional therapy can be effective for both induction and maintenance of remission, although patient adherence may limit responses. Exclusive enteral nutrition has demonstrated efficacy for the induction of clinical and biochemical remission in luminal PCD [84,85,86]. In a single-center comparative effectiveness analysis, EEN performed similarly to anti-TNF medication in inducing remission, with both being superior to a partial enteral nutrition regimen [87]. Maintenance EEN has also demonstrated significant mucosal healing rates (79%), although a much smaller proportion of patients (17%) achieved transmural healing [88]. Overall, published studies provide ample evidence to support EEN as a possible low-risk alternative to corticosteroids for the induction of remission.
Various diets that include whole foods have been investigated, with the optimal diet composition still under investigation. The CD exclusion diet is a whole-food diet designed to reduce dietary exposure of items that are considered proinflammatory. The CD exclusion diet was found to be better tolerated in children with mild-to-moderate CD and was associated with a higher rate of corticosteroid-free remission compared with EEN [89].
The specific carbohydrate diet is a whole-food diet that focuses on the exclusion of processed foods, sugars (except honey), grains, and most milk products. The specific carbohydrate diet has demonstrated significant clinical, biochemical, and endoscopic improvements in patients with PCD [90, 91]. The Mediterranean diet has gained recent interest for being less restrictive and potentially beneficial. It is a whole-food diet that emphasizes fresh fruits, vegetables, nuts, fish, whole grains, and olive oil as the main source of fat, and is associated with a lower risk of developing CD. A head-to-head trial including adult patients with CD with mild-to-moderate disease activity compared the efficacy of the Mediterranean diet and the specific carbohydrate diet as treatment. Similar rates of clinical remission were seen for both the specific carbohydrate diet and the Mediterranean diet with rare improvements in biochemical improvement for both treatments [92].
3.4.3 Vagus Nerve Stimulation
Vagus nerve stimulation has gained recent interest as an anti-inflammatory therapy. The inflammatory reflex, a neural reflex that carries information about peripheral inflammation to the central nervous system and a counter-regulatory response back to the periphery via the efferent vagus nerve, can be activated with use of a surgically implanted or transcutaneous electrical device [93]. A pilot study in biologic-naïve adults with mild-to-moderate CD found clinical, biochemical, and endoscopic improvements using a surgically implanted vagus nerve stimulation device [94]. A pediatric trial using transcutaneous auricular vagus nerve stimulation was recently completed, reporting clinical and calprotectin responses over a 16-week period of time [95]. Further investigation is needed to understand the optimal use of this and other bioelectronic therapies.
4 Conclusions
Pediatric CD is characterized by a significant disease burden and an increased rate of disease complication necessitating utilization of advanced therapies. Despite this, pediatric drug trials are typically conducted several years following regulatory agencies approval for adults, prompting extensive off-label use by pediatric clinicians. This real-world practice further deters enrollment of children in trials for drugs that are already considered standard of care. Additionally, the inappropriate application of adult pharmacokinetic data to pediatric dosing recommendations can lead to inadequate exposure and is of specific concern for smaller patients weighing < 30 kg. Consensus statements regarding a recommended clinical trial design in children with CD have been previously published and illustrate the importance of reasonable enrollment goals representative of pediatric prevalence, minimal deviation from routine care, and the obtainment of much needed pharmacokinetic data [96]. The pharmacologic landscape of PCD has changed rapidly over the last decade with multiple emerging treatment options. The future of treatment in PCD will likely focus on targeted immunologic therapies based on a patient-specific phenotype that increase efficacy and minimize adverse effects related to immunosuppression.
References
Pigneur B, Seksik P, Viola S, et al. Natural history of Crohn’s disease: comparison between childhood- and adult-onset disease. Inflamm Bowel Dis. 2010;16(6):953–61. https://doi.org/10.1002/ibd.21152.
Duricova D, Burisch J, Jess T, Gower-Rousseau C, Lakatos PL, ECCO-EpiCom. Age-related differences in presentation and course of inflammatory bowel disease: an update on the population-based literature. J Crohns Colitis. 2014;8(11):1351–61. https://doi.org/10.1016/j.crohns.2014.05.006.
Kurowski JA, Milinovich A, Ji X, et al. Differences in biologic utilization and surgery rates in pediatric and adult Crohn’s disease: results from a large electronic medical record-derived cohort. Inflamm Bowel Dis. 2021;27(7):1035–44. https://doi.org/10.1093/ibd/izaa239.
Ahmed S, Alam S, Alsabri M. Health-related quality of life in pediatric inflammatory bowel disease patients: a narrative review. Cureus. 2022;14(9): e29282. https://doi.org/10.7759/cureus.29282.
Sahn B, Markowitz J. The natural history of Crohn disease in children. In: Mamula P, Grossman A, Baldassano R, Kelsen J, Markowitz J, editors. Pediatric inflammatory bowel disease. Cham: Springer; 2017.
Colombel JF, Panaccione R, Bossuyt P, et al. Effect of tight control management on Crohn’s disease (CALM): a multicentre, randomised, controlled phase 3 trial. Lancet. 2017;390(10114):2779–89. https://doi.org/10.1016/S0140-6736(17)32641-7.
Turner D, Ricciuto A, Lewis A, et al. STRIDE-II: an update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) initiative of the International Organization for the Study of IBD (IOIBD): determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology. 2021;160(5):1570–83. https://doi.org/10.1053/j.gastro.2020.12.031.
Payen E, Neuraz A, Zenzeri L, et al. Adalimumab therapy in pediatric Crohn disease: a 2-year follow-up comparing “top-down” and “step-up” strategies. J Pediatr Gastroenterol Nutr. 2023;76(2):166–73. https://doi.org/10.1097/MPG.0000000000003643.
Hyams J, Walters TD, Crandall W, et al. Safety and efficacy of maintenance infliximab therapy for moderate-to-severe Crohn’s disease in children: REACH open-label extension. Curr Med Res Opin. 2011;27(3):651–62. https://doi.org/10.1185/03007995.2010.547575.
Jongsma MME, Aardoom MA, Cozijnsen MA, et al. First-line treatment with infliximab versus conventional treatment in children with newly diagnosed moderate-to-severe Crohn’s disease: an open-label multicentre randomised controlled trial. Gut. 2022;71(1):34–42. https://doi.org/10.1136/gutjnl-2020-322339.
Colman RJ, Lawton RC, Dubinsky MC, Rubin DT. Methotrexate for the treatment of pediatric Crohn’s disease: a systematic review and meta-analysis. Inflamm Bowel Dis. 2018;24(10):2135–41. https://doi.org/10.1093/ibd/izy078.
Rosh JR. The current role of methotrexate in patients with inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2020;16(1):43–6.
Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362(15):1383–95. https://doi.org/10.1056/NEJMoa0904492.
Chande N, Townsend CM, Parker CE, MacDonald JK. Azathioprine or 6-mercaptopurine for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2016;10(10): CD000545. https://doi.org/10.1002/14651858.CD000545.pub5.
Shale M, Kanfer E, Panaccione R, Ghosh S. Hepatosplenic T cell lymphoma in inflammatory bowel disease. Gut. 2008;57(12):1639–41. https://doi.org/10.1136/gut.2008.163279.
Hyams JS, Dubinsky MC, Baldassano RN, et al. Infliximab is not associated with increased risk of malignancy or hemophagocytic lymphohistiocytosis in pediatric patients with inflammatory bowel disease. Gastroenterology. 2017;152(8): 1901–14.e3. https://doi.org/10.1053/j.gastro.2017.02.004.
Spencer EA, Dubinsky MC. Precision medicine in pediatric inflammatory bowel disease. Pediatr Clin North Am. 2021;68(6):1171–90. https://doi.org/10.1016/j.pcl.2021.07.011.
Hyams JS, Turner D, Cohen SA, et al. Pharmacokinetics, safety and efficacy of intravenous vedolizumab in paediatric patients with ulcerative colitis or Crohn’s disease: results from the phase 2 HUBBLE Study. J Crohns Colitis. 2022;16(8):1243–54. https://doi.org/10.1093/ecco-jcc/jjac036.
Atia O, Shavit-Brunschwig Z, Mould DR, et al. Outcomes, dosing, and predictors of vedolizumab treatment in children with inflammatory bowel disease (VEDOKIDS): a prospective, multicentre cohort study. Lancet Gastroenterol Hepatol. 2023;8(1):31–42. https://doi.org/10.1016/S2468-1253(22)00307-7.
Schwartz DA, Peyrin-Biroulet L, Lasch K, Adsul S, Danese S. Efficacy and safety of 2 vedolizumab intravenous regimens for perianal fistulizing Crohn’s disease: ENTERPRISE Study. Clin Gastroenterol Hepatol. 2022;20(5): 1059–67.e9. https://doi.org/10.1016/j.cgh.2021.09.028.
Sandborn WJ, Panes J, Danese S, et al. Etrolizumab as induction and maintenance therapy in patients with moderately to severely active Crohn’s disease (BERGAMOT): a randomised, placebo-controlled, double-blind, phase 3 trial. Lancet Gastroenterol Hepatol. 2023;8(1):43–55. https://doi.org/10.1016/S2468-1253(22)00303-X.
Dayan JR, Dolinger M, Benkov K, et al. Real world experience with ustekinumab in children and young adults at a tertiary care pediatric inflammatory bowel disease center. J Pediatr Gastroenterol Nutr. 2019;69(1):61–7. https://doi.org/10.1097/MPG.0000000000002362.
Sandborn WJ, Rebuck R, Wang Y, et al. Five-year efficacy and safety of ustekinumab treatment in Crohn’s disease: the IM-UNITI Trial. Clin Gastroenterol Hepatol. 2022;20(3): 578–90.e4. https://doi.org/10.1016/j.cgh.2021.02.025.
Rosh JR, Turner D, Griffiths A, et al. Ustekinumab in paediatric patients with moderately to severely active Crohn’s disease: pharmacokinetics, safety, and efficacy results from UniStar, a phase 1 study. J Crohns Colitis. 2021;15(11):1931–42. https://doi.org/10.1093/ecco-jcc/jjab089.
Rosh JR, Lerer T, Markowitz J, et al. Retrospective Evaluation of the Safety and Effect of Adalimumab Therapy (RESEAT) in pediatric Crohn’s disease. Am J Gastroenterol. 2009;104(12):3042–9. https://doi.org/10.1038/ajg.2009.493.
Sands BE, Irving PM, Hoops T, et al. Ustekinumab versus adalimumab for induction and maintenance therapy in biologic-naive patients with moderately to severely active Crohn’s disease: a multicentre, randomised, double-blind, parallel-group, phase 3b trial. Lancet. 2022;399(10342):2200–11. https://doi.org/10.1016/S0140-6736(22)00688-2.
Danese S, Vermeire S, D’Haens G, et al. Treat to target versus standard of care for patients with Crohn’s disease treated with ustekinumab (STARDUST): an open-label, multicentre, randomised phase 3b trial. Lancet Gastroenterol Hepatol. 2022;7(4):294–306. https://doi.org/10.1016/S2468-1253(21)00474-X.
Yerushalmy-Feler A, Pujol-Muncunill G, Martin-de-Carpi J, et al. Safety and potential efficacy of escalating dose of ustekinumab in pediatric Crohn disease (the Speed-up Study): a multicenter study from the Pediatric IBD Porto Group of ESPGHAN. J Pediatr Gastroenterol Nutr. 2022;75(6):717–23. https://doi.org/10.1097/MPG.0000000000003608.
Bermejo F, Jimenez L, Algaba A, et al. Re-induction with intravenous ustekinumab in patients with Crohn’s disease and a loss of response to this therapy. Inflamm Bowel Dis. 2022;28(1):41–7. https://doi.org/10.1093/ibd/izab015.
Attauabi M, Burisch J, Seidelin JB. Efficacy of ustekinumab for active perianal fistulizing Crohn’s disease: a systematic review and meta-analysis of the current literature. Scand J Gastroenterol. 2021;56(1):53–8. https://doi.org/10.1080/00365521.2020.1854848.
Ruemmele FM, Rosh J, Faubion WA, et al. Efficacy of adalimumab for treatment of perianal fistula in children with moderately to severely active Crohn’s disease: results from IMAgINE 1 and IMAgINE 2. J Crohns Colitis. 2018;12(10):1249–54. https://doi.org/10.1093/ecco-jcc/jjy087.
Papamichael K, VandeCasteele N, Jeyarajah J, Jairath V, Osterman MT, Cheifetz AS. Higher postinduction infliximab concentrations are associated with improved clinical outcomes in fistulizing Crohn’s disease: an ACCENT-II post hoc analysis. Am J Gastroenterol. 2021;116(5):1007–14. https://doi.org/10.14309/ajg.0000000000001111.
D’Haens G, Panaccione R, Baert F, et al. Risankizumab as induction therapy for Crohn’s disease: results from the phase 3 ADVANCE and MOTIVATE induction trials. Lancet. 2022;399(10340):2015–30. https://doi.org/10.1016/S0140-6736(22)00467-6.
Ferrante M, Panaccione R, Baert F, et al. Risankizumab as maintenance therapy for moderately to severely active Crohn’s disease: results from the multicentre, randomised, double-blind, placebo-controlled, withdrawal phase 3 FORTIFY maintenance trial. Lancet. 2022;399(10340):2031–46. https://doi.org/10.1016/S0140-6736(22)00466-4.
Fumery M, Defrance A, Roblin X, et al. Effectiveness and safety of risankizumab induction therapy for 100 patients with Crohn’s disease: a GETAID multicentre cohort study. Aliment Pharmacol Ther. 2023;57(4):426–34. https://doi.org/10.1111/apt.17358.
Sands BE, Peyrin-Biroulet L, Kierkus J, et al. Efficacy and safety of mirikizumab in a randomized phase 2 study of patients with Crohn’s disease. Gastroenterology. 2022;162(2):495–508. https://doi.org/10.1053/j.gastro.2021.10.050.
Sandborn WJ, D’Haens GR, Reinisch W, et al. Guselkumab for the treatment of Crohn’s disease: induction results from the phase 2 GALAXI-1 Study. Gastroenterology. 2022;162(6): 1650–64.e8. https://doi.org/10.1053/j.gastro.2022.01.047.
Panes J, Sandborn WJ, Schreiber S, et al. Tofacitinib for induction and maintenance therapy of Crohn’s disease: results of two phase IIb randomised placebo-controlled trials. Gut. 2017;66(6):1049–59. https://doi.org/10.1136/gutjnl-2016-312735.
Lee SD, Singla A, Harper J, et al. Tofacitinib appears well tolerated and effective for the treatment of patients with refractory Crohn’s disease. Dig Dis Sci. 2022;67(8):4043–8. https://doi.org/10.1007/s10620-022-07444-5.
Fenster M, Alayo QA, Khatiwada A, et al. Real-world effectiveness and safety of tofacitinib in Crohn’s disease and IBD-U: a multicenter study from the TROPIC Consortium. Clin Gastroenterol Hepatol. 2021;19(10): 2207–9.e3. https://doi.org/10.1016/j.cgh.2020.10.025.
Collen LV. Rapid clinical remission with upadacitinib in a pediatric patient with refractory Crohn’s disease. Inflamm Bowel Dis. 2023;29(7):1175–6. https://doi.org/10.1093/ibd/izad048.
Sandborn WJ, Feagan BG, Loftus EV Jr, et al. Efficacy and safety of upadacitinib in a randomized trial of patients with Crohn’s disease. Gastroenterology. 2020;158(8): 2123–38.e8. https://doi.org/10.1053/j.gastro.2020.01.047.
D’Haens G, Panes J, Louis E, et al. Upadacitinib was efficacious and well-tolerated over 30 months in patients with Crohn’s disease in the CELEST Extension Study. Clin Gastroenterol Hepatol. 2022;20(10): 2337–46.e3. https://doi.org/10.1016/j.cgh.2021.12.030.
Loftus EV Jr, Panes J, Lacerda AP, et al. Upadacitinib induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2023;388(21):1966–80. https://doi.org/10.1056/NEJMoa2212728.
Feagan BG, Danese S, Loftus EV Jr, et al. Filgotinib as induction and maintenance therapy for ulcerative colitis (SELECTION): a phase 2b/3 double-blind, randomised, placebo-controlled trial. Lancet. 2021;397(10292):2372–84. https://doi.org/10.1016/S0140-6736(21)00666-8.
Vermeire S, Schreiber S, Petryka R, et al. Clinical remission in patients with moderate-to-severe Crohn’s disease treated with filgotinib (the FITZROY study): results from a phase 2, double-blind, randomised, placebo-controlled trial. Lancet. 2017;389(10066):266–75. https://doi.org/10.1016/S0140-6736(16)32537-5.
D’Haens GR, Lee S, Taylor SA, et al. Filgotinib for the treatment of small bowel Crohn’s disease: the DIVERGENCE 1 Trial. Gastroenterology. 2023;165(1): 289–92.e3. https://doi.org/10.1053/j.gastro.2023.03.234.
Feagan BG, Sandborn WJ, Danese S, et al. Ozanimod induction therapy for patients with moderate to severe Crohn’s disease: a single-arm, phase 2, prospective observer-blinded endpoint study. Lancet Gastroenterol Hepatol. 2020;5(9):819–28. https://doi.org/10.1016/S2468-1253(20)30188-6.
Feagan BG, Schreiber S, Afzali A, et al. Ozanimod as a novel oral small molecule therapy for the treatment of Crohn’s disease: the YELLOWSTONE clinical trial program. Contemp Clin Trials. 2022;122: 106958. https://doi.org/10.1016/j.cct.2022.106958.
Singh N, Rabizadeh S, Jossen J, et al. Multi-center experience of vedolizumab effectiveness in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(9):2121–6. https://doi.org/10.1097/MIB.0000000000000865.
Vermeire S, D’Haens G, Baert F, et al. Efficacy and safety of subcutaneous vedolizumab in patients with moderately to severely active Crohn’s disease: results from the VISIBLE 2 randomised trial. J Crohns Colitis. 2022;16(1):27–38. https://doi.org/10.1093/ecco-jcc/jjab133.
Dulai PS, Amiot A, Peyrin-Biroulet L, et al. A clinical decision support tool may help to optimise vedolizumab therapy in Crohn’s disease. Aliment Pharmacol Ther. 2020;51(5):553–64. https://doi.org/10.1111/apt.15609.
Park J, Chun J, Yoon H, Cheon JH. Feasibility of a clinical dDecision support tool for ustekinumab to predict clinical remission and relapse in patients with Crohn’s disease: a multicenter observational study. Inflamm Bowel Dis. 2023;29(4):548–54. https://doi.org/10.1093/ibd/izac105.
Ananthakrishnan AN, Luo C, Yajnik V, et al. Gut microbiome function predicts response to anti-integrin biologic therapy in inflammatory bowel diseases. Cell Host Microbe. 2017;21(5): 603–10.e3. https://doi.org/10.1016/j.chom.2017.04.010.
Doherty MK, Ding T, Koumpouras C, et al. Fecal microbiota signatures are associated with response to ustekinumab therapy among Crohn’s disease patients. MBio. 2018;9(2): e02120–17. https://doi.org/10.1128/mBio.02120-17.
Winter DA, Joosse ME, de Wildt SN, Taminiau J, de Ridder L, Escher JC. Pharmacokinetics, pharmacodynamics, and immunogenicity of infliximab in pediatric inflammatory bowel disease: a systematic review and revised dosing considerations. J Pediatr Gastroenterol Nutr. 2020;70(6):763–76. https://doi.org/10.1097/MPG.0000000000002631.
Grossi V, Lerer T, Griffiths A, et al. Concomitant use of immunomodulators affects the durability of infliximab therapy in children with Crohn’s disease. Clin Gastroenterol Hepatol. 2015;13(10):1748–56. https://doi.org/10.1016/j.cgh.2015.04.010.
Kappelman MD, Wohl DA, Herfarth HH, et al. Comparative effectiveness of anti-TNF in combination with low-dose methotrexate vs anti-TNF monotherapy in pediatric Crohn’s disease: a peagmatic randomized yrial. Gastroenterology. 2023;165(1): 149–61.e7. https://doi.org/10.1053/j.gastro.2023.03.224.
Plevris N, Lyons M, Jenkinson PW, et al. Higher adalimumab drug levels during maintenance therapy for Crohn’s disease are associated with biologic remission. Inflamm Bowel Dis. 2019;25(6):1036–43. https://doi.org/10.1093/ibd/izy320.
Wilson A, Choi B, Sey M, Ponich T, Beaton M, Kim RB. High infliximab trough concentrations are associated with sustained histologic remission in inflammatory bowel disease: a prospective cohort study. BMC Gastroenterol. 2021;21(1):77. https://doi.org/10.1186/s12876-021-01650-7.
Assa A, Dorfman L, Shouval DS, Shamir R, Cohen S. Therapeutic drug monitoring-guided high-dose infliximab for infantile-onset inflammatory bowel disease: a case series. J Pediatr Gastroenterol Nutr. 2020;71(4):516–20. https://doi.org/10.1097/MPG.0000000000002832.
Jongsma MME, Winter DA, Huynh HQ, et al. Infliximab in young paediatric IBD patients: it is all about the dosing. Eur J Pediatr. 2020;179(12):1935–44. https://doi.org/10.1007/s00431-020-03750-0.
Dreesen E, Verstockt B, Bian S, et al. Evidence to support monitoring of vedolizumab trough concentrations in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2018;16(12): 1937–46.e8. https://doi.org/10.1016/j.cgh.2018.04.040.
Hanzel J, Zdovc J, Kurent T, et al. Peak concentrations of ustekinumab after intravenous induction therapy identify patients with Crohn’s disease likely to achieve endoscopic and biochemical remission. Clin Gastroenterol Hepatol. 2021;19(1): 111–8.e10. https://doi.org/10.1016/j.cgh.2020.02.033.
Verstockt B, Dreesen E, Noman M, et al. Ustekinumab exposure-outcome analysis in Crohn’s disease only in part explains limited endoscopic remission rates. J Crohns Colitis. 2019;13(7):864–72. https://doi.org/10.1093/ecco-jcc/jjz008.
Ahmed W, Galati J, Kumar A, et al. Dual biologic or small molecule therapy for treatment of inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2022;20(3): e361–79. https://doi.org/10.1016/j.cgh.2021.03.034.
Yang E, Panaccione N, Whitmire N, et al. Efficacy and safety of simultaneous treatment with two biologic medications in refractory Crohn’s disease. Aliment Pharmacol Ther. 2020;51(11):1031–8. https://doi.org/10.1111/apt.15719.
Kwapisz L, Raffals LE, Bruining DH, et al. Combination biologic therapy in inflammatory bowel disease: experience from a tertiary care center. Clin Gastroenterol Hepatol. 2021;19(3):616–7. https://doi.org/10.1016/j.cgh.2020.02.017.
Dolinger MT, Spencer EA, Lai J, Dunkin D, Dubinsky MC. Dual biologic and small molecule therapy for the treatment of refractory pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2021;27(8):1210–4. https://doi.org/10.1093/ibd/izaa277.
Wlazlo M, Meglicka M, Wiernicka A, Osiecki M, Kierkus J. Dual biologic therapy in moderate to severe pediatric inflammatory Bbwel disease: a retrospective study. Children (Basel). 2022;10(1):11. https://doi.org/10.3390/children10010011.
Howard G, Weiner D, Bar-Or I, Levine A. Dual biologic therapy with vedolizumab and ustekinumab for refractory Crohn’s disease in children. Eur J Gastroenterol Hepatol. 2022;34(4):372–4. https://doi.org/10.1097/MEG.0000000000002203.
Lightner AL, Otero-Pineiro A, Reese J, et al. A phase I study of ex vivo expanded allogeneic bone marrow-derived mesenchymal stem cells for the treatment of pediatric perianal fistulizing Crohn’s disease. Inflamm Bowel Dis. 2023. https://doi.org/10.1093/ibd/izad100.
Garcia-Olmo D, Gilaberte I, Binek M, et al. Follow-up study to evaluate the long-term safety and efficacy of darvadstrocel (mesenchymal stem cell treatment) in patients with perianal fistulizing Crohn’s disease: ADMIRE-CD phase 3 randomized controlled trial. Dis Colon Rectum. 2022;65(5):713–20. https://doi.org/10.1097/DCR.0000000000002325.
Carvello M, Lightner A, Yamamoto T, Kotze PG, Spinelli A. Mesenchymal stem cells for perianal Crohn’s disease. Cells. 2019;8(7):764. https://doi.org/10.3390/cells8070764.
Vieujean S, Loly JP, Boutaffala L, et al. Mesenchymal stem cell injection in Crohn’s disease strictures: a phase I–II clinical study. J Crohns Colitis. 2022;16(3):506–10. https://doi.org/10.1093/ecco-jcc/jjab154.
Dulai PS, Gleeson MW, Taylor D, Holubar SD, Buckey JC, Siegel CA. Systematic review: the safety and efficacy of hyperbaric oxygen therapy for inflammatory bowel disease. Aliment Pharmacol Ther. 2014;39(11):1266–75. https://doi.org/10.1111/apt.12753.
Hasan B, Yim Y, Ur Rashid M, et al. Hyperbaric oxygen therapy in chronic inflammatory conditions of the pouch. Inflamm Bowel Dis. 2021;27(7):965–70. https://doi.org/10.1093/ibd/izaa245.
Kante B, Sahu P, Kedia S, et al. Efficacy and tolerability of hyperbaric oxygen therapy in small bowel stricturing Crohn’s disease: a pilot study. Intest Res. 2022;20(2):231–9. https://doi.org/10.5217/ir.2021.00056.
Lansdorp CA, Gecse KB, Buskens CJ, et al. Hyperbaric oxygen therapy for the treatment of perianal fistulas in 20 patients with Crohn’s disease. Aliment Pharmacol Ther. 2021;53(5):587–97. https://doi.org/10.1111/apt.16228.
Lansdorp CA, Buskens CJ, Gecse KB, et al. Hyperbaric oxygen therapy for the treatment of perianal fistulas in 20 patients with Crohn’s disease: results of the HOT-TOPIC trial after 1-year follow-up. United Eur Gastroenterol J. 2022;10(2):160–8. https://doi.org/10.1002/ueg2.12189.
Lansdorp CA, Buskens CJ, Gecse KB, D’Haens G, van Hulst RA. Hyperbaric oxygen therapy for the treatment of rectovaginal fistulas in patients with Crohn’s disease: results of the HOT-REVA pilot study. BJS Open. 2021;5(3): zrab042. https://doi.org/10.1093/bjsopen/zrab042.
Green MS, Purohi M, Sadacharam K, Mychaskiw G. Efficacy of hyperbaric oxygen in patients with Crohn’s disease: two case reports. Undersea Hyperb Med. 2013;40(2):201–4.
Sharma Y, Bousvaros A, Liu E, Bender SJ. Natural history of children with mild Crohn’s disease. World J Gastroenterol. 2019;25(30):4235–45. https://doi.org/10.3748/wjg.v25.i30.4235.
SigallBoneh R, Van Limbergen J, Wine E, et al. Dietary therapies induce rapid response and remission in pediatric patients with active Crohn’s disease. Clin Gastroenterol Hepatol. 2021;19(4):752–9. https://doi.org/10.1016/j.cgh.2020.04.006.
Sohouli MH, Fatahi S, Farahmand F, Alimadadi H, Seraj SS, Rohani P. Meta-analysis: efficacy of exclusive enteral nutrition as induction therapy on disease activity index, inflammation and growth factors in paediatric Crohn’s disease. Aliment Pharmacol Ther. 2022;56(3):384–95. https://doi.org/10.1111/apt.17109.
Cuomo M, Carobbio A, Aloi M, et al. Induction of remission with exclusive enteral nutrition in children with Crohn’s disease: determinants of higher adherence and response. Inflamm Bowel Dis. 2022. https://doi.org/10.1093/ibd/izac215.
Lee D, Baldassano RN, Otley AR, et al. Comparative effectiveness of nutritional and biological therapy in North American children with active Crohn’s disease. Inflamm Bowel Dis. 2015;21(8):1786–93. https://doi.org/10.1097/MIB.0000000000000426.
Chen JM, He LW, Yan T, et al. Oral exclusive enteral nutrition induces mucosal and transmural healing in patients with Crohn’s disease. Gastroenterol Rep (Oxf). 2019;7(3):176–84. https://doi.org/10.1093/gastro/goy050.
Levine A, Wine E, Assa A, et al. Crohn’s disease exclusion diet plus partial enteral nutrition induces sustained remission in a randomized controlled trial. Gastroenterology. 2019;157(2): 440–50.e8. https://doi.org/10.1053/j.gastro.2019.04.021.
Cohen SA, Gold BD, Oliva S, et al. Clinical and mucosal improvement with specific carbohydrate diet in pediatric Crohn disease. J Pediatr Gastroenterol Nutr. 2014;59(4):516–21. https://doi.org/10.1097/MPG.0000000000000449.
Suskind DL, Lee D, Kim YM, et al. The specific carbohydrate diet and diet modification as induction therapy for pediatric Crohn’s disease: a randomized diet controlled trial. Nutrients. 2020;12(12):3749. https://doi.org/10.3390/nu12123749.
Lewis JD, Sandler RS, Brotherton C, et al. A randomized trial comparing the specific carbohydrate diet to a Mediterranean diet in adults with Crohn’s disease. Gastroenterology. 2021;161(3): 837–52.e9. https://doi.org/10.1053/j.gastro.2021.05.047.
Pavlov VA, Chavan SS, Tracey KJ. Bioelectronic medicine: from preclinical studies on the inflammatory reflex to new approaches in disease diagnosis and treatment. Cold Spring Harb Perspect Med. 2020;10(3): a034140. https://doi.org/10.1101/cshperspect.a034140.
Sinniger V, Pellissier S, Fauvelle F, et al. A 12-month pilot study outcomes of vagus nerve stimulation in Crohn’s disease. Neurogastroenterol Motil. 2020;32(10): e13911. https://doi.org/10.1111/nmo.13911.
Sahn B, Lu Y, Hui-Yuen JS, et al. The safety of COVID-19 vaccination in immunocompromised children and young adults with immune-mediated inflammatory disease. Acta Paediatr. 2022;112(4):794–881. https://doi.org/10.1111/apa.16652.
Turner D, Griffiths AM, Wilson D, et al. Designing clinical trials in paediatric inflammatory bowel diseases: a PIBDnet commentary. Gut. 2020;69(1):32–41. https://doi.org/10.1136/gutjnl-2018-317987.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article.
Conflict of Interest
Julie Gallagher, Joel R. Rosh, and Benjamin Sahn have no conflicts of interest that are directly related to the content of this article.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Data Availability
Not applicable.
Code Availability
Not applicable.
Author Contributions
JG: conceptualization: lead; methodology: lead; writing, original draft: lead; writing, review and editing: lead. JR: conceptualization: support; writing, original draft: support; writing, review and editing: support. BS: conceptualization: lead; supervision: lead; writing, original draft: support; writing, review and editing: support.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gallagher, J., Rosh, J.R. & Sahn, B. The Future of Advanced Therapies for Pediatric Crohn’s Disease. Pediatr Drugs 25, 621–633 (2023). https://doi.org/10.1007/s40272-023-00590-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-023-00590-x