Abstract
Thyroid hormone has important physiologic functions in nearly every organ system. The critical role of thyroid hormone in growth and in physical and neurologic development lends particular importance to the prompt diagnosis and appropriate treatment of hypothyroidism in infants and children. Congenital hypothyroidism is common and has potentially devastating neurologic consequences. While the approach to diagnosis and treatment of severe congenital hypothyroidism is well established, data continue to emerge about the genetic causes, clinical significance, and prognosis of the milder forms of congenital hypothyroidism that are increasingly being diagnosed by newborn screening. Similarly, the diagnosis and treatment of severe acquired hypothyroidism is straightforward and clearly of clinical benefit, but uncertainty remains about the optimal management of mild subclinical hypothyroidism. This review summarizes current knowledge of the causes, clinical manifestations, diagnosis, treatment, and prognosis of hypothyroidism in infants and children, with a focus on recent developments and areas of uncertainty in this field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hypothyroidism in infants and children may have significant detrimental effects on health, growth, and development, but prompt diagnosis and treatment leads to excellent outcomes. |
Uncertainty remains about the optimal management of mild, subclinical forms of hypothyroidism in children. |
1 Introduction
The primary function of the thyroid gland is the production and secretion of thyroid hormone. Hypothyroidism occurs when the concentration of circulating thyroid hormone is inadequate to maintain a normal level of thyroid hormone signaling at the tissue level. Because thyroid hormone modulates the function of nearly every organ system, the consequences of hypothyroidism include important effects on cardiovascular, neurologic, gastrointestinal, and metabolic function. In children, thyroid hormone also plays a critical role in normal growth and development, and hypothyroidism results in significant impairments in these processes. Therefore, prompt recognition and treatment of hypothyroidism in infants and children is essential to optimizing physical and neurodevelopmental outcomes. This review aims to provide an overview of the causes of pediatric hypothyroidism and a practical approach to its diagnosis and treatment, including recent advances and controversies in this field.
2 Causes of Hypothyroidism in Infants and Children
Thyroid gland function is controlled directly by pituitary secretion of thyroid-stimulating hormone (TSH), which binds to its receptor on the thyroid follicular cell to stimulate thyroid hormone production and secretion as well as thyroid growth. Secretion of TSH by anterior pituitary thyrotropes is regulated in turn by thyrotropin-releasing hormone (TRH) secreted from the hypothalamus. In the hypothalamus and pituitary, circulating thyroid hormones suppress production of TRH and TSH, respectively, completing a negative feedback loop that maintains normal thyroid homeostasis.
The primary hormone secreted by the thyroid gland is thyroxine (T4). Circulating T4 has a long half-life (about 7 days) and functions as a prohormone that is converted in peripheral tissues to the biologically active hormone triiodothyronine (T3), which has a 15-fold higher affinity for thyroid hormone receptors than does T4. About 20% of circulating T3 is secreted directly by the thyroid. Pathophysiologically, causes of hypothyroidism can be divided into conditions that impair the function of the thyroid gland itself (primary hypothyroidism) and those that affect hypothalamic and/or pituitary control of the thyroid (central hypothyroidism). A number of rare disorders that cause hypothyroidism at the tissue level through alterations in the metabolism or transmembrane transport of thyroid hormone will not be discussed in this review.
2.1 Primary Hypothyroidism
2.1.1 Congenital Hypothyroidism
The first programs to establish universal neonatal screening for congenital hypothyroidism reported an incidence of about 1:3000–1:4000 births [1]; however, in the last decade the apparent incidence has nearly doubled to roughly 1:2000 births [2]. This change is due primarily to increased stringency of newborn screening (principally lowering of TSH thresholds for diagnosis), which has led to increased detection of milder cases but no change in the incidence of severe congenital hypothyroidism [3, 4]. Thyroid function abnormalities are present on newborn screening more commonly in infants born preterm or with low birth weight and in infants with trisomy 21 [5].
Congenital hypothyroidism may be caused by failure of normal thyroid gland development (dysgenesis) or by failure of an anatomically normal thyroid gland to produce thyroid hormone normally (dyshormonogenesis). Thyroid dysgenesis is more common and classically has accounted for 85% of congenital hypothyroidism, while dyshormonogenesis has accounted for only 15%. However, this pattern has shifted with recent changes in newborn screening strategies and demographics and, in several recent studies, 30–40% of infants diagnosed with congenital hypothyroidism had a eutopic thyroid gland consistent with a form of dyshormonogenesis [3, 4, 6].
Despite its relative frequency, thyroid dysgenesis remains a disorder whose causes are poorly understood. Most cases are sporadic, and it is doubtful that novel germline genetic changes will be found to account for a substantial proportion of thyroid dysgenesis given the high rate of discordance in monozygotic twins [7]. In fact, defects in known genes involved in thyroid development (such as PAX8, NKX2.1, and FOXE1) are found in only 2–5% of cases of thyroid dysgenesis [8]. In contrast, dyshormonogenesis is often caused by defects in the cellular machinery of thyroid hormone synthesis, including mutations of thyroglobulin (TG), thyroid peroxidase (TPO), dual oxidase 2 (DUOX2) and its associated protein (DUOXA2), the sodium-iodide symporter (SLC5A5), the apical iodide transporter pendrin (SLC26A4), and iodotyrosine deiodinase (IYD) [9]. Of these, mutations in DUOX2, TG, TPO, and the TSH receptor (TSHR) are most common, although the absolute and relative frequency of each varies substantially among studies, likely based on region, ethnicity, and clinical characteristics of the patient cohort examined [10,11,12,13].
Several extrinsic factors can cause hypothyroidism at birth or in the early neonatal period. Transplacental passage of antithyroid medications used to treat hyperthyroidism (methimazole, carbimazole, or propylthiouracil) or of maternal IgG antibodies that block activation of the TSH receptor can cause transient congenital hypothyroidism until the causative agent is cleared from the neonatal circulation. Iodine deficiency remains a common cause of neonatal hypothyroidism worldwide, although its global incidence has decreased dramatically with widespread introduction of salt iodization programs. Nevertheless, preterm infants remain at increased risk of iodine deficiency, particularly because of the low iodine content of preterm infant formulas and of the parental nutrition commonly used in intensive care nurseries [14]. Iodine excess can also cause hypothyroidism, particularly in preterm infants [15], and may originate from topical iodine-based antiseptics [16, 17], radiographic contrast agents [18], or high maternal dietary intake of iodine that is passed through breast milk [19, 20].
2.1.2 Acquired Hypothyroidism
The most common cause of acquired hypothyroidism in children is autoimmune thyroiditis, a T-cell-mediated response to thyroid autoantigens leading to inflammation, fibrosis, and impaired function of the thyroid. The underlying cause of autoimmune thyroiditis is not known, but the disorder is associated with numerous genetic loci including those related to the thyroid itself and to immune functions including CTLA-4, PTPN22, FOXP3, and the human leukocyte antigen (HLA) DR3 allele [21]. The incidence of autoimmune thyroiditis increases with age: it is rare in the first 3 years of life and becomes progressively more common through school age and adolescence. It is more common in females and in patients with trisomy 21 and Turner syndrome.
Other causes of thyroiditis besides autoimmunity may lead to acquired hypothyroidism. Thyroiditis occurring after a viral infection is often (but not always) associated with fever and thyroid tenderness, and is usually transient. Acute suppurative thyroiditis due to bacteria or fungi occurs rarely, usually in patients with pyriform sinus fistulae and/or immunocompromise, but these infections generally cause symptoms of local and systemic inflammation without significant abnormalities of thyroid function. Numerous medications can cause hypothyroidism including lithium, amiodarone, certain antiepileptics, biological agents like interferons and interleukins, and antithyroid medications (Table 1).
Iodine deficiency remains an important cause of acquired hypothyroidism in areas of the world with insufficient dietary iodine. On the other hand, recently attention has been drawn to the possible role of iatrogenic iodine excess from radiographic contrast as a potentially underappreciated cause of hypothyroidism in children. A recent study demonstrated that the odds of developing hypothyroidism are increased 2.6-fold in children receiving iodinated radiographic contrast compared with controls [22], but the duration and clinical significance of this hypothyroidism remain unclear. Certain cough suppressants and nutritional supplements may also contain large amounts of iodine that can suppress thyroid function. Iatrogenic hypothyroidism may occur after surgical thyroidectomy, radioiodine ablation for Graves’ disease, or exposure to external radiation (such as for cancer therapy). Children with mild defects in certain genes that can cause congenital hypothyroidism (such as DUOX2) may present with hypothyroidism later in childhood rather than at birth [23]. Rarely, a large hepatic hemangioma may cause consumptive hypothyroidism in an infant due to massive overexpression of the enzyme type 3 deiodinase, which converts both T4 and T3 to inactive metabolites [24].
2.2 Central Hypothyroidism
Because central hypothyroidism is caused by defects in hypothalamic or pituitary control of the thyroid axis, this type of hypothyroidism is usually associated with deficits of other pituitary hormones including growth hormone, gonadotropins, and adrenocorticotrophic hormone (ACTH). Congenital central hypothyroidism is rare, with an incidence between 1:16,000 and 1:110,000 [25,26,27], and is usually caused by inborn structural or functional defects. Some of these defects are caused by mutations in one of many genes involved in hypothalamic and pituitary development [28]. Multiple pituitary hormone deficiencies are present in about 75% of infants with congenital central hypothyroidism [29], but very rare cases of isolated congenital central hypothyroidism may be due to mutations in the TRH receptor (TRHR) [30], the TSH β-subunit (TSHB) [31], IGSF1 [32], or the newly implicated gene TBL1X [33]. Acquired central hypothyroidism is caused by structural changes, mass lesions, trauma, or central nervous system infection or inflammation affecting the hypothalamus or pituitary, and it is generally accompanied by multiple pituitary hormone deficits.
3 Clinical Manifestations of Hypothyroidism
Thyroid hormone signaling plays an important role in diverse physiologic processes. In addition to being critical for normal growth and neurodevelopment, thyroid hormone raises basal metabolic rate and body temperature; increases heart rate, decreases systemic vascular resistance, and increases cardiac output; promotes gastrointestinal motility; and increases renal clearance of salt and water. Common signs and symptoms of hypothyroidism are listed in Table 2, but these are highly variable among individuals and do not necessarily correlate with the degree of biochemical hypothyroidism. Therefore, any clinical suspicion of hypothyroidism in a child should prompt laboratory testing of thyroid function.
Because thyroid hormone is essential for normal neurologic and cognitive development [34], hypothyroidism in infants poses a risk of severe neurocognitive deficits if not treated promptly and adequately. Moreover, infants (particularly in the first few weeks of life) may manifest few or no symptoms even with significant hypothyroidism, making clinical diagnosis difficult in this age group. Fortunately, universal newborn screening has virtually eliminated severe intellectual disability due to congenital hypothyroidism in the developed world, but congenital hypothyroidism remains a leading cause of preventable intellectual disability in areas without newborn screening programs. Even in areas with active screening programs, up to 10% of cases of congenital hypothyroidism may not be detected by screening in the first few days of life [35, 36], so a high index of suspicion for hypothyroidism is necessary in any infant with poor growth, developmental delay, prolonged indirect hyperbilirubinemia, or other suggestive findings.
Symptoms of hypothyroidism in older children are often subtle and nonspecific, such as fatigue, cold intolerance, weight gain or constipation. Evaluation for primary hypothyroidism is often prompted by the finding of thyroid enlargement (goiter) or impaired linear growth. Hypothyroidism may cause delayed puberty, but rarely severe cases can cause pseudo-precocious puberty with breast development and/or premature menarche in girls [37] or testicular enlargement in boys [38]. This effect is presumably due to cross-reactivity of high serum concentrations of TSH with the follicle-stimulating hormone (FSH) receptor [39]. Such pseudoprecocity is distinguished from true precocious puberty by the presence of retarded—rather than accelerated—growth and bone maturation.
4 Diagnosis of Hypothyroidism
The diagnosis of hypothyroidism rests on biochemical confirmation of inadequate thyroid function by measuring serum concentrations of TSH and total or free T4. Thyroid hormones circulate bound to plasma proteins, and their biological action is exerted only by the tiny fraction of circulating hormone (0.02–0.1%) that is unbound or ‘free.’ The serum free T4 concentration can be assayed directly or can be estimated by using the total T4 concentration along with a measurement of protein binding (such as a thyroid hormone binding ratio) to calculate a ‘free T4 index.’ The direct free T4 assays available in most clinical laboratories are generally reliable in otherwise healthy ambulatory patients but may be inaccurate in patients with severe systemic illness or abnormalities of protein binding, so caution is needed when interpreting such tests in this setting.
In primary hypothyroidism, TSH elevation is the first detectable abnormality, with free T4 levels falling only when hypothyroidism becomes more severe. For this reason, TSH is the single most sensitive test for diagnosing primary hypothyroidism and for monitoring its treatment. In contrast, central hypothyroidism should be suspected when free T4 is low and TSH is low or normal (i.e., not appropriately elevated in response to low free T4). During hypothyroidism, changes in thyroid hormone metabolism serve to maintain normal circulating levels of T3 until the late stages of disease. For this reason, measurement of serum T3 or free T3 generally is not useful in the evaluation of hypothyroidism.
In infants and children, the normal ranges of serum TSH and free T4 differ by age. Therefore, it is important to use appropriate age-specific reference ranges when interpreting pediatric thyroid function tests [40,41,42]. Evaluation of a patient’s thyroid status may be affected by numerous medications (Table 1) as well as by the presence of nonthyroidal illness (‘euthyroid sick syndrome’), which causes changes in thyroid function tests that can mimic true thyroid dysfunction [43]. A careful history and physical examination is needed to identify such potential confounding factors.
4.1 Diagnosis of Congenital Hypothyroidism
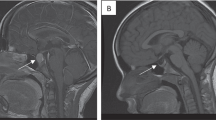
Universal newborn screening for congenital hypothyroidism is practiced in many countries [2]. Screening protocols vary by region but generally begin with measurement of TSH and/or T4 in a dried blood spot collected from each infant within a few days after birth. Prompt diagnosis and treatment of congenital hypothyroidism is critical for ensuring optimal developmental outcome, so any abnormal newborn screen result should prompt immediate confirmation of TSH and free T4 concentrations in a serum sample. TSH elevation, with or without low free T4, indicates the presence of congenital primary hypothyroidism. Central hypothyroidism may be present if free T4 is low and TSH is normal or low; however, this condition can be difficult to diagnose, particularly in ill or preterm infants (see below). If central hypothyroidism is confirmed, further evaluation should include assessment for other pituitary hormone deficits and brain imaging that includes the hypothalamus and pituitary. Examination of the optic discs by a pediatric ophthalmologist may reveal evidence of associated septo-optic dysplasia.
Many variables can influence the interpretation of newborn screening results, including the timing of sample collection and patient characteristics. Blood samples obtained within the first 24 h of life may give false-positive results due to the surge in TSH secretion (up to 60–80 mIU/L) that normally occurs within hours after birth. Preterm, low birth weight, or ill neonates may have altered patterns of thyroid function that may confound newborn screening, including low free T4 with normal or low TSH that mimics central hypothyroidism [44], or primary hypothyroidism with a delayed rise in TSH [45] that may be missed by early screening (see Sect. 5.3.2). Because of these issues, gestational age- and postnatal age-specific reference ranges should be used when interpreting neonatal thyroid function tests [46], and prompt consultation with a pediatric endocrinologist should be pursued in uncertain cases.
In infants with congenital hypothyroidism, determination of the etiology frequently does not alter initial management but may provide insight into prognosis. The presence or absence of a normally located thyroid gland can be assessed by ultrasound or thyroid scintigraphy (using 99mTc or 123I), which can help distinguish between thyroid dysgenesis and dyshormonogenesis. While hypothyroidism due to dysgenesis is usually permanent, about 35% of patients with a eutopic thyroid gland have transient disease and will not require lifelong therapy [47,48,49]. The potential presence of TSH receptor-blocking antibodies should be considered in patients with a eutopic thyroid gland on ultrasound even if there is no maternal history of autoimmune thyroid disease [50]. If TSH receptor antibodies are documented in maternal or neonatal serum, they portend a transient course of hypothyroidism that resolves within 3–4 months [51], although neurodevelopment may be impaired if the mother had unrecognized hypothyroidism during gestation, even with institution of prompt postnatal treatment [50].
4.2 Diagnosis of Acquired Hypothyroidism
Most cases of acquired hypothyroidism in children are caused by autoimmune thyroiditis. Circulating autoantibodies to thyroperoxidase and/or thyroglobulin are detectable in about 95% of such patients, and their presence is sufficient to confirm the diagnosis of autoimmune thyroiditis. A detailed medical, dietary, and medication history should reveal other causes of acquired hypothyroidism. Symptoms of fever and thyroid tenderness suggest infectious (usually postviral) thyroiditis. Measurement of urinary iodine concentration can diagnose iodine deficiency or excess. Thyroid imaging is generally not necessary in the evaluation of hypothyroidism, although the finding of heterogeneous echotexture on ultrasound may support a diagnosis of autoimmune thyroiditis in antibody-negative cases of uncertain etiology. As in infants, a diagnosis of central hypothyroidism in an older child or adolescent should prompt brain imaging and evaluation for other pituitary hormone deficits.
5 Treatment and Prognosis of Hypothyroidism
Treatment of hypothyroidism consists of replacing the deficiency of thyroid hormone to improve symptoms and prevent the adverse consequences of hypothyroidism. As in adults, levothyroxine (LT4) is the recommended treatment for hypothyroidism in children. In primary hypothyroidism, serum TSH is the most sensitive measure of thyroid status, and the goal of therapy is to maintain serum TSH within the age-specific normal range [52]. At present, data do not convincingly indicate a clinical benefit of maintaining TSH within a lower range (e.g., 0.5–2 mIU/L). For central hypothyroidism, in which by definition serum TSH does not reflect systemic thyroid status, serum free T4 levels should be maintained in the upper half of the reference range [52].
The dose of LT4 required to restore euthyroidism depends on patient age and on the severity of hypothyroidism. The dose required per kilogram body mass to fully replace thyroid function is significantly higher in children than in adults and decreases with age (Table 3). After starting therapy, thyroid function must be assessed and the LT4 dose adjusted regularly to achieve and maintain consistent euthyroidism.
In the United States, LT4 should be administered in tablet form only given the inconsistency of the liquid formulations available. For infants, LT4 tablets should be crushed, suspended, and administered in a small volume of water, breast milk, or infant formula. Older children can chew or swallow tablets. Although LT4 formulations produced by different manufacturers may vary slightly [despite apparent bioequivalence as determined by the Food and Drug Administration (FDA)], it remains uncertain whether—or under what circumstances—there is a clinically significant difference between generic and brand-name LT4 preparations in children. Limited data suggest that brand-name LT4 may be superior to generic in children with severe congenital hypothyroidism, but not in those with equally severe acquired hypothyroidism [53]. LT4 should not be administered with substances that can affect its absorption, including calcium or iron supplements, or soy products. The latter is particularly important in infants with congenital hypothyroidism, in whom introduction of soy-based infant formula is a well described cause of undertreatment [54, 55]. Celiac disease, more common in older children and adolescents, can also impair absorption of LT4 [56].
Some patients do not experience complete resolution of hypothyroid symptoms when treated with sufficient LT4 to normalize their TSH and free T4. It has been proposed that this may be due to the lower (though still normal) levels of serum T3 that are generally observed in hypothyroid patients treated with LT4, and that therefore addition of liothyronine (LT3) to traditional LT4 monotherapy may be beneficial in such patients [57]. The identification of a common polymorphism in the enzyme type 2 deiodinase that might alter conversion of T4 to T3 has generated interest as a potential pathophysiological rationale for this hypothesis [58]. However, this remains a theoretical prospect and the preponderance of clinical evidence does not support any benefit of combined LT4 + LT3 therapy over LT4 alone in most patients [59]. Therefore, LT3 treatment is not recommended routinely for the treatment of hypothyroidism in adults or children [52].
5.1 Treatment of Hypothyroidism in Infants
Because thyroid hormone plays a critical role in normal neurologic development, particularly through the first 3 years of life, infants with suspected hypothyroidism require rapid evaluation and treatment. As noted above, abnormal newborn screening results should be confirmed immediately by measurement of serum TSH and free T4 levels. LT4 should be initiated without delay in any patient with confirmatory serum TSH >20 mIU/L, or with TSH 6–20 mIU/L and low free T4 levels [60]. In infants whose screening whole blood TSH is >40 mIU/L, LT4 should be initiated as soon as the confirmatory serum sample is obtained, without awaiting the results. Optimally, treatment should be initiated no later than 2 weeks of age, since delays in treatment of congenital hypothyroidism are correlated with poorer outcomes [60,61,62].
The management of infants with mild TSH elevation (serum TSH 6–20 mIU/L) and normal free T4 levels is controversial. Although an increasing number of these patients is being identified by more stringent newborn screening thresholds, the precise neurodevelopmental risks posed by untreated mild disease remain uncertain [63]. One study of 284 Belgian children found no association between mild TSH elevation on newborn screening and psychomotor development at preschool age [64]. In contrast, a much larger study of over 500,000 Australian children found that mild elevations of newborn whole blood TSH were associated with poorer academic performance and greater odds of having special needs, after adjustment for potential confounders [65]. However, this retrospective study could not demonstrate causality, and (likely for ethical reasons) few studies have rigorously investigated whether infants with mild subclinical congenital hypothyroidism benefit from LT4 treatment. Therefore, many practitioners elect to treat infants with such mild subclinical congenital hypothyroidism to prevent any possible adverse developmental effects, but withholding treatment and closely monitoring thyroid function is also reasonable, in discussion with the family [60].
Infants diagnosed with congenital hypothyroidism should be treated with LT4 10–15 μg/kg daily. Starting treatment early with an adequate dose of LT4 facilitates rapid normalization of thyroid function, which appears to improve outcomes [61, 66,67,68]. However, high doses of LT4 can quickly result in overtreatment [69], which has also been associated with impaired development and decreased IQ [70]. Therefore, close monitoring of serum thyroid function tests 1–2 weeks after starting treatment and every 2–4 weeks thereafter, with adjustment of LT4 dose as appropriate, is necessary until they have normalized.
Since both undertreatment and overtreatment of congenital hypothyroidism are associated with adverse neurocognitive sequelae, the goal of ongoing management is scrupulous maintenance of euthyroidism, particularly in the first 3 years of life. Serum TSH should be maintained in the age-specific normal range, and serum free T4 should be maintained in the upper half of the age-specific normal range. To achieve this goal, frequent monitoring of serum thyroid function tests is necessary every 1–2 months in the first 6 months of life, every 1–3 months in the second 6 months, and then every 2–4 months through to 3 years of age. TSH and free T4 should also be checked 4 weeks after any change in LT4 dose. For a detailed review of evidence and recommendations for the diagnosis and management of congenital hypothyroidism, the reader is referred to comprehensive consensus guidelines on this topic [60, 62].
In patients who are not known to have thyroid dysgenesis, a trial off LT4 may be appropriate after 3 years of age to assess whether hypothyroidism is permanent. In patients with a eutopic thyroid gland, the degree of TSH elevation at diagnosis is not predictive of disease permanence, but patients who require <2 μg/kg of LT4 daily are more likely to have transient disease [47].
The prognosis of children born with congenital hypothyroidism is generally excellent. Early and adequate treatment with LT4 prevents severe neurocognitive deficits and results in normal global intelligence (IQ). However, in spite of optimal postnatal treatment, mild deficits may persist in several domains—including motor development, verbal skills, attention, and memory—particularly in children born with severe hypothyroidism [71,72,73,74]. Hearing deficits are also present in about 10% of patients with congenital hypothyroidism [75]. Patients and families should be counseled about these issues, and careful monitoring of development and academic progress is important to identify and address any problems early.
5.2 Treatment of Hypothyroidism in Children and Adolescents
For older children and adolescents with hypothyroidism, the dose of LT4 necessary to restore euthyroidism depends on both severity of the hypothyroidism and the age of the patient (Table 3). Patients with acquired hypothyroidism can generally be initiated immediately on the chosen dose of LT4 at the time of diagnosis. In rare cases, initiation of treatment in a child with severe hypothyroidism can be associated with severe behavioral symptoms [76] or pseudotumor cerebri [77]; however, it is not clear whether initiating a lower dose and increasing it over time decreases the risk of such reactions [77]. Once a child is stably euthyroid on LT4, TSH can be monitored every 6 months until the end of puberty and linear growth, and annually thereafter, as well as 4–8 weeks after any change in LT4 dose. Annual TSH monitoring may also be sufficient for older children who have demonstrated good adherence and stable euthyroidism on treatment. Monitoring of free T4 is useful in certain situations, such as when treatment nonadherence is suspected or in certain patients with congenital hypothyroidism who manifest a persistent pattern of simultaneously elevated TSH and free T4.
Treatment of acquired hypothyroidism is highly effective and results in the resolution of most symptoms. Significant weight loss is usually not observed [78]. Importantly, poor growth sustained during long-standing hypothyroidism may not be compensated after initiation of treatment, leading to an irremediable loss of adult height [79]. Adolescent female patients should be counseled about the potential need for increased LT4 dosing during future pregnancy or with use of estrogen-containing contraceptives, as well as the small but potentially serious risk of TSH receptor-blocking antibodies that could cause hypothyroidism in a future child.
5.3 Special Considerations
5.3.1 Subclinical Hypothyroidism
The state of mild primary hypothyroidism characterized by elevated serum TSH but free T4 concentrations within the normal range is termed subclinical hypothyroidism. Whether subclinical hypothyroidism is associated with adverse consequences in children remains uncertain. The issue of subclinical congenital hypothyroidism is discussed in Sect. 5.1. In older children, studies have examined the potential effects of subclinical hypothyroidism on such outcomes as cardiovascular health, lipid profile, cognitive function and behavior, and bone health (recently reviewed in [80]). Overall, subclinical hypothyroidism does not appear to have clinically significant adverse effects in any of these areas, but confidence in this conclusion is limited by the quality of many of the studies, and whether a subtle effect could potentially be present remains to be determined.
While subclinical hypothyroidism is often envisioned as an intermediate step on the path to overt hypothyroidism, this progression is far from certain in the pediatric population. In fact, subclinical hypothyroidism in children frequently resolves without treatment or may persist for long periods without progressing to overt hypothyroidism. In a large Israeli study, 74% of children with TSH 5.5–10 mIU/L reverted to euthyroidism and only 8.5% progressed to highly elevated TSH (>10 mIU/L) over 5 years [81]. Progression from subclinical to overt hypothyroidism is more common in children with autoimmune thyroiditis, but even in this group progression occurs in only 31% over 4 years, while 34% revert to euthyroidism over the same period [80]. Finally, even in infants under 1 year of age, in whom the threshold for treatment may be lower due to concerns about neurodevelopment, a large retrospective study demonstrated that mild subclinical TSH elevation (5–10 mIU/L) resolved spontaneously in 72% of infants and persisted without worsening in 18% over a median of 5 months, while only 10% progressed to worse hypothyroidism (TSH >10 mIU/L) [82].
Uncertainty about the clinical consequences of subclinical hypothyroidism and its variable natural history contribute to significant variation in the management of this condition, and high-quality evidence to guide treatment decisions is lacking. In general, treatment should be considered for children with persistent subclinical hypothyroidism who are under 3 years of age, who have symptoms strongly suggestive of hypothyroidism, or whose TSH is above 10 mIU/L. On the other hand, children with milder subclinical hypothyroidism can often be observed without treatment.
5.3.2 Preterm and Low Birth Weight Infants
Infants born preterm (<37 weeks) and/or with low birth weight (<2500 g) have a distinct pattern of postnatal thyroid function from term infants of normal weight. Differences include a smaller postnatal surge in TSH levels and lower initial serum total and free T4 concentrations that may decrease during the first days of life (rather than increase as in term infants). These differences are due to multiple factors including immaturity of the hypothalamic–pituitary–thyroid axis; loss of maternal T4 that would normally be transferred to the fetus in the third trimester; changes in thyroid hormone metabolism; frequent and often severe illness in these neonates; and exposure to medications that may affect thyroid function (such as dopamine, glucocorticoids, and iodine-contained antiseptics). As a result, preterm and low birth weight infants often present with abnormalities of thyroid function that require evaluation and possible treatment.
As in term infants, the presence of TSH elevation in a preterm or low birth weight infant indicates primary hypothyroidism that should be managed as congenital primary hypothyroidism (see Sect. 5.1). However, the natural history of thyroid function in these infants frequently results in a state of low T4 (or free T4) without TSH elevation, a pattern resembling central hypothyroidism or nonthyroidal illness. Although concern has existed for decades that this so-called ‘hypothyroxinemia of prematurity’ is harmful to neurodevelopment [83], studies have produced conflicting results. The only randomized, controlled trial to address this question showed no effect of LT4 treatment on clinical or neurodevelopmental outcomes at 2 years of age [84]. Although a post hoc subgroup analysis showed a possible benefit of LT4 in infants born before 27 weeks’ gestation, a significant benefit did not persist at 10 years of age [85]. Furthermore, other recent studies have shown no association between low free T4 in preterm infants and developmental outcomes [86], or even improved outcomes in infants with lower free T4 [87]. In summary, it remains uncertain whether treatment is beneficial for preterm or low birth weight infants with low T4 and no TSH elevation. However, if treatment with LT4 is elected, a starting dose of 8 μg/kg/day may be optimal for normalizing serum free T4 levels [88].
6 Summary
Pediatric hypothyroidism is common, and the combination of routine newborn screening and careful clinical observation should allow for prompt diagnosis and institution of treatment, which is highly effective and results in excellent outcomes in the vast majority of cases. While autoimmune thyroiditis remains the dominant cause of acquired hypothyroidism in children, the fundamental pathophysiology of most congenital hypothyroidism remains an enigma despite continued advances in our understanding of the genetic causes of dyshormonogenesis and central hypothyroidism. While the rationale for and approach to treating overt hypothyroidism are sound and generally uncontroversial, uncertainty still surrounds the issue of subclinical hypothyroidism, including whether this state has adverse clinical consequences and merits treatment. This uncertainty is particularly acute in the case of subclinical congenital hypothyroidism, given the high developmental stakes. Further high-quality, ideally prospective studies are necessary to provide evidence-based guidance on the management of these issues commonly faced by pediatricians in practice.
References
Fisher DA, Dussault JH, Foley TP Jr, Klein AH, LaFranchi S, Larsen PR, et al. Screening for congenital hypothyroidism: results of screening one million North American infants. J Pediatr. 1979;94(5):700–5.
Ford G, LaFranchi SH. Screening for congenital hypothyroidism: a worldwide view of strategies. Best Pract Res Clin Endocrinol Metab. 2014;28(2):175–87.
Deladoey J, Ruel J, Giguere Y, Van Vliet G. Is the incidence of congenital hypothyroidism really increasing? A 20-year retrospective population-based study in Quebec. J Clin Endocrinol Metab. 2011;96(8):2422–9.
Olivieri A, Fazzini C, Medda E. Collaborators. Multiple factors influencing the incidence of congenital hypothyroidism detected by neonatal screening. Horm Res. Paediatr. 2015;83(2):86–93.
van Trotsenburg AS, Vulsma T, van Santen HM, Cheung W, de Vijlder JJ. Lower neonatal screening thyroxine concentrations in down syndrome newborns. J Clin Endocrinol Metab. 2003;88(4):1512–5.
Chiesa A, Prieto L, Mendez V, Papendieck P, Calcagno Mde L, Gruneiro-Papendieck L. Prevalence and etiology of congenital hypothyroidism detected through an argentine neonatal screening program (1997–2010). Horm Res Paediatr. 2013;80(3):185–92.
Perry R, Heinrichs C, Bourdoux P, Khoury K, Szots F, Dussault JH, et al. Discordance of monozygotic twins for thyroid dysgenesis: implications for screening and for molecular pathophysiology. J Clin Endocrinol Metab. 2002;87(9):4072–7.
Nettore IC, Cacace V, De Fusco C, Colao A, Macchia PE. The molecular causes of thyroid dysgenesis: a systematic review. J Endocrinol Invest. 2013;36(8):654–64.
Grasberger H, Refetoff S. Genetic causes of congenital hypothyroidism due to dyshormonogenesis. Curr Opin Pediatr. 2011;23(4):421–8.
Nicholas AK, Serra EG, Cangul H, Alyaarubi S, Ullah I, Schoenmakers E, et al. Comprehensive screening of eight known causative genes in congenital hypothyroidism with gland-in-situ. J Clin Endocrinol Metab. 2016;101(12):4521–31.
Narumi S, Muroya K, Asakura Y, Aachi M, Hasegawa T. Molecular basis of thyroid dyshormonogenesis: genetic screening in population-based Japanese patients. J Clin Endocrinol Metab. 2011;96(11):E1838–42.
Fu C, Wang J, Luo S, Yang Q, Li Q, Zheng H, et al. Next-generation sequencing analysis of TSHR in 384 Chinese subclinical congenital hypothyroidism (CH) and CH patients. Clin Chim Acta. 2016;01(462):127–32.
Park KJ, Park HK, Kim YJ, Lee KR, Park JH, Park JH, et al. DUOX2 mutations are frequently associated with congenital hypothyroidism in the Korean population. Ann Lab Med. 2016;36(2):145–53.
Belfort MB, Pearce EN, Braverman LE, He X, Brown RS. Low iodine content in the diets of hospitalized preterm infants. J Clin Endocrinol Metab. 2012;97(4):E632–6.
Ahmet A, Lawson ML, Babyn P, Tricco AC. Hypothyroidism in neonates post-iodinated contrast media: a systematic review. Acta Paediatr. 2009;98(10):1568–74.
Linder N, Davidovitch N, Reichman B, Kuint J, Lubin D, Meyerovitch J, et al. Topical iodine-containing antiseptics and subclinical hypothyroidism in preterm infants. J Pediatr. 1997;131(3):434–9.
Williams FL, Watson J, Day C, Soe A, Somisetty SK, Jackson L, et al. Thyroid dysfunction in preterm neonates exposed to iodine. J Perinat Med. 2017;45(1):135–43.
Thaker VV, Leung AM, Braverman LE, Brown RS, Levine B. Iodine-induced hypothyroidism in full-term infants with congenital heart disease: more common than currently appreciated? J Clin Endocrinol Metab. 2014;99(10):3521–6.
Chung HR, Shin CH, Yang SW, Choi CW, Kim BI. Subclinical hypothyroidism in Korean preterm infants associated with high levels of iodine in breast milk. J Clin Endocrinol Metab. 2009;94(11):4444–7.
Connelly KJ, Boston BA, Pearce EN, Sesser D, Snyder D, Braverman LE, et al. Congenital hypothyroidism caused by excess prenatal maternal iodine ingestion. J Pediatr. 2012;161(4):760–2.
Lee HJ, Li CW, Hammerstad SS, Stefan M, Tomer Y. Immunogenetics of autoimmune thyroid diseases: a comprehensive review. J Autoimmun. 2015;64:82–90.
Barr ML, Chiu HK, Li N, Yeh MW, Rhee CM, Casillas J, et al. Thyroid dysfunction in children exposed to iodinated contrast media. J Clin Endocrinol Metab. 2016;101(6):2366–70.
Ohye H, Fukata S, Hishinuma A, Kudo T, Nishihara E, Ito M, et al. A novel homozygous missense mutation of the dual oxidase 2 (DUOX2) gene in an adult patient with large goiter. Thyroid. 2008;18(5):561–6.
Huang SA, Tu HM, Harney JW, Venihaki M, Butte AJ, Kozakewich HP, et al. Severe hypothyroidism caused by type 3 iodothyronine deiodinase in infantile hemangiomas. N Engl J Med. 2000;343(3):185–9.
Lanting CI, van Tijn DA, Loeber JG, Vulsma T, de Vijlder JJ, Verkerk PH. Clinical effectiveness and cost-effectiveness of the use of the thyroxine/thyroxine-binding globulin ratio to detect congenital hypothyroidism of thyroidal and central origin in a neonatal screening program. Pediatrics. 2005;116(1):168–73.
Hanna CE, Krainz PL, Skeels MR, Miyahira RS, Sesser DE, LaFranchi SH. Detection of congenital hypopituitary hypothyroidism: ten-year experience in the northwest regional screening program. J Pediatr. 1986;109(6):959–64.
Persani L. Central hypothyroidism: pathogenic, diagnostic, and therapeutic challenges. J Clin Endocrinol Metab. 2012;97(9):3068–78.
Schoenmakers N, Alatzoglou KS, Chatterjee VK, Dattani MT. Recent advances in central congenital hypothyroidism. J Endocrinol. 2015;227(3):R51–71.
van Tijn DA, de Vijlder JJ, Verbeeten B Jr, Verkerk PH, Vulsma T. Neonatal detection of congenital hypothyroidism of central origin. J Clin Endocrinol Metab. 2005;90(6):3350–9.
Collu R, Tang J, Castagne J, Lagace G, Masson N, Huot C, et al. A novel mechanism for isolated central hypothyroidism: inactivating mutations in the thyrotropin-releasing hormone receptor gene. J Clin Endocrinol Metab. 1997;82(5):1561–5.
Nicholas AK, Jaleel S, Lyons G, Schoenmakers E, Dattani MT, Crowne E, et al. Molecular spectrum of TSHbeta subunit gene defects in central hypothyroidism in the UK and Ireland. Clin Endocrinol (Oxf). 2017;86(3):410–8.
Joustra SD, Schoenmakers N, Persani L, Campi I, Bonomi M, Radetti G, et al. The IGSF1 deficiency syndrome: characteristics of male and female patients. J Clin Endocrinol Metab. 2013;98(12):4942–52.
Heinen CA, Losekoot M, Sun Y, Watson PJ, Fairall L, Joustra SD, et al. Mutations in TBL1X are associated with central hypothyroidism. J Clin Endocrinol Metab. 2016;101(12):4564–73.
Rovet JF. The role of thyroid hormones for brain development and cognitive function. Endocr Dev. 2014;26:26–43.
LaFranchi SH, Hanna CE, Krainz PL, Skeels MR, Miyahira RS, Sesser DE. Screening for congenital hypothyroidism with specimen collection at two time periods: results of the northwest regional screening program. Pediatrics. 1985;76(5):734–40.
Ford GA, Denniston S, Sesser D, Skeels MR, LaFranchi SH. Transient versus permanent congenital hypothyroidism after the age of 3 years in infants detected on the first versus second newborn screening test in Oregon, USA. Horm Res Paediatr. 2016;86(3):169–77.
Van Wyk JJ, Grumbach MM. Syndrome of precocious menstruation and galactorrhea in juvenile hypothyroidism: an example of hormonal overlap in pituitary feedback. J Pediatr. 1960;57(3):416–35.
Franks RC, Stempfel RS Jr. Juvenile hypothyroidism and precocious testicular maturation. J Clin Endocrinol Metab. 1963;23:805–10.
Anasti JN, Flack MR, Froehlich J, Nelson LM, Nisula BC. A potential novel mechanism for precocious puberty in juvenile hypothyroidism. J Clin Endocrinol Metab. 1995;80(1):276–9.
Elmlinger MW, Kuhnel W, Lambrecht HG, Ranke MB. Reference intervals from birth to adulthood for serum thyroxine (T4), triiodothyronine (T3), free T3, free T4, thyroxine binding globulin (TBG) and thyrotropin (TSH). Clin Chem Lab Med CCLM FESCC. 2001;39(10):973–9.
Chaler EA, Fiorenzano R, Chilelli C, Llinares V, Areny G, Herzovich V, et al. Age-specific thyroid hormone and thyrotropin reference intervals for a pediatric and adolescent population. Clin Chem Lab Med CCLM FESCC. 2012;50(5):885–90.
Bailey D, Colantonio D, Kyriakopoulou L, Cohen AH, Chan MK, Armbruster D, et al. Marked biological variance in endocrine and biochemical markers in childhood: establishment of pediatric reference intervals using healthy community children from the CALIPER cohort. Clin Chem. 2013;59(9):1393–405.
Fliers E, Bianco AC, Langouche L, Boelen A. Thyroid function in critically ill patients. Lancet Diabetes Endocrinol. 2015;3(10):816–25.
La Gamma EF, Paneth N. Clinical importance of hypothyroxinemia in the preterm infant and a discussion of treatment concerns. Curr Opin Pediatr. 2012;24(2):172–80.
Woo HC, Lizarda A, Tucker R, Mitchell ML, Vohr B, Oh W, et al. Congenital hypothyroidism with a delayed thyroid-stimulating hormone elevation in very premature infants: incidence and growth and developmental outcomes. J Pediatr. 2011;158(4):538–42.
Williams FL, Simpson J, Delahunty C, Ogston SA, Bongers-Schokking JJ, Murphy N, et al. Developmental trends in cord and postpartum serum thyroid hormones in preterm infants. J Clin Endocrinol Metab. 2004;89(11):5314–20.
Rabbiosi S, Vigone MC, Cortinovis F, Zamproni I, Fugazzola L, Persani L, et al. Congenital hypothyroidism with eutopic thyroid gland: analysis of clinical and biochemical features at diagnosis and after re-evaluation. J Clin Endocrinol Metab. 2013;98(4):1395–402.
Castanet M, Goischke A, Leger J, Thalassinos C, Rodrigue D, Cabrol S, et al. Natural history and management of congenital hypothyroidism with in situ thyroid gland. Horm Res Paediatr. 2015;83(2):102–10.
Wassner AJ, Brown RS. Congenital hypothyroidism: recent advances. Curr Opin Endocrinol Diabetes Obes. 2015;22(5):407–12.
Brown RS, Alter CA, Sadeghi-Nejad A. Severe unsuspected maternal hypothyroidism discovered after the diagnosis of thyrotropin receptor-blocking antibody-induced congenital hypothyroidism in the neonate: failure to recognize and implications to the fetus. Horm Res Paediatr. 2015;83(2):132–5.
Brown RS, Bellisario RL, Botero D, Fournier L, Abrams CA, Cowger ML, et al. Incidence of transient congenital hypothyroidism due to maternal thyrotropin receptor-blocking antibodies in over one million babies. J Clin Endocrinol Metab. 1996;81(3):1147–51.
Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association task force on thyroid hormone replacement. Thyroid. 2014;24(12):1670–751.
Carswell JM, Gordon JH, Popovsky E, Hale A, Brown RS. Generic and brand-name l-thyroxine are not bioequivalent for children with severe congenital hypothyroidism. J Clin Endocrinol Metab. 2013;98(2):610–7.
Chorazy PA, Himelhoch S, Hopwood NJ, Greger NG, Postellon DC. Persistent hypothyroidism in an infant receiving a soy formula: case report and review of the literature. Pediatrics. 1995;96(1 Pt 1):148–50.
Conrad SC, Chiu H, Silverman BL. Soy formula complicates management of congenital hypothyroidism. Arch Dis Child. 2004;89(1):37–40.
Virili C, Bassotti G, Santaguida MG, Iuorio R, Del Duca SC, Mercuri V, et al. Atypical celiac disease as cause of increased need for thyroxine: a systematic study. J Clin Endocrinol Metab. 2012;97(3):E419–22.
Bianco AC, Casula S. Thyroid hormone replacement therapy: three ‘simple’ questions, complex answers. Eur Thyroid J. 2012;1(2):88–98.
Panicker V, Saravanan P, Vaidya B, Evans J, Hattersley AT, Frayling TM, et al. Common variation in the DIO2 gene predicts baseline psychological well-being and response to combination thyroxine plus triiodothyronine therapy in hypothyroid patients. J Clin Endocrinol Metab. 2009;94(5):1623–9.
Grozinsky-Glasberg S, Fraser A, Nahshoni E, Weizman A, Leibovici L. Thyroxine-triiodothyronine combination therapy versus thyroxine monotherapy for clinical hypothyroidism: meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2006;91(7):2592–9.
Leger J, Olivieri A, Donaldson M, Torresani T, Krude H, van Vliet G, et al. European Society for Paediatric Endocrinology consensus guidelines on screening, diagnosis, and management of congenital hypothyroidism. Horm Res Paediatr. 2014;81(2):80–103.
Bongers-Schokking JJ, Koot HM, Wiersma D, Verkerk PH, de Muinck Keizer-Schrama SM. Influence of timing and dose of thyroid hormone replacement on development in infants with congenital hypothyroidism. J Pediatr. 2000;136(3):292–7.
Rose SR, Brown RS, Foley T, Kaplowitz PB, Kaye CI, Sundararajan S, et al. Update of newborn screening and therapy for congenital hypothyroidism. Pediatrics. 2006;117(6):2290–303.
Grosse SD, Van Vliet G. Prevention of intellectual disability through screening for congenital hypothyroidism: how much and at what level? Arch Dis Child. 2011;96(4):374–9.
Trumpff C, De Schepper J, Vanderfaeillie J, Vercruysse N, Van Oyen H, Moreno-Reyes R, et al. Neonatal thyroid-stimulating hormone concentration and psychomotor development at preschool age. Arch Dis Child. 2016;101(12):1100–6.
Lain SJ, Bentley JP, Wiley V, Roberts CL, Jack M, Wilcken B, et al. Association between borderline neonatal thyroid-stimulating hormone concentrations and educational and developmental outcomes: a population-based record-linkage study. Lancet Diabetes Endocrinol. 2016;4(9):756–65.
Bakker B, Kempers MJ, De Vijlder JJ, Van Tijn DA, Wiedijk BM, Van Bruggen M, et al. Dynamics of the plasma concentrations of TSH, FT4 and T3 following thyroxine supplementation in congenital hypothyroidism. Clin Endocrinol (Oxf). 2002;57(4):529–37.
Selva KA, Harper A, Downs A, Blasco PA, Lafranchi SH. Neurodevelopmental outcomes in congenital hypothyroidism: comparison of initial T4 dose and time to reach target T4 and TSH. J Pediatr. 2005;147(6):775–80.
Kempers MJ, van der Sluijs Veer L, Nijhuis-van der Sanden MW, Kooistra L, Wiedijk BM, Faber I, et al. Intellectual and motor development of young adults with congenital hypothyroidism diagnosed by neonatal screening. J Clin Endocrinol Metab. 2006;91(2):418–24.
Vaidyanathan P, Pathak M, Kaplowitz PB. In congenital hypothyroidism, an initial L-thyroxine dose of 10-12 mug/kg/day is sufficient and sometimes excessive based on thyroid tests 1 month later. J Pediatr Endocrinol Metab. 2012;25(9–10):849–52.
Bongers-Schokking JJ, Resing WC, de Rijke YB, de Ridder MA, de Muinck Keizer-Schrama SM. Cognitive development in congenital hypothyroidism: is overtreatment a greater threat than undertreatment? J Clin Endocrinol Metab. 2013;98(11):4499–506.
Bongers-Schokking JJ, de Muinck Keizer-Schrama SM. Influence of timing and dose of thyroid hormone replacement on mental, psychomotor, and behavioral development in children with congenital hypothyroidism. J Pediatr. 2005;147(6):768–74.
Simoneau-Roy J, Marti S, Deal C, Huot C, Robaey P, Van Vliet G. Cognition and behavior at school entry in children with congenital hypothyroidism treated early with high-dose levothyroxine. J Pediatr. 2004;144(6):747–52.
Rovet JF. Congenital hypothyroidism: long-term outcome. Thyroid. 1999;9(7):741–8.
Leger J. Congenital hypothyroidism: a clinical update of long-term outcome in young adults. Eur J Endocrinol. 2015;172(2):R67–77.
Lichtenberger-Geslin L, Dos Santos S, Hassani Y, Ecosse E, Van Den Abbeele T, Leger J. Factors associated with hearing impairment in patients with congenital hypothyroidism treated since the neonatal period: a national population-based study. J Clin Endocrinol Metab. 2013;98(9):3644–52.
Rovet JF, Daneman D, Bailey JD. Psychologic and psychoeducational consequences of thyroxine therapy for juvenile acquired hypothyroidism. J Pediatr. 1993;122(4):543–9.
Van Dop C, Conte FA, Koch TK, Clark SJ, Wilson-Davis SL, Grumbach MM. Pseudotumor cerebri associated with initiation of levothyroxine therapy for juvenile hypothyroidism. N Engl J Med. 1983;308(18):1076–80.
Lomenick JP, El-Sayyid M, Smith WJ. Effect of levo-thyroxine treatment on weight and body mass index in children with acquired hypothyroidism. J Pediatr. 2008;152(1):96–100.
Rivkees SA, Bode HH, Crawford JD. Long-term growth in juvenile acquired hypothyroidism: the failure to achieve normal adult stature. N Engl J Med. 1988;318(10):599–602.
Lazarus J, Brown RS, Daumerie C, Hubalewska-Dydejczyk A, Negro R, Vaidya B. 2014 European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur Thyroid J. 2014;3(2):76–94.
Lazar L, Frumkin RB, Battat E, Lebenthal Y, Phillip M, Meyerovitch J. Natural history of thyroid function tests over 5 years in a large pediatric cohort. J Clin Endocrinol Metab. 2009;94(5):1678–82.
Schuschan-Eisen I, Lazar L, Amitai N, Meyerovitch J. Hyperthyrotropinemia in healthy infants during the first year of life. J Pediatr. 2016;170:120–5.
Reuss ML, Paneth N, Pinto-Martin JA, Lorenz JM, Susser M. The relation of transient hypothyroxinemia in preterm infants to neurologic development at two years of age. N Engl J Med. 1996;334(13):821–7.
van Wassenaer AG, Kok JH, de Vijlder JJ, Briet JM, Smit BJ, Tamminga P, et al. Effects of thyroxine supplementation on neurologic development in infants born at less than 30 weeks’ gestation. N Engl J Med. 1997;336(1):21–6.
van Wassenaer AG, Westera J, Houtzager BA, Kok JH. Ten-year follow-up of children born at <30 weeks’ gestational age supplemented with thyroxine in the neonatal period in a randomized, controlled trial. Pediatrics. 2005;116(5):e613–8.
Hollanders JJ, Israels J, van der Pal SM, Verkerk PH, Rotteveel J, Finken MJ, et al. No association between transient hypothyroxinemia of prematurity and neurodevelopmental outcome in young adulthood. J Clin Endocrinol Metab. 2015;100(12):4648–53.
Scratch SE, Hunt RW, Thompson DK, Ahmadzai ZM, Doyle LW, Inder TE, et al. Free thyroxine levels after very preterm birth and neurodevelopmental outcomes at age 7 years. Pediatrics. 2014;133(4):e955–63.
van Wassenaer-Leemhuis A, Ares S, Golombek S, Kok J, Paneth N, Kase J, et al. Thyroid hormone supplementation in preterm infants born before 28 weeks gestational age and neurodevelopmental outcome at age 36 months. Thyroid. 2014;24(7):1162–9.
Thalmann S, Meier CA. Effects of drugs on TSH secretion, thyroid hormones absorption, synthesis, metabolism, and action. In: Braverman LE, Cooper DS, editors. Werner & Ingbar’s the thyroid: a fundamental and clinical text. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2013.
Skelin M, Lucijanic T, Amidzic Klaric D, Resic A, Bakula M, Liberati-Cizmek AM, et al. Factors affecting gastrointestinal absorption of levothyroxine: a review. Clin Ther. 2017;39(2):378–403.
Lafranchi S. Thyroiditis and acquired hypothyroidism. Pediatr Ann. 1992;21(1):29, 32–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that he has no conflict of interest.
Funding
No sources of funding were used to support the writing of this review.
Rights and permissions
About this article
Cite this article
Wassner, A.J. Pediatric Hypothyroidism: Diagnosis and Treatment. Pediatr Drugs 19, 291–301 (2017). https://doi.org/10.1007/s40272-017-0238-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-017-0238-0