Abstract
Oral delamanid (Deltyba®) is a useful addition to the treatment options currently available to treat patients with multidrug-resistant tuberculosis (MDR-TB). In the EU, it is indicated for use as part of an appropriate combination regimen in adults with MDR-TB when an effective treatment regimen cannot otherwise be composed due to resistance or tolerability. It exhibits potent antitubercular activity against drug-susceptible and -resistant strains of Mycobacterium tuberculosis. In a 3-month randomized control trial (2 months treatment + 1 month follow-up) in adults with MDR-TB, delamanid 100 mg twice daily + an optimized background regimen (OBR) improved 2-month sputum culture conversion rates to a significantly greater extent than placebo + OBR. In consecutive extension and follow-up studies, treatment with delamanid for ≥6 to 8 months was associated with higher rates of favourable outcomes and lower rates of unfavourable outcomes than treatment for ≤2 months. Delamanid was generally well tolerated in patients with MDR-TB. To reduce the potential risk of QT interval prolongation with delamanid, recommendations regarding monitoring and precautionary measures should be followed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adis evaluation of delamanid as part of appropriate combination regimen in multidrug-resistant tuberculosis
Improves sputum culture conversion rates when added to optimal background regimens |
Treatment for ≥6 to 8 months provides higher rates of favourable outcomes and lower rates of unfavourable outcomes (including mortality) than treatment for ≤2 months |
Not associated with clinically relevant pharmacokinetic drug interactions |
Generally well tolerated |
Associated with an increased risk of QT interval prolongation (use requires caution in at-risk patient populations) |
What is the rationale for developing delamanid?
Tuberculosis (TB), an infectious disease caused by Mycobacterium tuberculosis that primarily affects the lungs, is a major cause of morbidity and mortality [1, 2]. Currently available treatment regimens, including the standard WHO-recommended first-line regimen of rifampicin, isoniazid, ethambutol and pyrazinamide, are effective against most drug-susceptible strains of TB [2]. However, the improper use of effective TB therapy and other errors have led to the emergence of multidrug-resistant TB (MDR-TB; characterized by resistance to at least rifampicin and isoniazid), as well as the subcategory of extensively drug-resistant TB (XDR-TB; defined as MDR-TB that is also resistant to any fluoroquinolone and ≥1 injectable second-line drug, such as amikacin, capreomycin and kanamycin) [1–6]. In order to achieve the WHO’s goal of ending the global TB epidemic by 2035, there is a clear need for new drugs to be developed that can add to the currently limited treatment options for MDR- and XDR-TB [2, 5, 6].
One such agent is delamanid (Deltyba®), an oral anti-TB drug that is indicated for the treatment of MDR-TB when administered in combination with an optimized background regimen (OBR) in several countries. This article focuses on the use of delamanid in adults with MDR-TB as approved in the EU [7].
How does delamanid work?
Delamanid is a nitroimidazo-oxazole derivative that acts as a mycolic acid biosynthesis inhibitor, thereby disrupting metabolism of the cell wall and facilitating better drug penetration into mycobacteria [7, 8]. It is a prodrug with antibacterial activity specific for Mycobacteria; bioreduction of its nitro group by M. tuberculosis is required to produce a reactive species with antimycobacterial efficacy [8–10]. This activation is mediated via the mycobacterial F420 coenzyme system [8, 9]. Delamanid interferes with mycolic acid production by inhibiting the synthesis of ketomycolic and methoxymycolic acids [8, 10]. In vitro, concentrations of delamanid required to inhibit ketomycolic and methoxymycolic activity by 50 % were 0.021 and 0.036 µg/mL, which were lower than those of isoniazid [10].
Delamanid has been shown to be more active in vitro than currently available first-line anti-TB drugs [10]. The minimum inhibitory concentrations of delamanid against standard drug-susceptible and -resistant strains of M. tuberculosis were 0.006–0.012 µg/mL, and were 2–512 times lower than those of rifampicin, isoniazid, ethambutol and streptomycin [10]. Against clinically isolated M. tuberculosis strains, the minimum concentrations of delamanid required to inhibit 90 % of isolates were 0.006–0.024 µg/mL, and were 8–303 times lower than those of rifampicin, isoniazid, ethambutol and streptomycin [10]. A clinical breakpoint for delamanid has not yet been determined [7].
In vitro, delamanid displayed synergistic or partially synergistic activity with rifampicin, isoniazid, ethambutol or streptomycin against 92.6, 44.4, 88.9 and 25.9 % of all respective tested clinical isolates [10].
What is its potential mechanism of resistance?
Mutation in one of the five coenzyme F420 genes (fgd, Rv3547, fbiA, fbiB and fbiC) has been proposed as the mechanism for resistance against delamanid in mycobacteria [7, 8]. In vitro, the development of resistance to delamanid in clinical isolates of M. tuberculosis was due to lack of conversion of delamanid to the desnitro-imidazo-oxazole form by the bacteria [8].
Resistance to delamanid (defined as any growth in the presence of a delamanid concentration of 0.2 µg/mL that is >1 % of that in drug-free control cultures) occurred in clinical trials [7]. The risk of selecting for resistance to delamanid appears to be higher when the drug is used with few agents predicted to be active and/or when these additional agents are not among those considered to be most effective against M. tuberculosis [7]. Cross-resistance between delamanid and rifampicin, isoniazid, ethambutol or streptomycin has not been observed [7, 10].
For whom is delamanid indicated?
In the EU, delamanid is indicated for use as part of an appropriate combination regimen in adult patients with pulmonary MDR-TB when an effective treatment regimen cannot otherwise be composed due to resistance or tolerability [7]. Table 1 provides a summary of the prescribing information of delamanid in the EU [7].
Delamanid does not induce or inhibit cytochrome P450 (CYP) enzymes [11], and is not associated with clinically relevant drug interactions, including interactions with commonly used antiretroviral and anti-TB drugs [7]. However, as delamanid is associated with prolongation of the corrected QT (QTc interval), its concomitant use with other drugs that prolong the QTc is not recommended or requires caution (Table 1) [7].
What is the clinical efficacy of delamanid?
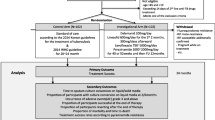
The delamanid development programme includes three consecutive clinical trials in adults (aged 18–64 years) with sputum culture-positive MDR-TB [12, 13]. Patients also received OBR as directly-observed therapy (DOT) according to WHO guidelines for treating MDR-TB. Where possible, the efficacy and the tolerability sections of this article focus on clinical trial data relevant to the approved dosage of delamanid (i.e. 100 mg twice daily).
In the pivotal 3-month, placebo-controlled, multinational phase 2 trial (Trial 204), 481 hospitalized patients were randomized to receive oral delamanid 100 or 200 mg twice daily + OBR or placebo + OBR for 2 months, followed by a 1 month follow-up period [12]. Patients who had a Karnofsky score <50 %, were HIV-positive, or had a significant relevant disease (e.g. cardiovascular disease) were excluded. Lung cavitation was present in ≈70 % of patients (bilateral in ≈25 % of patients). Overall, 91 % of patients had received previous anti-TB therapy ≥30 days prior to randomization, about half of whom had received a first-line regimen only [12].
Trial 208, a non-controlled, open-label extension study, included 213 patients from the delamanid and placebo groups of Trial 204. All patients received delamanid 100 mg twice daily (with the option of increasing the dosage to 200 mg twice daily after 2 weeks) + OBR for a further 6 months [13]. There was a ≥4-week break in delamanid treatment between Trials 204 and 208, with more than half of the patients resuming delamanid within 2 months [13].
An observational follow-up study (Study 116) evaluated long-term outcomes for up to 24 months after randomization in Trial 204 or until the end of treatment (whichever came first) in 421 patients (229 who had participated only in Trial 204 and 192 who had participated in Trials 204 and 208) [8]. Patients continued to receive OBR (but not delamanid) [13]. Based on the length of delamanid exposure, patients were categorized as receiving long-term (≥6 to 8 months) delamanid treatment (n = 192) or short-term (≤2 months) delamanid treatment (n = 229).
In multidrug-resistant tuberculosis
Delamanid 100 mg twice daily + OBR was more effective than placebo + OBR in improving sputum culture conversion (SCC) rates in adults with MDR-TB in Trial 204. In the modified intent-to treat population, the proportion of patients achieving 2-month SCC was significantly (p < 0.01) higher in the delamanid 100 mg twice-daily group than in the placebo group when assessed using an automated mycobacterial growth indicator tube (MGIT) system (45.4 vs. 29.6 %; primary endpoint), as well as when assessed using a solid mycobacteriological culture medium (53.8 vs. 65.2 %) [12]. SCC was defined as a series of ≥5 consecutive cultures that were negative for growth of M. tuberculosis, without subsequent positive cultures.
The time to SCC differed significantly (p = 0.001) between the delamanid 100 mg twice-daily and placebo groups in Trial 204 [12]. According to a Kaplan–Meier analysis of time to SCC using MGIT, there was a 10 % separation between delamanid and placebo by day 36. Based on a Cox regression analysis of SCC, the hazard ratio for increased time to sputum culture negativity in the delamanid 100 mg twice-daily group was 0.58 (95 % CI 0.39–0.89) with the use of MGIT and 0.54 (95 % CI 0.36–0.81) with the use of solid medium [12].
At 24 months in the overall population in Study 116, significantly more patients in the long-term delamanid treatment group had favourable outcomes (i.e. cured or completed all treatment) than in the short-term delamanid treatment group, although there was no significant between-group difference in cure rates (Fig. 1) [13]. Unfavourable outcomes [i.e. died, failed (pre-specified proportion of TB-positive sputum cultures) or defaulted (treatment discontinuation for ≥2 months without medical approval)] and patient mortality were also significantly reduced following long-term treatment with delamanid (Fig. 1) [13].
Treatment outcomes in a 24-month follow-up study of delamanid + an optimized background regimen (OBR) in patients with multidrug-resistant tuberculosis (study 116) [13]. Total favourable = cured + completed; total unfavourable = died + failed + defaulted. Numbers in brackets are 95 % CIs. RR risk ratio, *p < 0.001 vs. short-term group
The use of 2-month SCC as a surrogate efficacy endpoint in the treatment of MDR-TB and the benefits of long-term treatment with delamanid are supported by analyses based on updated prospective data from the delamanid development programme [14]. In 464 (96.5 %) patients for whom vital status was assessed and updated at ≥24 months, the risk of mortality was significantly lower in the 192 patients who achieved 2-month SCC than in the 272 patients who did not achieve this endpoint [mortality rate 3.1 vs. 11.4 %; odds ratio 0.25 (95 % CI 0.10–0.61); p = 0.002]. The risk of mortality was also significantly lower in 205 patients who received long-term delamanid treatment than in 259 patients who received short-term delamanid treatment; at the time of the assessment, 2.9 versus versus 12.0 % of patients in the respectively groups had died [odds ratio 0.22 (95 % CI 0.09–0.54); p = 0.001] [14].
In extensively drug-resistant tuberculosis
Delamanid + OBR appears to be effective in treating adults with complicated infections caused by XDR-TB strains, based on limited evidence from a post-hoc analysis in a small sample of patients with confirmed XDR-TB at baseline in the delamanid development programme [15].
In 26 patients with XDR-TB, the rate of 2-month SCC was numerically higher in 16 patients receiving delamanid + OBR than in 10 patients receiving placebo + OBR (44 vs. 10 %) [15]. Sustained SCC and successful treatment outcomes were at least twice as likely in patients with 2-month SCC than in those without 2-month SCC (p ≤ 0.02) [15]. At 24 months, 17 patients who received long-term delamanid treatment had numerically higher rates of sustained SCC than 9 patients who received short-term delamanid treatment (77 vs. 44 %), as well as numerically higher rates of successful treatment outcomes (65 vs. 44 %) and numerically lower rates of mortality (9 vs. 22 %) [15].
What is the tolerability profile of delamanid?
Treatment with oral delamanid + OBR was generally well tolerated in adults with MDR-TB in the clinical trial programme. The most prominent safety concern associated with delamanid is QTc interval prolongation, with paresthesia and tremor being other important adverse drug reactions [7].
In Trial 204, most treatment-emergent adverse events (TEAEs) were of mild to moderate severity, and led to treatment discontinuation in only a few (3 %) patients [12]. Nausea, vomiting and dizziness were reported in 38.3, 33.0 and 30.2 % of patients in the combined delamanid 100 or 200 mg twice-daily groups, respectively [7]. Adverse events considered to be potentially causally related to study drugs were reported in 38.5 and 35.6 % of delamanid 100 mg twice-daily and placebo recipients, respectively, and included insomnia, vomiting, QTc interval prolongation, somnolence, nausea and hypokalaemia [12].
Serious TEAEs (most commonly QTc interval prolongation, haemoptysis, anaemia and psychotic disorder) were reported in 9.9 and 8.8 % of patients in the delamanid 100 mg twice-daily and placebo groups, respectively, in Trial 204 [12], and in 11.7 % of delamanid recipients in Trial 208 [8]. Overall, 74 patients in Trials 204 and 208 experienced severe TEAEs, the majority of which occurred ≥4 months after starting delamanid [8].
Monitoring and precautionary measures are recommended to reduce the potential risk of electrocardiogram QTc interval prolongation with delamanid (Table 1) [7]. Fridericia’s QTc (QTcF) interval prolongation was significantly (p < 0.05) more frequent with delamanid 100 mg twice-daily than with placebo (9.9 vs. 3.8 % of patients, respectively) in Trial 204, but was not accompanied by clinical symptoms (e.g. arrhythmias or syncope) [12]. QTc interval prolongation increases slowly during the first 6–weeks of delamanid treatment, then stabilizes [7], and appears to be closely correlated with levels of the major delamanid metabolite DM-6705, the bioformation and metabolism of which is regulated by plasma albumin and CYP3A, respectively [7, 16, 17]. The risk of QTc interval prolongation is increased in patients with hypoalbuminaemia and hypokalaemia (Table 1) [7].
Palpitations were reported in 8.1 and 6.3 % of patients in the delamanid 100 mg twice-daily and placebo groups, respectively, in Trial 204 [12] and 13.1 % of delamanid 100 mg twice-daily recipients in Trial 208 [13]. They were the only cardiac adverse event reported in ≥2 % of patients in any treatment group. In general, palpitations were of mild severity, did not display a consistent pattern with regard to time to onset or duration, and occurred in patients who had pre-existing conditions and/or were receiving concomitant medications that had a possible causative role [8].
The nature and frequency of biochemical abnormalities were generally similar in the combined delamanid 100 and 200 mg twice-daily group and the placebo group in Trial 204 [8], with the exception of a numerically higher incidence of hyperuricaemia with delamanid than with placebo (26.1 vs. 22.9 % of patients). Elevated serum cortisol levels (≥26 µg/dL), which were reported in 36.0 and 29.4 % of delamanid 100 mg twice-daily and placebo recipients, respectively, may result from disturbances in the peripheral metabolism of cortisol associated with progressive TB. The most frequently reported potentially drug-related chemistry abnormality was hypokalaemia, which occurred in 2.5 % of delamanid and 1.9 % of placebo recipients [8].
What is the current clinical positioning of delamanid?
Delamanid is a useful addition to the treatment options for patients with MDR-TB. Oral delamanid 100 mg twice daily is effective and generally well tolerated when used in combination with an OBR in adults with MDR-TB, and limited data suggest it is also effective in adults with XDR-TB [15].
In an interim policy guidance based on the current clinical evidence [18], the WHO recommends that delamanid be added to a WHO-recommended regimen in adults with pulmonary MDR-TB (including those with HIV) under specific conditions. It may have a particular role in the treatment of patients with MDR-TB who are at higher risk for poor outcomes, have additional resistant to fluoroquinolones or injectable drugs, or have XDR-TB [18]. As clinical evidence is lacking in some patient populations, the WHO recommends that delamanid should be used with caution in patients who are elderly, have diabetes, hepatic or severe renal impairment, or use alcohol or substances, and advises against its use in children, pregnant/breastfeeding women and individuals with a QTc interval >500 ms; however, its use may be considered in patients with exclusive extrapulmonary disease [18].
Delamanid may have the potential to significantly shorten the usual 2-year duration of treatment for MDR-TB [19, 20]. Rates of 2-month SCC improved when delamanid was added to an OBR relative to OBR treatment without the addition of delamanid. However, long-term treatment provided better outcomes than short-term treatment, and treatment for ≥6 months may be necessary to achieve lasting sputum culture negativity. The optimal duration of treatment with delamanid has not been established (current recommended treatment duration in the EU is 24 weeks; Table 1). The EU marketing authorization for delamanid was conditional upon completion of a confirmatory double-blind, placebo-controlled, 6-month phase 3 trial of delamanid + OBR in adults with pulmonary sputum culture-positive MDR-TB (excluding patients with XDR-TB), which is currently being conducted [21].
In the absence of head-to-head trials, definitive conclusions on the comparative efficacy and tolerability of delamanid versus other anti-TB agents are not possible. According to a network meta-analysis of the comparative efficacy and acceptability of five anti-TB drugs in randomized, controlled trials in patients with MDR-TB, delamanid (OR 2.45; 95 % CI 1.36–4.89), bedaquiline (OR 2.69; 95 % CI 1.02–7.43) and moxifloxacin (OR 2.47; 95 % CI 1.01–7.31) were significantly more effective than placebo, but levofloxacin (OR 2.24; 95 % CI 0.54–9.70) and metronidazole (OR 0.93; 95 % CI 0.11–7.71) were not [22]. However, as there were no statistically significant differences between any of these drugs with regard to efficacy and acceptability, there is insufficient evidence to suggest that the efficacy of any of these drugs is superior to the others [22].
The oral administration of delamanid may provide advantages in terms of patient convenience and adherence to therapy relative to second-line injectable drugs (e.g. amikacin, capreomycin, kanamycin) [19]. In addition, delamanid appears to offer a better tolerability profile, as these injectable agents may cause severe adverse events such as deafness, vestibular toxicity, electrolyte imbalances and renal impairment [19, 23]. Delamanid-based therapy was generally well tolerated in clinical trials; however, its use may be limited by the potential risk of QT interval prolongation. To reduce the potential risk of QT interval prolongation with delamanid, monitoring recommendations and precautionary measures should be followed (Table 1). Of note, prolongation of the QT interval is also associated with other agents used in the treatment of TB (Table 1), including clofazamine and moxifloxacin and the recently approved novel anti-TB agent bedaquiline. Concomitant use of delamanid and bedaquline is not recommended at this time [24].
Patients with HIV infection have an increased risk of developing TB [2], with TB being a leading cause of death in this patient population [19]. Unlike other anti-TB and antiretroviral drugs, many of which are metabolized by CYP enzymes and are associated with drug interactions [3], delamanid does not inhibit or induce CYP450 enzymes [11] and has a low potential for pharmacokinetic drug interactions, including a lack of interactions with antiretrovirals, which may offer an advantage in HIV patients co-infected with TB. A sub-trial of HIV-infected patients co-infected with MDR-TB is being conducted as part of the confirmatory 6-month phase 3 trial at some investigational sites in South Africa [21].
The use of delamanid in the treatment of MDR-TB is currently limited to adults (Table 1) [7]. Clinical trials are being conducted to determine the appropriate dosage, efficacy, safety and pharmacokinetic profile of delamanid in paediatric patients [21], with preliminary data available from an open-label pharmacokinetic and safety phase 1 trial in 13 paediatric patients with MDR-TB [25]. Patients received twice-daily treatment with delamanid 50 mg (6 patients aged 6–11 years) or 100 mg (7 patients aged 12–17 years) + OBR for 10 days, followed by OBR for 8 days. Delamanid was well tolerated, with no patients discontinuing treatment early, experiencing serious adverse events, or having an absolute QTcF >500 ms or an increase from baseline in QTcF >60 ms [25]. In both paediatric age groups, pharmacokinetic parameters were within ranges reported in clinical trials in adults [25].
Treatment of MDR-TB is costly because of the high number of drugs involved and the long duration of treatment required to achieve relapse-free cure [1, 19, 23]. The costs of adding delamanid to OBR may be offset by the increased number of successfully treated patients. According to a modelled cost-utility analysis in patients with MDR-TB in Germany, the addition of delamanid to a five-drug background regimen relative to the background regimen alone was predicted to be cost saving under a wide range of assumptions from a societal perspective, and cost effective from a healthcare payer perspective (incremental cost per quality-adjusted life-years gained €5084; 2013 values) [26].
References
Lange C, Abubakar I, Alffenaar JW, et al. Management of patients with multidrug-resistant/extensively drug-resistant tuberculosis in Europe: a TBNET consensus statement. Eur Respir J. 2014;44(1):23–63.
Global tuberculosis report 2014. Geneva: World Health Organization; 2014.
Zumla AI, Gillespie SH, Hoelscher M, et al. New antituberculosis drugs, regimens, and adjunct therapies: needs, advances, and future prospects. Lancet Infect Dis. 2014;14(4):327–40.
Matteelli A, Roggi A, Carvalho ACC. Extensively drug-resistant tuberculosis: epidemiology and management. Clin Epidemiol. 2014;6(1):111–8.
Sotgiu G, Migliori GB. Facing multi-drug resistant tuberculosis. Pulm Pharmacol Ther. 2015;32:144–8.
Olaru ID, von Groote-Bidlingmaier F, Heychendorf J, et al. Novel drugs against tuberculosis: a clinician’s perspective. Eur Respir J. 2015;45(4):1119–31.
Deltyba (delamanid) 50 mg film-coated tablets: summary of product characteristics. London: European Medicines Agency; 2014.
Deltyba (delamanid): public assessment report. London: European Medicines Agency; 2014.
Hurdle JG, Lee RB, Budha NR, et al. A microbiological assessment of novel nitrofuranylamides as anti-tuberculosis agents. J Antimicrob Chemother. 2008;62(5):1037–45.
Matsumoto M, Hashizume H, Tomishige T, et al. OPC-67683, a nitro-dihydro-imidazooxazole derivative with promising action against tuberculosis in vitro and in mice. PLoS Med. 2006;3(11):e466.
Shimokawa Y, Sasahara K, Yoda N, et al. Delamanid does not inhibit or induce cytochrome p450 enzymes in vitro. Biol Pharm Bull. 2014;37(11):1727–35.
Gler MT, Skripconoka V, Sanchez-Garavito E, et al. Delamanid for multidrug-resistant pulmonary tuberculosis. N Engl J Med. 2012;366(23):2151–60.
Skripconoka V, Danilovits M, Pehme L, et al. Delamanid improves outcomes and reduces mortality in multidrug-resistant tuberculosis. Eur Respir J. 2013;41(6):1393–400.
Wells CD, Gupta R, Hittel N, et al. Long-term mortality assessment of multidrug-resistant tuberculosis patients treated with delamanid. Eur Respir J. 2015;45(5):1498–501.
Gupta R, Geiter LJ, Wells CD, et al. Delamanid for extensively drug-resistant tuberculosis. New Engl J Med. 2015;373(3):291–2.
Shimokawa Y, Sasahara K, Koyama N, et al. Metabolic mechanism of delamanid, a new anti-tuberculosis drug, in human plasma. Drug Metab Dispos. 2015;43(8):1277–83.
Sasahara K, Shimokawa Y, Hirao Y, et al. Pharmacokinetics and metabolism of delamanid, a novel anti-tuberculosis drug, in animals and humans; importance of albumin metabolism in vivo. Drug Metab Dispos. 2015;43(8):1267–76.
The use of delamanid in the treatment of multidrug-resistant tuberculosis: interim policy guidance. Geneva: World Health Organization; 2014.
Brigden G, Nyang’wa B-T, du Cros P, et al. Principles for designing future regimens for multidrug-resistant tuberculosis. Bull World Health Organ. 2014;92(1):68–74.
Diacon AH, Von Groote-Bidlingmaier F, Donald PR. Delamanid, a new 6-nitro-2,3-dihydroimidazo[2,1-b]oxazole for the management of tuberculosis resistant to at least isoniazid and rifampicin. Expert Opin Orphan Drugs. 2014;2(1):87–94.
US National Institutes of Health. ClinicalTrials.gov. 2015. http://www.clinicaltrials.gov/. Accessed 23 Sep 2015.
Wang H, Zhang X, Bai Y, et al. Comparative efficacy and acceptability of five anti-tubercular drugs in tretament of multidrug resistant tuberculosis: a network meta-analysis. J Clin Bioinforma. 2015;5:5.
Lessem E, Cox H, Daniels C, et al. Access to new medications for the treatment of drug-resistant tuberculosis: patient, provider and community perspectives. In J Infect Dis. 2015;32:56–60.
Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. Geneva: World Health Organization; 2014.
Hafkin J, Frias M, Hesseling A, et al. Pharmacokinetics and safety of delamanid in children ages 6–17 years with MDR TP [poster no. A-960]. In: Interscience Conference of Antimicrobial Agents and Chemotherapy (ICAAC)/International Congress of Chemotherapy and Infection (ICC); 2015.
Diel R, Hittlel N, Schaberg T. Cost effectiveness of treating multi-drug resistant tuberculosis by adding Deltyba™ to background regimens in Germany. Respir Med. 2015;109(5):632–41.
Blair HA, Scott LJ. Delamanid: a review of its use in patients with multidrug-resistant tuberculosis. Drugs. 2015;75(1):91–100.
Acknowledgments
The review was updated from Drugs 2015;75(1):91–100 [27], and was reviewed by: N. Cebotarenco, Coalition for Rational and Safe Use of Medicines (CoRSUM), Chişinău, Republic of Moldova; I. D. Olaru, Division of Clinical Infectious Diseases, Research Center Borstel, Borstel, Germany, S. Saluja, Saran Ashram Hospital, Dayalbagh, Agra, India; J-P. Zellweger, Swiss Lung Association, Berne, Switzerland. During the peer review process, the manufacturer of delamanid was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflicts of interest
K A. Lyseng-Williamson, H. A. Blair and L. J. Scott are salaried employees of Adis/Springer, are responsible for the article content and declare no relevant conflicts of interest.
Rights and permissions
About this article
Cite this article
Lyseng-Williamson, K.A., Blair, H.A. & Scott, L.J. Delamanid in multidrug-resistant tuberculosis: a guide to its use in the EU. Drugs Ther Perspect 31, 378–384 (2015). https://doi.org/10.1007/s40267-015-0251-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-015-0251-8