Abstract
Hypertension is a major global health issue and it accounts for a big proportion of disability and mortality worldwide even in adults aged 65 years and above. Moreover, advanced age per se is an independent risk factor for adverse cardiovascular events and there is abundant scientific evidence supporting the beneficial effects of blood pressure lowering, within certain limits, in this subset of hypertensive patients. The aim of this review article is to summarize the available evidence regarding the appropriate management of hypertension in this specific subgroup, in an era of a constantly increasing aging population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
With increasing aging of the population, the prevalence of hypertension increases and is associated with significant morbidity and mortality. |
Current antihypertensive medications mainly reduce peripheral vascular resistance having a small effect on arterial stiffness, which is a crucial etiologic factor of systolic hypertension in older adults. |
The recent guidelines suggest a lower blood pressure target of less than 130/80 mmHg; however, because of the heterogeneity of older adults, this target may not be applicable to all of them. |
Individualization and careful monitoring constitute the cornerstones of the efficient management of hypertension in these individuals. |
1 Introduction
Globally, hypertension constitutes a significant disease burden and a major risk factor for cardiovascular diseases (CVDs) [1]. Global data from 2015 have shown that hypertension is associated with 4.9 million, 2.0 million, and 1.5 million deaths annually due to ischemic heart disease, hemorrhagic stroke, and ischemic stroke, respectively [2]. Data from Europe indicate that the prevalence of hypertension is gradually increasing because of the aging population, being 27% in people aged less than 60 years and 74% in those aged above 80 years [3]. According to current estimations, by 2025, the percentage of patients with hypertension globally will rise by 15–20% reaching approximately the absolute number of 1.5 billion [4]. The results of the Framingham Heart Study revealed that more than 90% of normotensive individuals aged 55 years will finally develop hypertension sometime during their life [3]. In addition, it is estimated that by the age of 60 years, 60% of the total population will develop hypertension and nearly 65% of men and 75% of women will present hypertension by the age of 70 years [3].
Increased blood pressure (BP) levels are related to a higher risk of CVD morbidity and mortality [5]. Hypertension is associated with major cardiovascular complications including stroke, myocardial infarction, and heart failure [3]. However, older hypertensive adults have a seven-fold increased risk of developing chronic kidney disease, dementia, and peripheral artery disease as compared to their younger counterparts [5]. Interestingly, the results of a meta-analysis showed that a systolic BP (SBP) increase of more than 20 mmHg or a 10-mmHg rise in diastolic BP (DBP) in individuals aged between 40 and 69 years may be associated with doubling the risk of CVD development [3]. Recent studies revealed that therapeutic management of hypertension has favorable effects on decreasing the CVD risk, even in hypertensive patients aged above 80 years [6].
Nevertheless, the optimal threshold of antihypertensive therapy initiation still remains controversial as different therapeutic targets are recommended by various scientific bodies [1]. Specifically, the recent guidelines for the treatment of hypertension of the American College of Cardiology/American Heart Association (ACC/AHA) recommend a SBP therapeutic target below 130 mmHg in hypertensive individuals regardless of age [1]. In contrast, the 2018 guidelines of the European Society of Cardiology/European Society of Hypertension propose a SBP therapeutic target below 140 mmHg for hypertensive individuals aged above 65 years and a therapeutic target of 120–129 mmHg for those below 65 years of age [4]. The aim of this review article is to summarize the available evidence regarding the appropriate management of hypertension in adults aged 65 years and above, in an era of a constantly increasing aging population.
2 Literature Search Methods
The PubMed database was searched in order to identify papers using the keywords: “hypertension,” “older patients,” and “elderly”. No lower date limit was applied. Reference lists of papers were searched manually to identify relevant publications. Articles were also identified by use of the related-articles function in PubMed. The last literature search was performed on 15 October, 2022. Only articles written in English were reviewed. The final list of cited references was chosen on the basis of relevance to the topic of the review.
3 Pathophysiologic Mechanisms of Hypertension in Older Age
Hypertension is divided etiologically into two main categories: primary (also known as essential) hypertension that accounts for 85–95% of cases and secondary hypertension caused by certain causes such as renal artery stenosis and various endocrine disorders. Although the vast majority of hypertension in adults aged 65 years and above is essential, an estimated 10% of cases may be secondary and a thorough search for identifiable causes (such as renal artery stenosis mostly of atherosclerotic origin, hyperaldosteronism, and thyroid gland disorders) is necessary especially in cases of apparently resistant hypertension, recent and persistent BP destabilization, and flash pulmonary edema [7].
Several pathophysiologic mechanisms are related to the development of hypertension in older adults such as increased arterial stiffness, neuroendocrine and autonomic nervous system dysfunction, renal disease, and hemodynamic changes (Fig. 1) [3]. Human senescence affects both the function and structure of the vascular system, especially the endothelial function [8]. Several pathophysiologic mechanisms of age-related vascular dysfunction have been proposed including inflammation and oxidative stress [8]. Endothelial dysfunction is characterized by reduced levels of nitric oxide and increased reactive oxygen species and endothelin-1 levels, thus adversely affecting the mechanism of vasodilation [3, 8]. Numerous publications have indicated that the impaired endothelial vascular dilatation of coronary, renal, and forearm arteries and the subsequent formation of atherosclerosis contribute to the development of CVD and cerebrovascular diseases [8].
Furthermore, these age-related structural and functional alterations in the arterial system such as arterial wall hypertrophy, atheromatic plaque formation, and calcification also contribute to the process of arterial stiffening and thus to certain hypertension-related complications [3, 9]. Nevertheless, although arterial stiffness is a major determinant of the pathophysiologic mechanisms of hypertension in older adults, the process is different from that of atheromatic plaque formation [10]. By the age of 50–60 years, human senescence is accompanied by an increase in both SBP and DBP [9]. However, above the sixth decade of life, SBP continues to rise as opposed to DBP, which either remains constant or declines. Thus, arterial stiffness is a major determinant of increased SBP and pulse pressure, as well as decreased DBP [9]. Interestingly, a study showed that the NT‐proBNP levels could be used as a marker of arterial stiffness in adults aged 65 years and above without CVD manifestations. A positive association was found between the NT‐proBNP level and SBP [3, 11].
Aging is associated with a gradual impairment of the regulation of BP owing to various reasons, namely reduced baroreflex sensitivity, plasma volume depletion, and defected vasomotor tone [12]. These can be driven by the presence of comorbidities including diabetes mellitus and Parkinson’s disease as well as the use of medications such as antihypertensive and diuretic drugs. However, the reduced baroreflex sensitivity has major consequences such as orthostatic hypotension and supine hypertension. Remarkably, orthostatic hypotension is frequently encountered in older adults and has been related to an increased risk of falls and mortality. Thus, it is of imperative importance to properly inform the older patients on the recognition of baroreflex insensitivity-related symptoms giving also practical advice regarding their appropriate management [12].
Notably, there are important age-related changes in renal function including an increase in salt sensitivity due to an impaired function of calcium adenosine triphosphate and sodium-potassium channel pumps. This altered function of ion channels leads to vasoconstriction and increased vascular resistance [3]. Aging has also been linked to a decreased function of the renin angiotensin aldosterone system, especially above the age of 60 years and an accompanying 40–60% reduction in the renin levels may occur in adults aged 65 years and above compared with younger individuals [3]. Additionally, a hypersecretion of angiotensin II enzyme, which is responsible for inducing inflammation and the production of reactive oxygen species, is also linked to arterial hemodynamic changes and further renal dysfunction [13]. Last but not least, a reduced serum aldosterone level has been observed in older adults, thus increasing their susceptibility to drug-related hyperkalemia [3, 13].
4 Complications of Uncontrolled Hypertension
Hypertension has been related to several adverse cardiovascular outcomes, namely ischemic and hemorrhagic strokes, retinal disease, cognitive decline and dementia, atrial fibrillation, and renal disease [3, 14,15,16]. One of the main and well-described complications of poorly controlled hypertension is coronary heart disease [17]. In fact, a large-scale observational study revealed that coronary heart disease risk was largely influenced by aging, whilst pulse pressure and SBP are strong predictors of coronary heart disease risk in patients older than 60 years of age [18]. Moreover, hypertension is the most common cause of heart failure. The pathogenesis is largely due to two distinct pathways: either by causing left ventricular hypertrophy and diastolic dysfunction or by accelerating the process of atherosclerosis and sequential myocardial infarction [19]. Another commonly reported complication of uncontrolled hypertension is peripheral artery disease. The pathogenesis of peripheral artery disease is based on the formation of atheromatic plaques as a result of the constantly imposed shear stress on the vascular walls of peripheral vessels (e.g., carotids), which might lead to subsequent arterial stenosis or plaque migration and obstruction and thus an ischemic stroke may ensue. Apart from ischemia, the incidence of parenchymal intracranial hemorrhage was reported to be doubled in patients with hypertension, in part owing to the mechanism of a hypertensive crisis [20]. Additionally, the occurrence of further neurological manifestations has also been reported, namely subarachnoid hemorrhage, hypertensive encephalopathy, and subdural hematoma [21].
Furthermore, hypertension has been strongly associated with chronic renal disease, in the sense that most patients with chronic renal disease were proven to be hypertensive and undertreated [22]. Another complication of uncontrolled hypertension is hypertensive retinopathy, owing to retinal microvascular changes, such as focal retinal arteriolar narrowing, arteriovenous nicking, retinal hemorrhages, and microaneurysms [23].
5 Treatment of Hypertension
The American and European hypertension guidelines present significant differences related to the definitions and therapeutic targets in older adults [24]. The main explanation for this difference is that the European population is much more homogeneous mainly regarding ethnic characteristics compared with the American population. However, both emphasize the significance of hypertension management in older adults aiming thus to reduce their associated CVD risk [24].
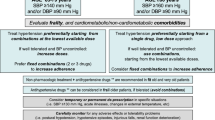
The recent 2018 European Society of Cardiology/European Society of Hypertension BP guidelines have divided older adults into two categories: (a) individuals aged between 65 and 79 years referred to as “elderly” and (b) individuals aged ≥80 years characterized as “very old” [24]. Based on these guidelines, antihypertensive treatment should be instituted when SBP is ≥ 140 mmHg and DBP is ≥ 90 mmHg in older hypertensive adults [24]. Moreover, antihypertensive therapy should be offered in fit patients aged above 80 years with SBP ≥ 160 mmHg and/or DBP ≥ 90 mmHg. Both in elderly and in very old hypertensive individuals, the therapeutic goal is set at SBP 130–139 mmHg and DBP 70–79 mmHg only on the condition that these BP values are well tolerated [24]. Most importantly, European guidelines recommend that a clinical decision pertaining to the initiation of antihypertensive therapy should take into consideration the frailty status, as well as the presence of any underlying comorbidities and polypharmacy in older adults [6].
On the contrary, the novel ACC/AHA hypertension guidelines recommend the following categorization of BP: (a) normal, defined as SBP < 120 mmHg and DBP < 80 mmHg, (b) elevated, with SBP between 120 and 129 mmHg and DBP between 80 and 89 mmHg, (c) stage 1 hypertension, defined as SBP between 130 and 139 mmHg or DBP between 80 and 89 mmHg, and (d) stage 2 hypertension, with SBP ≥140 mmHg or DBP ≥ 90 mmHg [25].
5.1 Ambulatory BP Measurement
All the aforementioned treatment goals are based on office BP measurements. However, there are numerous studies promoting the out-of-office BP measurement as a strategy to improve the diagnostic accuracy and the appropriate management of hypertension. White coat hypertension and white coat phenomenon, as well as the difficulty of accessibility amongst a number of older patients are only some of the factors underpinning the importance of ambulatory BP measurement as a beneficial alternative. However, further investigation is needed to illustrate the potential benefits of routine ambulatory BP measurement in older patients [26,27,28].
5.2 Non-pharmacological Treatment
Several non-pharmacological interventions proved to have a favorable effect on BP reduction [29]. The ACC/AHA guidelines highlight the importance of lifestyle modifications including diet and reduced salt intake, increased exercise uptake and reduced body weight, stress reduction, tobacco cessation, and moderate alcohol consumption [29]. Additional non-pharmacological approaches include high potassium, magnesium, and calcium supplementation and also high protein and fiber, as well as tea and dark chocolate consumption [3, 30]. Behavioral therapies such as yoga, Thai chi, transcendental meditation, as well as acupuncture can lower BP [3, 31]. A proposed physiologic mechanism by which these interventions reduce BP is the downregulation of the sympathetic nervous system [31].
A diet rich in vegetables, whole grains, fruits, low-fat dairy products, virgin olive oil, and fish is recommended for lowering BP in hypertensive individuals [31]. Furthermore, reduced intake of sugar, red meat, and saturated and total fat is also recommended [30, 31]. Various heart-healthy dietary patterns such as a vegetarian and plant-based diet, a Dietary Approaches to Stop Hypertension (DASH) diet, a low-carbohydrate diet, and a Mediterranean diet have been proposed for the management of hypertension [3, 31]. The DASH diet was found to reduce SBP by 5.5 mmHg and DBP by 3 mmHg [31]. The SUN (Seguimiento Universidad de Nevarra) Study showed that following a Mediterranean dietary pattern at a moderate level can lower SBP by 2.4 mmHg and DBP by 1.3 mmHg while a stricter adherence can reduce SBP by 3.1 mmHg and DBP by 1.9 mmHg [31]. The typical Mediterranean diet mainly consists of fresh fruits and vegetables, nuts, fatty fish, virgin olive oil, whole grains, and red wine. However, moderate consumption of dairy foods is advised, whereas processed food and red meat consumption should be limited [32]. Remarkably, high-risk individuals for the development of CVD who followed the Mediterranean diet showed a 7.1-mmHg decrease in terms of SBP [31].
Studies have also reported that a reduced sodium consumption may be linked to BP lowering [31]. The suggested amount of sodium intake in adults is less than 2.400 mg/day, which is equal to approximately 1 teaspoon of table salt [31]. This is associated with a reduction of SBP/DBP by 2/1 mmHg respectively [31]. However, the optimal target of daily sodium consumption is less than 1.500 mg/day and can cause a SBP/DBP decrease by 7/3 mmHg, respectively [30, 31]. It has been found that sodium intake less than 1200 mg is effective and safe for the cardiovascular system [33]. Moreover, increased intake of dietary potassium can reduce SBP and DBP in both normotensive and hypertensive individuals by 4.7 mmHg and 3.5 mmHg, respectively [31]. This favorable effect of dietary potassium though, is more effective in hypertensive patients with a reduction of SBP by 6.8 mmHg and DBP by 4.6 mmHg [30, 31]. Additionally, the administration of magnesium supplements has been related to a reduction in both SBP and DBP by 2.0 mmHg and 1.8 mmHg, accordingly. However, further studies are needed to specify their role in antihypertensive interventions [31]. The Trial of Nonpharmacologic Interventions in the Elderly (TONE) showed that both weight loss and low sodium consumption constitute efficient methods of BP regulation [33]. Moreover, the American obesity guidelines report a strong association between increased weight, obesity, and hypertension. Furthermore, a dose–response effect of weight loss on BP reduction is reported [34].
Regarding alcohol consumption, a positive correlation between moderate intake and diminished BP levels was found [31]. Interestingly, individuals who presented with a significantly increased BP above the optimal target had the most favorable impact on BP levels [31]. Heavy drinkers have shown a SBP decrease by 5 mmHg and DBP by 3 mmHg following a month of consultation or replacement with low alcoholic products [31]. Thus, limiting alcohol consumption to ≤1 drink daily for women and ≤ 2 drinks for men is suggested [30].
Based on the updated Physical Activity Guidelines of 2018, and the 2019 ACC/AHA Guidelines on the primary prevention of CVD, increased physical activity including both aerobic and muscle-strengthening exercise (resistance) is highly indicated for every American individual [35]. Specifically, according to the recommendations of 2017 Hypertension Clinical Practice Guidelines, individuals should engage in 90–150 minutes of moderate-to-vigorous intensity of aerobic training every week and 90–150 minutes of muscle-strengthening exercise ≥ 2 times per week. The 2018 Physical Activity Guidelines Advisory Committees highlighted that exercise can significantly affect BP levels. Most importantly, aerobic exercise has been demonstrated to reduce SBP by 4 mmHg and DBP by 3 mmHg on average, whereas resistance exercise can lower SBP by 2 mmHg and DBP by 3 mmHg [35]. A meta-analysis reported that physically active individuals have a 21% lower risk of developing CVD and a 36% lower risk of CVD mortality compared with their physically inactive counterparts [36].
5.3 Pharmacological Treatment
Before the initiation of antihypertensive treatment in adults aged 65 years and above with uncontrolled hypertension, several factors must be taken into serious consideration, namely the functional status of the patient, adherence to the medication(s), kidney function, and electrolyte levels [3]. Several trials have investigated the various effects of the main antihypertensive drug classes including angiotensin-converting enzyme inhibitors, diuretics, angiotensin II receptor blockers, calcium channel blockers (CCB), and beta blockers in older hypertensive adults [37]. Administration of all the above-mentioned antihypertensive drugs proved to be associated with favorable CVD outcomes in this particular subset of hypertensive subjects [3]. Relevant meta-analyses revealed that a decrease of 10 mmHg in SBP or 5 mmHg in DBP reduces the relative risk of heart failure by 40%, stroke by 35%, all major CVD events by 20%, and overall mortality by 10–15% [4]. Remarkably, these relative risk reductions were independent of the CVD risk, underlying comorbidities, age, sex, the baseline BP value, being within the hypertensive range [4]. Current meta-analyses showed that these classes of drugs were related to different favorable outcomes (e.g., beta-blockers were mainly associated with a reduced stroke incidence) but the overall CVD outcomes and mortality were equivalent among these therapeutic agents [4].
Although all major drug classes are effective, older adults with isolated systolic hypertension may preferentially be managed with a CCB or diuretic [4]. Additionally, the Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) showed that daily administration of chlorthalidone in low doses was more efficacious than amlodipine (CCB) or lisinopril (angiotensin-converting enzyme inhibitors) with regard to the prevention of major CVD events as well as the increase in survival rates [38].
According to the 2018 European Society of Cardiology/European Society of Hypertension guidelines, most hypertensive individuals should be initially managed with dual therapy consisting of a renin-angiotensin-system blocker with a CCB or a diuretic [4]. Interestingly, certain compelling indications exist when it comes to combine a beta-blocker with any other antihypertensive drug category. These indications include heart failure, angina, heart rate control, and post-myocardial infarction cases [4]. The Losartan Intervention for Endpoint reduction in hypertension study (LIFE) showed that hypertensive patients treated with an angiotensin II receptor blocker and a diuretic combination had fewer CVD outcomes as compared with those who received a beta-blocker and a diuretic combination [39]. Similarly, the Anglo-Scandinavian Cardiac Outcomes Trial-BP Lowering Arm (ASCOT-BPLA) found that the combination of a CCB and an angiotensin-converting enzyme inhibitor was associated with a more pronounced decrease in CVD outcomes compared with the beta-blocker–diuretic combination [40]. Remarkably, based on observational studies, the beta-blocker–diuretic combination displays diabetogenic effects, leading thus to the development of new-onset diabetes especially in susceptible patients [41].
However, according to the same guidelines, the use of monotherapy is recommended for frail and older hypertensive adults, those with SBP < 150 mmHg and very high-risk individuals having high-normal BP levels [4]. In cases of uncontrolled hypertension after the initial trial with a dual therapy, the next therapeutic step is a triple-combination therapy consisting of a renin-angiotensin-system blocker, a CCB, and a diuretic [4]. Last but not least, in truly resistant hypertension, spironolactone or another diuretic is added to the triple-combination therapy [4].
5.3.1 Benefits of Drug-Based BP Lowering in the Older Adults
A plethora of randomized placebo-controlled clinical trials have confirmed the beneficial effects of drug treatment-based BP lowering in adults aged 65 years and above with or without established CVD (Table 1). The Systolic Hypertension in the Elderly Program (SHEP), where participants had isolated systolic hypertension, showed dramatic decreases in the prevalence of stroke (both ischemic and hemorrhagic), as well as in heart failure and in all-cause mortality linked to the administration of antihypertensive therapy during a 4.5-year follow-up period [42]. Moreover, both the Systolic Hypertension in Europe (Syst-Eur) [43] and China (Syst-China) [44] trials have also brought into light the life-saving effects of antihypertensive therapy in older adults with isolated systolic hypertension. The HYVET (Hypertension in the Very Elderly trial) was a game changer in terms of drug-based antihypertensive treatment in patients aged 80 years or older and it crucially affected hypertension management guidelines coming from various national and international scientific organizations [45]. Study participants were randomized to either placebo or indapamide ± perindopril with a target systolic BP below 160 mmHg. Over a median 1.8-year follow-up period, older adults randomized to the active drug regimen exhibited a 39% reduction in fatal stroke, a 64% reduction in heart failure, as well as a 21% decrease in all-cause mortality, and a 23% in cardiovascular mortality, as compared to their placebo randomized counterparts.
The SPRINT (Systolic BP Intervention Trial) trial, a randomized controlled study that questioned current BP goals emphasizing the potential benefits of intensive (SBP < 120 mmHg) versus standard (SBP <140 mmHg) BP lowering shed more light on the concept of antihypertensive therapy in older adults [46]. Among the total of 9361 study participants (SBP of 130–180 mmHg at a high cardiovascular risk), 2636 (almost 28%) were aged 75 years or older and they were randomized to either placebo or active treatment (based on azilsartan mainly). In this particular trial, intensive SBP lowering (< 120 mmHg), compared with standard lowering (< 140 mmHg) was associated with a statistically significant 34% decrease in the primary endpoint (consisting of myocardial infarction and other acute coronary syndrome, stroke, heart failure, and cardiovascular death), as well as with a 33% reduction regarding all-cause mortality and a 38% decrease in the heart failure.
Furthermore, intensive SBP lowering was linked to only a numerically augmented risk of electrolyte disorders, syncope, orthostatic hypotension (which was not associated with injurious falls), as well as acute kidney injury. Of particular note is the fact that the beneficial effects of intensive SBP lowering in the subgroup of SPRINT participants aged 75 years or older remained unaffected by the frailty status [47]. However, we need to emphasize that the results of the SPRINT study, which did not include diabetic patients, were driven mainly by the reduction in heart failure, while the intensive and standard arms of treatment did not differ in myocardial infarction and stroke outcomes. In addition, in this study, BP measurement was performed by an electronic device with the patient unattended in contrast to the common attended method, a fact that could have had a significant impact on the study results. Nevertheless, the SPRINT has shown a decline in the occurrence of dementia and of chronic kidney disease in those patients with normal kidney function at baseline.
In support of the findings of this landmark trial, a recent systematic review with a meta-analysis and meta-regression, which included 16 studies totaling almost 66,000 hypertensive participants (average age 69.4 years) with a follow-up period that ranged from 1.8 to 4.9 years, showed that intensive BP treatment was associated with a significant reduction in major adverse cardiovascular events by 26%, a 13% reduction in myocardial infarction, a 28% decrease in stroke, a 47% reduction in heart failure, and 24% and 17% decreases in cardiovascular and all-cause mortality, respectively [48]. At this point, we need to clarify though that these results may not be applicable to the frailest older adults, namely those who are institutionalized or absolutely dependent on caregivers, as in general these subjects are excluded from clinical trials.
5.3.2 Which Drug to Choose?
It seems that there is no ideal drug therapy regarding the management of hypertension in older adults, in the sense that all major drug classes have been shown to be safe and effective in these individuals. Compelling indications, such as the presence of diabetes, coronary artery disease, and heart failure should lead the therapeutic decisions on which drug to prefer, always exercising extreme caution in potential drug–drug interactions, and also having in mind the specific issues pertaining to drug absorption and metabolism related to the aging process (Table 2) [49].
According to a position statement paper released by the ESH, CCB and diuretics may constitute rational first choices concerning the pharmaceutical approach in older adults with hypertension [4]. Moreover, contrary to the current trend of initiating single-pill fixed-dose combination therapy from the beginning, it seems prudent to start with monotherapy in older adults, carefully uptitrating the dosage or adding a second agent according to the patients’ response.
Polypharmacy is a specific issue in older adults as it is not only associated with decreased compliance to proposed therapy, but it also increases the risk of adverse events [9]. Poor compliance because of polypharmacy together with pseudo-resistant hypertension as a result of problematic BP measurement due to increased arterial stiffness and age-associated arterial calcification are major factors contributing to resistant hypertension in older adults. Particular attention should be paid among others to patients receiving anti-Parkinsonian drugs, as well as alpha-blockers for the treatment of prostatic hyperplasia, as it is well known that their use is linked to an increased risk of orthostatic hypotension [9]. Last but not least, as aging per se is associated with a decline in renal function, the choice of a specific diuretic drug should take into serious consideration the estimated glomerular filtration rate and the need for more frequent laboratory checks regarding the estimated glomerular filtration rate and electrolytes may be larger in this subset of hypertensive individuals [50].
Type 2 diabetes affects millions of people and it is commonly associated with hypertension. Currently, there is evidence that sodium-glucose cotransporter 2 inhibitors may have a favorable effect on BP control amongst patients with diabetes and heart failure. It has been reported that this effect is not just a short-term result but rather a long-term impact on both DBP and SBP levels [51, 52].
Interestingly, in a multicenter, phase II, open-label study including 256 overweight patients, it was reported that a first-in-class brain aminopeptidase A inhibitor, firibastat, was effective in decreasing BP [53, 54]. Most importantly, the effects of firibastat in patients with resistant hypertension show great promise. Indeed, this novel agent might be very effective in particular in older patients with uncontrolled hypertension and this is currently under investigation in a phase III clinical trial called Firibastat in Treatment-resistant Hypertension (FRESH) [55]. Of particular notice is the fact that up until now there is no evidence regarding potential drug–drug interactions in patients receiving firibastat, thus having significant implications regarding the treatment of older adults with hypertension who usually face polypharmacy as a consequence of their comorbidities [55].
5.3.3 Non-Steroidal Anti-Inflammatory Drugs, Acetaminophen, and Hypertension
There is a great discussion in the literature as to whether non-steroidal anti-inflammatory drugs (NSAIDs) elevate BP especially in older subjects and possibly affect the antihypertensive treatment effectiveness. In a recently published study, NSAID usage was found to be a potential independent risk factor for uncontrolled hypertension [56]. More specifically, both cyclooxygenase-1 inhibitors and cyclooxygenase-2 inhibitors may adversely affect BP levels. Indeed, there is evidence that NSAIDs increase BP by negatively impacting on prostaglandin production, which might have adverse renal effects. Non-steroidal anti-inflammatory drugs may also enhance the systemic vascular resistance through endothelin-1 synthesis and by altering arachidonic metabolism [57]. Apart from NSAIDs, acetaminophen is also a common first-line treatment for chronic pain. Although it is reported that in contrast to NSAIDs, acetaminophen has only a minimal effect on BP, the latest evidence showed that a regular intake of 4 g of acetaminophen per day increases SBP compared with placebo [58, 59].
5.3.4 Timing of Anti-Hypertensive Medications
Another point of investigation through recent years has been whether bedtime versus the commonly used upon-waking hypertension treatment administration has a more prominent effect on CVD risk reduction. There are clinical studies reporting that timing differences regarding the administration of several classes of anti-hypertensive medications could actually play a role in their effectiveness. The results from the Hygia Chronotherapy Trial, conducted within the clinical primary care setting, also suggested that bedtime administration significantly resulted in a more effective decrease in asleep BP, while it enhanced the sleep-time relative BP decline. Most interestingly, bedtime administration showed a decreased occurrence of major CVD events compared with conventional upon-waking administration [60]. In a recent study, it has been shown that bedtime administration with ≥ 1 BP-lowering treatment, compared with conventional upon-waking administration, more effectively improved the control of BP as well as significantly reduced the CVD mortality [61]. In line with these results, in a meta-analysis of randomized controlled trials investigating the impact of bedtime dosing of antihypertensive agents compared to morning therapy, it has been shown that bedtime administration of antihypertensive medication is correlated to a decrease of cardiovascular and cerebrovascular events when compared with the more commonly used morning administration [62].
However, in a very recently published prospective, randomized, open-label, blinded-endpoint clinical trial evaluating cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensive medications in the UK (TIME study), it was reported that evening dosing of a usual antihypertensive medication was not different from morning dosing in terms of major cardiovascular outcomes. Based on these results, the authors conclude that “patients can be advised that they can take their regular antihypertensive medications at a convenient time that minimizes any undesirable effects” [63].
6 Conclusions
Hypertension is a real epidemic in the current era, which is characterized by a constantly and rapidly aging population, further perplexing the whole issue of the associated cardiovascular morbidity and mortality. However, there is sound scientific evidence supporting the need for the institution of early and effective antihypertensive treatment in the specific subgroup of older adults with hypertension with the ultimate goal to combat CVD, leading thus to the optimal prognosis of these particular individuals.
References
Baffour-Awuah B, Dieberg G, Pearson MJ, Smart NA. Blood pressure control in older adults with hypertension: a systematic review with meta-analysis and meta-regression. Int J Cardiol Hypertens. 2020;6: 100040.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA. 2017;317:165–82.
Oliveros E, Patel H, Kyung S, Fugar S, Goldberg A, Madan N, et al. Hypertension in older adults: assessment, management, and challenges. Clin Cardiol. 2020;43:99–107.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Burnier M, Polychronopoulou E, Wuerzner G. Hypertension and drug adherence in the elderly. Front Cardiovasc Med. 2020;7:49.
Zieleniewicz P, Zdrojewski T. Current guidelines and controversies in the diagnosis and therapy of hypertension in the elderly and very elderly: a review of international recommendations. Arterial Hypertension. 2020;24:1–9.
Harrison DG, Coffman TM, Wilcox CS. Pathophysiology of hypertension: the mosaic theory and beyond. Circ Res. 2021;128:847–63.
Higashi Y, Kihara Y, Noma K. Endothelial dysfunction and hypertension in aging. Hypertens Res. 2012;35:1039–47.
Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res. 2019;124:1045–60.
Durham AL, Speer MY, Scatena M, Giachelli CM, Shanahan CM. Role of smooth muscle cells in vascular calcification: implications in atherosclerosis and arterial stiffness. Cardiovasc Res. 2018;114:590–600.
Sasaki N, Yamamoto H, Ozono R, Fujiwara S, Kihara Y. Association of N-terminal pro B-type natriuretic peptide with blood pressure and pulse pressure in elderly people: a cross-sectional population study. Circ J. 2018;82:2049–54.
Low PA, Tomalia VA. Orthostatic hypotension: mechanisms, causes, management. J Clin Neurol. 2015;11:220–6.
Musso CG, Jauregui JR. Renin-angiotensin-aldosterone system and the aging kidney. Expert Rev Endocrinol Metab. 2014;9:543–6.
Sierra C. Hypertension and the risk of dementia. Front Cardiovasc Med. 2020;7:5.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383:1899–911.
Wilson PW. Established risk factors and coronary artery disease: the Framingham Study. Am J Hypertens. 1994;7:7S-12S.
Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–9.
Papademetriou V. From hypertension to heart failure. J Clin Hypertens (Greenwich). 2004;6:14–7.
Thrift AG, McNeil JJ, Forbes A, Donnan GA. Risk factors for cerebral hemorrhage in the era of well-controlled hypertension. Melbourne Risk Factor Study (MERFS) Group. Stroke. 1996;27:2020–5.
Haddadin F, Munoz Estrella A, Herzog E. Hypertensive emergency presenting with acute spontaneous subdural hematoma. J Cardiol Cases. 2019;19:25–8.
Coresh J, Wei GL, McQuillan G, Brancati FL, Levey AS, Jones C, et al. Prevalence of high blood pressure and elevated serum creatinine level in the United States: findings from the third National Health and Nutrition Examination Survey (1988–1994). Arch Intern Med. 2001;161:1207–16.
Bhargava M, Ikram MK, Wong TY. How does hypertension affect your eyes? J Hum Hypertens. 2012;26:71–83.
American College of Cardiology. Older adults and hypertension: beyond the 2017 guideline for prevention, detection, evaluation, and management of high blood pressure in adults. https://www.acc.org/latest-in-cardiology/articles/2020/02/26/06/24/http%3a%2f%2fwww.acc.org%2flatest-in-cardiology%2farticles%2f2020%2f02%2f26%2f06%2f24%2folder-adults-and-hypertension. Accessed 14 Jan 2023.
Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30:160–4.
Mediavilla García JD, Jaén Águila F, Fernández Torres C, Gil Extremera B, Jiménez AJ. Ambulatory blood pressure monitoring in the elderly. Int J Hypertens. 2012;2012: 548286.
Parati GMG. The role of ambulatory blood pressure monitoring in elderly hypertensive patients. Blood Press. 2000;9:12–6.
Camafort M, Chung W-J, Shin J-H. Role of ambulatory blood pressure monitoring in elderly hypertensive patients. Clin Hypertens. 2022;28:22.
Oza R, Garcellano M. Nonpharmacologic management of hypertension: what works? Am Fam Physician. 2015;91:772–6.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:1269–324.
Verma N, Rastogi S, Chia Y-C, Siddique S, Turana Y, Cheng H-M, et al. Non-pharmacological management of hypertension. J Clin Hypertens (Greenwich). 2021;23:1275–83.
De Pergola G, D’Alessandro A. Influence of Mediterranean diet on blood pressure. Nutrients. 2018;10:1700.
Shea MK, Nicklas BJ, Houston DK, Miller ME, Davis CC, Kitzman DW, et al. The effect of intentional weight loss on all-cause mortality in older adults: results of a randomized controlled weight-loss trial. Am J Clin Nutr. 2011;94:839–46.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985–3023.
Barone Gibbs B, Hivert M-F, Jerome GJ, Kraus WE, Rosenkranz SK, Schorr EN, et al. Physical activity as a critical component of first-line treatment for elevated blood pressure or cholesterol: who, what, and how? A scientific statement from the American Heart Association. Hypertension. 2021;78:e26-37.
Wahid A, Manek N, Nichols M, Kelly P, Foster C, Webster P, et al. Quantifying the association between physical activity and cardiovascular disease and diabetes: a systematic review and meta-analysis. J Am Heart Assoc. 2016;5: e002495.
Dickerson LM, Gibson MV. Management of hypertension in older persons. Am Fam Physician. 2005;71:469–76.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–97.
Dahlöf B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:995–1003.
Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366:895–906.
Mancia G, Grassi G, Zanchetti A. New-onset diabetes and antihypertensive drugs. J Hypertens. 2006;24:3–10.
Hansson L. Future goals for the treatment of hypertension in the elderly with reference to STOP-Hypertension, SHEP, and the MRC trial in older adults. Am J Hypertens. 1993;6:40S-43S.
Fagard RH, Staessen JA. Treatment of isolated systolic hypertension in the elderly: the Syst-Eur trial. Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Clin Exp Hypertens. 1999;21:491–7.
Wang JG, Staessen JA, Gong L, Liu L. Chinese trial on isolated systolic hypertension in the elderly. Systolic Hypertension in China (Syst-China) Collaborative Group. Arch Intern Med. 2000;160:211–20.
Bulpitt CJ, Fletcher AE, Amery A, Coope J, Evans JG, Lightowlers S, et al. The hypertension in the very elderly trial (HYVET). J Hum Hypertens. 1994;8:631–2.
Cushman WC, Whelton PK, Fine LJ, Wright JT, Reboussin DM, Johnson KC, et al. SPRINT trial results: latest news in hypertension management. Hypertension. 2016;67:263–5.
Jovanovich A, Ginsberg C, You Z, Katz R, Ambrosius WT, Berlowitz D, et al. FGF23, frailty, and falls in SPRINT. J Am Geriatr Soc. 2021;69:467–73.
Takami Y, Yamamoto K, Arima H, Sakima A. Target blood pressure level for the treatment of elderly hypertensive patients: a systematic review and meta-analysis of randomized trials. Hypertens Res. 2019;42:660–8.
Musini VM, Tejani AM, Bassett K, Puil L, Wright JM. Pharmacotherapy for hypertension in adults 60 years or older. Cochrane Database Syst Rev. 2019;6: CD000028.
Lee J-H, Kim K-I, Cho M-C. Current status and therapeutic considerations of hypertension in the elderly. Korean J Intern Med. 2019;34:687–95.
Cheng L, Fu Q, Zhou L, Fan Y, Liu F, Fan Y, et al. Effect of SGLT-2 inhibitor, empagliflozin, on blood pressure reduction in Chinese elderly hypertension patients with type 2 diabetes and its possible mechanisms. Sci Rep. 2022;12:3525.
Gupta R, Maitz T, Egeler D, Mehta A, Nyaeme M, Hajra A, et al. SGLT2 inhibitors in hypertension: role beyond diabetes and heart failure. Trends Cardiovasc Med. 2022. https://doi.org/10.1016/j.tcm.2022.05.005.
Aronow WS. Managing hypertension in the elderly: what’s new? Am J Prev Cardiol. 2020;1: 100001.
Ferdinand KC, Balavoine F, Besse B, Black HR, Desbrandes S, Dittrich HC, et al. Efficacy and safety of firibastat, a first-in-class brain aminopeptidase A inhibitor, in hypertensive overweight patients of multiple ethnic origins. Circulation. 2019;140:138–46.
Gupta R, Alcantara R, Popli T, Tariq U, Sood A, Mahajan S, et al. Firibastat: a novel brain aminopeptidase inhibitor: a new era of antihypertensive therapy. Curr Probl Cardiol. 2022;47: 100859.
Johnson AG, Simons LA, Simons J, Friedlander Y, McCallum J. Non-steroidal anti-inflammatory drugs and hypertension in the elderly: a community-based cross-sectional study. Br J Clin Pharmacol. 1993;35:455–9.
Aronow WS. Drug-induced causes of secondary hypertension. Ann Transl Med. 2017;5:349.
Gupta R, Behnoush AH, Egeler D, Aronow WS. Effect of acetaminophen on blood pressure: a systematic review and meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2022;29:e326–30.
MacIntyre IM, Turtle EJ, Farrah TE, Graham C, Dear JW, Webb DJ, et al. Regular acetaminophen use and blood pressure in people with hypertension: the PATH-BP Trial. Circulation. 2022;145:416–23.
Hermida RC, Crespo JJ, Domínguez-Sardiña M, Otero A, Moyá A, Ríos MT, et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2020;41:4565–76.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010;27:1629–51.
Gupta R, Malik AH, Popli T, Ranchal P, Yandrapalli S, Aronow WS. Impact of bedtime dosing of antihypertensives compared to morning therapy: a meta-analysis of randomised controlled trials. Eur J Prev Cardiol. 2021;28:e5-8.
Mackenzie IS, Rogers A, Poulter NR, Williams B, Brown MJ, Webb DJ, et al. Cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensives in the UK (TIME study): a prospective, randomised, open-label, blinded-endpoint clinical trial. Lancet. 2022;400:1417–25.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this article.
Conflict of interest/competing interests
Dimitrios G. Chatzis, Kalliopi Magounaki, Ioannis Pantazopoulos, Eleftherios T Beltsios, Vasiliki Katsi, and Konstantinos P. Tsioufis have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analyzed.
Code availability
Not applicable.
Author contributions
DGC, KM, IP, ETB, and VK contributed equally to manuscript writing. DGC, KM, IP, ETB, VK, and KPT contributed equally to gathering the relevant data. KPT and DC contributed equally to the final revision and polishing of this paper.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chatzis, D.G., Magounaki, K., Pantazopoulos, I. et al. Current Management of Hypertension in Older Adults. Drugs Aging 40, 407–416 (2023). https://doi.org/10.1007/s40266-023-01013-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-023-01013-9