Abstract
Background
Prescription drug costs have been rising rapidly in the USA, contributing to the persistent problem of cost-related medication nonadherence (CRN) among older Medicare beneficiaries. Given the importance of CRN and the negative outcomes associated with it, it is important to examine the factors that affect CRN. This study aims to estimate the factors influencing CRN among older Medicare beneficiaries and to rank their relative contribution in explaining CRN.
Methods
We used a 2015 Medicare Current Beneficiary Survey linked to Medicare claims data to identify older Medicare beneficiaries aged 65 years and over. Multivariate logistic regression was performed to identify factors associated with CRN. Factors included in the regression analyses were based on a conceptual framework adapted from Piette et al., including main effects (financial factors and regimen complexity) and contextual factors (sociodemographic, lifestyle and health factors). Dominance analysis was conducted to determine their relative importance in predicting CRN.
Results
Our study sample included 4427 older Medicare beneficiaries, 13.43% of whom reported CRN. For main effects, drug coverage and regimen complexity were significantly associated with CRN. Compared to beneficiaries with public coverage, those with private drug coverage were less likely to report CRN while those without drug coverage were more likely to report CRN. Having more than two monthly prescriptions was also associated with higher CRN. Significant contextual factors included age, activities of daily living limitations, perceived health status, cancer, rheumatoid arthritis, non-rheumatoid arthritis, depression, and lung disease. Dominance analysis showed drug coverage was the most influential factor in explaining CRN, after which age, ADL limitations, and depression ranked in sequence.
Conclusions
These findings can help policy makers understand the relative importance of factors affecting CRN and identify the most important areas for intervention to improve CRN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cost-related medication nonadherence (CRN) is common among elderly Medicare beneficiaries. |
Financial factors plays a significant role in CRN. |
A relatively younger group (age 65–74 years) is especially vulnerable to CRN and depression is a leading chronic condition associated with CRN. |
1 Introduction
The older population is expected to double by 2050 and be nearly 17% of the world’s population [1]. Older individuals are more likely to be vulnerable to health-related expenses and financial burden, in part owing to comorbidities and polypharmacy [2]. As prescription drug costs continue to soar in the USA [3, 4], many patients face a high medication financial burden and resort to medication nonadherence to save costs. Such behaviors include stopping or delaying filling prescriptions and taking smaller doses to make medications last longer, referred to as cost-related medication nonadherence (CRN) [5].
There are several studies in the literature that examined the relationship between CRN and insurance coverage before and after the implementation of Medicare Part D. Before Medicare Part D was introduced in 2006 to alleviate the financial burden of prescriptions for Medicare beneficiaries, many beneficiaries had insufficient insurance coverage for medications and CRN rates were high [6]. Even after part D was implemented, older beneficiaries are still burdened by their out-of-pocket prescription costs [7, 8] and CRN continues to be a significant problem [9, 10]. As CRN has been shown to have a variety of negative outcomes [6,7,8], such as more emergency utilization, hospitalization, poorer health, and even higher mortality, addressing the factors related to CRN for older Medicare beneficiaries is urgently needed. Studying risk factors related to CRN may help identify vulnerable groups and develop tailored interventions that could reduce CRN. Additionally, examining the relative importance of risk factors may also help in prioritizing social and clinical resources for reducing CRN.
Although there have been a variety of studies examining financial risk factors associated with CRN, such as healthcare coverage and income, less is known about the non-financial factors [9]. However, patients’ cost-saving behaviors and CRN can be affected by non-financial factors as some patients take their medications as prescribed regardless of the cost burden while others have medication nonadherence even though they can afford medication [10]. While some studies of CRN among older populations identified financial and non-financial factors simultaneously [6, 11,12,13,14,15], very few used a comprehensive theoretically grounded framework to guide their studies [10, 11] or determined the relative importance of these factors in CRN [16]. Additionally, current estimates of CRN rates among the general older population are lacking; indeed, most rates are based on data that are nearly a decade old. Most recent estimates of CRN are based on specific older populations, e.g., those with diabetes mellitus or glaucoma [14, 16]. As medication nonadherence is a significant public health concern, identifying current determinants and rates of CRN among the older population is of considerable clinical and social importance.
A previous study used a theoretically grounded conceptual model to identify risk factors associated with CRN in older adults based on 2004–2005 Health and Retirement Study data. While factors associated with CRN were identified (e.g., younger age [65–74 years] and female), the relative importance of the risk factors in CRN was not elucidated [9]. A recent study used a similar conceptual framework and dominance analysis to examine the importance of risk factors for adult patients with diabetes and found that depression and household income were the most important determinants of CRN [16]; depression is a well-known predictor of poor treatment adherence among patients with diabetes [17]. However, no such studies have been conducted for the overall older Medicare beneficiary population, yet findings from this line of research are likely to be more generalizable. To fill this knowledge gap, the aims of this study were to estimate the prevalence and risk factors of CRN among these beneficiaries and examine the relative importance of these factors in CRN to help inform important areas for intervention.
2 Methods
2.1 Data Sources and Study Design
This study used a 2015 survey and cost supplement files of the Medicare Current Beneficiary Survey (MCBS)-Medicare, which is sponsored by the Centers for Medicare & Medicaid Services. The MCBS is a continuous multipurpose survey of a nationally representative sample of Medicare beneficiaries. Additionally, survey and cost supplement files together contain comprehensive and detailed information on patient demographics, socioeconomic status, healthcare cost and utilization, and self-reported health status and symptoms [18]. In imputing the data, all partial information from survey respondents was preserved to the extent possible, and health insurance data from the survey and Medicare administrative files were used to identify potential payers. Analytic edits and hot-decking methods were used to estimate missing payments and charges [18]. For other variables, we deleted the records with missing data. We have added clarification about missing data: “A small number of patients with missing data were deleted from the analysis”. Data for most variables in the MCBS are fairly complete. The MCBS has established a reasonably reliable algorithm to impute healthcare cost and use variables [18]. We adopted a cross-sectional design for this quantitative study.
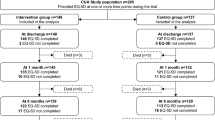
2.2 Study Cohort
This study included older community-dwelling beneficiaries aged 65 years or over. All participants included in the analytical sample were continuously enrolled in Medicare Parts A and B without Medicare Advantage enrollment and had prescription records during 2015. We excluded patients with Medicare Advantage Plans from this study to ensure complete healthcare utilization information as the Centers for Medicare & Medicaid Services Medicare data files do not include complete detailed information on healthcare usage for patients who have Medicare Advantage Plans. Patients living in institutional care settings were also excluded because they are very different from non-institutionalized patients in terms of healthcare needs, utilization pattern, and also medication adherence.
2.3 Outcome Variable
The outcome variable was CRN. A beneficiary was considered to have CRN if they reported ever having any of the following behaviors: “skipping doses of a prescription to make it last longer”, “taking smaller doses to make the medicine last longer”, and “failing or delaying to fill a prescription because of cost” [19].
2.4 Conceptual Framework and Independent Variables
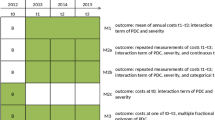
Our conceptual framework (shown in Fig. 1) was adapted from Piette et al.’s conceptual model to understand the determinants of CRN [10]. Piette et al. suggested medication adherence is modified by a wide array of cost and non-cost factors, and the cost–adherence relationship is determined by the interplay of various factors in context, such as patients’ characteristics, clinician-related factors, and health system factors. The model has been adapted to understand CRN in different populations including older adults and patients with chronic illness [9, 16, 20].
The list of independent variables included in our multivariate analyses was guided by published studies [9, 10, 16, 20] that adopted this model while taking into consideration data elements available in the MCBS-Medicare. The model included the following domains: financial factors, regimen complexity, patients’ sociodemographic factors, lifestyle factors, and health factors. Financial factors and regimen complexity have been previously shown to be the main determinants of CRN and other domains were considered contextual factors that modify their effects [10, 16].
Financial factors were: yearly income (≤ $US25,000, ≥ $US25,000), drug coverage type (Medicare Part D only, Medicaid or other public drug coverage [other state- and community-level plan], both public and private drug coverage, private drug coverage only, none), monthly out-of-pocket drug cost (cut around median: ≤ $US30, > $US30) and monthly out-of-pocket cost of other healthcare services (median split: ≤ $US50, > $US50). Regimen complexity: number of monthly prescriptions (median split: ≤ 2, > 2). Patients’ sociodemographic factors were: age (65–74, 75–84, 85 years and over), sex (male, female), race/ethnicity (non-Hispanic white, non-Hispanic black, other), marital status (married, other), and educational attainment (less than high school, high school, some college, college). Lifestyle factors were body mass index (BMI) [under-weight or normal, referred to as BMI < 25 kg/m2; overweight, referred to as BMI ≥ 25–29.9 kg/m2; obese/morbid obese, referred to as BMI ≥ 30 kg/m2] [21] and smoking status (current, past, never). Health factors were the number of activities of daily living (ADL) with limitations (none, one limitation, more than one limitation), the number of instrumental ADL with limitations (none, one limitation, more than one limitation), perceived health status (excellent/very good/good, fair/poor), chronic conditions (cardiac disease, hypertension, stroke, cancer, diabetes, rheumatoid arthritis, non-rheumatoid arthritis, depression, neurological conditions, and lung disease).
We followed the MCBS classification strategy [22, 23] to identify depression: if a beneficiary responded “all of the time” or “most of the time” to the question “In the last 12 months, how much of the time did you feel sad, blue or depressed?” and/or answered “yes” to the question “In the last 12 months, have you had 2 weeks or more when you lost interest or pleasure in the things that you usually cared about or enjoyed?”, then they were classified as depressed. These questions were found to be in high concordance with depression diagnoses in clinical settings [24, 25]. Out-of-pocket cost information and monthly prescriptions were obtained from cost supplement files and other variables were obtained from survey files.
2.5 Statistical Analyses
A Chi-square test was used to analyze patients’ characteristics by patients’ CRN status; the tests were weighted using cross-sectional sampling weights [18]. Multivariate logistic regression including all independent variables was used to determine significant variables associated with CRN. Chi-square test and logistic regression were adjusted for the MCBS complex survey design [18] and performed using survey sampling and analysis procedures in SAS Enterprise Guide version 6.1 (SAS Institute Inc., Cary, NC, USA).
To determine the relative importance of predictors of CRN, a dominance analysis [26, 27] was used. Dominance analysis is an appropriate analytic technique because it has advantages over traditional methods as it compares the relative importance of predictors in regression equations in all subset regressions [28]. The relative contribution of each predictor can be measured numerically as the percentage of explained CRN. Both the unstandardized and standardized general dominance statistics are the numerical measures. The unstandardized general dominance statistics is the average additional, unique, explained variance contribution of each independent variable to all subset models. The standardized version is the average additional, unique model, fit-scaled, explained variance contribution of each independent variable to all subset models (the unstandardized version of the statistic divided by the model fit value). Dominance analysis can also be applied to logistic regressions with complex survey data by using probability weights [29]. For dominance analysis, we included all variables that were statistically significant in multivariable logistic regressions. The dominance analysis used cross-sectional sampling weights [18] as probability weights and was performed in Stata 14.2 (StataCorp, College Station, TX, USA).
3 Results
There were 4427 older Medicare beneficiaries in our sample, 13.43% of whom reported CRN. Table 1 compares the patients’ characteristics by CRN status. Beneficiaries reporting CRN were significantly more likely to have a lower income, part D only, Medicaid or other public drug coverage, both public and private coverage, no drug coverage, higher monthly out-of-pocket drug costs, and more monthly prescriptions, be of younger age (65–74 years), female, not married, obese/morbid obese, have more ADL/instrumental ADL limitations, fair/poor perceived health status, and have chronic conditions including diabetes, rheumatoid arthritis, non-rheumatoid arthritis, depression, and lung disease than those not reporting CRN.
Table 2 presents the results from the multivariate logistic regression controlling for all factors. Significant associations were identified between CRN and the following factors: financial (drug coverage); regimen complexity; sociodemographic (age); and health (ADL limitations, perceived health status, cancer, rheumatoid arthritis, non-rheumatoid arthritis, depression, and lung disease). For instance, compared with individuals with private-only coverage, beneficiaries with part D only were more likely to report CRN (odds ratio [OR] 2.23; 95% confidence interval [CI] 1.41–3.53) and beneficiaries without drug coverage were more likely to report CRN (OR 3.30; 95% CI 1.95–5.56). Older beneficiaries were less likely to experience CRN compared with those aged 65–74 years (OR75–84 years 0.55; 95% CI 0.42–0.72; OR85+ 0.29; 95% CI 0.18–0.46). Compared with those with no ADL, individuals with two or more ADL limitations were more likely to report CRN (OR 1.60; 95% CI 1.09–2.36). Of note, the following chronic conditions were not significantly associated with CRN: cardiac disease, hypertension, stroke, diabetes, and neurological conditions.
Table 3 presents the results from dominance analysis with the unstandardized and standardized general dominance statistics. Drug coverage, a financial factor, ranked highest, followed by age, ADL limitations, depression, perceived health status, lung disease, non-rheumatoid arthritis, monthly prescriptions, rheumatoid arthritis, and cancer. The top three factors accounted for about 50% of the relative importance in explaining CRN in older Medicare beneficiaries. Depression ranked number one among the chronic conditions, with dominance of 10.41%. Although regimen complexity also plays a role in CRN, it ranked toward the bottom.
4 Discussion
Our results show that of 4427 older Medicare beneficiaries, 13.43% reported CRN based on 2015 MCBS-Medicare data, which provide a nationally representative sample of the Medicare population. This CRN rate is close to the CRN rate (12.6%) identified in another study about older Medicare beneficiaries using 2004 MCBS data [30]. Beneficiaries with private drug insurance were less likely to have CRN and individuals without coverage were more likely to have CRN. This result is as expected and is consistent with a previous study [14], as having no drug coverage increases vulnerability to CRN while public drug coverage does not protect beneficiaries from CRN effectively; private coverage alone provides more benefits. Based on our dominance analysis, drug coverage was the most influential factor in explaining CRN for older Medicare beneficiaries. Lower out-of-pocket costs due to lower cost sharing can be the main underlying reason. Cost sharing is usually lower for private drug coverage than public coverage such as Part D and Medicaid [31] and lower cost sharing has been shown to be linked with higher medication adherence in previous studies [32, 33]. Therefore, one policy implication here is that reducing cost sharing for patients with public drug coverage may help prevent CRN. Our finding that younger age is associated with CRN is consistent with previous studies [5, 9, 14, 16], indicating CRN continues to be problematic particularly for the younger group. Some possible explanations can account for this issue. For example, because the physician’s interactions and level of experience in medication management are increasing as patients’ age and the belief in the importance of medication management is greater for the older patients [34,35,36], the younger group may be more vulnerable to CRN than the older group. As with the previous studies’ conclusions, the findings from our analyses emphasize the need for policy makers to prioritize interventions for CRN to the relatively younger group of older beneficiaries. That the CRN rate identified in our study is similar to or even higher than the rate identified a decade previously indicates that interventions have been mostly ineffective for these individuals.
The number of ADL limitations also had a high ranking as a determinant of CRN. Activities of daily living limitations are a measure of disability severity and may reflect the effects of underlying diseases. Previous research also showed that older adults with a greater number of ADL limitations are more likely to report CRN [37]. Activities of daily living limitations are a measure of disability severity and may reflect the effects of underlying diseases. Prior studies have shown that ADL limitation is associated with decreased access to care [38, 39] and can act as an obstacle to purchasing and adhering to medications [12].
Depression had a relatively high importance of association with CRN in our dominance analysis and was most influential to CRN of all the chronic conditions included in our study. This finding is consistent with those of another study on older patients with diabetes [16]. Previous research has identified depression as an important predictor of CRN among the general older population [9, 22, 23]; these studies used data from 2004 to 2006. Depression medications may place an additional medication cost burden on the older population because some psychiatric medications are expensive [22]. Additionally, depression is associated with increased cognitive impairment [40], which can in turn negatively affect medication adherence among the older population [41]. These data highlight the importance of providing effective depression management for older patients with depression to decrease CRN and also warrant further investigation to determine causative factors between depression and increased risk of CRN.
Other significant factors associated with CRN included number of monthly prescriptions, perceived health status, lung disease, and arthritis, similar to other studies of different populations [5, 6, 9, 15, 16, 22]. This study found a 46% higher odds of CRN for having cancer based on a multivariate logistic regression analysis, but previous studies did not find a significant relationship [9, 16, 42]. Costs associated with cancer care continue to increase owing in part to advancements in oncologic technologies including more targeted treatments. For instance, new oncology drugs such as molecularly targeted and immunotherapy drugs are increasingly available and in use but their prices and cost sharing are very high. The fact that many of the new therapies are orally administered and thus covered under drug insurance coverage exacerbates the cost burden on patients [43, 44]. The high economic burden of cancer can cause “financial toxicity” leading to nonadherence to medication [43, 44]. Additionally, cancer risk increases with age, with an aging population, interventions designed to decrease CRN in older Medicare beneficiaries with cancer should be a priority.
There are some limitations to our study. First, the results cannot imply causality because of the cross-sectional study design. Second, CRN was based on all types of medications. We could not analyze CRN by specific medications, which could vary substantially. Knowing the exact medication to which patients were non-adherent could help clinicians and other stakeholders to target efforts to improve adherence to therapy, but our data do not contain this information. Fourth, some of the factors associated with CRN might be correlated with each other leading to potential multicollinearity. Therefore, results need to be interpreted with caution. Fifth, CRN was based on a self-report survey, therefore recall bias may occur. Sixth, our data also lacked details about factors such as patient beliefs about medication, adverse effects of medication use and healthcare system, which may also have influenced CRN [9, 45,46,47]. Hence, future studies should seek to examine the degree to which these factors affect CRN.
Despite these limitations, this study also has several strengths. First, it adds up-to-date findings to the literature documenting the rates of CRN for older Medicare beneficiaries, highlighting the continued importance and need to address CRN for this population. Second, to our best knowledge, this is the first study using nationally representative data and a dominance analysis to determine the relative importance of risk factors of CRN for older Medicare beneficiaries. Additionally, the factors examined in our study are theoretically based, which has an advantage over other studies [5, 14, 22, 30, 42] that did not have a structured approach to examine the factors affecting CRN.
In summary, this study provides a ranking list of the importance of factors correlated with CRN, and corresponding implications from these findings. The results show that drug coverage is the strongest influencing factor of CRN and public insurance alone is not sufficient in preventing CRN. More research is needed to measure how well current public drug coverage types, such as Part D, protect the older beneficiaries against CRN and how to increase or modify coverage to prevent CRN. Because age ranked the second highest predictor of CRN, screening and monitoring for CRN among the relatively younger group is necessary and may help to curtail nonadherence in a large proportion of individuals.
As depression overrode all other chronic conditions, including arthritis and lung disease, as an influencer of CRN, the clinicians should carefully consider antidepressant prescribing to depressed patients as the use of antidepressants can improve not only the management of depression itself but also potentially adherence of other types of medications that may be essential to the management of other conditions. Additionally, the importance of managing depression effectively is paramount for high-quality care. Although prior research has recommended potentially effective depression management methods for the older patients such as integrated collaborative care models [48], treating depression may also worsen the medication cost burden. Hence, cost-effectiveness studies are needed to determine the most appropriate depression management strategies in the geriatric population.
5 Conclusions
Cost-related medication nonadherence prevalence among older Medicare beneficiaries was 16.5% based on our data from 2015. Drug coverage was the most important determinant of CRN. Aside from this financial factor, age and several health factors were also associated with CRN. As CRN is associated with adverse health events and increased health services utilization [6,7,8] such as higher mortality and more emergency utilization, policy makers can use this information to identify high-risk subgroups and provide targeted interventions to improve CRN and health outcomes among these groups.
Data Availability
The data source used for this study is the Medicare Current Beneficiary Survey (MCBS) linked with Medicare claims. It is available upon request from the MCBS program.
References
He W, Goodkind D, Kowal PR. An aging world: 2015. Washington, DC: United States Census Bureau; 2016.
Nobili A, Garattini S, Mannucci PM. Multiple diseases and polypharmacy in the elderly: challenges for the internist of the third millennium. J Comorbidities. 2011;1:28–44.
Schumock GT, Stubbings J, Wiest MD, Li EC, Suda KJ, Matusiak LM, et al. National trends in prescription drug expenditures and projections for 2018. Am J Health Syst Pharm. 2018;75:1023–38.
Kesselheim AS, Avorn J, Sarpatwari A. The high cost of prescription drugs in the United States: origins and prospects for reform. JAMA. 2016;316:858–71.
Madden JM, Graves AJ, Zhang F, Adams AS, Briesacher BA, Ross-Degnan D, et al. Cost-related medication nonadherence and spending on basic needs following implementation of Medicare Part D. JAMA. 2008;299:1922–8.
Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically III adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94:1782–7.
Tamblyn R, Laprise R, Hanley JA, Abrahamowicz M, Scott S, Mayo N, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285:421–9.
Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care. 2004;42:626–34.
Zivin K, Ratliff S, Heisler MM, Langa KM, Piette JD. Factors influencing cost-related nonadherence to medication in older adults: a conceptually based approach. Value Health. 2010;13:338–45.
Piette JD, Heisler M, Horne R, Alexander GC. A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures. Soc Sci Med. 2006;62:846–57.
Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007;22:864–71.
Zhang JX, Lee JU, Meltzer DO. Risk factors for cost-related medication non-adherence among older patients with diabetes. World J Diabetes. 2014;5:945–50.
Zhang JX, Meltzer DO. Risk factors for cost-related medication non-adherence among older patients with cancer. Integr Cancer Sci Ther. 2015;2:300–4.
Blumberg DM, Prager AJ, Liebmann JM, Cioffi GA, De Moraes CG. Cost-related medication nonadherence and cost-saving behaviors among patients with glaucoma before and after the implementation of Medicare Part D. JAMA Ophthalmol. 2015;133:985–96.
Harrold LR, Briesacher BA, Peterson D, Beard A, Madden J, Zhang F, et al. Cost-related medication nonadherence in older patients with rheumatoid arthritis. J Rheumatol. 2013;40:137–43.
Kang H, Lobo JM, Kim S, Sohn M-W. Cost-related medication non-adherence among US adults with diabetes. Diabetes Res Clin Pract. 2018;143:24–33.
Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008;31:2398–403.
Centers for Medicare and Medicaid Service. Medicare Current Beneficiary Survey related files. https://www.cms.gov/MCBS. Accessed Dec 2018.
Burcu M, Alexander GC, Ng X, Harrington D. Construct validity and factor structure of survey-based assessment of cost-related medication burden. Med Care. 2015;53:199–206.
Piette JD, Beard A, Rosland AM, McHorney CA. Beliefs that influence cost-related medication non-adherence among the “haves” and “have nots” with chronic diseases. Patient Pref Adherence. 2011;5:389–96.
Centers for Disease Control and Prevention. About adult BMI. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Accessed Dec 2018.
Bambauer KZ, Safran DG, Ross-Degnan D, Zhang F, Adams AS, Gurwitz J, et al. Depression and cost-related medication nonadherence in Medicare beneficiaries. Arch Gen Psychiatry. 2007;64:602–8.
Zivin K, Madden JM, Zhang F, Soumerai SB, Graves AJ. Cost-related medication nonadherence among beneficiaries with depression following Medicare Part D. Am J Geriatr Psychiatry. 2009;17:1068–76.
Rogers WH, Wilson IB, Bungay KM, Cynn DJ, Adler DA. Assessing the performance of a new depression screener for primary care (PC-SAD). J Clin Epidemiol. 2002;55:164–75.
Rogers WH, Adler DA, Bungay KM, Wilson IB. Depression screening instruments made good severity measures in a cross-sectional analysis. J Clin Epidemiol. 2005;58:370–7.
Azen R, Budescu DV. The dominance analysis approach for comparing predictors in multiple regression. Psychol Methods. 2003;8:129–48.
Azen R, Traxel N. Using dominance analysis to determine predictor importance in logistic regression. J Educ Behav Stat. 2009;34:319–47.
Grömping U. Estimators of relative importance in linear regression based on variance decomposition. Am Statistician. 2007;261:139–47.
Luchman JN. Determining subgroup difference importance with complex survey designs: an application of weighted dominance analysis. Surv Pract. 2015;8:1–10.
Soumerai SB, Pierre-Jacques M, Zhang F, Ross-Degnan D, Adams AS, Gurwitz J, et al. Cost-related medication nonadherence among elderly and disabled medicare beneficiaries: a national survey 1 year before the medicare drug benefit. Arch Intern Med. 2006;166:1829–35.
Kaiser Family Foundation. How does prescription drug spending and use compare across large employer plans, Medicare Part D, and Medicaid? https://www.kff.org/medicare/issue-brief/how-does-prescription-drug-spending-and-use-compare-across-large-employer-plans-medicare-part-d-and medicaid/. Accessed May 2019.
Gellad WF, Grenard J, McGlynn EA, Gellad WF, Grenard JL, McGlynn EA. A review of barriers to medication adherence. In: A framework for driving policy options. Santa Monica, CA: RAND Corp; 2009.
Aziz H, Hatah E, Bakry MM, et al. How payment scheme affects patients’ adherence to medications? A systematic review. Patient Prefer Adherence. 2016;10:837–50.
Cohen MJ, Shaykevich S, Cawthon C, Kripalani S, Paasche-Orlow MK, Schnipper JL. Predictors of medication adherence postdischarge: the impact of patient age, insurance status, and prior adherence. J Hosp Med. 2012;7:470–5.
Gazmararian J, Jacobson KL, Pan Y, Schmotzer B, Kripalani S. Effect of a pharmacy-based health literacy intervention and patient characteristics on medication refill adherence in an urban health system. Ann Pharmacother. 2010;44:80–7.
Hinkin CH, Hardy DJ, Mason KI, Castellon SA, Durvasula RS, Lam MN, et al. Medication adherence in HIV-infected adults: effect of patient age, cognitive status, and substance abuse. AIDS. 2004;18(Suppl. 1):S19–25.
Zhang JX, Lee JU, Pandey K, Meltzer DO. Variation in cost-related medication non-adherence with functional limitations and frequency of hospitalization in older adults. Ann Gerontol Geriatric Res. 2015;2(1):1023.
Chan L, Beaver S, MacLehose RF, Jha A, Maciejewski M, Doctor JN. Disability and health care costs in the Medicare population. Arch Phys Med Rehab. 2002;83:1196–201.
MacLachlan M, Mannan H, McAuliffe E. Access to health care of persons with disabilities as an indicator of equity in health systems. Open Med. 2011;5:e10.
Pellegrino LD, Peters ME, Lyketsos CG, Marano CM. Depression in cognitive impairment. Curr Psychiatry Rep. 2013;15:384.
Campbell NL, Boustani MA, Skopelja EN, Gao S, Unverzagt FW, Murray MD. Medication adherence in older adults with cognitive impairment: a systematic evidence-based review. Am J Geriatr Pharmacother. 2012;10:165–77.
Nekhlyudov L, Madden J, Graves AJ, Zhang F, Soumerai SB, Ross-Degnan D. Cost-related medication nonadherence and cost-saving strategies used by elderly Medicare cancer survivors. J Cancer Surviv. 2011;5:395–404.
Tran G, Zafar SY. Financial toxicity and implications for cancer care in the era of molecular and immune therapies. Ann Transl Med. 2018;6(9):166.
Peppercorn J. Financial toxicity and societal costs of cancer care: distinct problems require distinct solutions. Oncologist. 2017;22(2):123–5.
Aikens JE, Piette JD. Diabetic patients’ medication underuse, illness outcomes, and beliefs about antihyperglycemic and antihypertensive treatments. Diabetes Care. 2009;32:19–24.
Piette JD, Heisler M, Wagner TH. Medication characteristics beyond cost alone influence decisions to underuse pharmacotherapy in response to financial pressures. J Clin Epidemiol. 2006;59:739–46.
Yap AF, Thirumoorthy T, Kwan YH. Medication adherence in the elderly. J Clin Gerontol Geriatr. 2016;7:64–7.
Chang-Quan H, Bi-Rong D, Zhen-Chan L, Yuan Z, Yu-Sheng P, Qing-Xiu L. Collaborative care interventions for depression in the elderly: a systematic review of randomized controlled trials. J Investig Med. 2009;57:446–55.
Acknowledgements
We thank Gary Deyter for his editorial assistance.
Author information
Authors and Affiliations
Contributions
All authors contributed to the planning, conduct, and reporting of the work described in the article. Dian Gu is responsible for the overall content as the guarantor.
Corresponding author
Ethics declarations
Funding
No funding was received for the conduct of this study or the preparation of this article.
Conflict of interest
Dian Gu and Chan Shen have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
This study received institutional review board exemption status from the University of Texas MD Anderson Cancer Center.
Rights and permissions
About this article
Cite this article
Gu, D., Shen, C. Assessing the Importance of Factors Associated with Cost-Related Nonadherence to Medication for Older US Medicare Beneficiaries. Drugs Aging 36, 1111–1121 (2019). https://doi.org/10.1007/s40266-019-00715-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00715-3