Abstract
The introduction of multi-valent pneumococcal vaccines around the world, such as the 13-valent pneumococcal conjugate vaccine (PCV13), has had a significant effect in reducing the burden of disease caused by Streptococcus pneumoniae infection globally. However, S. pneumoniae serotypes not covered by PCV13 still cause significant disease. A 20-valent pneumococcal conjugate vaccine (PCV20; Prevnar20®; Apexxnar®) has recently been licensed for active immunisation for the prevention of invasive disease and pneumonia caused by S. pneumoniae in adults. PCV20 contains all components of PCV13 with the addition of polysaccharide conjugates of seven more serotypes, selected based on their generalised geographic distribution and relative prevalence as a cause of pneumococcal disease. The immunogenicity of PCV20 in adults has been demonstrated in a well-designed program of clinical trials which showed that PCV20 administered as a single dose by intramuscular injection induced robust immune responses to all 20 S. pneumoniae serotypes covered by the vaccine. PCV20 was well tolerated, with a tolerability and safety profile similar to that for PCV13. By expanding the coverage of disease-causing S. pneumoniae serotypes relative to other PCVs, PCV20 presents a valuable new tool with the potential to further reduce the impact of pneumococcal disease.
Plain Language Summary
Pneumonia and other diseases caused by infection with the bacterium Streptococcus pneumoniae are a significant health concern. The introduction of vaccines targeting multiple S. pneumoniae serotypes [such as the 13-valent pneumococcal conjugate vaccine (PCV13)] has had a significant effect in reducing pneumococcal disease; however, serotypes not covered by PCV13 still cause significant disease. Recently, a new vaccine [20-valent pneumococcal conjugate vaccine (PCV20; Prevnar20®; Apexxnar®)] has been developed and licensed for use in immunisation for the prevention of invasive disease and pneumonia caused by S. pneumoniae in adults. The ability of PCV20 (administered as a single dose by intramuscular injection) to elicit strong immune responses to all 20 serotypes covered by the vaccine was demonstrated in a well-designed program of clinical trials. PCV20 is well tolerated, with pain at the injection site and muscle pain being the most common adverse reactions. By expanding the coverage of disease-causing S. pneumoniae serotypes, PCV20 presents a valuable new tool with the potential to further reduce the impact of pneumococcal disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features for this Adis Drug Evaluation can be found at https://doi.org/10.6084/m9.figshare.19860529 |
Based on PCV13, with the addition of polysaccharide conjugates of seven more S. pneumoniae serotypes |
Licensed in the USA and EU for active immunisation for the prevention of invasive disease and pneumonia caused by S. pneumoniae in adults. |
Elicits robust immune responses to all 20 S. pneumoniae serotypes covered by the vaccine |
Well tolerated, with a tolerability and safety profile similar to that for PCV13 |
1 Introduction
Streptococcus pneumoniae infection, manifesting as invasive pneumococcal disease (IPD; e.g. bacteraemic pneumonia, bacteraemia, meningitis) or non-invasive disease [including non-bacteraemic community-acquired pneumonia (CAP)], is a significant cause of morbidity and mortality worldwide [1,2,3]. More than 100 S. pneumoniae serotypes have been identified (with distinct capsule polysaccharides), although a minority subset of these serotypes is responsible for the majority of pneumococcal disease [4].
Vaccines that target multiple S. pneumoniae serotypes are widely available for the prevention of pneumococcal disease, including the 23-valent pneumococcal polysaccharide vaccine (PPSV23; Pneumovax23®) and pneumococcal conjugate vaccines (PCVs) [5,6,7,8]. PPSV23 is widely used and has been shown to be an effective tool in reducing the burden of pneumococcal disease [8]. However, PPSV23 is limited in that it elicits a T-cell independent immune response, without inducing immunological memory associated with long-lasting immunity [9]. Furthermore, there remains conflicting evidence of its effectiveness against non-invasive pneumococcal pneumonia [10]. PCVs, such as the 13-valent PCV (PCV13; Prevnar13®; Prevenar 13®), are comprised of purified serotype-specific polysaccharides that are covalently linked (i.e. conjugated) to an immunogenic carrier protein [8]. In contrast to unconjugated pneumococcal vaccines, PCVs have been shown to elicit a T-cell dependent immune response, resulting in robust functional antibody responses and immunological memory [8, 11]. Another advantage of PCVs is that mucosal immunity stimulated by these vaccines has the potential to reduce S. pneumoniae nasopharyngeal carriage, thereby lowering transmission [6, 12, 13]. A seven-valent PCV (PCV7), containing polysaccharides from S. pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F and 23F conjugated to the immunogenic carrier protein CRM197 (a non-toxic variant of diphtheria toxin), was the first PCV to become widely available. PCV7 was later succeeded by PCV13, which (along with the seven polysaccharides in PCV7) contains additional polysaccharides from S. pneumoniae serotypes 1, 3, 5, 6A, 7F and 19A [8, 11, 14]. A 10-valent PCV (PCV10; Synflorix®) containing 10 of the PCV13 serotypes (conjugated to different carrier proteins to that used in PCV7/PCV13) is also licensed and available in some countries (including those in the EU [15]) for paediatric use [8].
The introduction of pneumococcal vaccines around the world has had a significant impact in reducing the burden of pneumococcal disease globally, both through direct and indirect means, whereby wide use of vaccination has reduced both S. pneumoniae infection and carriage rates [6, 16], with the effects of PCV vaccines on carriage rates also contributing towards significant herd immunity benefits by reducing transmission [13, 17]. However, S. pneumoniae serotypes not covered by PCV13 still cause significant disease [5, 18,19,20], partly due to vaccine-induced serotype replacement, whereby the success of pneumococcal vaccines has (to a degree) driven the replacement of vaccine serotypes by non-vaccine serotypes [21, 22]. Given the persisting burden of pneumococcal disease, the development of pneumococcal vaccines has continued.
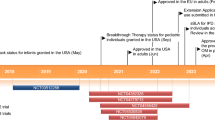
Two further PCVs containing additional serotypes to expand vaccine coverage have recently been licensed (including in the USA and EU) for active immunisation for the prevention of invasive disease and pneumonia caused by S. pneumoniae in adults: a 15-valent PCV (PCV15; Vaxneuvance®) containing the same polysaccharides as PCV13 plus those of two additional serotypes (22F and 33F), each conjugated to CRM197 [23, 24]; and a 20-valent PCV (PCV20; Prevnar20®; Apexxnar®) [25, 26], the focus of this review. PCV20 is based on the PCV13 formulation and contains all components of PCV13 with the addition of polysaccharide conjugates of seven more serotypes (8, 10A, 11A, 12F, 15B, 22F and 33F) [5, 25, 26]. The additional serotypes were selected for inclusion based on their generalised geographic distribution and relative prevalence (among residual serotypes) as a cause of pneumococcal disease, as well as other factors that support their inclusion, such as a potential association with antibiotic resistance and/or greater disease severity [27]. Serotypes covered by PCV20 but not by PCV13 are responsible for a significant proportion (approximately 30% or more) of IPD cases in adults [28,29,30].
This article reviews the immunogenicity, tolerability and safety of PCV20 in its use for active immunisation for the prevention of invasive disease and pneumonia caused by S. pneumoniae in adults.
2 Immunogenicity of PCV20
The immunogenicity of PCV20 in adults has been established over a number of double-blind [27, 31,32,33,34,35,36] and open-label [37] randomised, controlled clinical trials (Table 1), with the pivotal trial (B7471007) evaluating the immunological non-inferiority of PCV20 to PCV13 (for the 13 matched S. pneumoniae serotypes in PCV13) and PPSV23 (for the seven additional S. pneumoniae serotypes) [34]. In the trials, immune responses elicited against pneumococcal serotypes were evaluated using opsonophagocytic activity (OPA) assays with serotype-specific OPA geometric mean titres (GMTs) measured before the first vaccination and ~1 month after each vaccination [27, 31,32,33,34, 37]. The OPA assay is a complex, functional assay designed to replicate the host defence against pneumococcal infection [38]. Involving phagocytes, complement and bacterial cells, the assay measures the ability of serum antibodies to opsonise pneumococci [38]. Although no specific opsonic antibody titre that is predictive of protection against pneumococcal disease has been established [25, 26], OPA acts as a surrogate marker for vaccine efficacy against invasive disease [38]. Unless otherwise indicated, immunogenicity data presented in this section are based on responses at 1 month after vaccination. Individuals in immunocompromised groups were excluded from the trials.
2.1 Pivotal Phase III Trial
In B7471007, pneumococcal vaccine-naïve adults (n = 3902) were enrolled into one of three cohorts based on age (18–49 years, 50–59 years or ≥60 years) [34]. Healthy subjects as well as immunocompetent subjects with stable underlying health conditions (including chronic cardiovascular disease, chronic pulmonary disease, renal disorders, diabetes mellitus and chronic liver disease) or with medical risk conditions and behaviours known to increase the risk of serious pneumococcal pneumonia and IPD (e.g., smoking) were included [34].
In the main cohort, 3009 subjects aged ≥60 years were randomly assigned (1꞉1) to PCV20 followed 1 month later with saline placebo or to PCV13 followed 1 month later with PPSV23 [34]. Immune responses elicited by PCV20 1 month after vaccination were evaluated against those elicited by PCV13 (for the 13 matched serotypes) or PPSV23 (for the seven additional serotypes), with non-inferiority inferred if the lower bound of the two-sided 95% confidence interval (CI) for the OPA GMT ratio was >0.50 (i.e. two-fold). Baseline characteristics and demographics were well balanced between the two groups in the cohort. The mean age of subjects was 64.6 years in both groups, with approximately one third of subjects in each group being aged ≥65 years. Similar proportions of subjects in the PCV20/placebo and PCV13/PPSV23 groups had one or more risk factor (32.4% vs 36.3%), with the most common risk factors being diabetes mellitus (14.6% vs 17.1%), current smoker (11.4% vs 12.6%), chronic pulmonary disease (9.1% vs 8.2%) and chronic cardiovascular disease (4.9% vs 7.7%) [34].
PCV20 induced robust immune responses to all 20 S. pneumoniae serotypes covered by the vaccine [34]. Immune responses elicited by PCV20 1 month after vaccination were non-inferior to those elicited by PCV13 for all 13 matched serotypes (OPA GMT ratios of 0.76–1.00 across the 13 serotypes) and non-inferior to those elicited by PPSV23 for six of the seven additional serotypes (OPA GMT ratios of 1.38–3.12 across the six serotypes). The immune response elicited by PCV20 against the one other serotype (serotype 8) missed the non-inferiority criterion by a narrow margin (OPA GMT ratio vs PPSV23, 0.55; 95% CI 0.49–0.62). In further analyses supporting the immunogenicity of PCV20, a ≥4-fold rise in OPA titres from baseline to 1 month post PCV20 vaccination was observed for 55.6–87.4% of PCV20 recipients across the 20 serotypes [39]. Also of note, the percentage of PCV20 recipients achieving a ≥4-fold rise in OPA titres for serotype 8 (77.8%) fell within the range observed for the 13 matched serotypes following vaccination with PCV13 (54.0%–84.0%) [34].
In B7471007, the immunogenicity of PCV20 in subjects aged 18–59 years was demonstrated through immuno-bridging, whereby the effectiveness of the vaccine was inferred through comparison of the immune responses to each of the 20 vaccine serotypes for subjects aged 18–49 years and for subjects aged 50–59 years with those of the corresponding immune responses in subjects aged 60–64 years [34]. In each of these cohorts, subjects were randomised 3:1 to receive PCV20 or PCV13, with comparative analyses performed between the responses elicited in PCV20 recipients in these cohorts versus those elicited in PCV20 recipients aged 60–64 years from the main cohort. Immunobridging was declared to be successful if the lower bound of the two-sided 95% CI for the OPA GMT ratio was >0.50 (i.e. two-fold) [34].
In these analyses, serotype-specific immune responses elicited by PCV20 met the criteria for successful immunobridging for each of the 20 vaccine serotypes [34]. OPA GMT ratios ranged (across the different serotypes) from 1.00 to 4.80 for subjects aged 18–49 years (n = 251–317) and from 0.80 to 1.68 for subjects aged 50–59 years (n = 266–320) relative to those aged 60–64 years (n = 765–941) [25].
2.2 Phase III Trial in Vaccine-Experienced Adults Aged ≥65 Years
The immunogenicity of PCV20 in adults ≥65 years of age who had previously been vaccinated with different pneumococcal vaccine regimens was evaluated in a randomised, open-label phase III trial (B7471006) involving 875 subjects [37]. Healthy subjects as well as immunocompetent subjects with pre-existing stable disease were included and were enrolled into one of three cohorts based on their prior pneumococcal vaccination history. The first cohort included participants (n = 375) who had received PPSV23 (only) ≥1 to ≤5 years prior, the second cohort included participants (n = 375) who had received PCV13 (only) ≥6 months prior and the third cohort included participants (n = 125) who had received PCV13 followed by PPSV23 (with PPSV23 given ≥1 year prior to study vaccination). Participants with prior PPSV23 vaccination (only) were randomised 2:1 to receive PCV20 or PCV13 and participants with prior PCV13 vaccination (only) were randomised 2:1 to receive PCV20 or PPSV23, whereas all participants with prior vaccination with both PCV13 and PPSV23 received PCV20 [37].
The trial was not designed for hypothesis testing, and statistical analyses performed were descriptive only [37]. Furthermore, the study design did not permit comparisons across cohorts since the initial (i.e. pre-baseline) pneumococcal vaccine regimen received was not randomised. Nonetheless, the trial showed that robust immune responses were elicited by PCV20 in vaccine-experienced adults aged ≥65 years to all 20 serotypes covered by the vaccine, regardless of prior pneumococcal vaccination. Noting that interpretation of the results is complicated by the different initial vaccine regimens received (including timelines) affecting baseline OPA GMTs, for almost all of the 13 serotypes common to PCV20 and PCV13 and for all seven additional serotypes, OPA GMTs 1 month post PCV20 vaccination were highest in the cohort with prior PCV13 vaccination only, followed by the cohorts with prior PCV13 and PPSV23 and with prior PPSV23 only [37].
2.3 Co-Administration with Other Vaccines
Two randomised, double-blind phase III trials have recently been completed which investigated the co-administration of PCV20 with a quadrivalent inactivated influenza vaccine (Fluad Quadrivalent; QIV) (B7471004) [35] or with a booster dose of the RNA-based SARS-CoV-2 (COVID-19) vaccine BNT162b2 (B7471026) [36]. Both trials were conducted in subjects aged ≥65 years, with subjects stratified by pneumococcal vaccine history [35, 36].
In B7471004, immune responses to both PCV20 and the QIV after co-administration were non-inferior to those when the vaccines were given 1 month apart [35]. In total, 1796 subjects (median age, 71 years) were randomised 1:1 to receive PCV20 with the QIV (co-administration group) or the QIV followed by PCV20 1 month later (separate administration group), with saline injections used as appropriate to maintain blinding. Using OPA assays and haemagglutination inhibition (HAI) assays to assess PCV20 and QIV immunogenicity, respectively, GMTs 1 month post vaccination in the co-administration group were non-inferior to those in the separate administration group for all 20 pneumococcal vaccine serotypes (prespecified two-fold criterion) and all four influenza vaccine strains (prespecified 1.5-fold criterion) [35].
In B7471026, no hypothesis testing was performed, and the statistical analysis was descriptive only; however, robust immune responses to both PCV20 and a booster dose of BNT162b2 were observed both with concomitant and separate administration of the vaccines [36]. In the trial, 570 subjects (mean time of 8.1 months since receiving a second dose of BNT162b2 and 3.5 years since the most recent pneumococcal vaccination) were randomised 1:1:1 to receive PCV20 only, BNT162b2 only, or PCV20 and BNT162b2 in opposite arms at the same visit. Again, saline injections were used as appropriate to maintain blinding. PCV20 elicited robust immune responses (based on OPA assay GMTs) to all 20 pneumococcal serotypes, with similar responses observed whether PCV20 was co-administered with BNT162b2 or given alone. Similarly, a BNT162b2 booster dose elicited a strong immune response against SARS-CoV-2 (based on SARS-CoV-2 full-length S-binding protein IgG geometric mean concentrations) regardless of concomitant administration with PCV20 or when given alone, with similar responses observed in both conditions [36].
2.4 Other Trials of Interest
Further supportive evidence for the immunogenicity of PCV20 is available from several other randomised controlled trials in the PCV20 clinical development program (Table 1), with robust immune responses to all 20 vaccine serotypes elicited by PCV20 in each of these trials.
As part of the clinical development program for PCV20, a phase III clinical trial (B7471008) was conducted to assess lot-to-lot consistency by evaluating the immune responses across three different vaccine lots of PCV20 [32]. In B7471008, 1710 pneumococcal vaccine-naïve subjects aged 18–49 years were randomised (2:2:2:1) to one of three lots of PCV20, or PCV13 (included as a safety control group). Based on pairwise comparisons of OPA GMTs between groups, equivalence in immune responses across the three PCV20 lots was demonstrated for all 20 vaccine serotypes, with the 95% CI of the OPA GMT ratios all within the prespecified equivalence interval (0.5–2.0). Secondary immunogenicity endpoint data [including OPA geometric mean fold rises (GMFRs), the percentages of subjects with a ≥4-fold rise in OPA titres and the percentages of subjects with OPA titres ≥ the lower limit of quantitation] were generally similar across the three vaccine lots. Across all lots, OPA GMFRs ranged from 4.6 to 175.7 depending on the serotype, again demonstrating strong responses for all 20 vaccine serotypes [32].
In the randomised, double-blind, active-controlled, multicentre phase II trial B7471002, 444 pneumococcal vaccine-naïve subjects aged 60–64 years were randomised to receive PCV20 followed 1 month later by saline placebo or PCV13 followed 1 month later by PPSV23 [31]. Again, this trial showed that PCV20 elicited robust immune responses to all 20 vaccine serotypes, with GMFRs among PCV20 recipients ranging from 6.0 to 113.4 across the 20 serotypes and the percentages of subjects with a ≥4-fold rise from baseline in OPA titres ranging from 53.5% to 90.2% [31]. Of note, this trial also investigated the persistence of the antibody response elicited by PCV20, with follow-up out to 12 months post vaccination [40]. While there was a decline in OPA GMTs from Month 1 to Month 12 post PCV20 vaccination, antibody responses at Month 12 remained elevated from baseline, with OPA GMFRs from baseline to Month 12 ranging from 1.9 to 15.6 across the 20 vaccine serotypes [40].
3 Tolerability and Safety of PCV20
Tolerability and safety data on PCV20 in adults are available from the eight randomised controlled trials detailed in Table 1. In the trials, solicited local reactions (i.e. redness, swelling, pain at the injection site) and systemic events (i.e. fever, headache, fatigue, muscle pain, joint pain) were recorded for 10 (or 14 [27, 33]) days and 7 (or 14 [27, 33]) days, respectively, after study vaccination; data on adverse events were collected for 1 month post vaccination and data on serious adverse events (SAEs) and newly-diagnosed chronic medical conditions (NDCMCs) were collected for 6 (or 12 [31]) months post vaccination [27, 31,32,33,34,35,36,37].
Based on pooled data from six of the trials (B7471001, -02, -05, -06, -07, -08), in which 4552 subjects received PCV20, the most commonly reported solicited adverse reactions in subjects aged 18–59 years were pain at the injection site (reported in > 70% of subjects), muscle pain (> 50%), fatigue (> 40%), headache (> 30%), arthralgia (> 10%) and injection site swelling (> 10%), and the most commonly reported solicited adverse reactions in subjects aged ≥ 60 years were pain at the injection site (> 50%), muscle pain (> 30%), fatigue (> 30%), headache (> 20%) and arthralgia (> 10%) [25]. Across all six trials, 67 (1.5%) of 4552 subjects experienced one or more SAE within 6 months of vaccination with PCV20 compared with 44 (1.8%) of 2496 subjects after vaccination with PCV13 or another control vaccine, while the percentage of subjects experiencing SAEs within 1 month of vaccination was 0.4% in both groups [25].
In the pivotal B7471007 trial in pneumococcal vaccine-naïve adults (Sect. 2.1), within each age cohort similar percentages of subjects receiving PCV20 and PCV13 reported local site reactions (Fig. 1a–c) or systemic events (Fig. 1d–f), with a general trend (in both groups) of fewer older subjects reporting reactions than younger subjects [34]. Pain at the injection site was the most common local reaction and muscle pain was the most common systemic event (Fig. 1). The vast majority of reactions and events (both among PCV20 and PCV13 recipients) were mild to moderate in severity. Within each age cohort, similar percentages of PCV20 and PCV13 recipients experienced one or more adverse events in the 1 month post vaccination (15.2% vs 11.6%, 10.2% vs 8.1% and 9.8% vs 11.1% of subjects aged 18–49 years, 50–59 years and ≥ 60 years, respectively), and few subjects (< 1.5% after either vaccine across the age cohorts) experienced adverse events considered by the investigator to be related to the study vaccine. Immediate adverse events (occurring within 30 min of vaccination) were reported infrequently (in < 1.0% of subjects). SAEs and NDCMCs through 6 months after vaccination with PCV20 or PCV13 were also reported infrequently (SAEs in ≤ 2.4% and NDCMCs in ≤ 2.3% of subjects after either vaccine across age cohorts) and at a similar incidence between vaccine groups within each age cohort. No SAEs or NDCMCs reported in the trial were considered to be vaccine related. There was one death during the trial, in a subject in the PCV20/saline group, the result of a traumatic injury, unrelated to the study vaccine [34].
Solicited local reactions occurring within 10 days (a–c) and solicited systemic events occurring within 7 days (d–f) of vaccination with PCV20 or PCV13 in subjects aged 18–49 years (a, d), 50–59 years (b, e) and ≥ 60 years (c, f) in the pivotal B7471007 trial [34]. PCV13 13-valent pneumococcal conjugate vaccine, PCV20 20-valent pneumococcal conjugate vaccine. * ≥ 38 °C
Data from the B7471006 trial (Sect. 2.2) in subjects aged ≥ 65 years with prior pneumococcal vaccination demonstrated a PCV20 safety and tolerability profile consistent with that observed in the pivotal B7471007 trial in pneumococcal vaccine-naïve adults [34, 37]. The incidences of local reactions, systemic events and adverse events after PCV20 vaccination in B7471006 were similar across cohorts with previous PCV13 (only), PPSV23 (only) or PCV13 and PPSV23 vaccination and comparable with the incidences observed after PCV13 or PPSV23 vaccination in control groups [37]. Again, injection-site pain and muscle pain were the most commonly reported local reactions and systemic events, respectively, following PCV20 vaccination. No vaccine-related SAEs or NDCMCs were observed [37].
Of further interest, co-administration of PVC20 with a QIV or a booster dose of BNT162b2 appears to be well tolerated, based on data from B7471004 and B7471026, respectively (Sect. 2.3) [35, 36]. Besides a slight increase in the incidence of systemic events, particularly mild fatigue (20.0% with co-administration versus 10.8–12.6% with separate administration), co-administration of PCV20 and the QIV had a similar tolerability profile to that for either individual vaccine [35]. In B7471026, co-administration of PCV20 and BNT162b2 had a tolerability profile that was overall similar to that of BNT162b2 administered alone [36].
Finally, given the similarities between PCV20 and PCV13 (in terms of manufacture and formulation), post-marketing experience with PCV13 has some relevance to PCV20 [25, 26]. Adverse reactions of interest reported in post-marketing experience with PCV13 include anaphylactic/anaphylactoid reactions (including shock), angioneurotic oedema, erythema multiforme and injection-site reactions including injection-site lymphadenopathy, dermatitis, pruritus and urticaria [25, 26].
4 Dosage and Administration of PCV20
In the USA, PCV20 is indicated for active immunisation for the prevention of pneumonia and invasive disease caused by S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F and 33F in adults aged ≥ 18 years [25]. PCV20 is also approved for active immunisation for the prevention of invasive disease and pneumonia caused by S. pneumoniae in individuals aged ≥ 18 years in the EU [26].
PCV20 is administered by intramuscular injection as a single dose of 0.5 mL [25, 26]. Appropriate medical treatment and supervision used to manage immediate allergic reactions must be immediately available should an acute anaphylactic reaction occur following PCV20 administration [25, 26]. Local prescribing information should be consulted for full details relating to the administration of PCV20, including further information on contraindications, warnings and precautions, and its use in special patient populations.
5 PCV20 in Adults—Current Status
Based on an October 2021 update, the US Advisory Committee on Immunization Practices (ACIP) now recommends the use of either PCV20 alone or PCV15 in series with PPSV23 for all adults aged ≥ 65 years who have not previously received a PCV or whose previous vaccination history is unknown [5]. Furthermore, either PCV20 alone or PCV15 in series with PPSV23 is also recommended for adults aged 19–64 years with certain underlying medical conditions or other risk factors who have not previously received a PCV or whose previous vaccination history is unknown [5]. If PCV15 is used, this should be followed by a dose of PPSV23 after an interval of ≥ 1 year (although a minimum interval of 8 weeks can be considered for adults in certain vulnerable groups) [5]. In adults who have previously received PPSV23 (only), either PCV20 or PCV15 can be given ≥ 1 year after their last PPSV23 dose (without the need for another dose of PPSV23 in those given PCV15) [5]. Any potential public health benefits of PCV20 or PCV15 in adults who have previously received PCV13 (with or without PPSV23) are unknown, and it is recommended that adults with previous PCV13 alone should complete the previously recommended PPSV23 series [6], although PCV20 may be used if PPSV23 is not available [5].
In Europe, recommendations for pneumococcal vaccinations in adults are complex, with substantial variation across different countries in terms of the age and risk groups recommended for vaccination and which vaccine(s) should be used [41,42,43]. Across Europe, PPSV23 is widely recommended in adults aged ≥ 65 years, with several countries recommending its use in series with a PCV (e.g. PCV13). Several countries also recommend vaccination with PPSV23 (with or without a PCV) in younger adults, particularly those with factors that put them at higher risk of pneumococcal disease [41]. It has been suggested that simplifying and unifying pneumococcal vaccination recommendations across Europe could help improve vaccine uptake and further reduce pneumococcal disease burden [42, 43]. Coinciding such a process with an updated evaluation of the potential roles of PCV20 and PCV15 in European vaccination recommendations could indeed be of value.
For lower-middle-income countries in other parts of the world, World Health Organization (WHO) guidelines recommend that the introduction of PCVs into national childhood vaccination programs should be prioritised over the introduction of a pneumococcal vaccination program for older adults [44]. In countries that have an effective childhood program operating, the WHO guidelines recommend that decisions about initiating a pneumococcal vaccination program in adults should take into account the local disease burden and cost-effectiveness considerations [44]. Furthermore, emerging data on the direct and indirect clinical effects of higher valency PCVs (including PCV20) should guide discussion on the relative merits of these newer vaccines [44].
The immunogenicity of PCV20 in adults has been demonstrated in a well-designed and thorough program of clinical trials (Sect. 2), modelled on the clinical trial program that supported PCV13 licensure in adults. As demonstrated in the trials, PCV20 induced robust immune responses to all 20 S. pneumoniae serotypes covered by the vaccine (Sect. 2). PCV20 was well tolerated, with a tolerability and safety profile similar to that for PCV13 (Sect. 3). Pain at the injection site and muscle pain were the most commonly reported local reactions and systemic events; although relatively common (reported in >50% and >30% of PCV20 recipients), these events were mostly mild. In the pivotal trial, no vaccine-related SAEs were observed through 6 months of follow-up after PCV20 administration (Sect. 3) [34]. Of further interest, emerging data from two recently completed randomised phase III trials (B7471004 and B7471026) suggest that co-administration of PCV20 with a QIV or a booster dose of BNT162b2 is well tolerated (Sect. 3) and elicits robust immune responses to the relevant vaccine targets (Sect. 2.3). These two trials were conducted in subjects aged ≥ 65 years, with such patients making up a key target group for each of the vaccines [35, 36]. Furthermore, with the increased convenience from the possibility of receiving PCV20 with a QIV or BNT162b2 at the same visit, there may be the potential to increase uptake of the vaccines [35, 36].
A further potential benefit of PCV20 could be in the fight against antibiotic resistance. IPD caused by antibiotic-nonsusceptible isolates has declined dramatically following the introduction of PCVs into immunisation programs [45]. With the addition of further serotypes in PCV20 (including some of the most common antibiotic-nonsusceptible serotypes, such as 22F and 33F), the introduction of PCV20 has the potential to further reduce the incidence of IPD caused by antibiotic-nonsusceptible isolates [45]. This effect could also have benefits in terms of antibiotic stewardship by reducing the (need for or) use of antibiotics, itself a driver of antibiotic resistance.
There are some limitations to the currently available data on PCV20. Most notably, although there are strong data supporting the immunogenicity of PCV20 based on OPA assays (Sect. 2), there is no minimum threshold of protection established for OPA assays and data on the effectiveness of PCV20 in preventing pneumococcal disease are lacking. Nonetheless, as a functional assay which replicates the in vivo mechanism of antibody protection [38], the OPA assay is considered to be an acceptable surrogate marker for vaccine efficacy [39]. Furthermore, given the similarities between PCV20 and PCV13 in terms of manufacture and formulation, the demonstrated effectiveness of PCV13 in preventing vaccine-type pneumococcal CAP and IPD (including from the large, randomised, placebo-controlled CAPiTA trial [14]) is supportive of the likely effectiveness of PCV20, particularly for disease caused by the 13 S. pneumoniae serotypes common to both vaccines [25, 39]. Nonetheless, a planned confirmatory study in adults aged ≥ 65 years to describe the clinical benefit of PCV20 for the prevention of pneumonia caused by the seven new serotypes in PCV20 will be of interest [39].
A further limitation of the currently available data on PCV20 is the general lack of longer-term immunogenicity data, with most trials in the PCV20 clinical development program limited to describing immune responses at 1 month post vaccination (Sect. 2). Data from the phase II B7471002 trial showed that antibody responses against the 20 vaccine serotypes at Month 12 remained elevated from baseline, indicating persistence of the immune response elicited by vaccine [31, 40]. Furthermore, post-hoc analyses from the CAPiTA trial found that the effectiveness of PCV13 was sustained, with no substantial waning of vaccine efficacy observed over the 5-year duration of the study [14, 46]. Nonetheless, further data on the long-term persistence (and effectiveness) of the immune response elicited by PCV20 would be of interest. In addition, longer term surveillance will be required to evaluate the potential impact of further serotype replacement which could be induced by the use of PCV20, in which vaccine serotypes could be replaced by non-vaccine serotypes over time, thereby potentially eroding the benefits of the vaccine [21, 22].
Another question of interest in the post-marketing phase for PCV20 will be regarding the effectiveness of the vaccine against S. pneumoniae serotype 3. Unlike disease caused by most other S. pneumoniae serotypes covered by PCV13, there has been no substantial decline in pneumococcal disease caused by serotype 3 after the widespread introduction of PCV13 into immunisation programs [47,48,49]. This remains an area of concern, with serotype 3 not only now being responsible for a significant proportion of remaining pneumococcal disease but also appearing to often be associated with more severe disease [48,49,50,51]. Given the substantial similarities between PCV13 and PCV20, it seems likely that PCV20 may also have a less significant impact on pneumococcal disease caused by serotype 3 than that caused by other vaccine serotypes. Nonetheless, despite the more limited impact of PCV13 on serotype 3 at the population level, there is evidence that the vaccine may provide some direct protection at the individual level [52], suggesting that PCV20 (like PCV13) may still be a useful tool for reducing some of the impact of pneumococcal disease caused by serotype 3.
Finally, it should be noted that immunocompromised and immunosuppressed individuals were excluded from the clinical trials on PCV20 (Sect. 2). Based on experience with other pneumococcal vaccines, individuals with altered immunocompetence and those on immunosuppressive therapy may have reduced immune responses to PCV20 [25, 26]. Nonetheless, some clinical benefit from PCV20 could still be anticipated in immunocompromised and immunosuppressed individuals (particularly noting that these individuals are at higher risk of pneumococcal disease) [5, 43], and the use of PCV20 for individuals in immunocompromised groups should be considered on an individual basis [25, 26].
In conclusion, by expanding the coverage of disease-causing S. pneumoniae serotypes relative to other PCVs, PCV20 presents a valuable new tool with the potential to further reduce the impact of pneumococcal disease. This value is recognised in the latest ACIP recommendations, which recommend the use of either PCV20 alone or PCV15 in series with PPSV23 in select adults (based on age and risk factors) who have not previously received a PCV. Besides the additional serotype coverage of PCV20 versus PCV15, PCV20 also has the advantage of providing broad protection against pneumococcal disease in a (single-dose) single vaccine rather than the two-vaccine series of PCV15 followed by PPSV23 ≥1 year later as the other ACIP-recommended alternative.
Data Selection 20-Valent Pneumococcal Conjugate Vaccine: 137 records identified
Duplicates removed | 33 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomised trial) | 29 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomised/phase I/II trials) | 23 |
Cited immunogenicity/tolerability articles | 9 |
Cited articles not immunogenicity/tolerability | 43 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were: Prevnar 20, Prevenar 20, pneumococcal 20-valent conjugate vaccine, 20vPnC, PCV 20, 20-valent PCV, PF-06482077, NCT03828617, NCT03642847, NCT03313050. Records were limited to those in English language. Searches last updated 09 May 2022. | |
References
Drijkoningen JJ, Rohde GG. Pneumococcal infection in adults: burden of disease. Clin Microbiol Infect. 2014;20(Suppl 5):45–51.
Said MA, Johnson HL, Nonyane BA, et al. Estimating the burden of pneumococcal pneumonia among adults: a systematic review and meta-analysis of diagnostic techniques. PLoS ONE. 2013;8(4): e60273.
Wahl B, O’Brien KL, Greenbaum A, et al. Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000–15. Lancet Glob Health. 2018;6(7):e744–57.
Centers for Disease Control and Prevention. Streptococcus pneumoniae. 2022. https://www.cdc.gov/pneumococcal/clinicians/streptococcus-pneumoniae.html. Accessed 02 May 2022.
Kobayashi M, Farrar JL, Gierke R, et al. Use of 15-valent pneumococcal conjugate vaccine and 20-valent pneumococcal conjugate vaccine among U.S. adults: updated recommendations of the Advisory Committee on Immunization Practices—United States, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(4):109–17.
Matanock A, Lee G, Gierke R, et al. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged ≥65 years: updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2019;68(46):1069–75.
World Health Organization. Pneumococcal disease. 2022. https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccine-standardization/pneumococcal-disease. Accessed 02 May 2022.
World Health Organization. Pneumococcal vaccines : WHO position paper—2012. Wkly Epidemiol Rec. 2012;87(14):129–44.
World Health Organization. 23-valent pneumococcal polysaccharide vaccine—WHO position paper. Wkly Epidemiol Rec. 2008;83(42):373–84.
Tomczyk S, Bennett NM, Stoecker C, et al. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged ≥ 65 years: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2014;63(37):822–5.
Jackson LA, Gurtman A, Rice K, et al. Immunogenicity and safety of a 13-valent pneumococcal conjugate vaccine in adults 70 years of age and older previously vaccinated with 23-valent pneumococcal polysaccharide vaccine. Vaccine. 2013;31(35):3585–93.
Moore MR, Link-Gelles R, Schaffner W, et al. Effect of use of 13-valent pneumococcal conjugate vaccine in children on invasive pneumococcal disease in children and adults in the USA: analysis of multisite, population-based surveillance. Lancet Infect Dis. 2015;15(3):301–9.
van Deursen AMM, van Houten MA, Webber C, et al. The impact of the 13-valent pneumococcal conjugate vaccine on pneumococcal carriage in the Community Acquired Pneumonia immunization Trial in Adults (CAPiTA) study. Clin Infect Dis. 2018;67(1):42–9.
Bonten MJ, Huijts SM, Bolkenbaas M, et al. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N Engl J Med. 2015;372(12):1114–25.
European Medicines Agency. Synflorix (pneumococcal polysaccharide conjugate vaccine): summary of product characteristics. 2021. https://www.ema.europa.eu/en/documents/product-information/synflorix-epar-product-information_en.pdf. Accessed 02 May 2022.
Vadlamudi NK, Chen A, Marra F. Impact of the 13-valent pneumococcal conjugate vaccine among adults: a systematic review and meta-analysis. Clin Infect Dis. 2019;69(1):34–49.
Shiri T, Datta S, Madan J, et al. Indirect effects of childhood pneumococcal conjugate vaccination on invasive pneumococcal disease: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(1):e51–9.
Vyse A, Campling J, Czudek C, et al. The proportion of contemporary invasive pneumococcal disease and pneumococcal pneumonia in UK adults reflected by serotypes included in the 13-valent pneumococcal conjugate vaccine and next generation higher valency pneumococcal conjugate vaccines in development. Vaccine. 2020;38(51):8068–70.
Torres A, Menéndez R, España PP, et al. The evolution and distribution of pneumococcal serotypes in adults hospitalized with community-acquired pneumonia in Spain using a serotype-specific urinary antigen detection test: the CAPA study, 2011–2018. Clin Infect Dis. 2021;73(6):1075–85.
Isturiz R, Grant L, Gray S, et al. Expanded analysis of 20 pneumococcal serotypes associated with radiographically confirmed community-acquired pneumonia in hospitalized US adults. Clin Infect Dis. 2021;73(7):1216–22.
Ladhani SN, Collins S, Djennad A, et al. Rapid increase in non-vaccine serotypes causing invasive pneumococcal disease in England and Wales, 2000–17: a prospective national observational cohort study. Lancet Infect Dis. 2018;18(4):441–51.
Lewnard JA, Hanage WP. Making sense of differences in pneumococcal serotype replacement. Lancet Infect Dis. 2019;19(6):e213–20.
European Medicines Agency. Vaxneuvance pneumococcal polysaccharide conjugate vaccine (15-valent, adsorbed): summary of product characteristics. 2022. https://www.ema.europa.eu/en/documents/product-information/vaxneuvance-epar-product-information_en.pdf. Accessed 02 May 2022.
US FDA. VAXNEUVANCE™ (pneumococcal 15-valent conjugate vaccine): US prescribing information. 2021. https://www.fda.gov/media/150819/download. Accessed 02 May 2022.
US FDA. PREVNAR 20 (pneumococcal 20-valent conjugate vaccine), suspension for intramuscular injection: US prescribing information. 2021. https://www.fda.gov/vaccines-blood-biologics/vaccines/prevnar-20. Accessed 02 May 2022.
European Medicines Agency. Apexxnar [pneumococcal polysaccharide conjugate vaccine (20-valent, adsorbed)]: summary of product characteristics. 2022. https://www.ema.europa.eu/en/documents/product-information/apexxnar-epar-product-information_en.pdf. Accessed 17 May 2022.
Thompson A, Lamberth E, Severs J, et al. Phase 1 trial of a 20-valent pneumococcal conjugate vaccine in healthy adults. Vaccine. 2019;37(42):6201–7.
van der Linden M, Imöhl M, Perniciaro S. Limited indirect effects of an infant pneumococcal vaccination program in an aging population. PLoS ONE. 2019;14(8):1–19.
de Miguel S, Domenech M, Gonzalez-Camacho F, et al. Nationwide trends of invasive pneumococcal disease in Spain from 2009 through 2019 in children and adults during the pneumococcal conjugate vaccine era. Clin Infect Dis. 2021;73(11):e3778–87.
Janssens E, Flamaing J, Vandermeulen C, et al. The 20-valent pneumococcal conjugate vaccine (PCV20): expected added value. Acta Clin Belg. 2022. https://doi.org/10.1080/17843286.2022.2039865.
Hurley D, Griffin C, Young M Jr, et al. Safety, tolerability, and immunogenicity of a 20-valent pneumococcal conjugate vaccine (PCV20) in adults 60 to 64 years of age. Clin Infect Dis. 2021;73(7):e1489–97.
Klein NP, Peyrani P, Yacisin K, et al. A phase 3, randomized, double-blind study to evaluate the immunogenicity and safety of 3 lots of 20-valent pneumococcal conjugate vaccine in pneumococcal vaccine-naive adults 18 through 49 years of age. Vaccine. 2021;39(38):5428–35.
Fitz-Patrick D, Young M Jr, Scott DA, et al. A randomized phase 1 study of the safety and immunogenicity of 2 novel pneumococcal conjugate vaccines in healthy Japanese adults in the United States. Hum Vaccin Immunother. 2021;17(7):2249–56.
Essink B, Sabharwal C, Cannon K, et al. Pivotal phase 3 randomized clinical trial of the safety, tolerability, and immunogenicity of 20-valent pneumococcal conjugate vaccine in adults 18 years and older. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab990.
Cannon K, Cardona J, Belanger T, et al. Immunogenicity and safety of a 20-valent pneumococcal conjugate vaccine (PCV20) administered concomitantly with a quadrivalent inactivated influenza vaccine in adults ≥65 years of age [abstract and poster no. 1923]. In: 32nd ECCMID. 2022.
Fitz-Patrick D, Jennings T, Young M, et al. Safety, tolerability, and immunogenicity of a booster dose of BNT162b2 COVID-19 vaccine coadministered with 20-valent pneumococcal conjugate vaccine (PCV20) in adults 65 years of age and above [abstract and poster no. 2245]. In: 32nd ECCMID. 2022.
Cannon K, Elder C, Young M, et al. A trial to evaluate the safety and immunogenicity of a 20-valent pneumococcal conjugate vaccine in populations of adults ≥65 years of age with different prior pneumococcal vaccination. Vaccine. 2021;39(51):7494–502.
Song JY, Moseley MA, Burton RL, et al. Pneumococcal vaccine and opsonic pneumococcal antibody. J Infect Chemother. 2013;19(3):412–25.
US FDA. Pneumococcal 20-valent conjugate vaccine: BLA clinical review memorandum. 2021. https://www.fda.gov/media/150460/download. Accessed 02 May 2022.
Hurley D, Griffin C, Young M Jr, et al. Persistence of circulating antibody through 12 months following vaccination with a 20-valent pneumococcal conjugate vaccine in adults 60–64 years of age. Open Forum Infect Dis. 2020;7(Suppl 1):S639.
European Centre for Disease Prevention and Control. Pneumococcal disease: recommended vaccinations. 2022. https://vaccine-schedule.ecdc.europa.eu/Scheduler/ByDisease?SelectedDiseaseId=25&SelectedCountryIdByDisease=-1. Accessed 02 May 2022.
Castiglia P. Recommendations for pneumococcal immunization outside routine childhood immunization programs in Western Europe. Adv Ther. 2014;31(10):1011–44.
Bonnave C, Mertens D, Peetermans W, et al. Adult vaccination for pneumococcal disease: a comparison of the national guidelines in Europe. Eur J Clin Microbiol Infect Dis. 2019;38(4):785–91.
World Health Organization. Considerations for pneumococcal vaccination in older adults. Wkly Epidemiol Rec. 2021;96(23):217–28.
Bajema KL, Gierke R, Farley MM, et al. Impact of pneumococcal conjugate vaccines on antibiotic-nonsusceptible invasive pneumococcal disease in the United States. J Infect Dis. 2022. https://doi.org/10.1093/infdis/jiac154.
Patterson S, Webber C, Patton M, et al. A post hoc assessment of duration of protection in CAPiTA (Community Acquired Pneumonia immunization Trial in Adults). Trials Vaccinol. 2016;5:92–6.
Pilishvili T. Impact of PCV13 on invasive pneumococcal disease (IPD) burden and the serotype distribution in U.S. In: Advisory Committee on Immunization Practices. 2018.
Groves N, Sheppard CL, Litt D, et al. Evolution of Streptococcus pneumoniae serotype 3 in England and Wales: a major vaccine evader. Genes (Basel). 2019;10(11):845.
Bahrs C, Kesselmeier M, Kolditz M, et al. A longitudinal analysis of pneumococcal vaccine serotypes in pneumonia patients in Germany. Eur Respir J. 2022;59(2):2102432.
Grabenstein JD, Musey LK. Differences in serious clinical outcomes of infection caused by specific pneumococcal serotypes among adults. Vaccine. 2014;32(21):2399–405.
Luck JN, Tettelin H, Orihuela CJ. Sugar-coated killer: serotype 3 pneumococcal disease. Front Cell Infect Microbiol. 2020;10: 613287.
McLaughlin JM, Jiang Q, Gessner BD, et al. Pneumococcal conjugate vaccine against serotype 3 pneumococcal pneumonia in adults: a systematic review and pooled analysis. Vaccine. 2019;37(43):6310–6.
Acknowledgements
During the peer review process, the manufacturer of PCV20 was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and Conflict of interest
Matt Shirley is a salaried employee of Adis International Ltd/Springer Nature, and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent to publish, Availability of data and material, Code availability
Not applicable.
Additional information
The manuscript was reviewed by: C. Ardanuy, Department of Microbiology, Hospital Universitari de Bellvitge, University of Barcelona-IDIBELL, Barcelona, Spain; J. J. Mousa, Center for Vaccines and Immunology, Department of Infectious Diseases, University of Georgia, Athens, GA, USA; C. J. Orihuela, Department of Microbiology, The University of Alabama at Birmingham, Birmingham, AL, USA; M. W. Pletz, Institute for Infectious Diseases and Infection Control, Jena University Hospital, Jena, Germany.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shirley, M. 20-Valent Pneumococcal Conjugate Vaccine: A Review of Its Use in Adults. Drugs 82, 989–999 (2022). https://doi.org/10.1007/s40265-022-01733-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-022-01733-z