Abstract
Eosinophilic granulomatosis with polyangiitis (formerly Churg–Strauss syndrome) is a rare type of anti-neutrophil cytoplasm antibody-associated vasculitis. Nevertheless, eosinophilic granulomatosis with polyangiitis stands apart because it has features of vasculitis and eosinophilic disorders that require targeted therapies somewhat different from those used for other anti-neutrophil cytoplasm antibody-associated vasculitides. Considerable advances have been made in understanding the underlying pathophysiology of eosinophilic granulomatosis with polyangiitis that have highlighted the key role of eosinophils and opened new therapeutic opportunities. Its conventional treatment relies mainly on agents that decrease inflammation: corticosteroids and immunosuppressant adjunction for severe manifestations. New therapeutic approaches are needed for refractory disease, relapses and issues associated with corticosteroid dependence, especially for asthma manifestations. Drugs under evaluation mostly target eosinophils and B cells. Results of low-evidence-based trials suggested possible efficacies of biologicals: B-cell-blocking rituximab and anti-immunoglobulin E omalizumab. Recently, the first large-scale randomised controlled trial on eosinophilic granulomatosis with polyangiitis proved the efficacy of anti-interleukin-5 mepolizumab. That finding opens a new era in eosinophilic granulomatosis with polyangiitis management, with mepolizumab approval but also in future drug evaluations and trial designs for eosinophilic granulomatosis with polyangiitis. Additional studies are needed to determine which patients would benefit most from targeted therapies and achieve personalised treatment for patients with eosinophilic granulomatosis with polyangiitis. Herein, we review eosinophilic granulomatosis with polyangiitis characteristics and provide an overview of established and novel pharmacological agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Eosinophilic granulomatosis with polyangiitis (EGPA) is a systemic inflammatory necrotising vasculitis with multiple aetiological factors and a suspected key role of eosinophils in its pathophysiology. |
EGPA management relies on pharmacological agents chosen according to disease severity. |
Corticosteroids are the mainstay of EGPA treatment but relapses are frequent. Immunosuppressants are required for patients with poorer prognoses but are of limited efficacy for relapse prevention and chronic asthma/rhinosinusitis manifestations. |
Mepolizumab (anti-interleukin-5) is the first biological approved to treat EGPA. Several agents targeting eosinophils and B cells are being evaluated. |
1 Introduction
Eosinophilic granulomatosis with polyangiitis (EGPA, formerly Churg–Strauss syndrome), a systemic necrotising vasculitis occurring in asthmatic individuals, is classified as an anti-neutrophil cytoplasm antibody (ANCA)-associated vasculitis (AAV) [1], even though < 30% of patients are ANCA positive. This classification reflects the disease’s pathogenic heterogeneity, characterised by at least two phenotypes: one closely linked to ANCA positivity with prominent vasculitis (alveolar haemorrhage, glomerulonephritis, peripheral neuropathy) and the other with more predominant cardiac involvement [2, 3].
Conventional EGPA treatment combines corticosteroids (CS) and immunosuppressant(s) for the most severely ill [4]. Corticosteroids are always useful to control asthma and vasculitis, while immunosuppressants help obtain vasculitis remission and prevent relapses. Considering EGPA heterogeneity and its various pathogenic mechanisms, EGPA therapies could differ according to phenotype, severity and predictable outcomes. Independently of vasculitis treatment, a major issue in EGPA is controlling asthma, which usually persists after vasculitis enters remission. New therapeutic approaches for EGPA should treat the vasculitis and asthma together but also prevent asthma flares and limit the CS dependence developing in > 80% of the patients [5]. New drugs targeting EGPA pathogenic mechanisms look promising but their efficacies must be demonstrated at the different disease stages (remission induction and maintenance) and for the different phenotypes. This review summarises the pathophysiology of EGPA and details the available data on the use of both conventional treatments and novel targeted biological therapies.
2 Background
2.1 Classification
Several classification systems have been devised to differentiate vasculitis entities. Early during the last century, several vasculitides were individualised: microscopic polyangiitis (MPA) [initially named microscopic polyarteritis nodosa] [6] and granulomatosis with polyangiitis (GPA) [formerly Wegener’s granulomatosis] [7]. The American College of Rheumatology classification, based mainly on disease clinical symptoms, is valid for the identification of some vasculitides, like EGPA [8]. The 2012-revised Chapel Hill Conference Consensus Nomenclature integrates clinical symptoms and includes laboratory findings, histology and pathogenesis [1]. It classifies vasculitides into three groups according to the affected vessel size. Anti-neutrophil cytoplasm antibody-associated vasculitides belong to the necrotising small-vessel vasculitis group. Although considered an AAV, EGPA is distinct from MPA and GPA. Eosinophils are clearly the main cell implicated in EGPA, as opposed to neutrophils in GPA and MPA. Eosinophilic granulomatosis with polyangiitis shares features with other eosinophil-associated disorders and asthma in addition to vasculitis symptoms, thereby highlighting the limitation of classification and confirming Chapel Hill Conference Consensus Nomenclature validity to categorise but not diagnose vasculitides.
Genetics might have a major impact on vasculitis classification and help characterise disease phenotypes and predict outcomes. Genome-wide association studies on MPA and GPA revealed that patients’ genotypes could be clustered according to their ANCA specificity [9], and another on EGPA confirmed its heterogeneity with at least an anti-myeloperoxidase (MPO)-ANCA phenotype and the other without [10].
2.2 Epidemiology
Eosinophilic granulomatosis with polyangiitis is the least common AAV [11]. Its annual incidence, estimated in different world regions, never exceeds 2.3 cases/million inhabitants, and its prevalence is 23 cases/million inhabitants. [12]. Noteworthy, the disease may be under-recognised owing to the lack of consensual diagnostic criteria. Unlike most autoimmune diseases, EGPA has no clear sex, familial or ethnic predisposition [13].
Eosinophilic granulomatosis with polyangiitis is considered an idiopathic disease with many factors contributing to its complex pathophysiology: allergens, medications, infections and genetic predisposition. Gene studies demonstrated increased susceptibility conferred by some HLA-DR alleles [14,15,16] and interleukin (IL)-10 polymorphisms [17], highlighting the immune system’s role in its aetiopathogenesis. Environmental factor involvement as a causative or triggering agent remains unclear. Allergens are thought to be pivotal players in the disease manifestations. However, systematic testing for allergies in patients with EGPA established that less than one third had positive results for common allergens [18], suggesting that a canonical allergic process is not the only mechanism underlying EGPA’s ‘allergic phenotype’ or that the responsible allergens remain unknown. Asthma in EGPA could be more indicative of a non-allergic eosinophilic phenotype, according to current asthma-phenotype definitions. The possibility of drug-induced disease persists for leukotriene receptor anatagonists frequently used to treat asthma [19]. However, EGPA onset under those agents is likely to result from their effective CS sparing unmasking the autoimmune disorder [20].
2.3 Pathophysiology
Eosinophilic granulomatosis with polyangiitis immunopathogenesis is complex and its elucidation hampered by the lack of a suitable animal model. The currently accepted disease mechanism is largely inferred from clinical studies that revealed the pivotal role of eosinophils found in blood and/or tissues at all EGPA stages. However, it remains unclear whether eosinophils are responsible for disease initiation or play a secondary role as effectors of organ damage. Several eosinophil-regulating cytokines are overexpressed during EGPA: IL-4, IL-13 and especially IL-5 [21,22,23]. Those cytokines are thought to be synthesised by mostly activated CD4 + T-helper (Th) cells and define the Th2 phenotype [24, 25]. Another major source of Th2 cytokines, notably IL-5, are the type-2 innate lymphoid cells located in epithelia, e.g. the respiratory epithelium [26]. The role of type-2 innate lymphoid cells in tissue eosinophil recruitment has been established in allergic diseases but not specifically in EGPA. By secreting IL-25, activated eosinophils further amplify the Th2 response [27]. The Th2 phenotype is usually associated with B-cell activation and antibody secretion, especially immunoglobulin G (IgG) and immunoglobulin E (IgE). B-cell mobilisation [28] and ANCA secretion (in ~ 30%) [2, 3, 5] have been demonstrated in patients with EGPA. Eotaxin-3, a chemokine regulating eosinophil recruitment, and CCL-17, a Th2 chemokine, are elevated during EGPA and sometimes associated with disease activity [29, 30]. Those soluble mediators might activate and attract eosinophils to tissues, where they would induce organ-specific pathological processes via different pathways: adherence to the endothelium, tissue infiltration and granuloma formation, ultimately leading to small-vessel occlusion and ischaemia. Eosinophils can also directly affect organs with their granule contents, able to induce oxidative burst, fibrosis, thrombosis and enhanced inflammatory signalling [31].
This EGPA paradigm of an eosinophil-centred Th2 role should be nuanced because other studies obtained conflicting results for CCL-17 and eotaxin-3 [32, 33]. Similarly, the importance of other cytokines and Th1 and/or Th17 profile(s) has been emphasised [25, 34]. Other actors also warrant being mentioned, e.g. ANCA-targeted neutrophils. Anti-neutrophil cytoplasm antibodies recognise mainly MPO or proteinase-3 in neutrophil granules, and by activating neutrophils can trigger vasculitis [35]. Pertinently, ANCA do not recognise eosinophil antigens [36]. Eosinophilic granulomatosis with polyangiitis immunopathogenesis is schematised in Fig. 1, showing the targets of emerging therapeutics.
Immunopathogenesis of eosinophilic granulomatosis with polyangiitis and the main targets of emerging biological agents. Initial ill-defined causative and triggering agents induce a predominant T-helper type 2 (Th2) inflammation process. Classical Th2 cells and tissue-resident innate lymphoid cells type 2 (ILC2s) are the main producers of Th2 cytokines [interleukin (IL)-5, IL-4 and IL-13] responsible for eosinophil (Eo) activation and tissue recruitment. Activated Eos induce tissue lesions in many ways, further enhanced by other cell types [mast cells and/or basophils, T-helper type 1 (Th1) and T-helper type 17 (Th17) T cells, B cells] and humoral mediators (antibodies, cytokines). ANCA anti-neutrophil cytoplasm antibody, IFNα interferon-α, IFNγ interferon-γ, IgE immunoglobulin E, IgG immunoglobulin G, IL-5Rα IL-5 receptor-α, MPO myeloperoxidase
2.4 Clinical, Biological and Pathological Manifestations
Eosinophilic granulomatosis with polyangiitis may occur at any age but usually begins in the fifth or sixth decade [5, 37]. Traditionally, prodromal, eosinophilic and small-vessel vasculitis, chronological clinical phases are recognised [38]. Prodromal phase manifestations, mainly late-onset asthma, rhinosinusitis and polyposis, may last several years or decades, and individuals who will develop EGPA cannot be foreseen. The eosinophilic phase, characterised by increased blood and tissue eosinophilia, is responsible for organ injury. The vasculitic process and granuloma formation further affect organ impairment. Although EGPA can affect any organ, certain organ systems are preferentially affected. The predominant post-prodromal-phase manifestations and organ involvements are: asthma (> 90%), rhino-sinusitis (50–90%), general symptoms (80%), lung infiltrate(s) (40–60%), mononeuritis multiplex (50%), skin (40–50%), arthralgias and myalgias (30–50%), heart (20–50%), gastrointestinal tract (20–30%) and kidneys (20%) [4, 5, 37].
The clinical distinction between eosinophilic and vasculitis phenotypes is supported by observed patient segregation according to ANCA status. Anti-neutrophil cytoplasm antibody-positive patients (~ 30%) are more prone to peripheral neuropathy, purpura, renal involvement and biopsy-proven vasculitis, whereas ANCA-negative patients (70%) have more frequent cardiac manifestations [2, 3, 5, 39]. First an immunofluorescence assay screens for ANCA, then an enzyme-linked immunosorbent assay determines their specificity. A recently reached consensus proposes that an enzyme-linked immunosorbent assay surpasses immunofluorescence for detection [40]. Eosinophilic granulomatosis with polyangiitis is usually associated with a perinuclear immunofluorescence labelling pattern and MPO specificity.
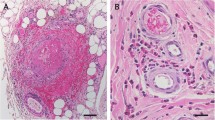
Laboratory investigations, including non-specific inflammation biomarkers, supporting EGPA diagnosis are blood eosinophilia (usually a count > 1500/mm3 and/or > 10%), high IgE titres and ANCA positivity [38, 41], but they are not reliable relapse predictors or disease-activity biomarkers [42]. Eosinophil infiltrates, small-sized-vessel vasculitis and/or eosinophil-rich granulomas seen in involved-organ biopsies also contribute to the diagnosis [43]. Other biological and radiological investigations should be performed to seek frequent organ involvement(s) that condition treatment strategy [44].
2.5 Prognosis and Outcomes
Adequately treated EGPA has a fair prognosis. A retrospective study on 348 patients showed that, with a median follow-up at 50 months, only 11.7% died [5]. The outcomes of patients with EGPA differ according to clinical manifestations (like cardiac involvement), relapse rate, asthma persistence and its relationship with vasculitis flare, and adverse events (AEs), mainly attributable to CS. In a retrospective series [4], 91% of patients entered remission, with cardiac and/or gastrointestinal involvement responsible for poor outcomes. Identifying patients with poor-prognosis factors also has the advantage of defining those without such factors whose regimens can be less intensive [45, 46]. Clinicians’ therapeutic objectives are to obtain disease remission, prevent relapses and minimise long-term drug numbers and doses to improve long-term prognosis and limit AE frequency and severity. No correlation/association could be established between initial intensive induction and fewer long-term relapses or AEs. However, a meta-analysis of our prospective EGPA trials [47] showed that overall survival was good, reaching 90% at 7 years, regardless of baseline severity; only age ≥ 65 years was associated with a higher risk of death during follow-up. The relapse risk was higher for patients with anti-MPO ANCA and lower for those with > 3000 eosinophils/mm3. Sequelae, predominantly chronic asthma and peripheral neuropathy, remained frequent.
3 Treatment
A treatment approach is proposed in Fig. 2, according to data from studies reviewed hereafter.
3.1 Corticosteroids
At present, EGPA therapy is based on CS, with the most severely ill patients also given immunosuppressants. Corticosteroids have the major advantages of rapid efficacy against vasculitis and asthma flares, inducing clinical remission, and eosinophilia normalisation within several days. However, long-term CS use can cause major AEs, especially when they cannot be tapered because of uncontrolled asthma and persistent or new-onset EGPA extrapulmonary manifestations.
Immunosuppressants, usually cyclophosphamide in conjunction with CS, are commonly prescribed to treat severe EGPA, as defined by the Five-Factor Score (FFS) [48]. The FFS comprises five items scoring 1 point each if present: age > 65 years, cardiac involvement, gastrointestinal tract involvement, creatininemia ≥ 150 μmol/L and/or absence of ear, nose and throat (ENT) manifestations [46]. In the final FFS version (2009), the positive impact of ENT manifestations on prognosis was demonstrated for patients with GPA and patients with EGPA mainly. However, clinicians using the FFS should be aware that the presence of ENT manifestations does not account for a negative point, and that only the absence of ENT signs should be taken into consideration to calculate the score. This is important to stress to avoid inappropriate use of the FFS because ENT manifestations are frequent in EGPA. In severe EGPA cases (FFS ≥ 1), a combination of CS and cyclophosphamide is used to induce remission, usually reached in 3–6 months. A cyclophosphamide regime is followed by azathioprine or methotrexate maintenance therapy given for 12–18 months or longer if clinical (asthma or extrapulmonary symptoms) or biological manifestations (eosinophilia) persist.
However, no consensus has been reached on the optimal regime for patients without poor prognosis factors (FFS = 0). We showed that CS alone could suffice, reserving the addition of immunosuppressants for CS failure [49]. The EGPA Consensus Task Force recommendations [44] stated that immunosuppressants are not compulsory for patients with FFS = 0 but a more recent recommendation, largely based on an expert consensus with many coauthors of the former [50], preferred treating all patients with CS and immunosuppressants. A randomised controlled trial (RCT) on systemic necrotising vasculitides without poor prognosis factors, which included a majority of patients with EGPA, compared CS and azathioprine or placebo, and found that azathioprine was unable to induce remissions or prevent relapses more frequently than CS alone [51]. That study showed that “light” immunosuppressants, like azathioprine, failed to achieve CS sparing, which is a major objective for patients requiring long-term CS, at least to control asthma.
3.2 Place of Immunosuppressants
Cyclophosphamide is the most frequently prescribed immunosuppressant to control the most severe vasculitides. No other drug has yet been demonstrated to have greater efficacy than cyclophosphamide in this setting. The prospective RCT on mepolizumab [52] and case series on other biotherapies did not address severe vasculitides. The promising results of only one prospective open study successfully evaluating mepolizumab for acute EGPA warrant confirmation [53]. Therefore, cyclophosphamide should remain the remission-induction agent of choice for the most severe EGPA forms. Our group initiated several prospective RCTs to evaluate rituximab for induction-and-maintenance therapy [54, 55], and mepolizumab for EGPA remission-induction.
Although a consensus exists for cyclophosphamide’s indication, that is not the case for other immunosuppressants. After induction, patients with AAV usually received azathioprine or methotrexate. Azathioprine for GPA was shown to be as effective as cyclophosphamide to maintain remission but rituximab remission-induction has since challenged the efficacy of azathioprine [56, 57]. In a prospective study [58], azathioprine did not maintain EGPA remission. Similar conclusions can be drawn for methotrexate [59] and mycophenolate mofetil [60]. However, no prospective study has specifically addressed EGPA and our therapeutic options mainly reflect the results of other prospective studies.
3.3 Plasma Exchanges
No trial has specifically examined plasma exchange (PE) indications for EGPA. However, based on experience with other AAVs, PEs could be helpful for patients with pneumo-renal syndrome, i.e. extracapillary glomerulonephritis causing severe renal insufficiency and/or severe alveolar haemorrhage. Short-term PE efficacy was demonstrated in patients with creatininemia ≥ 500 μmol/L [61] and evaluation is ongoing for patients with an estimated glomerular filtration rate < 50 mL/min [62]. Plasma exchanges are also prescribed for severe alveolar haemorrhage, based on their efficacy against anti-glomerular basement membrane vasculitis, but remain unconfirmed by a prospective study. The prognosis is good for isolated mild alveolar haemorrhage and PEs are not indicated [63].
3.4 Intravenous Immunoglobulins
Intravenous immunoglobulins has rarely been used to treat vasculitis but they warrant a place in its treatment. Intravenous immunoglobulins effectively induce vasculitis remission or reverse its relapses [64, 65]. Intravenous immunoglobulins prescribed alone have a short-term efficacy [66]. Without prospective or retrospective studies exclusively on EGPA, we speculate that intravenous immunoglobulins could be effective only against ANCA-positive disease, but it has never been clinically proven. At present, intravenous immunoglobulins have a niche indication, requiring case-by-case evaluation.
3.5 Targeted Therapies
The need for new therapeutic approaches to control the inflammatory disease burden of relapsing disease and assure CS sparing was previously highlighted. The emergence of biotherapies targeting molecules and receptors involved in EGPA aetiopathogenesis has revolutionised disease management. Currently, eosinophil-targeted therapies are the strongest scientifically based biologicals to treat EGPA. Below, we mainly focus on the molecules with the most promising results that mediate eosinophil (anti-IL-5, anti-IgE) and B-cell (rituximab) interventions (Table 1).
3.5.1 Rituximab
Rituximab (MabThera® or Rituxan®), an anti-CD20 IgG1 mouse–human chimeric antibody, selectively depletes mature and memory B lymphocytes. Originally developed to treat B-cell lymphomas, rituximab generated good responses in various autoimmune disorders [67], for which it was given because its induction of B-cell apoptosis hypothetically led to autoreactive antibody-production abrogation. Because plasma cells, the final stage of B-cell differentiation, lack CD20 and thus, are not affected by rituximab and can persist for years or decades in bone marrow, this hypothesis is only partially supported. Moreover, the demonstrated clinical efficacy of rituximab contrasts with persistent autoantibodies in some autoimmune disorders [67]. Obviously, the mechanisms underlying the efficacy of rituximab in autoimmune disorders remain poorly elucidated. Because B cells have pleiotropic functions, B-cell-targeting therapies might function by affecting antigen presentation, T-cell activation or cytokine production.
In AAV, rituximab non-inferiority to cyclophosphamide as an induction agent was proven [56, 57, 68] and its remission maintenance is superior to azathioprine [58]. Consequently, rituximab has revolutionised the standard of care for AAV and is now recommended as first-line therapy for severe GPA and MPA management only because RCTs did not include EGPA. According to the European Medicines Agency and US Food and Drug Administration licencing, the recommended remission-induction dose is 375 mg/m2 body-surface area infused once a week for 4 weeks. Empirically, a double dose every fortnight (two infusions) has also been proposed and seems to be as effective [69].
Information on the potential clinical benefits of rituximab for patients with EGPA is currently restricted to low-evidence-based, open-label, uncontrolled studies and case reports [70,71,72,73,74,75,76,77,78]. Globally, those studies’ results support rituximab use for severe refractory/relapsing EGPA. In the largest retrospective series [77], 36/41 (88%) showed clinical improvement at 12 months: 49% remission and 39% partial responses. This efficacy encompassed asthma/ENT symptoms and vasculitis-induced organ impairment. Interestingly, rituximab appeared more effective for ANCA-positive patients, but ANCA negativity did not exclude potential benefit. Notably, the CS dose was halved but only two patients achieved complete weaning. Its main AEs were allergic reactions during infusion, infections and a trend towards lower IgG levels. Thus, the safety profile was the same as that for other AAVs [56, 57, 68], except for more frequent infusion reactions. The latter may be an obstacle for patients with disease-facilitated allergic reactions, potentially causing severe bronchospasms [72]. A retrospective 3-year follow-up study [78], comparing rituximab with a conventional cyclophosphamide induction regime between two groups of 14 age- and sex-matched patients, showed rituximab to be as effective as cyclophosphamide, even for patients with prior cyclophosphamide failure. No severe AE was reported. Four rituximab-treated patients developed asymptomatic hypogammaglobulinemia.
Taken together, all those observations indicate a potential benefit of rituximab in EGPA, but controlled study confirmation is needed. Indeed, an ongoing phase III RCT is assessing rituximab induction [54] and another RCT is planned for maintenance therapy [55]. Despite the limited evidence, rituximab was recently recommended by an expert consensus to treat patients with EGPA with renal involvement or refractory disease [44]. Future elucidation of B-cell roles in EGPA may provide new targeted therapeutic opportunities, e.g. to block B cells responsible for long-lasting antibody secretion.
3.5.2 Mepolizumab (Anti-Interleukin-5)
Mepolizumab (Nucala®) is a humanised monoclonal IgG1 antibody that binds free IL-5, which is the major specific factor for eosinophil growth, differentiation and survival. Interleukin-5 exerts its effects via a heterodimeric receptor, whose α-subunit (IL-5-Rα) is specific to IL-5. The β-subunit, shared with other cytokine receptors (IL-3, granulocyte-macrophage colony-stimulating factor), is responsible for signal transduction. IL-5 receptor-α is predominantly expressed on human eosinophils [79]. Mepolizumab inhibits IL-5 signalling in eosinophils, thereby preventing their activation, recruitment and tissue accumulation, as demonstrated in asthma with fewer blood and sputum eosinophilia [80].
Mepolizumab has been investigated in several eosinophilic disorders such as asthma, rhinosinusitis, hypereosinophilic syndrome and atopic dermatitis. In 2015, the Food and Drug Administration and European Medicines Agency approved mepolizumab as add-on therapy to manage severe eosinophilic asthma [81]. In RCTs, it better controlled disease (exacerbations), slightly improved lung function test results and had a glucocorticoid-sparing effect [82,83,84]. No safety concerns were raised. The recommended mepolizumab dose for this indication is 100 mg injected subcutaneously once every 4 weeks.
The supposed key role played by eosinophils, and the elevated IL-5 levels in EGPA [22] make mepolizumab a logical candidate. A potential mepolizumab benefit in EGPA was derived from small open-label pilot studies and a case report [53, 85,86,87]. Those findings supported conducting a large multinational RCT on relapsing/refractory EGPA [52], in which patients received subcutaneous mepolizumab (300 mg) injection every 4 weeks or placebo (68/group) for 1 year. Patients with EGPA were representative of those requiring new therapeutic options, with previous relapses/difficult-to-treat disease, all taking CS and ~ 50% taking immunosuppressants. The protocol-defined primary efficacy endpoints reached significance: comparing mepolizumab with placebo, respectively, 28 vs. 3% had > 24 weeks of accrued remission; 32 vs. 3% were in remission at weeks 36 and 48, with 44 vs. 7% of the patients benefiting from CS dose tapering receiving < 5 mg of prednisone or equivalent. Although the mepolizumab-group’s 1-year relapse rate was 50% lower, 56% of them still relapsed, with asthma, ENT symptoms exacerbation and/or vasculitis manifestations. Remission was less likely for patients with baseline eosinophil counts < 150/mm3. Mepolizumab also met multiple secondary outcomes (time to remission, lower circulating eosinophil counts, Asthma Control Questionnaire 6-Item version score, rhinosinusitis 22-item Sinonasal Outcome Test score), but lung function test results did not improve, unlike previous studies on eosinophilic asthma [81]. Only more frequent systemic reactions to infusion marred its safety profile. The most common AEs were headache, nasopharyngitis, arthralgias, sinusitis and upper respiratory tract infection. These AEs and their frequency were similar in the placebo group.
The first completed RCT conducted on EGPA probably constitutes a milestone in its treatment evaluation and management [52]. Mepolizumab was effective in ~ 50% of the participants, leading to Food and Drug Administration approval in December 2017. Although those findings underscore the major mediating role of eosinophils in EGPA pathophysiology, some questions persist. Why was mepolizumab ineffective in ~ 50% of the patients? How do we identify future non-responders at baseline? Is mepolizumab more effective against specific EGPA phenotypes, e.g. ANCA negative vs. ANCA positive. Choosing 300 mg, which is three times the recommended asthma dose, was based on observations made in severe asthma but no specific dose evaluation was undertaken for EGPA, with severe eosinophilia. Because patients with life-threatening manifestations were excluded, their risk/benefit balance remains unknown, as does the efficacy of mepolizumab against specific vasculitis-related symptoms because remission criteria combined vasculitis control and asthma/sinusitis manifestations that are not always easily distinguished from vasculitis relapse. Prolongation of the first RCT should help resolve the question of optimal mepolizumab duration [88]. After successfully treating asthma, other anti-IL-5 agents are being tested in phase II trials on EGPA: reslizumab [89] and IL-5-Rα-targeting benralizumab [90].
3.5.3 Omalizumab (Anti-Immunoglobulin E)
Omalizumab (Xolair®), a humanised monoclonal IgG antibody, targets the Fc fragment of free circulating, but not membrane-bound, IgE [91]. Its binding prevents interaction with specific receptor FcεRI on basophils and mast cells, thereby inhibiting their degranulation in response to allergen exposure and blocking the allergic cascade. Long-term omalizumab use also induces FcεRI downregulation, eventually diminishing eosinophil tissue infiltration through still unelucidated mechanisms. In RCTs, omalizumab was proven effective and safe as add-on therapy for severe persistent allergic asthma and chronic spontaneous urticaria [92, 93]. Omalizumab is injected subcutaneously, its dosage and frequency (once or twice per month) varying according to the patient’s weight and IgE levels.
The impact of omalizumab on allergic asthma and eosinophilia has suggested its potential in patients with EGPA, particularly those with uncontrolled asthma. As of early 2018, information on omalizumab treatment of EGPA remains limited to case reports with < 30 patients [94,95,96,97,98,99,100,101]. It was almost always started to counter severe CS-dependent asthma with hypereosinophilia, rarely for resistant rhinosinusitis. Very few patients had active non-severe extrapulmonary vasculitis features, e.g. skin or musculoskeletal disorders [94, 99]. Although anti-IgE omalizumab effectively controlled ‘allergic’ symptoms (asthma-exacerbation rate and airway obstruction) for most patients, two patients from the largest series had severe asthma exacerbations mandating discontinuation [94]. Although patients generally tolerated omalizumab well, three developed EGPA flares [94, 98]. Similarly, at least ten patients given omalizumab for isolated asthma were subsequently diagnosed with EGPA [102,103,104,105]. Like the leukotriene receptor anatagonist controversy, whether this sequence represents a causal relationship or coincidental revelation of smouldering EGPA during CS weaning is unclear. Pertinently, those reports indicate a potential omalizumab benefit for patients with EGPA with severe asthma or rhinosinusitis, whereas the impact on vasculitis was not remarkable. No RCT testing omalizumab in patients with EGPA is currently ongoing and its place in treating EGPA is undetermined.
3.5.4 Other Targeted Drugs
3.5.4.1 Interferon-α
Interferon-α is a cytokine with pleiotropic effects on immune cells, notably interferon-α can decrease blood eosinophilia, block IL-5 secretion in vitro and attenuate a skewed Th2 profile [22, 106, 107]. On this basis, interferon-α has been tested in a small number of patients as reported in case series and small prospective open-label studies [108,109,110,111], and also in an uncontrolled retrospective study of 30 patients followed for > 24 months [112]. Even if some remission-induction success was reported, long-term follow-up indicated high relapse rates and numerous AEs, e.g. depression and neuropathy. Therefore, in 2015, the EGPA Consensus Task Force advocated its use only as second- or third-line therapy in relapsing/resistant cases [44].
3.5.4.2 Anti-Tumour Necrosis Factor-α
In-vitro studies and animal models implicated tumour necrosis factor-α in AAV pathophysiology [113], thereby suggesting clinical benefits with tumour necrosis factor-α blockers. However, no benefit for GPA patients was found in a small-scale open-label study with infliximab [114] and a large RCT with etanercept [115]. Potential benefit was reported for four EGPA patient cases [116, 117]. Based on those findings, further studies do not seem warranted. Tumour necrosis factor-α-blocking agents should be avoided in EGPA, and AAV in general.
3.6 Associated Measures
Beyond medications for the systemic manifestations detailed herein, other disease management measures should be considered. Conventional asthma and rhinosinusitis treatments should also be prescribed [118, 119]. If needed for asthma, oral leukotriene receptor anatagonists can be prescribed with close monitoring given the reported hypothetical risk of EGPA relapse [119]. Patients should be encouraged to stop smoking [44, 118]. Despite some flares after desensitisation or vaccinations [120] and because of lung involvement and frequent treatment-induced immunosuppression, vaccination against influenza and pneumococci is strongly recommended. The risk/benefit ratio favours immunisation, except during an EGPA flare. Co-trimoxazole prophylaxis against Pneumocystis jirovecii pneumonia is recommended in the case of severe immunosuppression, e.g. the use of cyclophosphamide, rituximab or high-dose CS [121]. Although Pneumocystis jirovecii pneumonia is not the most common cause of infection during EGPA, and other AAVs, it is the only infection for which the use of chemoprophylaxis has proven efficacy in primary vasculitis and can thus be encouraged [122]. These measures are important because infections are responsible for high morbidity/mortality [123].
4 Perspectives
In our opinion, the following future EGPA therapeutic strategies warrant consideration. Current assessments of treatment response are global with activity scores such as the Birmingham Vasculitis Activity Score, which combines vasculitis, respiratory and ENT symptoms. It creates ambiguities in analysing treatment efficacy for each type of manifestation and would thus require clarification. Notably, differentiating between clinical vasculitis and asthma flares can be difficult, generating uncertainty in determining treatment efficacy and diagnosing flares. Hence, new practical tools must be devised to improve disease-activity evaluations and achieve patient-centred therapy.
Several drugs evaluated for other eosinophilic disorders (asthma, chronic rhinosinusitis, hypereosinophilic syndrome) were deemed beneficial and are potential candidates to treat EGPA. Other than reslizumab or benralizumab (both in ongoing phase II trials), drugs targeting CCR3 or other Th2 cytokines (e.g. IL-4 and/or IL-13 with dupilumab, pitrakinra, lebrikizumab) can modulate eosinophil biology [124].
Future approaches can consider the usefulness of combining drugs. Recent RCT results show that some vasculitides cannot be treated without CS. We think combined-drug regimens will achieve better disease control and minimisation of AEs beyond targeted biologicals replacing ‘old drugs’. A major question persists: what is the indication for combining biotherapies for selected patients? Because pathogenic mechanisms differ from one EGPA subgroup to another and within a given subgroup, mepolizumab plus rituximab sequentially or simultaneously could be prescribed for some patients. Such aersonalised management can only be established through new prospective trials.
References
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheum. 2013;65:1–11.
Sinico RA, Di Toma L, Maggiore U, Bottero P, Radice A, Tosoni C, et al. Prevalence and clinical significance of antineutrophil cytoplasmic antibodies in Churg-Strauss syndrome. Arthritis Rheum. 2005;52:2926–35.
Sablé-Fourtassou R, Cohen P, Mahr A, Pagnoux C, Mouthon L, Jayne D, et al. Antineutrophil cytoplasmic antibodies and the Churg-Strauss syndrome. Ann Intern Med. 2005;143:632–8.
Guillevin L, Cohen P, Gayraud M, Lhote F, Jarrousse B, Casassus P. Churg-Strauss syndrome: clinical study and long-term follow-up of 96 patients. Medicine (Baltimore). 1999;78:26–37.
Comarmond C, Pagnoux C, Khellaf M, Cordier J-F, Hamidou M, Viallard J-F, et al. Eosinophilic granulomatosis with polyangiitis (Churg–Strauss): clinical characteristics and long-term followup of the 383 patients enrolled in the French Vasculitis Study Group cohort. Arthritis Rheum. 2013;65:270–81.
Wohlwill F. Über die nur mikroskopisch erkennbare Form der Periarteriitis nodosa. Virchows Arch Path Anat. 1923;246:377–411.
Wegener F. Über generalisierte, septische Gefässerkrankungen. Verhandlungen der Deutschen Pathologischen Gesselschaft. 1936;29:202–10.
Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990;33:1094–100.
Lyons PA, Rayner TF, Trivedi S, Holle JU, Watts RA, Jayne DRW, et al. Genetically distinct subsets within ANCA-associated vasculitis. N Engl J Med. 2012;367:214–23.
Smith K. Genetic studies in ANCA-associated vasculitis point to a new, practical disease classification based on autoantibody specificity. Presented at the 18th International Vasculitis and ANCA Workshop, Tokyo, Japan. Rheumatology (Oxford). 2017;56(Suppl. S3):iii3–4.
Watts RA, Mahr A, Mohammad AJ, Gatenby P, Basu N, Flores-Suárez LF. Classification, epidemiology and clinical subgrouping of antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis. Nephrol Dial Transplant. 2015;30(Suppl. 1):i14–22.
Watts RA, Lane SE, Scott DG, Koldingsnes W, Nossent H, Gonzalez-Gay MA, et al. Epidemiology of vasculitis in Europe. Ann Rheum Dis. 2001;60:1156–7.
Watts RA, Scott DGI, Lane SE. Epidemiology of Wegener’s granulomatosis, microscopic polyangiitis, and Churg–Strauss syndrome. Cleve Clin J Med. 2002;69(Suppl. 2):SII84–6.
Stassen PM, Cohen-Tervaert JW, Lems SPM, Hepkema BG, Kallenberg CGM, Stegeman CA. HLA-DR4, DR13(6) and the ancestral haplotype A1B8DR3 are associated with ANCA-associated vasculitis and Wegener’s granulomatosis. Rheumatology (Oxford). 2009;48:622–5.
Vaglio A, Martorana D, Maggiore U, Grasselli C, Zanetti A, Pesci A, et al. HLA-DRB4 as a genetic risk factor for Churg-Strauss syndrome. Arthritis Rheum. 2007;56:3159–66.
Wieczorek S, Hellmich B, Gross WL, Epplen JT, et al. Associations of Churg-Strauss syndrome with the HLA-DRB1 locus, and relationship to the genetics of antineutrophil cytoplasmic antibody-associated vasculitides: comment on the article by Vaglio. Arthritis Rheum. 2008;58:329–30.
Wieczorek S, Hellmich B, Arning L, Moosig F, Lamprecht P, Gross WL, et al. Functionally relevant variations of the interleukin-10 gene associated with antineutrophil cytoplasmic antibody-negative Churg-Strauss syndrome, but not with Wegener’s granulomatosis. Arthritis Rheum. 2008;58:1839–48.
Bottero P, Bonini M, Vecchio F, Grittini A, Patruno GM, Colombo B, et al. The common allergens in the Churg-Strauss syndrome. Allergy. 2007;62:1288–94.
Wechsler ME, Garpestad E, Flier SR, Kocher O, Weiland DA, Polito AJ, et al. Pulmonary infiltrates, eosinophilia, and cardiomyopathy following corticosteroid withdrawal in patients with asthma receiving zafirlukast. JAMA. 1998;279:455–7.
Hauser T, Mahr A, Metzler C, Coste J, Sommerstein R, Gross WL, et al. The leucotriene receptor antagonist montelukast and the risk of Churg-Strauss syndrome: a case-crossover study. Thorax. 2008;63:677–82.
Kiene M, Csernok E, Müller A, Metzler C, Trabandt A, Gross WL. Elevated interleukin-4 and interleukin-13 production by T cell lines from patients with Churg-Strauss syndrome. Arthritis Rheum. 2001;44:469–73.
Hellmich B, Csernok E, Gross WL. Proinflammatory cytokines and autoimmunity in Churg-Strauss syndrome. Ann N Y Acad Sci. 2005;1051:121–31.
Jakiela B, Szczeklik W, Plutecka H, Sokolowska B, Mastalerz L, Sanak M, et al. Increased production of IL-5 and dominant Th2-type response in airways of Churg-Strauss syndrome patients. Rheumatology (Oxford). 2012;51:1887–93.
Fagin U, Csernok E, Müller A, Pitann S, Fazio J, Krause K, et al. Distinct proteinase 3-induced cytokine patterns in Wegener’s granulomatosis, Churg-Strauss syndrome, and healthy controls. Clin Exp Rheumatol. 2011;29(1 Suppl. 64):S57–62.
Jakiela B, Sanak M, Szczeklik W, Sokolowska B, Plutecka H, Mastalerz L, et al. Both Th2 and Th17 responses are involved in the pathogenesis of Churg-Strauss syndrome. Clin Exp Rheumatol. 2011;29(1 Suppl. 64):S23–34.
Symowski C, Voehringer D. Interactions between innate lymphoid cells and cells of the innate and adaptive immune system. Front Immunol. 2017;8:1422.
Terrier B, Bièche I, Maisonobe T, Laurendeau I, Rosenzwajg M, Kahn J-E, et al. Interleukin-25: a cytokine linking eosinophils and adaptive immunity in Churg-Strauss syndrome. Blood. 2010;116:4523–31.
Tsurikisawa N, Saito H, Oshikata C, Tsuburai T, Akiyama K. Decreases in the numbers of peripheral blood regulatory T cells, and increases in the levels of memory and activated B cells, in patients with active eosinophilic granulomatosis and polyangiitis. J Clin Immunol. 2013;33:965–76.
Dallos T, Heiland GR, Strehl J, Karonitsch T, Gross WL, Moosig F, et al. CCL17/thymus and activation-related chemokine in Churg-Strauss syndrome. Arthritis Rheum. 2010;62:3496–503.
Zwerina J, Bach C, Martorana D, Jatzwauk M, Hegasy G, Moosig F, et al. Eotaxin-3 in Churg-Strauss syndrome: a clinical and immunogenetic study. Rheumatology (Oxford). 2011;50:1823–7.
Khoury P, Grayson PC, Klion AD. Eosinophils in vasculitis: characteristics and roles in pathogenesis. Nat Rev Rheumatol. 2014;10:474–83.
Khoury P, Zagallo P, Talar-Williams C, Santos CS, Dinerman E, Holland NC, et al. Serum biomarkers are similar in Churg-Strauss syndrome and hypereosinophilic syndrome. Allergy. 2012;67:1149–56.
Dejaco C, Oppl B, Monach P, Cuthbertson D, Carette S, Hoffman G, et al. Serum biomarkers in patients with relapsing eosinophilic granulomatosis with polyangiitis (Churg–Strauss). PLoS One. 2015;10:e0121737.
Saito H, Tsurikisawa N, Tsuburai T, Oshikata C, Akiyama K. Cytokine production profile of CD4+ T cells from patients with active Churg-Strauss syndrome tends toward Th17. Int Arch Allergy Immunol. 2009;149(Suppl. 1):61–5.
Jennette JC, Falk RJ. New insight into the pathogenesis of vasculitis associated with antineutrophil cytoplasmic autoantibodies. Curr Opin Rheumatol. 2008;20:55–60.
Sullivan S, Salapow MA, Breen R, Broide DH. Eosinophil peroxidase differs from neutrophil myeloperoxidase in its ability to bind antineutrophil cytoplasmic antibodies reactive with myeloperoxidase. Int Arch Allergy Immunol. 1994;105:150–4.
Moosig F, Bremer JP, Hellmich B, Holle JU, Holl-Ulrich K, Laudien M, et al. A vasculitis centre based management strategy leads to improved outcome in eosinophilic granulomatosis and polyangiitis (Churg–Strauss, EGPA): monocentric experiences in 150 patients. Ann Rheum Dis. 2013;72:1011–7.
Lanham JG, Elkon KB, Pusey CD, Hughes GR. Systemic vasculitis with asthma and eosinophilia: a clinical approach to the Churg-Strauss syndrome. Medicine (Baltimore). 1984;63:65–81.
Cottin V, Bel E, Bottero P, Dalhoff K, Humbert M, Lazor R, et al. Revisiting the systemic vasculitis in eosinophilic granulomatosis with polyangiitis (Churg–Strauss): a study of 157 patients by the Groupe d’Etudes et de Recherche sur les Maladies Orphelines Pulmonaires and the European Respiratory Society Taskforce on Eosinophilic Granulomatosis with Polyangiitis (Churg–Strauss). Autoimmun Rev. 2017;16:1–9.
Bossuyt X, Cohen Tervaert J-W, Arimura Y, Blockmans D, Flores-Suárez LF, Guillevin L, et al. Position paper: revised 2017 international consensus on testing of ANCAs in granulomatosis with polyangiitis and microscopic polyangiitis. Nat Rev Rheumatol. 2017;13:683–92.
Mouthon L, Dunogue B, Guillevin L. Diagnosis and classification of eosinophilic granulomatosis with polyangiitis (formerly named Churg-Strauss syndrome). J Autoimmun. 2014;48–49:99–103.
Grayson PC, Monach PA, Pagnoux C, Cuthbertson D, Carette S, Hoffman GS, et al. Value of commonly measured laboratory tests as biomarkers of disease activity and predictors of relapse in eosinophilic granulomatosis with polyangiitis. Rheumatology (Oxford). 2015;54:1351–9.
Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol. 1951;27:277–301.
Groh M, Pagnoux C, Baldini C, Bel E, Bottero P, Cottin V, et al. Eosinophilic Granulomatosis with Polyangiitis (Churg–Strauss) (EGPA) Consensus Task Force recommendations for evaluation and management. Eur J Intern Med. 2015;26:545–53.
Guillevin L, Lhote F, Gayraud M, Cohen P, Jarrousse B, Lortholary O, et al. Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome: a prospective study in 342 patients. Medicine (Baltimore). 1996;75:17–28.
Guillevin L, Pagnoux C, Seror R, Mahr A, Mouthon L, Le Toumelin P, et al. The Five-Factor Score revisited: assessment of prognoses of systemic necrotizing vasculitides based on the French Vasculitis Study Group (FVSG) cohort. Medicine (Baltimore). 2011;90:19–27.
Samson M, Puéchal X, Devilliers H, Ribi C, Cohen P, Stern M, et al. Long-term outcomes of 118 patients with eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome) enrolled in two prospective trials. J Autoimmun. 2013;43:60–9.
Cohen P, Pagnoux C, Mahr A, Arène J-P, Mouthon L, Le Guern V, et al. Churg-Strauss syndrome with poor-prognosis factors: a prospective multicenter trial comparing glucocorticoids and six or twelve cyclophosphamide pulses in forty-eight patients. Arthritis Rheum. 2007;57:686–93.
Ribi C, Cohen P, Pagnoux C, Mahr A, Arène J-P, Lauque D, et al. Treatment of Churg-Strauss syndrome without poor-prognosis factors: a multicenter, prospective, randomized, open-label study of seventy-two patients. Arthritis Rheum. 2008;58:586–94.
Yates M, Watts RA, Bajema IM, Cid MC, Crestani B, Hauser T, et al. EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis. 2016;75:1583–94.
Puéchal X, Pagnoux C, Baron G, Quémeneur T, Néel A, Agard C, et al. Adding azathioprine to remission-induction glucocorticoids for eosinophilic granulomatosis with polyangiitis (Churg–Strauss), microscopic polyangiitis, or polyarteritis nodosa without poor prognosis factors: a randomized, controlled trial. Arthritis Rheumatol. 2017;69:2175–86.
Wechsler ME, Akuthota P, Jayne D, Khoury P, Klion A, Langford CA, et al. Mepolizumab or placebo for eosinophilic granulomatosis with polyangiitis. N Engl J Med. 2017;376:1921–32.
Moosig F, Gross WL, Herrmann K, Bremer JP, Hellmich B. Targeting interleukin-5 in refractory and relapsing Churg-Strauss syndrome. Ann Intern Med. 2011;155:341–3.
US National Library of Medicine. Rituximab in eosinophilic granulomatosis with polyangiitis. ClinicalTrials.gov identifier: NCT02807103. https://clinicaltrials.gov/ct2/show/NCT02807103. Accessed 20 Dec 2017.
US National Library of Medicine. Maintenance of remission with rituximab versus azathioprine for newly-diagnosed or relapsing eosinophilic granulomatosis with polyangiitis. ClinicalTrials.gov identifier: NCT03164473. https://clinicaltrials.gov/ct2/show/NCT03164473. Accessed 20 Dec 2017.
Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363:221–32.
Specks U, Merkel PA, Seo P, Spiera R, Langford CA, Hoffman GS, et al. Efficacy of remission-induction regimens for ANCA-associated vasculitis. N Engl J Med. 2013;369:417–27.
Guillevin L, Pagnoux C, Karras A, Khouatra C, Aumaître O, Cohen P, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014;371:1771–80.
Pagnoux C, Mahr A, Hamidou MA, Boffa J-J, Ruivard M, Ducroix J-P, et al. Azathioprine or methotrexate maintenance for ANCA-associated vasculitis. N Engl J Med. 2008;359:2790–803.
Hiemstra TF, Walsh M, Mahr A, Savage CO, de Groot K, Harper L, et al. Mycophenolate mofetil vs azathioprine for remission maintenance in antineutrophil cytoplasmic antibody-associated vasculitis: a randomized controlled trial. JAMA. 2010;304:2381–8.
Jayne DRW, Gaskin G, Rasmussen N, Abramowicz D, Ferrario F, Guillevin L, et al. Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. J Am Soc Nephrol. 2007;18:2180–8.
US National Library of Medicine. Plasma exchange and glucocorticoids for treatment of anti-neutrophil cytoplasm antibody (ANCA)-associated vasculitis (PEXIVAS). ClinicalTrials.gov identifier: NCT00987389. https://clinicaltrials.gov/ct2/show/NCT00987389. Accessed 12 Jan 2018.
Kostianovsky A, Hauser T, Pagnoux C, Cohen P, Daugas E, Mouthon L, et al. Alveolar haemorrhage in ANCA-associated vasculitides: 80 patients’ features and prognostic factors. Clin Exp Rheumatol. 2012;30(1 Suppl. 70):S77–82.
Martinez V, Cohen P, Pagnoux C, Vinzio S, Mahr A, Mouthon L, et al. Intravenous immunoglobulins for relapses of systemic vasculitides associated with antineutrophil cytoplasmic autoantibodies: results of a multicenter, prospective, open-label study of twenty-two patients. Arthritis Rheum. 2008;58:308–17.
Jayne DR, Chapel H, Adu D, Misbah S, O’Donoghue D, Scott D, et al. Intravenous immunoglobulin for ANCA-associated systemic vasculitis with persistent disease activity. QJM. 2000;93:433–9.
Jayne DR, Lockwood CM. Intravenous immunoglobulin as sole therapy for systemic vasculitis. Br J Rheumatol. 1996;35:1150–3.
Faurschou M, Jayne DRW. Anti-B cell antibody therapies for inflammatory rheumatic diseases. Annu Rev Med. 2014;65:263–78.
Jones RB, Tervaert JWC, Hauser T, Luqmani R, Morgan MD, Peh CA, et al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med. 2010;363:211–20.
Charles P, Néel A, Tieulié N, Hot A, Pugnet G, Decaux O, et al. Rituximab for induction and maintenance treatment of ANCA-associated vasculitides: a multicentre retrospective study on 80 patients. Rheumatology (Oxford). 2014;53:532–9.
Koukoulaki M, Smith KGC, Jayne DRW. Rituximab in Churg-Strauss syndrome. Ann Rheum Dis. 2006;65:557–9.
Pepper RJ, Fabre MA, Pavesio C, Gaskin G, Jones RB, Jayne D, et al. Rituximab is effective in the treatment of refractory Churg-Strauss syndrome and is associated with diminished T-cell interleukin-5 production. Rheumatology (Oxford). 2008;47:1104–5.
Bouldouyre M-A, Cohen P, Guillevin L. Severe bronchospasm associated with rituximab for refractory Churg-Strauss syndrome. Ann Rheum Dis. 2009;68:606.
Dønvik KK, Omdal R. Churg-Strauss syndrome successfully treated with rituximab. Rheumatol Int. 2011;31:89–91.
Cartin-Ceba R, Keogh KA, Specks U, Sethi S, Fervenza FC. Rituximab for the treatment of Churg-Strauss syndrome with renal involvement. Nephrol Dial Transplant. 2011;26:2865–71.
Thiel J, Hässler F, Salzer U, Voll RE, Venhoff N. Rituximab in the treatment of refractory or relapsing eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome). Arthritis Res Ther. 2013;15:R133.
Novikov P, Moiseev S, Smitienko I, Zagvozdkina E. Rituximab as induction therapy in relapsing eosinophilic granulomatosis with polyangiitis: a report of 6 cases. Joint Bone Spine. 2016;83:81–4.
Mohammad AJ, Hot A, Arndt F, Moosig F, Guerry M-J, Amudala N, et al. Rituximab for the treatment of eosinophilic granulomatosis with polyangiitis (Churg–Strauss). Ann Rheum Dis. 2016;75:396–401.
Thiel J, Troilo A, Salzer U, Schleyer T, Halmschlag K, Rizzi M, et al. Rituximab as induction therapy in eosinophilic granulomatosis with polyangiitis refractory to conventional immunosuppressive treatment: a 36-month follow-up analysis. J Allergy Clin Immunol Pract. 2017;5:1556–63.
Yanagibashi T, Satoh M, Nagai Y, Koike M, Takatsu K. Allergic diseases: from bench to clinic-contribution of the discovery of interleukin-5. Cytokine. 2017;98:59–70.
Leckie MJ, ten Brinke A, Khan J, Diamant Z, O’Connor BJ, Walls CM, et al. Effects of an interleukin-5 blocking monoclonal antibody on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet. 2000;356:2144–8.
Keating GM. Mepolizumab: first global approval. Drugs. 2015;75:2163–9.
Ortega HG, Liu MC, Pavord ID, Brusselle GG, FitzGerald JM, Chetta A, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371:1198–207.
Bel EH, Wenzel SE, Thompson PJ, Prazma CM, Keene ON, Yancey SW, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med. 2014;371:1189–97.
Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380:651–9.
Kahn J-E, Grandpeix-Guyodo C, Marroun I, Catherinot E, Mellot F, Roufosse F, et al. Sustained response to mepolizumab in refractory Churg-Strauss syndrome. J Allergy Clin Immunol. 2010;125:267–70.
Kim S, Marigowda G, Oren E, Israel E, Wechsler ME. Mepolizumab as a steroid-sparing treatment option in patients with Churg-Strauss syndrome. J Allergy Clin Immunol. 2010;125:1336–43.
Herrmann K, Gross WL, Moosig F. Extended follow-up after stopping mepolizumab in relapsing/refractory Churg-Strauss syndrome. Clin Exp Rheumatol. 2012;30(1 Suppl. 70):S62–5.
US National Library of Medicine. Long-term access program (LAP) of mepolizumab for subjects who participated in study MEA115921. ClinicalTrials.gov identifier: NCT03298061. https://clinicaltrials.gov/ct2/show/NCT03298061. Accessed 20 Dec 2017.
US National Library of Medicine. Reslizumab in the treatment of eosinophilic granulomatosis with polyangiitis (EGPA) study. ClinicalTrials.gov identifier: NCT02947945. Available from: https://clinicaltrials.gov/ct2/show/NCT02947945. Accessed 20 Dec 2017.
US National Library of Medicine. Benralizumab in the treatment of eosinophilic granulomatosis with polyangiitis (EGPA) study. ClinicalTrials.gov identifier: NCT03010436. https://clinicaltrials.gov/ct2/show/NCT03010436. Accessed 20 Dec 2017.
Soresi S, Togias A. Mechanisms of action of anti-immunoglobulin E therapy. Allergy Asthma Proc. 2006;27(2 Suppl. 1):S15–23.
McKeage K. Omalizumab: a review of its use in patients with severe persistent allergic asthma. Drugs. 2013;73:1197–212.
McCormack PL. Omalizumab: a review of its use in patients with chronic pontaneous urticaria. Drugs. 2014;74:1693–9.
Jachiet M, Samson M, Cottin V, Kahn J-E, Le Guenno G, Bonniaud P, et al. Anti-IgE monoclonal antibody (omalizumab) in refractory and relapsing eosinophilic granulomatosis with polyangiitis (Churg–Strauss): data on seventeen patients. Arthitis Rheumatol. 2016;68:2274–82.
Detoraki A, Capua LD, Varricchi G, Genovese A, Marone G, Spadaro G. Omalizumab in patients with eosinophilic granulomatosis with polyangiitis: a 36-month follow-up study. J Asthma. 2016;53:201–6.
Giavina-Bianchi P, Giavina-Bianchi M, Agondi R, Kalil J. Administration of anti-IgE to a Churg-Strauss syndrome patient. Int Arch Allergy Immunol. 2007;144:155–8.
Pabst S, Tiyerili V, Grohé C. Apparent response to anti-IgE therapy in two patients with refractory “forme fruste” of Churg-Strauss syndrome. Thorax. 2008;63:747–8.
Lau EMT, Cooper W, Bye PT, Yan K. Difficult asthma and Churg–Strauss-like syndrome: a cautionary tale. Respirology. 2011;16:180–1.
Iglesias E, Camacho Lovillo M, Delgado Pecellín I, Lirola Cruz MJ, Falcón Neyra MD, Salazar Quero JC, et al. Successful management of Churg-Strauss syndrome using omalizumab as adjuvant immunomodulatory therapy: first documented pediatric case. Pediatr Pulmonol. 2014;49:E78–81.
Graziani A, Quercia O, Girelli F, Martelli A, Mirici Cappa F, Stefanini GF. Omalizumab treatment in patient with severe asthma and eosinophilic granulomatosis with polyangiitis: a case report. Eur Ann Allergy Clin Immunol. 2014;46:226–8.
Aguirre-Valencia D, Posso-Osorio I, Bravo J-C, Bonilla-Abadía F, Tobón GJ, Cañas CA. Sequential rituximab and omalizumab for the treatment of eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome). Clin Rheumatol. 2017;36:2159–62.
Nazir S, Tachamo N, Fareedy SB, Khan MS, Lohani S. Omalizumab-associated eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome). Ann Allergy Asthma Immunol. 2017;118:372–4.
Bekçibaşı M, Barutçu S, Çelen MK, Dayan S, Hoşoğlu S. Churg-Strauss syndrome occurring during omalizumab treatment. Eur J Rheumatol. 2015;2:129–30.
Szwarc D, Veillon F, Moser T, Averous G, De Blay F, Riehm S. Churg-Strauss syndrome under omalizumab treatment: a rare visceral manifestation [in French]. J Radiol. 2009;90:1737–9.
Wechsler ME, Wong DA, Miller MK, Lawrence-Miyasaki L. Churg-Strauss syndrome in patients treated with omalizumab. Chest. 2009;136:507–18.
Schandené L, Del Prete GF, Cogan E, Stordeur P, Crusiaux A, Kennes B, et al. Recombinant interferon-alpha selectively inhibits the production of interleukin-5 by human CD4 + T cells. J Clin Invest. 1996;97:309–15.
Shibuya H, Hirohata S. Differential effects of IFN-alpha on the expression of various TH2 cytokines in human CD4+ T cells. J Allergy Clin Immunol. 2005;116:205–12.
Tatsis E, Schnabel A, Gross WL. Interferon-alpha treatment of four patients with the Churg-Strauss syndrome. Ann Intern Med. 1998;129:370–4.
Lesens O, Hansmann Y, Nerson J, Pasquali J, Gasser B, Wihlm J, et al. Severe Churg-Strauss syndrome with mediastinal lymphadenopathy treated with interferon therapy. Eur J Intern Med. 2002;13:458.
Simon H-U, Seelbach H, Ehmann R, Schmitz M. Clinical and immunological effects of low-dose IFN-alpha treatment in patients with corticosteroid-resistant asthma. Allergy. 2003;58:1250–5.
Metzler C, Csernok E, Gross WL, Hellmich B. Interferon-alpha for maintenance of remission in Churg-Strauss syndrome: a long-term observational study. Clin Exp Rheumatol. 2010;28:24–30.
Seeliger B, Förster M, Happe J, Forberg T, Moeser A, Neumann T, et al. Interferon-α for induction and maintenance of remission in eosinophilic granulomatosis with polyangiitis: a single-center retrospective observational cohort study. J Rheumatol. 2017;44:806–14.
Feldmann M, Pusey CD. Is there a role for TNF-alpha in anti-neutrophil cytoplasmic antibody-associated vasculitis? Lessons from other chronic inflammatory diseases. J Am Soc Nephrol. 2006;17:1243–52.
Morgan MD, Drayson MT, Savage COS, Harper L. Addition of infliximab to standard therapy for ANCA-associated vasculitis. Nephron Clin Pract. 2011;117:c89–97.
Wegener’s Granulomatosis Etanercept Trial. (WGET) Research Group. Etanercept plus standard therapy for Wegener’s granulomatosis. N Engl J Med. 2005;352:351–61.
Arbach O, Gross WL, Gause A. Treatment of refractory Churg-Strauss syndrome (CSS) by TNF-alpha blockade. Immunobiology. 2002;206:496–501.
Tiliakos A, Shaia S, Hostoffer R, Kent L. The use of infliximab in a patient with steroid-dependent Churg-Strauss syndrome. J Clin Rheumatol. 2004;10:96–7.
Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43:343–73.
Beswick DM, Gray ST, Smith TL. Pharmacological management of chronic rhinosinusitis: current and evolving treatments. Drugs. 2017;77:1713–21.
Guillevin L, Guittard T, Blétry O, Godeau P, Rosenthal P. Systemic necrotizing angiitis with asthma: causes and precipitating factors in 43 cases. Lung. 1987;165:165–72.
Park JW, Curtis JR, Moon J, Song YW, Kim S, Lee EB. Prophylactic effect of trimethoprim-sulfamethoxazole for Pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high-dose glucocorticoids. Ann Rheum Dis. 2018;77(5):644–9.
Moosig F, Holle JU, Gross WL. Value of anti-infective chemoprophylaxis in primary systemic vasculitis: what is the evidence? Arthritis Res Ther. 2009;11:253.
Samson M, Puéchal X, Mouthon L, Devilliers H, Cohen P, Bienvenu B, et al. Microscopic polyangiitis and non-HBV polyarteritis nodosa with poor-prognosis factors: 10-year results of the prospective CHUSPAN trial. Clin Exp Rheumatol. 2017;35(Suppl. 103):176–84.
Sriaroon P, Ballow M. Biological modulators in eosinophilic diseases. Clin Rev Allergy Immunol. 2016;50:252–72.
Acknowledgements
The authors thank Benjamin Terrier for critical appraisal of the manuscript and figure.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the preparation of this article.
Conflict of interest
Loïc Raffray received financial support for attending symposia from Amgen in 2017 and AbbVie in 2016. Loïc Guillevin has no conflicts of interest directly relevant to the content of this article.
Rights and permissions
About this article
Cite this article
Raffray, L., Guillevin, L. Treatment of Eosinophilic Granulomatosis with Polyangiitis: A Review. Drugs 78, 809–821 (2018). https://doi.org/10.1007/s40265-018-0920-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-0920-8