Abstract
Kidney transplant is the preferred treatment of pediatric end-stage renal disease. One of the most challenging aspects of pediatric kidney transplant is the prevention and treatment of antibody-mediated rejection (ABMR), which is one of the main causes of graft dysfunction and early graft loss. Most challenges are similar to those faced in adult kidney transplants; however, factors unique to the pediatric realm include naivety of the immune system and the small number of studies and randomized controlled trials available when considering pharmacological treatment options. Here, we present a case of ABMR in a pediatric patient and a review of the pathophysiology, diagnosis, and management of ABMR. ABMR in pediatric kidney transplant continues to be a frustrating condition to treat because (1) there still remain many unidentified potential antigens leading to ABMR, (2) children and adults are at different stages of their immune system development, and, thus, (3) the full pathophysiology of alloimmunity is still not completely understood, and (4) the efficacy and safety of treatment in adults may not be directly translated to children. As we continue to gain a better understanding towards the precise alloimmune mechanism that drives a particular ABMR, we can also improve pharmacotherapeutic choices. With continued research, they will become more precise in treating a particular mechanism versus using a broad scope of immunosuppression such as steroids. However, there is much more to be uncovered, such as identifying more non-human leukocyte antigens and their role in alloimmunity, determining the exact mechanism of adults achieving complete operational tolerance, and understanding the difference between pediatric and adult transplant recipients. Making strides towards a better understanding of these mechanisms will lead to continued efficacy and safety in treatment of pediatric ABMR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Antibody-mediated rejection (ABMR) continues to be a difficult-to-treat complication of kidney transplantation. |
Non human leukocyte antigen (nHLA) antibodies should also be considered for recurrent episodes of ABMR. |
Age-related differences in immunity and thus alloimmunity could contribute to variable responses to treatment. |
1 Introduction
Kidney transplant is the preferred treatment of end-stage renal disease (ESRD) in pediatric patients. Despite the advancements in pediatric kidney transplant, challenges remain in the area of maintaining long-term stable graft function and avoiding rejection. One of these challenges is the prevention and treatment of antibody-mediated rejection (ABMR), which continues to be the largest risk factor for graft dysfunction and loss [1–3]. ABMR occurs when there is deterioration in graft function associated with the development of alloreactive antibodies or donor-specific antibodies (DSAs) and characteristic histological changes on biopsy. For the most part, the challenges that exist in the pediatric population are similar to the adult population in that sensitization, development of de novo DSAs, and non-adherence to post-transplant immunosuppression regimens pose risks towards the development of ABMR. Additional challenges that exist in the pediatric population are associated with the naivety of their immune system and the fact that they will most likely require more than one graft in their lifetime. Preventive measures such as adequate and timely monitoring of alloantibodies and adequate maintenance immunosuppression are taken; however, even with strict adherence, the development of ABMR still persists as we lack sufficiently sensitive non-invasive monitoring tools to accurately measure the alloimmune response and subtle graft inflammation [4].
Though this review focuses on the management of ABMR in the pediatric population, the majority of our treatment experience comes from the management of ABMR in adult populations. This review does not focus on the variations in the immune response based on age, as they in themselves do not directly impact the management of ABMR, but it is important to mention some salient differences in the maturation of the immune response over time. Immaturity of the newborn immune system leads to a ‘physiological immunodeficiency’ that encompasses all arms of the host response as reflected by the increased susceptibility of young children to infections by both viral and bacterial pathogens. Differences in innate immunity involve variations in toll-like receptor-dependent [5], and dendritic cell immune function in infancy [6–8], and androgen and estrogen alterations in puberty affect Th1/Th2 balance [9–12]. The humoral immune system remains relatively underdeveloped [13], with the neonate initially being almost entirely dependent upon passively acquired maternal antibody. Age-specific variations in the immune response can continue to play a role in late childhood, as the capacity of mononuclear cells to synthesize interleukin (IL)-12 is still below adult levels at 12 years of age [14, 15]. The inherent Epstein–Barr virus (EBV) and cytomegalovirus (CMV) seronegativity in most children at time of transplant makes them more susceptible to post-transplant CMV infection, and disease is deleterious to graft function and rejection [16]. This also contributes to an increased risk of post-transplant lymphoproliferative disorder (PTLD) in the younger population [17], specifically when the burden of immunosuppression increases due to the treatment of T-cell-mediated rejection and ABMR. Immunosuppression protocols have now been tailored towards the pediatric populations to extend the use of antiviral agents [16] and to minimize the use of maintenance steroids [16, 18], which reduce the risk of viral replication and bone and cardiovascular morbidity.
We also present an illustrative case of ABMR in a pediatric patient in order to highlight the complexities of the pathogenesis, diagnosis, and current treatment options for ABMR of the kidney transplant in the pediatric population.
2 Literature Search Methods
Literature review was performed in PubMed using the following terms alone or in combination: pediatric, transplant, transplantation, renal, antibody mediated rejection, treatment. In addition, a search of the National Institutes of Health clinical trial database was performed for pharmaceuticals mentioned in this review.
4 Pathophysiology
ABMR, also known as humoral rejection, involves T cells, B cells, antibody formation, and the activation of complement. It can be classified into three groups: hyperacute (onset: seconds to days), acute [onset: days (early) to years (late)], or chronic (onset: months to years). Regardless of its classification, it involves the presence of alloantibodies directed towards antigens originating from the donor allograft, e.g., DSAs. They can be pre-formed or have formed de novo post-transplant. Pre-formed alloreactive antibodies lead to sensitization [19], which plays a large role in ABMR. Factors most relevant in pediatrics that contribute to sensitization include blood transfusions, prior transplants, and infections (bacterial and viral). Pregnancy is also a risk factor; however, it is less relevant in pediatrics. Risk factors that lead to formation of de novo antibodies include infection, usually concurrent with a decrease in immunosuppression, and non-adherence with the post-transplant immunosuppression regimen. These factors increase the risk for development of ABMR. Recently, it has been demonstrated that a previous episode of cell-mediated rejection predisposes to formation of de novo antibodies in unsensitized patients [20].
Presence of an allograft, in the absence of adequate immunosuppression, will permit for activation of a humoral-mediated response via antibodies directly binding to the allograft antigen or by alloantigen presentation by circulating antigen-presenting cells (APCs). Germinal centers have been found within the kidney [21] where APCs can present antigen and activate CD4+ effector T cells. CD4+ T cells interact with B cells via binding of their T-cell receptor to major histocompatibility complex (MHC)-I. Co-stimulatory signals are delivered via CTLA4 (CD152) or CD28 and CD40L on the T cells to the B7 (CD80/86) complex and CD40 on B cells. These co-stimulatory signals (CD28-B7 complex and CD40L-CD40) are required for IL-2-induced proliferation and differentiation of B cells into memory B cells and plasma cells, which secrete the DSAs (Fig. 1). Lack of the CD28 signal results in cell death. The CTLA4-B7 signal results in down-regulation of T-cell activity. Once the humoral response is activated, this leads to cellular infiltrates within the kidney and its vasculature, activation of complement, and graft destruction. If there is complement fixation, there is complement end product (C4d) deposition. A complement-independent mechanism of ABMR also exists as evidenced by a lack of C4d deposition in patients with ABMR [14]; however, it is the presence of complement-activating antibodies that is predictive of graft loss [22]. It is thought that the renal endothelial tissue can also directly activate T cells and thus B cells for antibody production.
Humoral immune pathway and targets of pharmacological treatments used in antibody-mediated rejection. Abs antibodies, BCR B-cell receptor, CTLA cytotoxic T-lymphocyte-associated protein, IL interleukin, IVIG intravenous immunoglobulin, MAC membrane attack complex, MHC major histocompatibility complex, mTOR mammalian target of rapamycin, TCR T-cell receptor
Conventionally, the most relevant DSAs were those formed against HLA; however, it is now known that non-HLA (nHLA) antibodies are also important in the context of ABMR. However, current routine testing for DSAs is rudimentary and only tests for HLA at six loci. Unfortunately, in the case presented, she had both pre-formed and de novo HLA antibodies and due to the weakly positive nature of her pre-formed DSAs at only one HLA locus, removal by plasmapheresis was waived. In hindsight, this weakly positive result was indeed significant, but in addition, her prompt onset of rejection may have been due to other pre-formed DSAs and/or non-HLA antibodies since she developed her second episode of rejection within 2 months of transplant.
4.1 Human Leukocyte Antigen (HLA) Antibodies
DSAs that contribute to ABMR have specificity for HLA. Currently, the HLA antibodies for which we test are directed towards MHC class I (HLA‐A, B, C) and MHC class II (HLA‐DR, DP, DQ).
4.2 Non-HLA Antibodies
The importance of nHLA antibodies in alloimmunity became evident when antibodies against endothelial antigens were identified as the culprit in hyperacute rejection [23–27] and the unexpected occurrence of rejection in HLA-matched donors and recipients [28]. In an ABO incompatible transplant, the ABO blood group antigens are the most common causes of rejection; however, in ABO-compatible transplants, other nHLA antigens and antibodies have been implicated. They include collagen type IV and VI, vimentin, myosin, protein kinase C zeta (PKCζ), MHC I-related chain A (MICA) [29], angiotensin II type I receptor (AT1R) [30], endothelial-1 type A receptors [30], and anti-endothelial antibodies (AECA) [16]. While HLA and ABO antibodies are most implicated in acute ABMR, it is postulated that nHLA antibodies currently may play a larger role in chronic ABMR [31]. AT1R antibodies have been associated with chronic ABMR [32]. AECA and MICA have been found to be up-regulated in patients who are undergoing renal transplant rejection [33]. In addition, MICA antibodies have been associated with an increased frequency of graft loss, especially if found in conjunction with anti-HLA antibodies [34, 35]. Endothelial-1 type A receptor (ETAR) antibodies were also studied in renal transplant patients and although there was no clear association with acute rejection, it was associated with poorer graft function as defined by higher serum creatinine levels when compared with patients who were anti-ETAR negative. However, an increased incidence of acute rejection was not observed on biopsy, therefore the significance of the presence of these antibodies in an ABMR is not clear, but it is possible they are associated with chronic ABMR. We have shown that nHLA antibodies such as those formed against PKCζ [36] and angiotensinogen [32] can play a critical role in steroid-resistant rejection and the hypertension of chronic kidney disease. With improved strategies to prevent hyperacute rejection, the association with nHLA antibodies and rejection has shifted towards a more chronic process; however, they still continue to play a role in acute rejection. A recent study by our group identified novel antigenic targets [endoglin, epidermal growth factor (EGF)-like repeats and discoidin I-like domains 3, intercellular adhesion molecule 4, and FMS-like tyrosine kinase-3 ligand], which were relevant to the development of acute ABMR as evidenced by a positive endothelial positive cross-match [37]. In addition, upregulation of nHLA proteins in acute rejection in transplant [38] have been described; it would be important to know whether these proteins serve as alloantigens.
4.3 Age
The age of the recipient may affect the development of ABMR. B-cell subsets change with age, thus affecting the B-cell repertoire and level of antibody production. It has been shown that the pediatric B-cell repertoire contains more naïve cells than memory B cells, while the memory compartment dominates in the adult B cell repertoire as evidenced by less immunoglobulin D in adults. The naivety in pediatrics is due to the lack of exposure to many antigens, including EBV and CMV, and has advantages and disadvantages. They may either be able to induce a level of tolerance if they still possess an intact thymus or create an entire subset of memory cells that are reactive to the newly transplanted organ. In contrast, adults have fewer B cells to respond to new antigens, but have a larger memory cell population [39–42], thus increasing their chance of being sensitized but decreasing their ability to form new antibodies against new antigens, which may explain the ability of some adult transplant patients to achieve operational tolerance. Age also affects de novo antibody formation. Pediatric patients are more likely to form de novo antibodies within the first 2 years of transplant [3] compared with adults who have a rate of de novo antibody formation ranging from 1 to 10 years, with a majority in the 5–10 years range [22, 43]. However, the incidence of de novo antibody formation in the pediatric population has been shown by one study to be around 6 % [3], whereas in the adult population it can be up to 30 %. This variation in timing and incidence may underlie the immune mechanism at play (memory vs. new), and it may be advantageous to be mindful of the nature of the origin of the antibodies when choosing an agent for treatment.
The development of ABMR is affected by factors that include age, sensitization, infection, and level of immunosuppression at induction and maintenance. An additional risk is receiving an ABO-incompatible transplant; however, in the USA, ABO-incompatible transplants are not performed in the pediatric population.
5 Diagnosis
5.1 Clinical and Histological Diagnosis
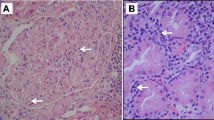
Diagnosis of acute ABMR involves the presence of acute graft dysfunction, as represented by elevated creatinine and decreased GFR, which prompts a diagnostic biopsy of the allograft and serological testing for DSAs. Progression from acute to chronic is evident with development of proteinuria and hypertension with a slow decline in graft function. Histological evidence of acute and chronic ABMR in the kidney transplant is based on the presence of tissue damage, microvascular inflammation, and evidence of complement activity that fulfill the Banff criteria as well as serological evidence of DSAs. The Banff criteria for ABMR were first published in 2003 and recently updated in 2013 [44, 45]. Table 3 presents a summary of the Banff 2013 update. The most notable update is the addition of acute AMBR type 2, which now does not require the presence of C4d staining of the peritubular capillaries [45] if vascular and microvascular injury in the absence of C4d staining is present with serological evidence of DSAs and graft dysfunction [46]. Histological findings of transplant glomerulopathy and moderate inflammation with presence of plasma cells distinguishes a chronic process from an acute process.
5.2 Serological Diagnosis
Serological testing for DSAs are most commonly carried out using solid-phase detection methods with single antigen beads (SABs, Luminex) for anti-HLA antibodies. The use of Luminex beads has shifted from the use of the complement fixation assays such as the complement-dependent cytotoxicity (CDC) method to C1q and C3d assays. The CDC method is less sensitive and is being abandoned due to evidence that not all non-complement-fixing DSAs are insignificant. However, the C1q assay, in addition to being more sensitive than the CDC, may have value in that the presence of de novo antibodies that are C1q-positive HLA class I antibodies may be predictive of ABMR and the development of glomerulopathy and carry a poor prognosis [47, 48]. Most recently developed is the C3d complement-binding assay than may be more sensitive at predicting graft loss than the C1q assay [49].
The disadvantages of relying on these methods include that, in addition to the lack of consensus over the years in regards to the histological changes that make up ABMR and that DSA detection is only limited to six HLAs, it is also well established that once serum creatinine is elevated, injury to the kidney has already taken place. The treatment for ABMR was often foregone due to an absence of C4d staining; however, it is now evident that ABMR can be present without C4d deposition [33]. In addition, treating a rejection after a rise in creatinine becomes an attempt to reverse the rejection in order to salvage an already damaged graft. This is why the presence of DSAs in association with graft dysfunction also carries a poor prognosis for the graft [50]. In addition, protocol biopsies, conducted at set intervals post-transplant, have uncovered the phenomenon of subclinical rejection, which is detection of rejection on biopsy prior to the rise of creatinine and can occur in up to 10 % of kidney transplants [51, 52]. Although advances have been made in treating ABMR at an earlier time point and preventing it in sensitized patients via desensitization protocols, we can do better by targeting treatment towards preventing antibody formation and the onset of ABMR and thus preventing damage to the graft. However, with our current methods, early diagnosis of ABMR is difficult; thus, the discovery of biomarkers has become integral.
5.3 Molecular Diagnosis
Biomarkers, originating from blood or urine, can serve as molecular ‘signatures’ for rejection and are quickly being discovered. The ability to diagnose rejection at a molecular level from a blood or urine specimen is beneficial because it allows for non-invasive diagnosis and risk stratification of rejection without the traumatic biopsy of an organ that is already undergoing the trauma of rejection. Recently, studies have described patterns of gene expression [53, 54] and microarray analysis [55–57], urine proteomics [38], and a constitution of both molecular and clinical markers specific to acute rejection [58, 59] in solid organ transplants, including kidney transplants. Some of these studies [52, 59] have led to the development of the kidney Solid Organ Response Test [60], which can accurately diagnose acute kidney rejection with a peripheral blood sample. These developments confirm that a non-invasive molecular signature for ABMR in the kidney exists and, most importantly, can predate the rise in creatinine and histological changes [54]. In addition, genomic differences also exist in DSA-positive transplant patients who develop rejection compared with DSA-positive transplant patients who do not [61]. Once these are well developed, they will serve as valuable guides for immunomodulation and determining the effectiveness of treatment without having to re-biopsy post-treatment, and will allow for earlier initiation of treatment for ABMR and serve as a tool for treatment decisions to avoid unnecessary exposure to aggressive immunosuppression. However, continued biomarker discovery is needed, especially in differentiating between cellular-mediated, ABMR, or mixed rejection. Thus, until a well-developed superior method of noninvasive diagnosis and/or prediction of transplant rejection can also differentiate acute versus chronic as well as ABMR versus cellular-mediated rejection, we continue to rely on our current methods of diagnosis.
6 Treatment
Treatment for all types of ABMR target (1) the elimination of circulating allograft antibodies, (2) immunomodulation, and/or (3) the deactivation/inhibition of complement. The co-occurrence of DSAs and decreased graft function represents a poor prognosis for the graft, and abrupt removal of DSAs improves prognosis [43]; thus, removal of antibodies is often the first-line treatment of acute ABMR. However, removal alone is inadequate and thus arise the challenges in treating acute and chronic ABMR. These are the same challenges seen in the adult population and include resistance to steroid treatment and non-responsiveness to standard treatment, as evidenced by frequent repeat episodes. The main drawback to selecting therapy for pediatrics is that efficacy is based on adult studies and, as previously mentioned, age affects immune mechanisms and thus may dictate efficacy. Until recently, randomized controlled trials have been scarce, and treatment selection was often based on small single-center studies or case reports. Treatment strategy remains non-specific, especially in pediatrics. This is due to the lack of clinical trials and the limited number of studies on newer agents for pediatric use. The most available and widely used agents are broad-based immunosuppression, which is essentially analogous to throwing the kitchen sink at recurrent episodes (plasmapheresis, IVIG, steroids, and rituximab).
6.1 Acute and Sub-Acute
In pediatrics, studies involve new applications for old drugs or drugs that have been used to treat other inflammatory diseases, and treatment has been tailored to try to better target different aspects of the antibody rejection pathway to achieve better outcomes. Here, we present a summary of the different modalities and drugs available, different combinations of treatments applied, and a summary of some, mostly adult and some pediatric, studies available for first-time and recurrent episodes of acute ABMR (Table 4).
6.1.1 Removal of Circulating Anti-Allograft Antibodies
Plasmapheresis or therapeutic plasma exchange (TPE) is the most common initial treatment for acute ABMR. This process requires a large centrally placed catheter and removes large molecular-weight proteins, including alloantibodies, from the blood. The patient’s plasma is removed and replaced with either 5 % albumin or fresh frozen plasma (FFP) at different ratios. For the treatment of ABMR, FFP is used to replace lost protective antibodies and clotting factors, since many rounds are required for clearance of DSAs. In pediatrics, the most common ratio used (1.5 exchange) allows for removal and replacement of approximately 75 % of the plasma compartment and thus removal of a significant portion (~65 % per round) of DSAs; thus, multiple rounds are required [62, 63]. Most common side effects include hypotension due to volume depletion associated with plasma removal, especially in smaller patients, and hypocalcemia due to the use of citrate as an anticoagulant. Blood priming and co-administration of a calcium infusion as preventive measures facilitates this modality to be well tolerated by the pediatric population including smaller (<20 kg) children. The response rate for TPE is approximately 50 %. Thus, it is rarely used as monotherapy; however, when used in conjunction with IVIG, the success rate is 80–90 % for the treatment of acute ABMR [64, 65]. The use of TPE with chronic ABMR is variable; however, one adult study reports improvement in GFR with the use of up to 14 rounds of TPE when used in combination with IVIG [66].
Immunoadsorption is used mainly for preconditioning in the treatment of ABO-incompatible transplants and rarely in pediatrics. However, as these are not routinely conducted in the USA and immunoadsorption is not used, it is not discussed in depth in this review. Briefly, it is similar to plasmapheresis, but involves the use of a filter that specifically isolates anti-ABO antibodies. While plasmapheresis removes both IgG and IgM antibodies, immunoadsorption is more efficacious but removes only IgG antibodies.
6.1.2 Immunomodulators
Mechanisms of immunomodulation include B- and/or T-cell depletion, inhibition of cell signaling, and inhibition of complement. Current antibodies and biologics have been developed to target these points of the pathway and have been adapted to treat ABMR. Some are primarily only used in adults; however, some have been transitioned for use in pediatrics after clinical trials demonstrated efficacy and safety.
6.1.3 Cell Depletion
Rituximab, originally used to treat B-cell lymphomas, is a humanized chimeric anti-CD20 antibody that depletes mature antigen-presenting B cells from circulation and spares immature and terminally differentiated plasma cells. Its uses have extended to treating autoimmune disease as well as various pathologies for transplant, including kidney transplant rejection. A typical dose is 375 mg/m2; however, one study reports using 650 mg/m2 [67]. It has been shown to improve graft function when added to conventional therapy in treating acute ABMR in pediatrics [50, 68] and adults [69–71] via high percentage, and in some cases complete, depletion of circulating CD20+ B cells. A meta-analysis by Hychko et al. [72] favored the use of rituximab over alternative therapies [72]. It has also been successful when used for desensitization in conjunction with IVIG [46]. However, results with chronic ABMR [73] and some acute ABMR remain variable [50, 67]. The therapeutic effects can be attributed to the elimination of preconditioned B cells from circulation and reconstitution of the naïve B-cell subpopulation since pediatric ABMR patients who did not relapse after rituximab demonstrated a higher percentage of naïve B cells after repopulation [68], suggesting that the B-cell repertoire has been reprogrammed and has less propensity to form a pre-programmed immune response towards the alloantigen and thus re-achieve desensitization. Some use of rituximab is associated with increased incidences BK nephropathy [74] and other infections [72]; however, larger studies [71, 75] have suggested that there is no significant difference in infectious complications when compared with other treatments. However, in cancer studies, an increased incidence of interstitial pneumonitis has been observed when rituximab is added to the regimen [76]. This may be due to concomitant use with other chemotherapeutic agents known to have pulmonary toxicity, such as cyclophosphamide; however, this is also an agent used in some pediatric kidney patients and therefore should be taken into consideration. Due to these complications, and since other immunomodulatory therapies are available and may avoid this complication, it may be more advantageous to use an alternative such as the inhibition of complement when appropriate. Non-responders to rituximab who experience improvement with bortezomib or eculizumab may already have many terminally differentiated plasma cells, another reason to favor alternative treatment.
Bortezomib is a protease inhibitor that reduces antibody production from mature plasma cells via apoptosis and has been shown to effectively lower DSA levels [77]. Currently, it is only approved for use in multiple myeloma and mantle cell lymphoma; however, success in reduction of DSAs and treatment of ABMR for solid organ transplant has been demonstrated in large studies [78, 79]. Adult kidney transplant rejection studies have shown variable results for success when measured in terms of decreased DSAs, histological improvement, and/or improvement in graft function [80–85]. However, the cases that showed no response in graft function had improvements in DSA levels, but TPE was also used and follow-up was short, which may not have allowed enough time for reconstitution of DSAs. Subjects who maintained significantly low levels of DSAs were also given rituximab. Long-term improved graft function and DSA suppression is seen in cases where bortezomib is given after plasmapheresis, IVIG, rituximab, and steroids [67, 86], often due to minimal response to conventional treatment. A few small studies and case reports are available for pediatrics and report initial success for decrease in DSA when used at a dose of 1.3 mg/m2/dose for four doses [87]; however, rebound occurred at 1 year. A larger case–control study in adults from Waiser et al. [123] had an 18-month follow-up and shows equal efficacy in DSA reduction compared with rituximab, but more patients in the bortezomib arm had better graft function. Another pediatric case showed a decrease in all alloantibodies as well as protective tetanus and measles antibodies at 1 year when given after rituximab [88]. A downfall is that plasma cells need to already be activated, and serious hematologic, neurologic, and gastrointestinal side effects are reported in adults with the use of multiple doses. Thus, it may be more effective as adjunct therapy or for desensitization for patients with pre-formed DSA versus monotherapy for AMR. It appears that DSA suppression is better when used in conjunction with rituximab. It may also be a good alternative for rituximab non-responders. It has not yet been studied, but could be considered as preventive therapy for recurrence in transplants for patients with primary diseases that are or may be antibody driven such as autoimmune diseases (lupus) and focal segmental glomerulosclerosis. Clinical trials to assess its efficacy for treatment of chronic ABMR and late ABMR [TRIBUTE (NCT02201576; Bortezomib in Rejection of Kidney Transplants) and BORTEJECT (NCT01873157; Bortezomib in Late Antibody-Mediated Kidney Transplant Rejection)] are underway.
Alemtuzumab is an anti-CD52 antibody that results in depletion of total T cells. It is typically used for induction and prevention of development of acute and hyperacute ABMR and has not been reported as a treatment for acute ABMR. In pediatric patients, studies highlight its effect when used in induction, which results in greater prolonged depletion of CD4+ effector T cells over CD8+ T cells and an increase in the ratio of T-regulatory:effector cells at 3 months post-transplant. However at 1 year, this ratio returned to baseline, which the authors attributed to an initial increased depletion of effector memory cells and sparing of regulatory cells [89]. At the 2-year time point, 33 % of patients had developed DSAs. Other studies, including a pediatric study, describes a higher rate of rejection with alemtuzumab as induction therapy [90, 91]. Since it has a great effect in depleting effector T cells, but does not seem to prevent formation of an allo-specific T-cell effector population, it may be more effective as treatment for acute rejection and ABMR. Case studies exist that have demonstrated better efficacy in adults who were status post-living related donor transplants who had mixed ABMR and cellular rejection [92, 93] and one failed case of an adult who was status post his fourth deceased donor transplant with pure ABMR [94].
Splenectomy is the most aggressive form of treatment for all forms of antibody rejection. It effectively removes most of the peripheral reactive B cells and has been useful in the most extreme cases [95]. However, this is the least practical form of treatment for the pediatric population since it will predispose them for a longer period or a lifetime of a higher risk of infections.
6.1.4 Inhibition of Co-Stimulation
Belatacept is a biologic that is a fusion protein made from the extracellular portion of CTLA4 and a fragment of the Tc domain of IgG1. Thus, it selectively inhibits the co-stimulatory signal between T and B cells by binding to the CD86/CD80 (B7) complex. It is currently approved only for use in prevention of rejection. The Belatacept Evaluation of Nephroprotection and Efficacy as First-line Immunosuppression Trial was a 3-year randomized prospective study in adults that investigated the use of belatacept compared with cyclosporine. The purpose of this trial was to find a comparable alternative to a calcineurin inhibitor (CNI), which is known to be nephrotoxic and to lead to long-term graft dysfunction. The results not only showed improvement in long-term graft function, but also, of those who developed rejection post-belatacept, none were antibody mediated, and there was a lower rate of DSA formation in the belatacept group [96]. However, the use of belatacept in children may be limited due to the incidence of PTLD in this study being higher in those who were EBV negative. This finding is consistent with other findings that EBV seronegativity is a large risk factor for development of PTLD [97, 98]. More pediatric patients than adults who receive kidney transplants have not seroconverted (up to 40 %) [97]. The manifestations of PTLD associated with the use of belatacept, especially central nervous system manifestations (>50 %), is quite severe, putting the pediatric population at high risk; however, treatment for PTLD is also improving [99]. Currently, there are no reports on the use of belatacept in children.
Abatacept is another biologic with the same target as belatacept that is currently used for autoimmune disorders. Theoretically, it could also be effective for treatment of ABMR; however, the side effect profile is not very favorable and, in addition to a higher risk of PTLD, other side effects reported include severe viral and bacterial infections, multiple sclerosis (MS), lymphoma, dyspnea, purpura, and transaminitis. The benefits of graft survival may need to be weighed against the risks.
6.2 Chronic Antibody-Mediated Rejection
Chronic ABMR remains the most difficult to treat and has the poorest prognosis. The presence of transplant glomerulopathy on biopsy is diagnostic. The cause of chronic ABMR is not completely understood, but is strongly associated with de novo antibodies. Those who have low levels of DSA are also mildly C4d+; however, there are also some with undetectable DSA and C4d−. Some believe this is most likely due to persistently low levels of alloantibodies (anti-HLA and anti-nHLA). The treatment strategy is the same as for acute ABMR and most commonly consists of a combination of IVIG and rituximab [107], which has been shown to be somewhat successful in pediatrics; however, when not successful they are extremely difficult to treat. Bortezomib has also been shown to be successful in some recalcitrant cases. Overall, chronic ABMR remains difficult to treat. In extreme cases, as a last ditch approach, a splenectomy has been performed in adults.
No form of pharmacotherapy has been successful as monotherapy for acute or chronic ABMR; a combination of drugs that work in synergy is required. Most treatment regimens that are successful include TPE and IVIG. Currently, conventional therapy remains a combination of multiple rounds of TPE, followed by multiple rounds of IVIG and rituximab. Recalcitrant cases are treated successfully with either bortezomib or eculizumab. Prevention of ABMR via desensitization, and optimizing the induction and maintenance regimen is also an important factor. Studies for the most effective desensitization strategies include multiple rounds of IVIG with rituximab as the most commonly used regimen. Studies on eculizumab as desensitization are currently underway. However, in desensitizing a patient, in addition to clearing preformed alloantibodies, targets such as destruction of memory B cells and prior inhibition of proliferation would also be beneficial. The most commonly used induction protocols for pediatrics are either thymoglobulin or basiliximab, MMF, with or without MP. Large pediatric trials have shown that the steroid-free regimens are safe and have equal effects on DSA. Thus, even with the inclusion of steroids into induction and maintenance protocols, ABMR still develops [18, 50, 67, 108, 109]. Maintenance therapies are usually composed of a CNI such as tacrolimus and continuation of MMF.
7 Conclusions
ABMR continues to be detrimental towards graft survival. Because the age at transplantation is getting younger, improved graft survival is vital in the pediatric population since it is extremely likely that they will require more than one graft within their lifetime, such as the case of the patient presented. Unfortunately, she had lost her first graft due to mechanical complications, and difficulties encountered with her subsequent graft illustrates the difficulties we face in transplantation, such as sensitization, the naivety of the pediatric immune system and its capacity to respond to new antigen, infectious complications, the difficulties in treating ABMR, and the sequelae of difficult-to-treat ABMR. Thus, it is very important to increase the life of the first graft, prevent ABMR, and decrease the degree of sensitization to subsequent grafts.
Early formation of de novo antibodies leads to eventual graft loss [2], and pediatric patients are more likely than adults to form de novo antibodies within the first 2 years of transplant [3]. Prevention, early diagnosis, and predictive markers are key to improving graft survival. AMBR prevention lies in optimizing and emphasizing the importance of adherence to maintenance immunosuppression protocols. In treating the pediatric population, there are also special considerations such EBV and CMV status, which affect the choice of cell-depletion therapies and the use of steroids to avoid malignancy and infectious complications. Some protocols still include steroids; however, they have not been shown to affect DSA levels [3] or to be superior to other agents in treating [68] and preventing ABMR [18], and it would be beneficial to avoid them in the pediatric population.
Predictive strategies and earlier diagnosis may also lead to a shift from plasmapheresis, rituximab, and IVIG towards immunomodulators that inhibit T-/B-cell interaction to prevent antibody formation and possibly induce a peripheral immune compartment that may induce operational tolerance (Fig. 2). The immaturity of the pediatric immune system may make this more feasible. In patients who have mixed cellular rejection and ABMR, cell depletion and signal blockade therapies may also be more successful earlier in their course. The molecular signature for tolerance is currently being studied [110, 111] and may possibly be induced by specific immunomodulators, suggesting that there may be a potential for induction of operational tolerance, which would be the ultimate prevention of ABMR.
Current treatment regimens in antibody-mediated rejection are mainly targeted at the removal of antibodies followed by suppression of cellular activity and inhibition of complement. They are typically initiated after allograft damage and elevation of creatinine. With continued improvement of diagnostic tools that are less invasive and have the potential to predict antibody-mediated rejection prior to elevated creatinine, we propose that this will improve prognosis of the graft by shifting the initiation of treatment to an early time point as well as shifting the target towards immunomodulation to prevent or decrease the formation of antibodies. ABMR antibody-mediated rejection, cPRA calculated panel reactive antibodies, CRM common rejection module, DSA donor-specific antibodies, kSORT kidney Solid Organ Response Test
The continued research and discovery of nHLA alloantigens will help improve the DSA screening process while the tools for prediction and early diagnosis of ABMR become available. Together, they will hopefully change the focus of management of ABMR from treatment towards prevention and improved graft survival.
References
Einecke G, Sis B, Reeve J, Mengel M, Campbell PM, Hidalgo LG, et al. Antibody-mediated microcirculation injury is the major cause of late kidney transplant failure. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2009;9(11):2520–31. doi:10.1111/j.1600-6143.2009.02799.x.
Lee PC, Zhu L, Terasaki PI, Everly MJ. HLA-specific antibodies developed in the first year posttransplant are predictive of chronic rejection and renal graft loss. Transplantation. 2009;88(4):568–74. doi:10.1097/TP.0b013e3181b11b72.
Chaudhuri A, Ozawa M, Everly MJ, Ettenger R, Dharnidharka V, Benfield M, et al. The clinical impact of humoral immunity in pediatric renal transplantation. J Am Soc Nephrol JASN. 2013;24(4):655–64. doi:10.1681/ASN.2012070663.
Naesens M, Khatri P, Li L, Sigdel TK, Vitalone MJ, Chen R, et al. Progressive histological damage in renal allografts is associated with expression of innate and adaptive immunity genes. Kidney Int. 2011;80(12):1364–76. doi:10.1038/ki.2011.245.
Kurt-Jones EA, Belko J, Yu C, Newburger PE, Wang J, Chan M, et al. The role of toll-like receptors in herpes simplex infection in neonates. J Infect Dis. 2005;191(5):746–8. doi:10.1086/427339.
Shey MS, Nemes E, Whatney W, de Kock M, Africa H, Barnard C, et al. Maturation of innate responses to mycobacteria over the first nine months of life. J Immunol. 2014;192(10):4833–43. doi:10.4049/jimmunol.1400062.
Adkins B. T-cell function in newborn mice and humans. Immunol Today. 1999;20(7):330–5.
Salio M, Dulphy N, Renneson J, Herbert M, McMichael A, Marchant A, et al. Efficient priming of antigen-specific cytotoxic T lymphocytes by human cord blood dendritic cells. Int Immunol. 2003;15(10):1265–73.
Kutlu NO, Akinci A, Sonmezgoz E, Temel I, Evliyaoglu E. The effects of androstenediol and dehydroepiandrosterone on the immune response to BCG at puberty. J Trop Pediatr. 2003;49(3):181–5.
Kissick HT, Sanda MG, Dunn LK, Pellegrini KL, On ST, Noel JK, et al. Androgens alter T-cell immunity by inhibiting T-helper 1 differentiation. Proc Natl Acad Sci USA. 2014;111(27):9887–92. doi:10.1073/pnas.1402468111.
Maret A, Coudert JD, Garidou L, Foucras G, Gourdy P, Krust A, et al. Estradiol enhances primary antigen-specific CD4 T cell responses and Th1 development in vivo. Essential role of estrogen receptor alpha expression in hematopoietic cells. Eur J Immunol. 2003;33(2):512–21. doi:10.1002/immu.200310027.
Straub RH, Schuld A, Mullington J, Haack M, Scholmerich J, Pollmacher T. The endotoxin-induced increase of cytokines is followed by an increase of cortisol relative to dehydroepiandrosterone (DHEA) in healthy male subjects. J Endocrinol. 2002;175(2):467–74.
Splawski JB, Lipsky PE. Cytokine regulation of immunoglobulin secretion by neonatal lymphocytes. J Clin Investig. 1991;88(3):967–77. doi:10.1172/JCI115400.
Siegrist CA. Neonatal and early life vaccinology. Vaccine. 2001;19(25–26):3331–46.
Upham JW, Lee PT, Holt BJ, Heaton T, Prescott SL, Sharp MJ, et al. Development of interleukin-12-producing capacity throughout childhood. Infect Immun. 2002;70(12):6583–8.
Li L, Chaudhuri A, Weintraub LA, Hsieh F, Shah S, Alexander S, et al. Subclinical cytomegalovirus and Epstein–Barr virus viremia are associated with adverse outcomes in pediatric renal transplantation. Pediatr Transplant. 2007;11(2):187–95. doi:10.1111/j.1399-3046.2006.00641.x.
Nalesnik MA. Clinicopathologic characteristics of post-transplant lymphoproliferative disorders. Recent Results Cancer Res Fortschritte der Krebsforschung Progres dans les recherches sur le Cancer. 2002;159:9–18.
Sarwal MM, Ettenger RB, Dharnidharka V, Benfield M, Mathias R, Portale A, et al. Complete steroid avoidance is effective and safe in children with renal transplants: a multicenter randomized trial with three-year follow-up. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2012;12(10):2719–29. doi:10.1111/j.1600-6143.2012.04145.x.
Patel R, Terasaki PI. Significance of the positive crossmatch test in kidney transplantation. N Engl J Med. 1969;280(14):735–9. doi:10.1056/NEJM196904032801401.
Chemouny JM, Suberbielle C, Rabant M, Zuber J, Alyanakian MA, Lebreton X, et al. De novo donor-specific human leukocyte antigen antibodies in nonsensitized kidney transplant recipients after t cell-mediated rejection. Transplantation. 2014;. doi:10.1097/TP.0000000000000448.
Sarwal M, Chua M-S, Kambham N, Hsieh S-C, Satterwhite T, Masek M, et al. Molecular heterogeneity in acute renal allograft rejection identified by DNA microarray profiling. N Engl J Med. 2003;349(2):125–38.
Loupy A, Lefaucheur C, Vernerey D, Prugger C, Duong van Huyen JP, Mooney N, et al. Complement-binding anti-HLA antibodies and kidney-allograft survival. N Engl J Med. 2013;369(13):1215–26. doi:10.1056/NEJMoa1302506.
Cerilli J, Brasile L, Galouzis T, Lempert N, Clarke J. The vascular endothelial cell antigen system. Transplantation. 1985;39(3):286–9.
Paul LC, Baldwin WM 3rd, van Es LA. Vascular endothelial alloantigens in renal transplantation. Transplantation. 1985;40(2):117–23.
Jordan SC, Yap HK, Sakai RS, Alfonso P, Fitchman M. Hyperacute allograft rejection mediated by anti-vascular endothelial cell antibodies with a negative monocyte crossmatch. Transplantation. 1988;46(4):585–7.
Opelz G, Collaborative Transplant S. Non-HLA transplantation immunity revealed by lymphocytotoxic antibodies. Lancet. 2005;365(9470):1570–6. doi:10.1016/S0140-6736(05)66458-6.
Sumitran-Karuppan S, Tyden G, Reinholt F, Berg U, Moller E. Hyperacute rejections of two consecutive renal allografts and early loss of the third transplant caused by non-HLA antibodies specific for endothelial cells. Transplant Immunol. 1997;5(4):321–7.
Zafar MN, Terasaki PI, Naqvi SA, Rizvi SA. Non-HLA antibodies after rejection of HLA identical kidney transplants. Clin Transpl. 2006;421–6.
Sumitran-Holgersson S. Relevance of MICA and other non-HLA antibodies in clinical transplantation. Curr Opin Immunol. 2008;20(5):607–13. doi:10.1016/j.coi.2008.07.005.
Banasik M, Boratynska M, Koscielska-Kasprzak K, Krajewska M, Mazanowska O, Kaminska D, et al. The impact of non-HLA antibodies directed against endothelin-1 type A receptors (ETAR) on early renal transplant outcomes. Transpl Immunol. 2014;30(1):24–9. doi:10.1016/j.trim.2013.10.007.
Sun Q, Liu Z, Chen J, Chen H, Wen J, Cheng D, et al. Circulating anti-endothelial cell antibodies are associated with poor outcome in renal allograft recipients with acute rejection. Clin J Am Soc Ephrol CJASN. 2008;3(5):1479–86. doi:10.2215/CJN.04451007.
Butte AJ, Sigdel TK, Wadia PP, Miklos DB, Sarwal MM. Protein microarrays discover angiotensinogen and PRKRIP1 as novel targets for autoantibodies in chronic renal disease. Mol Cell Proteomics MCP. 2011;10(3):M110.000497. doi:10.1074/mcp.M110.000497.
Sis B, Halloran PF. Endothelial transcripts uncover a previously unknown phenotype: C4d-negative antibody-mediated rejection. Curr Opin Organ Transplant. 2010;15(1):42–8. doi:10.1097/MOT.0b013e3283352a50.
Panigrahi A, Gupta N, Siddiqui JA, Margoob A, Bhowmik D, Guleria S, et al. Post transplant development of MICA and anti-HLA antibodies is associated with acute rejection episodes and renal allograft loss. Hum Immunol. 2007;68(5):362–7. doi:10.1016/j.humimm.2007.01.006.
Zou Y, Stastny P, Susal C, Dohler B, Opelz G. Antibodies against MICA antigens and kidney-transplant rejection. N Engl J Med. 2007;357(13):1293–300. doi:10.1056/NEJMoa067160.
Sutherland SM, Li L, Sigdel TK, Wadia PP, Miklos DB, Butte AJ, et al. Protein microarrays identify antibodies to protein kinase Czeta that are associated with a greater risk of allograft loss in pediatric renal transplant recipients. Kidney Int. 2009;76(12):1277–83. doi:10.1038/ki.2009.384.
Jackson AM, Sigdel TK, Delville M, Hsieh SC, Dai H, Bagnasco S, et al. Endothelial cell antibodies associated with novel targets and increased rejection. J Am Soc Nephrol JASN. 2014;. doi:10.1681/ASN.2013121277.
Sigdel TK, Salomonis N, Nicora CD, Ryu S, He J, Dinh V, et al. The identification of novel potential injury mechanisms and candidate biomarkers in renal allograft rejection by quantitative proteomics. Mol Cell Proteomics MCP. 2014;13(2):621–31. doi:10.1074/mcp.M113.030577.
van Twillert I, van Gaans-van den Brink JA, Poelen MC, Helm K, Kuipers B, Schipper M, et al. Age related differences in dynamics of specific memory B cell populations after clinical pertussis infection. PloS One. 2014;9(1):e85227. doi:10.1371/journal.pone.0085227.
Comans-Bitter WM, de Groot R, van den Beemd R, Neijens HJ, Hop WC, Groeneveld K, et al. Immunophenotyping of blood lymphocytes in childhood. Reference values for lymphocyte subpopulations. J Pediatr. 1997;130(3):388–93.
van Gent R, van Tilburg CM, Nibbelke EE, Otto SA, Gaiser JF, Janssens-Korpela PL, et al. Refined characterization and reference values of the pediatric T- and B-cell compartments. Clin Immunol. 2009;133(1):95–107. doi:10.1016/j.clim.2009.05.020.
Morbach H, Eichhorn EM, Liese JG, Girschick HJ. Reference values for B cell subpopulations from infancy to adulthood. Clin Exp Immunol. 2010;162(2):271–9. doi:10.1111/j.1365-2249.2010.04206.x.
Everly MJ, Everly JJ, Arend LJ, Brailey P, Susskind B, Govil A, et al. Reducing de novo donor-specific antibody levels during acute rejection diminishes renal allograft loss. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2009;9(5):1063–71. doi:10.1111/j.1600-6143.2009.02577.x.
Haas M. An updated Banff schema for diagnosis of antibody-mediated rejection in renal allografts. Curr Opin Organ Transplant. 2014;19(3):315–22. doi:10.1097/MOT.0000000000000072.
Racusen LC, Colvin RB, Solez K, Mihatsch MJ, Halloran PF, Campbell PM, et al. Antibody-mediated rejection criteria - an addition to the Banff 97 classification of renal allograft rejection. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2003;3(6):708–14.
Vo AA, Choi J, Cisneros K, Reinsmoen N, Haas M, Ge S, et al. Benefits of rituximab combined with intravenous immunoglobulin for desensitization in kidney transplant recipients. Transplantation. 2014;98(3):312–9. doi:10.1097/TP.0000000000000064.
Crespo M, Torio A, Mas V, Redondo D, Perez-Saez MJ, Mir M, et al. Clinical relevance of pretransplant anti-HLA donor-specific antibodies: does C1q-fixation matter? Transpl Immunol. 2013;29(1–4):28–33. doi:10.1016/j.trim.2013.07.002.
Thammanichanond D, Mongkolsuk T, Rattanasiri S, Kantachuvesiri S, Worawichawong S, Jirasiritham S, et al. Significance of C1q-fixing donor-specific antibodies after kidney transplantation. Transplant Proc. 2014;46(2):368–71. doi:10.1016/j.transproceed.2013.11.011.
Sicard A, Ducreux S, Rabeyrin M, Couzi L, McGregor B, Badet L, et al. Detection of C3d-binding donor-specific anti-HLA antibodies at diagnosis of humoral rejection predicts renal graft loss. J Am Soc Nephrol JASN. 2014;. doi:10.1681/ASN.2013101144.
Gulleroglu K, Baskin E, Bayrakci US, Turan M, Ozdemir BH, Moray G, et al. Antibody-mediated rejection and treatment in pediatric patients: one center’s experience. Exp Clin Transplant Off J Middle East Soc Organ Transplant. 2013;11(5):404–7.
Loupy A, Suberbielle-Boissel C, Hill GS, Lefaucheur C, Anglicheau D, Zuber J, et al. Outcome of subclinical antibody-mediated rejection in kidney transplant recipients with preformed donor-specific antibodies. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2009;9(11):2561–70. doi:10.1111/j.1600-6143.2009.02813.x.
Naesens M, Salvatierra O, Benfield M, Ettenger RB, Dharnidharka V, Harmon W, et al. Subclinical inflammation and chronic renal allograft injury in a randomized trial on steroid avoidance in pediatric kidney transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2012;12(10):2730–43. doi:10.1111/j.1600-6143.2012.04144.x.
Pham MX, Teuteberg JJ, Kfoury AG, Starling RC, Deng MC, Cappola TP, et al. Gene-expression profiling for rejection surveillance after cardiac transplantation. N Engl J Med. 2010;362(20):1890–900. doi:10.1056/NEJMoa0912965.
Sarwal M, Sigdel T. A common blood gene assay predates clinical and histological rejection in kidney and heart allografts. Clin Transpl. 2013;241–7.
Chen R, Sigdel TK, Li L, Kambham N, Dudley JT, Hsieh SC, et al. Differentially expressed RNA from public microarray data identifies serum protein biomarkers for cross-organ transplant rejection and other conditions. PLoS Comput Biol. 2010;6(9). doi:10.1371/journal.pcbi.1000940.
Khatri P, Roedder S, Kimura N, De Vusser K, Morgan AA, Gong Y, et al. A common rejection module (CRM) for acute rejection across multiple organs identifies novel therapeutics for organ transplantation. J Exp Med. 2013;210(11):2205–21. doi:10.1084/jem.20122709.
Halloran PF, Pereira AB, Chang J, Matas A, Picton M, De Freitas D, et al. Microarray diagnosis of antibody-mediated rejection in kidney transplant biopsies: an international prospective study (INTERCOM). Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2013;13(11):2865–74. doi:10.1111/ajt.12465.
Loupy A, Lefaucheur C, Vernerey D, Chang J, Hidalgo LG, Beuscart T, et al. Molecular microscope strategy to improve risk stratification in early antibody-mediated kidney allograft rejection. J Am Soc Nephrol JASN. 2014;25(10):2267–77. doi:10.1681/ASN.2013111149.
Li L, Khatri P, Sigdel TK, Tran T, Ying L, Vitalone MJ, et al. A peripheral blood diagnostic test for acute rejection in renal transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2012;12(10):2710–8. doi:10.1111/j.1600-6143.2012.04253.x.
Roedder S, Sigdel T, Salomonis N, Hsieh S, Dai H, Bestard O, et al. The kSORT assay to detect renal transplant patients at high risk for acute rejection: results of the multicenter AART study. PLoS Med. 2014;11(11):e1001759. doi:10.1371/journal.pmed.1001759.
Hayde N, Broin PO, Bao Y, de Boccardo G, Lubetzky M, Ajaimy M, et al. Increased intragraft rejection-associated gene transcripts in patients with donor-specific antibodies and normal biopsies. Kidney Int. 2014;86(3):600–9. doi:10.1038/ki.2014.75.
Jackups R Jr, Canter C, Sweet SC, Mohanakumar T, Morris GP. Measurement of donor-specific HLA antibodies following plasma exchange therapy predicts clinical outcome in pediatric heart and lung transplant recipients with antibody-mediated rejection. J Clin Apher. 2013;28(4):301–8. doi:10.1002/jca.21270.
Okafor C, Ward DM, Mokrzycki MH, Weinstein R, Clark P, Balogun RA. Introduction and overview of therapeutic apheresis. J Clin Apher. 2010;25(5):240–9.
Montgomery RA, Zachary AA, Racusen LC, Leffell MS, King KE, Burdick J, et al. Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. Transplantation. 2000;70(6):887–95.
Rocha PN, Butterly DW, Greenberg A, Reddan DN, Tuttle-Newhall J, Collins BH, et al. Beneficial effect of plasmapheresis and intravenous immunoglobulin on renal allograft survival of patients with acute humoral rejection. Transplantation. 2003;75(9):1490–5. doi:10.1097/01.TP.0000060252.57111.AC.
Ruangkanchanasetr P, Satirapoj B, Termmathurapoj S, Namkhanisorn K, Suaywan K, Nimkietkajorn V, et al. Intensive plasmapheresis and intravenous immunoglobulin for treatment of antibody-mediated rejection after kidney transplant. Exp Clin Transplant Off J Middle East Soc Organ Transplant. 2014;12(4):328–33.
Nguyen S, Gallay B, Butani L. Efficacy of bortezomib for reducing donor-specific antibodies in children and adolescents on a steroid minimization regimen. Pediatr Transplant. 2014;18(5):463–8. doi:10.1111/petr.12274.
Zarkhin V, Lovelace PA, Li L, Hsieh SC, Sarwal MM. Phenotypic evaluation of B-cell subsets after rituximab for treatment of acute renal allograft rejection in pediatric recipients. Transplantation. 2011;91(9):1010–8. doi:10.1097/TP.0b013e318213df29.
Becker YT, Becker BN, Pirsch JD, Sollinger HW. Rituximab as treatment for refractory kidney transplant rejection. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2004;4(6):996–1001. doi:10.1111/j.1600-6143.2004.00454.x.
Faguer S, Kamar N, Guilbeaud-Frugier C, Fort M, Modesto A, Mari A, et al. Rituximab therapy for acute humoral rejection after kidney transplantation. Transplantation. 2007;83(9):1277–80. doi:10.1097/01.tp.0000261113.30757.d1.
Kaposztas Z, Podder H, Mauiyyedi S, Illoh O, Kerman R, Reyes M, et al. Impact of rituximab therapy for treatment of acute humoral rejection. Clin Transplant. 2009;23(1):63–73. doi:10.1111/j.1399-0012.2008.00902.x.
Hychko G, Mirhosseini A, Parhizgar A, Ghahramani N. A Systematic Review and Meta-Analysis of Rituximab in Antibody-mediated Renal Allograft Rejection. Int J Organ Transplant Med. 2011;2(2):51–6.
Kahwaji J, Najjar R, Kancherla D, Villicana R, Peng A, Jordan S, et al. Histopathologic features of transplant glomerulopathy associated with response to therapy with intravenous immune globulin and rituximab. Clin Transplant. 2014;28(5):546–53. doi:10.1111/ctr.12345.
Delbue S, Ferraresso M, Elia F, Belingheri M, Carloni C, Signorini L, et al. Investigation of polyomaviruses replication in pediatric patients with nephropathy receiving rituximab. J Med Virol. 2012;84(9):1464–70. doi:10.1002/jmv.23339.
Kahwaji J, Sinha A, Toyoda M, Ge S, Reinsmoen N, Cao K, et al. Infectious complications in kidney-transplant recipients desensitized with rituximab and intravenous immunoglobulin. Clin J Am Soc Nephrol CJASN. 2011;6(12):2894–900. doi:10.2215/CJN.03710411.
Salmasi G, Li M, Sivabalasundaram V, Panzarella T, Tsang R, Kukreti V, et al. Incidence of pneumonitis in patients with non-Hodgkin lymphoma receiving chemoimmunotherapy with Rituximab. Leuk Lymphoma. 2014;1–19. doi:10.3109/10428194.2014.963075.
Perry DK, Burns JM, Pollinger HS, Amiot BP, Gloor JM, Gores GJ, et al. Proteasome inhibition causes apoptosis of normal human plasma cells preventing alloantibody production. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2009;9(1):201–9. doi:10.1111/j.1600-6143.2008.02461.x.
Patel J, Everly M, Chang D, Kittleson M, Reed E, Kobashigawa J. Reduction of alloantibodies via proteasome inhibition in cardiac transplantation. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2011;30(12):1320–6. doi:10.1016/j.healun.2011.08.009.
Paterno F, Shiller M, Tillery G, O’Leary JG, Susskind B, Trotter J, et al. Bortezomib for acute antibody-mediated rejection in liver transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2012;12(9):2526–31. doi:10.1111/j.1600-6143.2012.04126.x.
Tzvetanov I, Spaggiari M, Joseph J, Jeon H, Thielke J, Oberholzer J, et al. The use of bortezomib as a rescue treatment for acute antibody-mediated rejection: report of three cases and review of literature. Transplant Proc. 2012;44(10):2971–5. doi:10.1016/j.transproceed.2012.02.037.
Hardinger KL, Murillo D. The influence of bortezomib on donor specific antibody reduction in patients with antibody mediated rejection. Clin Transpl. 2011;401–8.
Sureshkumar KK, Hussain SM, Marcus RJ, Ko TY, Khan AS, Tom K, et al. Proteasome inhibition with bortezomib: an effective therapy for severe antibody mediated rejection after renal transplantation. Clin Nephrol. 2012;77(3):246–53.
Yang KS, Jeon H, Park Y, Jo IH, Kim JI, Moon IS, et al. Use of bortezomib as anti-humoral therapy in kidney transplantation. J Korean Med Sci. 2014;29(5):648–51. doi:10.3346/jkms.2014.29.5.648.
Gupta G, Abu Jawdeh BG, Racusen LC, Bhasin B, Arend LJ, Trollinger B, et al. Late antibody-mediated rejection in renal allografts: outcome after conventional and novel therapies. Transplantation. 2014;97(12):1240–6. doi:10.1097/01.TP.0000442503.85766.91.
Sberro-Soussan R, Zuber J, Suberbielle-Boissel C, Legendre C. Bortezomib alone fails to decrease donor specific anti-HLA antibodies: 4 case reports. Clin Transpl. 2009;433–8.
Kranz B, Kelsch R, Kuwertz-Broking E, Brocker V, Wolters HH, Konrad M. Acute antibody-mediated rejection in paediatric renal transplant recipients. Pediatr Nephrol. 2011;26(7):1149–56. doi:10.1007/s00467-011-1864-3.
Morrow WR, Frazier EA, Mahle WT, Harville TO, Pye SE, Knecht KR, et al. Rapid reduction in donor-specific anti-human leukocyte antigen antibodies and reversal of antibody-mediated rejection with bortezomib in pediatric heart transplant patients. Transplantation. 2012;93(3):319–24. doi:10.1097/TP.0b013e31823f7eea.
Claes DJ, Yin H, Goebel J. Protective immunity and use of bortezomib for antibody-mediated rejection in a pediatric kidney transplant recipient. Pediatr Transplant. 2014;18(4):E100–5. doi:10.1111/petr.12256.
De Serres SA, Mfarrej BG, Magee CN, Benitez F, Ashoor I, Sayegh MH, et al. Immune profile of pediatric renal transplant recipients following alemtuzumab induction. J Am Soc Nephrol JASN. 2012;23(1):174–82. doi:10.1681/ASN.2011040360.
Kirk AD, Hale DA, Mannon RB, Kleiner DE, Hoffmann SC, Kampen RL, et al. Results from a human renal allograft tolerance trial evaluating the humanized CD52-specific monoclonal antibody alemtuzumab (CAMPATH-1H). Transplantation. 2003;76(1):120–9. doi:10.1097/01.TP.0000071362.99021.D9.
Bartosh SM, Knechtle SJ, Sollinger HW. Campath-1H use in pediatric renal transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2005;5(6):1569–73. doi:10.1111/j.1600-6143.2005.00879.x.
Csapo Z, Benavides-Viveros C, Podder H, Pollard V, Kahan B. Campath-1H as rescue therapy for the treatment of acute rejection in kidney transplant patients. Transplant Proc. 2005;37(5):2032–6.
Jirasiritham S, Khunprakant R, Techawathanawanna N, Jirasiritham S, Mavichak V. Treatment of simultaneous acute antibody-mediated rejection and acute cellular rejection with alemtuzumab in kidney transplantation: a case report. Transplant Proc. 2010;42(3):987–9. doi:10.1016/j.transproceed.2010.03.018.
Thomas PG, Ishihara K, Vaidya S, Gugliuzza KK. Campath and renal transplant rejection. Clin Transplant. 2004;18(6):759–61. doi:10.1111/j.1399-0012.2004.00288.x.
Locke J, Zachary A, Haas M, Melancon J, Warren D, Simpkins C, et al. The utility of splenectomy as rescue treatment for severe acute antibody mediated rejection. Am J Transplant. 2007;7(4):842–6.
Vincenti F, Larsen CP, Alberu J, Bresnahan B, Garcia VD, Kothari J, et al. Three-year outcomes from BENEFIT, a randomized, active-controlled, parallel-group study in adult kidney transplant recipients. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2012;12(1):210–7. doi:10.1111/j.1600-6143.2011.03785.x.
Rahimzadeh N, Otukesh H, Hoseini R, Riahifard A. Pretransplant Epstein–Barr virus serostatus and incidence of posttransplant lymphoproliferative disorder in pediatric renal transplants. Exp Clin Transplant Off J Middle East Soc Organ Transplant. 2013;11(4):299–302.
Ellis D, Jaffe R, Green M, Janosky JJ, Lombardozzi-Lane S, Shapiro R, et al. Epstein–Barr virus-related disorders in children undergoing renal transplantation with tacrolimus-based immunosuppression. Transplantation. 1999;68(7):997–1003.
Wistinghausen B, Gross TG, Bollard C. Post-transplant lymphoproliferative disease in pediatric solid organ transplant recipients. Pediatr Hematol Oncol. 2013;30(6):520–31. doi:10.3109/08880018.2013.798844.
Jordan SC, Vo AA, Toyoda M, Tyan D, Nast CC. Post-transplant therapy with high-dose intravenous gammaglobulin: applications to treatment of antibody-mediated rejection. Pediatr Transplant. 2005;9(2):155–61. doi:10.1111/j.1399-3046.2005.00256.x.
Tyan DB, Li VA, Czer L, Trento A, Jordan SC. Intravenous immunoglobulin suppression of HLA alloantibody in highly sensitized transplant candidates and transplantation with a histoincompatible organ. Transplantation. 1994;57(4):553–62.
Stegall MD, Diwan T, Raghavaiah S, Cornell LD, Burns J, Dean PG, et al. Terminal complement inhibition decreases antibody-mediated rejection in sensitized renal transplant recipients. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2011;11(11):2405–13. doi:10.1111/j.1600-6143.2011.03757.x.
Locke JE, Magro CM, Singer AL, Segev DL, Haas M, Hillel AT, et al. The use of antibody to complement protein C5 for salvage treatment of severe antibody-mediated rejection. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2009;9(1):231–5. doi:10.1111/j.1600-6143.2008.02451.x.
Orandi BJ, Zachary AA, Dagher NN, Bagnasco SM, Garonzik-Wang JM, Van Arendonk KJ, et al. Eculizumab and splenectomy as salvage therapy for severe antibody-mediated rejection after HLA-incompatible kidney transplantation. Transplantation. 2014;98(8):857–63. doi:10.1097/TP.0000000000000298.
Ghirardo G, Benetti E, Poli F, Vidal E, Della Vella M, Cozzi E, et al. Plasmapheresis-resistant acute humoral rejection successfully treated with anti-C5 antibody. Pediatr Transplant. 2014;18(1):E1–5. doi:10.1111/petr.12187.
Burbach M, Suberbielle C, Brocheriou I, Ridel C, Mesnard L, Dahan K, et al. Report of the inefficacy of eculizumab in two cases of severe antibody-mediated rejection of renal grafts. Transplantation. 2014;98(10):1056–9. doi:10.1097/TP.0000000000000184.
Billing H, Rieger S, Ovens J, Süsal C, Melk A, Waldherr R, et al. Successful treatment of chronic antibody-mediated rejection with IVIG and rituximab in pediatric renal transplant recipients. Transplantation. 2008;86(9):1214–21.
Twombley K, Thach L, Ribeiro A, Joseph C, Seikaly M. Acute antibody-mediated rejection in pediatric kidney transplants: a single center experience. Pediatr Transplant. 2013;17(7):E149–55. doi:10.1111/petr.12129.
Comoli P, Quartuccio G, Cioni M, Parodi A, Nocera A, Basso S, et al. Posttransplant soluble B-cell activating factor kinetics in pediatric recipients of first kidney allograft. Transplantation. 2015;99(1):243–9. doi:10.1097/TP.0000000000000276.
Gokmen R, Hernandez-Fuentes MP. Biomarkers of tolerance. Curr Opin Organ Transplant. 2013;18(4):416–20. doi:10.1097/MOT.0b013e3283636fd5.
Soulillou JP, Giral M, Brouard S. Operational tolerance in kidney transplantation-improved terminology may enable more precise investigation. Transplantation. 2013;96(5):e36–8. doi:10.1097/TP.0b013e31829f75c1.
Solez K, Colvin RB, Racusen LC, Haas M, Sis B, Mengel M, et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2008;8(4):753–60. doi:10.1111/j.1600-6143.2008.02159.x.
Racusen LC, Solez K, Colvin RB, Bonsib SM, Castro MC, Cavallo T, et al. The Banff 97 working classification of renal allograft pathology. Kidney Int. 1999;55(2):713–23. doi:10.1046/j.1523-1755.1999.00299.x.
Solez K, Benediktsson H, Cavallo T, Croker B, Demetris AJ, Drachenberg C, et al. Report of the third Banff conference on allograft pathology (July 20–24, 1995) on classification and lesion scoring in renal allograft pathology. Transplant Proc. 1996;28(1):441–4.
Solez K, Axelsen RA, Benediktsson H, Burdick JF, Cohen AH, Colvin RB, et al. International standardization of criteria for the histologic diagnosis of renal allograft rejection: the Banff working classification of kidney transplant pathology. Kidney Int. 1993;44(2):411–22.
Steinmetz OM, Lange-Husken F, Turner JE, Vernauer A, Helmchen U, Stahl RA, et al. Rituximab removes intrarenal B cell clusters in patients with renal vascular allograft rejection. Transplantation. 2007;84(7):842–50. doi:10.1097/01.tp.0000282786.58754.2b.
Mulley WR, Hudson FJ, Tait BD, Skene AM, Dowling JP, Kerr PG, et al. A single low-fixed dose of rituximab to salvage renal transplants from refractory antibody-mediated rejection. Transplantation. 2009;87(2):286–9. doi:10.1097/TP.0b013e31819389cc.
Zarkhin V, Li L, Kambham N, Sigdel T, Salvatierra O, Sarwal MM. A randomized, prospective trial of rituximab for acute rejection in pediatric renal transplantation. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2008;8(12):2607–17. doi:10.1111/j.1600-6143.2008.02411.x.
Everly MJ, Everly JJ, Susskind B, Brailey P, Arend LJ, Alloway RR, et al. Bortezomib provides effective therapy for antibody- and cell-mediated acute rejection. Transplantation. 2008;86(12):1754–61. doi:10.1097/TP.0b013e318190af83.
Everly MJ. A summary of bortezomib use in transplantation across 29 centers. Clin Transpl. 2009;323–37.
Flechner SM, Fatica R, Askar M, Stephany BR, Poggio E, Koo A, et al. The role of proteasome inhibition with bortezomib in the treatment of antibody-mediated rejection after kidney-only or kidney-combined organ transplantation. Transplantation. 2010;90(12):1486–92. doi:10.1097/TP.0b013e3181fdd9b0.
Walsh RC, Everly JJ, Brailey P, Rike AH, Arend LJ, Mogilishetty G, et al. Proteasome inhibitor-based primary therapy for antibody-mediated renal allograft rejection. Transplantation. 2010;89(3):277–84. doi:10.1097/TP.0b013e3181c6ff8d.
Waiser J, Budde K, Schutz M, Liefeldt L, Rudolph B, Schonemann C, et al. Comparison between bortezomib and rituximab in the treatment of antibody-mediated renal allograft rejection. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc. 2012;27(3):1246–51. doi:10.1093/ndt/gfr465.
Lonze BE, Dagher NN, Simpkins CE, Locke JE, Singer AL, Segev DL, et al. Eculizumab, bortezomib and kidney paired donation facilitate transplantation of a highly sensitized patient without vascular access. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2010;10(9):2154–60. doi:10.1111/j.1600-6143.2010.03191.x.
Chandran S, Baxter-Lowe L, Olson JL, Tomlanovich SJ, Webber A. Eculizumab for the treatment of de novo thrombotic microangiopathy post simultaneous pancreas-kidney transplantation—a case report. Transplant Proc. 2011;43(5):2097–101. doi:10.1016/j.transproceed.2011.02.064.
Noone D, Al-Matrafi J, Tinckam K, Zipfel PF, Herzenberg AM, Thorner PS, et al. Antibody mediated rejection associated with complement factor h-related protein 3/1 deficiency successfully treated with eculizumab. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2012;12(9):2546–53. doi:10.1111/j.1600-6143.2012.04124.x.
Csapo Z, Benavides-Viveros C, Podder H, Pollard V, Kahan BD. Campath-1H as rescue therapy for the treatment of acute rejection in kidney transplant patients. Transplant Proc. 2005;37(5):2032–6. doi:10.1016/j.transproceed.2005.03.042.
Acknowledgments
The authors would like to thank Dr. Aris Oates for providing us with the case write up used in our review. Y. W. Ng, M Singh, and M. M. Sarwal declare no relevant conflicts of interest. No sources of funding were used to support the writing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ng, Y.W., Singh, M. & Sarwal, M.M. Antibody-Mediated Rejection in Pediatric Kidney Transplantation: Pathophysiology, Diagnosis, and Management. Drugs 75, 455–472 (2015). https://doi.org/10.1007/s40265-015-0369-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-015-0369-y